Abstract
Psoriasis generally does not affect survival but has significant detrimental effect on quality of life (QOL), which may be comparable to that of ischemic heart disease, diabetes, depression, and cancer. The foremost important thing in the management of psoriasis is counseling of the patient. The clinician needs to be empathetic and spend adequate time with the patient and educating the patient about psoriasis. Clinicians should make it clear to the patient that the primary goal of treatment is control of the disease rather than cure. Eating a balanced and low glycemic diet could be an important adjuvant factor in the prevention and treatment of moderate nonpustular psoriasis. Obese people are more likely to have severe psoriasis and psoriatic arthritis than people with an average body mass index. Dietary supplementation with oily fish, rich in n-3 fatty acids, in psoriasis had shown mixed results in trials. Promising results have been documented for parenteral application of n-3 fatty acid, but not with oral supplementation. Increased smoking or alcohol abuse increases the risk of developing psoriasis and may influence disease severity, and hence must be avoided. Soaking in warm water with bath oil can be done in extensive psoriasis for hydration and emollient effect, and bland soaps or soap substitutes should be used; antiseptics should be avoided as they may irritate the skin. Relatively small, localized patches of psoriasis may improve with occlusion, i.e., waterproof adhesive dressings. The use of emollients is an internationally accepted standard adjunctive to the treatment of psoriasis. Dermatology Life Quality Index is a psychometrically sound and responsive measure of psoriasis-specific outcomes and most comprehensively captures the impact of clinical signs and symptoms on patient's well-being.
Keywords: General measures, psoriasis, therapeutic guidelines
INTRODUCTION
Psoriasis affects approximately 2% of the world's population, affecting both men and women. Although psoriasis generally does not affect survival, it has significant detrimental effect on quality of life (QOL), which may be comparable to that of ischemic heart disease, diabetes, depression, and cancer.[1] It is often linked with social stigmatization, loss of self-confidence, pain, discomfort, physical disability, and psychological distress.[2] Many patients report moderate to extreme feelings of anxiety, anger, and depression and higher frequency of suicidal ideation. According to a study using a 33-item questionnaire, anticipation of rejection and feelings of guilt and shame were the major aspects of stigmatization and correlated significantly with pruritus intensity and QOL.[3]
QOL includes all the factors that have an impact on an individual's life and represents the extent to which the hopes of an individual are matched by experience, whereas health-related quality of life (HRQOL) relates only to health aspects, including psychological, social, and physical wellbeing. Psoriasis can be a frustrating disease both for the patient and the healthcare provider, and its impacts on HRQOL have been well-documented leading to limitation in daily activities, occupational, and sexual functioning with psychosocial factors being more severely impaired than physical activities.[1,2,4,5,6]
Various factors may be attributed to the low QOL in psoriasis patients, especially the chronic and recurring nature of the disease, lack of control and fear of unexpected breakout, and feeling of hopelessness in terms of cure.[7] Moreover, measures of disease status have questionable validity in describing the true burden of illness and disease severity, thereby making HRQOL indices more relevant in the clinical scenario.[8]
These effects of psoriasis have a significant negative impact at patients’ workplace affecting employment as measured by the validated scales, including Work Productivity Assessment Index (WPAI), SF-8, and Hospital Anxiety and Depression (HADS), leading to absenteeism with nearly 60% patients reporting missing an average of 26 days a year, which is directly related to their psoriasis leading to higher financial burden.[5,9]
Gupta et al. in their study of 127 psoriasis patients found that 9.7% of patients reported their wish to be dead and 5.5% reported active suicidal ideation at the time of the study.[10]
The QOL is impaired not only in adults but also in children as assessed by a study in juvenile psoriasis patients [Children's Dermatology Life Quality Index (CDLQI)] where itching and problems with treatment had the highest impact while Psoriasis Area Severity Index (PASI) had poor correlation with QOL and treatment (especially dithranol and systemic), leading to significant decline in CDLQI.[11]
Psoriasis has a huge socioeconomic impact on patients’ lives; thus, it is important to ascertain patient's goals and prepare a treatment plan which is practical and realistic. This includes both specific treatment and general measures, including counseling, rest, and emollients, which may be important in improving the QOL of the patients.
