Key Clinical Message
Splenic injury is one of the most critical complications of chest tube insertion and often requires invasive emergency management. However, noninvasive management such as delayed removal of the malpositioned tube may be considered for a stable patient without severe adverse event.
Keywords: Case report, chest tube, iatrogenic splenic injury, noninvasive management
Introduction
Chest tube insertion is one of the most important procedures in thoracic medicine. This procedure has a risk of critical complications 1. In particular, it may be fatal in there is injury caused to the cardiac cavity, an intercostal artery, pulmonary vessels, or intra‐abdominal organs 2, 3. In this situation, invasive management such as emergency surgery and transcatheter arterial embolization (TAE) may be required 4, 5, 6. However, if there is no severe adverse event immediately after injury of vital organs by the tube insertion, emergency treatment may not be required 7. Here, we describe successful noninvasive management for iatrogenic penetrating splenic injury caused by chest tube insertion.
Case Report
A 61‐year‐old Japanese male visited the internal medicine department complaining of a ten‐day episode of fatigue and left chest pain. He had a high fever (body temperature, 40.0°C), but was lucid with stable vital signs (heart rate, 96 beats/min; blood pressure, 119/70 mmHg). Blood examination showed an elevated inflammatory response (white blood cell, 12,350 cells/μL; C‐reactive protein, 35.1 mg/dL). Chest X‐ray and computed tomography (CT) scan showed an accumulation of a large amount of fluid in the left thoracic cavity. He was admitted to the internal medicine department with a diagnosis of left empyema. A chest tube was immediately inserted, and a further 800 mL of purulent pleural effusion was drained. Additionally, he was administered antibiotics. On hospital day 7, the chest tube was removed as the amount of drainage had decreased. On hospital day 13, he developed exacerbation of empyema and the chest tube was inserted again. Under local anesthesia, a 20‐French trocar tube was inserted through the 9th left intercostal space at the posterior axillary line after the location of the empyema cavity was confirmed by ultrasonography. After insertion of the tube, there was almost no fluid drainage. Chest X‐ray showed no improvement of empyema. It was gathered that fluid in the empyema cavity was too sticky to be drained. The patient was subsequently transferred to our department due to the persistent empyema despite drainage and antibiotics, and video‐assisted thoracoscopic decortications for left empyema were performed on hospital day 17. Thoracoscopic observation revealed that the chest tube was not in the thoracic cavity and was therefore left intact during operation. After the operation, CT revealed that the chest tube was malpositioned into the abdominal cavity as it had penetrated through the spleen (Fig. 1). He was thus diagnosed with iatrogenic splenic injury caused by the chest tube insertion. However, he had no symptoms and normal abdominal findings. His vital signs were stable (heart rate, 89 beats/min; blood pressure, 99/63 mmHg; body temperature, 36.2°C), and there was no drop in his hemoglobin level. There was still no drainage of fluid from the malpositioned tube.
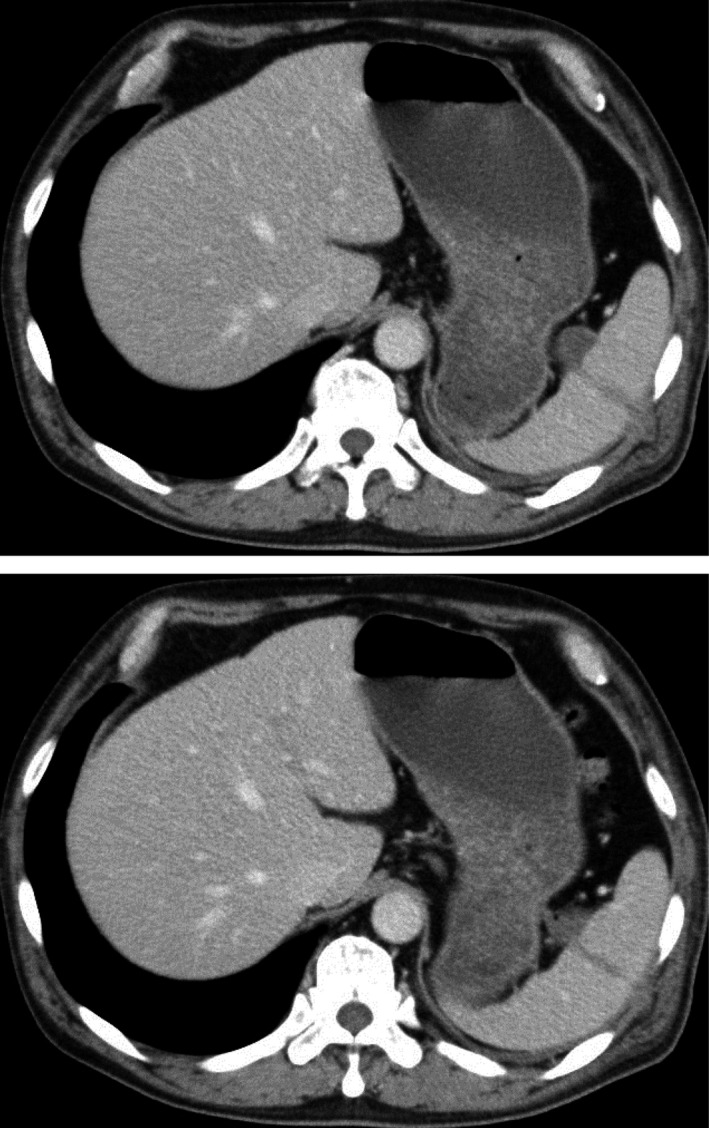
Figure 1.