GENERAL MEASURES
Counseling
The foremost important thing in the management of psoriasis is counseling of the patient. The clinician needs to be empathetic and spend adequate time with the patient, proactively ask questions, and counsel him with regards to the nature of the disease; its noncontagious nature (by touching the lesions while examination); its remitting and relapsing course; the factors which lead to its exacerbation such as stress, both physical and mental, drugs, and alcohol; and how to cope with the disease and carry out routine activities.[12] Educating the patient about psoriasis is important and encouragement to join organizations such as the National Psoriasis Foundation (www.psoriasis.org) may be recommended. The treating physicians need to address the patient's psychosocial needs, individualize the treatment, and ensure compliance.
Talking
Patients can be encouraged to form a group of people who support each other. Studies have shown that developing a support system (especially tangible support) including friends, family, counselors, doctors, nurses, and talking to others regarding the noncontagious nature of psoriasis lessens the negative impact on the QOL, reduces depression, and thereby reduces social discomfort.[13]
Listening
The most important aspect of patient–doctor communication is patient's perception of the doctor's interpersonal skills and their expression of empathy for the difficulties faced by the patient as a result of living with psoriasis.
Therapy should be individualized based on patients’ needs, deterioration of QOL, disease severity, relevant comorbidities (psoriasis has association with heart disease, diabetes, obesity, arthritis, inflammatory bowel disease, lymphoma, and depression), patient preference (including cost and convenience), efficacy of therapy, potential side effects, and evaluation of individual patient response. When patients are actively involved in the decisions related to the management of their psoriasis, adherence significantly increases. For long-term treatment, interventions should include care, information, reminders, self-monitoring, reinforcement, counseling, family therapy, psychological therapy, crisis intervention, telephone follow-up, and supportive care.[14] Patients are typically started on safer therapies progressing to more aggressive therapies if the response is inadequate. Patient adherence may be the largest barrier to treatment success with topical therapies, thereby necessitating frequent follow-up visits.
Patients should also be informed regarding the therapeutic options available and the potential adverse effects. Clinicians should make it clear to the patient that the primary goal of treatment is control of the disease rather than cure.[15]
RELAXATION TECHNIQUE OR MIND–BODY MEDICINE
These include intervention strategies that promote health such as Yoga, relaxation, hypnosis, visual imagery, meditation, biofeedback, tai chi, qi gong, cognitive-behavioral therapies, group support, autogenic training, and spirituality. These forms of intervention, when used as an adjunct to regular pharmacological therapy, produce a significant clinical benefit by reducing stress.
Rest
Rest, particularly bed rest, even for a short duration (few weeks) in hospital settings can really help in psoriasis patients, especially in erythrodermic and pustular psoriasis.
Role of stress in psoriasis
Emotional stress may influence the development and exacerbation of psoriasis in 37–78% patients.[16] It also lengthens the time to disease clearance further adding to psychological sequelae. According to a study, “stress reactors” were more likely to be female and those who have a family history of psoriasis, greater disease severity, higher levels of psoriasis-related stress, and greater impairment in psoriasis-related QOL.[17]
Thus, stress reduction through psychotherapy and pharmacotherapy may be useful, especially in stress responders, because they have greater disease severity than nonstress responders at the same PASI scores.[18]
Moreover, patients undergoing psoralen and ultraviolet A radiation therapy, who are high or pathological worriers, clear significantly more slowly as compared with their counterparts who are low worriers.[19]
DIETARY SUPPLEMENTS
Though unproven, a variety of dietary supplements have been used by psoriasis patients to control their disease, including evening primrose oil, milk thistle, turmeric, and oregano oil.[20]
Functional foods
Overproduction of arachidonic acid derived eicosanoids has been implicated in psoriatic skin lesions.[21] Dietary supplementation with oily fish such as mackerel, sardine, salmon, pilchard, kipper, or herring, which are rich in n-3 fatty acids, might be a useful adjunct in the treatment of psoriasis[22,23] because of its immune modulatory functions. However, randomized controlled trials have shown conflicting results. In contrast to the mostly negative results from oral supplementation studies with n-3 fatty acids, promising results are documented for parenteral application of n-3 fatty acids.[24]
Patients with psoriasis respond variably to different diets with same factors causing remission in some patients while relapse in others. Most scientific studies, however, do not show a definitive link between diet and psoriasis or psoriatic arthritis.