Contrast‐enhanced CT after insertion of the tube. The chest tube was malpositioned into the abdominal cavity as it had penetrated through the spleen.
There were no severe adverse events such as massive bleeding immediately after accidental insertion of the tube into the spleen. A substantial time had elapsed between the accidental insertion of the tube and the diagnosis of tube malpositioning. Furthermore, his condition was stable with no evidence of bleeding at the time of diagnosis of iatrogenic splenic injury by CT. Based on these facts, we decided to perform noninvasive treatment. A treatment plan was developed to remove the malpositioned tube penetrating through the spleen 2 weeks after insertion.
The treatment for empyema was continued with antibiotics and drainage, while abdominal findings were examined and the drainage fluid from the malpositioned tube was checked every day. On hospital day 27 (14 days after insertion of the malpositioned tube), contrast study through the malpositioned tube showed that only a tube track was visualized without spreading of the contrast into the abdominal cavity, suggesting that formation of a fistula around the tube had occurred (Fig. 2). As there was a potential of bleeding in the fistula after removal, a radiologist was prepared and ready to perform TAE if severe bleeding occurred. The malpositioned tube was successfully removed through a slow, stepwise withdrawal with careful attention paid to bleeding. CT after removal showed no hemorrhage (Fig. 3). The patient's empyema was cured, and he was discharged on hospital day 34.
Figure 2.

Contrast study through the malpositioned tube. Only the tube track was visualized, without spreading of the contrast into the abdominal cavity. It suggested that formation of a fistula around the tube had occurred.
Figure 3.
Contrast‐enhanced CT after removal of the tube. There was no finding of hemorrhage.
We provided a sufficient explanation and an apology concerning iatrogenic splenic injury caused by chest tube insertion for a patient and family.
Discussion
If splenic injury unfortunately occurs as a complication after chest tube insertion, it often develops into a critical situation such as severe bleeding and shock and requires emergency treatment. In emergency surgery for iatrogenic splenic injury, attempts to preserve the spleen must be made because of the risk of overwhelming postsplenectomy infection syndrome 8. Successful hemostasis with splenic preservation by some materials, such as fibrin glue, argon beam coagulation, and absorbable mesh wrapping, has been reported 9, 10, 11. Angiographic embolization of splenic bleeding has been reported as a noninvasive emergency management for iatrogenic splenic injury 12.
If there is no severe adverse event immediately after injury of spleen by the tube insertion, emergency treatment may not be required. There have been two reported methods of conservative treatment for iatrogenic penetrating splenic injury 13, 14, 15, 16. In one method, the penetrating tube was removed with deposition of some materials such as a collagen–thrombin hemostatic sealant and an absorbable gelatin‐compressed sponge along the transsplenic tube tract 13, 14. In the second method that was the most noninvasive management, the penetrating tube was removed about 2 weeks after the insertion without any treatment 15, 16. The latter method had been reported in the patients who underwent percutaneous nephrolithotomy. Our case is the first report in noninvasive management with delayed removal of the tube for iatrogenic splenic injury after chest tube insertion. Noninvasive treatments require a long hospital stay but provide the advantage of a less invasive treatment for patients who unfortunately suffer an iatrogenic injury.
In the present case, we chose a noninvasive management with delayed removal of the malpositioned tube. There were two reasons for waiting 2 weeks. First, the hemorrhage from the damaged spleen had to be restrained by compression of the transsplenic track of the tube. As the tube had only a few lateral holes near the tip, these lateral holes were located outside of the spleen and consequently no bleeding from the spleen occurred. However, there was a potential of severe bleeding from the spleen if the tube was removed too early. Therefore, an attempt was made to restrain the hemorrhage through compression of the transsplenic track of the malpositioned tube for an extended duration. The second reason for waiting was to form a fistula around the tube. There was a risk of intra‐abdominal bleeding from the spleen even if the tube was removed after compression for an extended duration. If a fistula was formed around the tube, removal of the tube might result in bleeding in the fistula, but without intra‐abdominal bleeding. A time of 2 weeks was estimated for granulation and fistula formation around the malpositioned tube.
In the present case, a radiologist was prepared and ready to perform TAE during the delayed removal of the malpositioned tube. In conservative management, it is important to make preparations to control for any unexpected bleeding. It should be kept in mind that conservative management may fail.
To prevent this serious complication on chest tube insertion, the most important thing is to use ultrasonography to demonstrate a good site for insertion with the patient in the same position as insertion. In the present case, ultrasonography was used prior to chest tube insertion. However, the 9th left intercostal space was very low for chest tube insertion, so it was inferred that the internal medical doctor who inserted chest tube misidentified a spleen as the empyema cavity and did not make a count of ribs. Ultrasonography to demonstrate a good site for insertion prior to chest tube insertion must be performed or witnessed by a clinician who has familiarity with positional relationship between ribs and thoracic cavity.
We report a case of iatrogenic penetrating splenic injury that was successfully treated with noninvasive management and subsequent removal of the malpositioned tube 2 weeks after insertion. If a patient who unfortunately suffers an iatrogenic injury is hemodynamically stable, noninvasive management with delayed removal of the malpositioned tube may be considered.
Conflict of Interest
None declared.
Authorship
KO, RH, RC, MM, SS, YS, TL and NS treated the patient. KO drafted the manuscript. RH, RC, MM, SS, YS, TL, NS, KK and YM helped to draft the manuscript. All authors read and approved the final manuscript.
References
- 1. Kesieme, E. B. , Dongo A., Ezemba N., Irekpita E., Jebbin N., and Kesieme C.. 2012. Tube thoracotomy: complications and its management. Pulm. Med. 2012:256878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Harris, A. , O'Driscoll B. R., and Turkington P. M.. 2010. Survey of major complications of intercostals chest drain insertion in the UK. Postgrad. Med. J. 86:68–72. [DOI] [PubMed] [Google Scholar]
- 3. Boazzani, A. , Arici V., Bellinzona G., Pirrelli S., Forni E., and Oder A.. 2010. Iatrogenic pulmonary artery rupture due to chest‐tube insertion. Tex. Heart Inst. J. 37:732–733. [PMC free article] [PubMed] [Google Scholar]
- 4. Bae, J. M. 2015. Life threatening hemoperitoneum and liver injury as a result of chest tube thoracostomy. Clin. Med. Insights Case Rep. 8:15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rombolá, C. A. , Tomatis S. B., Honguero Martínexz A. F., and Atance L.. 2008. Parapneumonic pleural effusion. Accidental insertion of a chest tube into right pulmonary artery. Eur. J. Cardiothorac. Surg. 34:903. [DOI] [PubMed] [Google Scholar]
- 6. Khalil, M. W. , Cleveland T. J., Sarkar P. K., and Rao J.. 2009. Successful angiographic embolisation of bleeding into the chest wall after chest drain insertion. Interact. Cardiovasc. Thorac. Surg. 8:166–167. [DOI] [PubMed] [Google Scholar]
- 7. Tait, P. , Waheed U., and Bell S.. 2009. Successful removal of malpositioned chest drain within the liver by embolization of the transhepatic track. Cardiovasc. Intervent. Radiol. 32:825–827. [DOI] [PubMed] [Google Scholar]
- 8. Sinwar, P. D. 2014. Overwhelming post splenectomy infection syndrome – review study. Int. J. Surg. 12:1314–1316. [DOI] [PubMed] [Google Scholar]
- 9. Olmi, S. , Scaini A., Erba L., Bertolini A., Guaglio M., and Croce E.. 2007. Use of fibrin glue (Tissucol) as a hemostatic in laparoscopic conservative treatment of spleen trauma. Surg. Endosc. 21:2051–2054. [DOI] [PubMed] [Google Scholar]
- 10. Kwon, A. H. , Inui H., and Kamiyama Y.. 2001. Successful laparoscopic splenorrhaphy using argon beam coagulator for blunt traumatic splenic injury. Eur. J. Surg. 167:316–318. [DOI] [PubMed] [Google Scholar]
- 11. Steiner, Z. , Iuchtman M., Litmanovitch M., and Breitgand A.. 2008. Low morbidity profile of spleen mesh wrapping in children. Eur. J. Pediatr. Surg. 18:150–152. [DOI] [PubMed] [Google Scholar]
- 12. Kelly, M. D. 2009. Iatrogenic penetrating splenic injury treated by embolization. ANZ. J. Surg. 79:393–394. [DOI] [PubMed] [Google Scholar]
- 13. Thomas, A. A. , Pierce G., Walsh R. M., Sands M., and Noble M.. 2009. Splenic injury during percutaneous nephrolithotomy. JSLS. 13:233–236. [PMC free article] [PubMed] [Google Scholar]
- 14. Desai, A. C. , Jain S., Benway B. M., Grubb R. L. III, Picus D., and Figenshau R. S.. 2010. Splenic injury during percutaneous nephrolithotomy: a case report with novel management technique. J. Endourol. 24:541–545. [DOI] [PubMed] [Google Scholar]
- 15. Carey, R. I. , Siddiq F. M., Guerra J., and Bird V. G.. 2006. Conservative management of a splenic injury related to percutaneous nephrostolithotomy. JSLS. 10:504–506. [PMC free article] [PubMed] [Google Scholar]
- 16. Schaeffer, A. J. , Handa S. E., Lingeman J. E., and Matlaga B. R.. 2008. Transsplenic percutaneous nephrolithotomy. J. Endourol. 22:2481–2484. [DOI] [PubMed] [Google Scholar]