However, it is recommended that eating a balanced diet minimizes the risk of heart disease, diabetes, and other associated health conditions associated with psoriasis. Moreover, in a study, psoriasis patients on low energy diet had significantly lower disease severity as compared to patients on normal hospital diet; thus, low energy diet could be an important adjuvant factor in the prevention and treatment of moderate nonpustular psoriasis.[25] In addition, obese people are more likely to have severe psoriasis and psoriatic arthritis than people with an average body mass index.[26]
Role of anti-inflammatory diet?
Psoriatic patients should be advised to eat plenty of fruits, vegetables, and whole gains and avoid saturated and trans fats and refined carbohydrates and processed foods.[27] Anti-gliadin antibodies are more common in patients with psoriasis than in healthy persons and gluten-free diet may improve psoriasis severity in patients with IgA and/or IgG antibodies.[28]
A placebo controlled study showed no effect of daily supplementation of 600 µg selenium-enriched yeast alone or together with 600 IU of vitamin E on the clinical symptoms of 69 patients with psoriasis.[29]
Vitamin B12 may influence psoriasis due to its role in nucleic acid synthesis and immunomodulatory effects on T lymphocytes and cytokines. There are controversial reports of therapeutic efficacy of parenteral administration of vitamin B12.[30] The efficacy of topical vitamin B12 treatment in plaque psoriasis has been established in one study using a vitamin B12 cream containing avocado oil compared with calcipotriol treatment. Although calcipotriol produced rapid improvement, there was no significant difference between both therapies at 12 weeks of treatment and better tolerated.[31] In the Indian set up, dietary supplementation with iron, vitamin B12, and antioxidants might be useful in patients with psoriasis.
Smoking
Smoking has been described both as a risk factor for psoriasis as well as a comorbid entity to which psoriatic patients are more predisposed.[26,27] It affects the onset of psoriasis and its clinical appearance. Smoking nearly doubles a person's risk of getting psoriasis; the risk increases with the number of cigarettes smoked per day (>20 per day), and is higher in women (2.5 times) than men (1.7 times).[32] Studies have also found a very strong association between smoking and palmoplantar pustulosis and its remission on cession of smoking.[33]
Alcohol
Alcohol appears to affect psoriasis in men more strongly than in women.[27] One study found that heavy drinking lowered treatment response in men. Other studies have shown that men with psoriasis drink more and vice versa, i.e., there is a significantly higher incidence of psoriasis in alcoholics, with abstinence improving the severity of the disease. Alcohol has a negative effect on clinical response to treatment and on the likelihood of remission.[34]
Drinking alcohol may also have dangerous side effects when combined with certain psoriasis medications such as methotrexate or acitretin. Hence, cessation of alcohol is advised in psoriatic patients.
GENERAL MEASURES
Baths
Soaking in warm water with a bath oil or tar solution and use of soft brush softens and lifts the scales in patients with psoriasis. Bland soaps or soap substitutes should be used while antiseptics should be avoided because they may irritate the skin. Oatmeal baths and wet dressings relieve itching.
Occlusive dressings
Relatively small, localized patches of psoriasis may improve with occlusion, i.e., waterproof adhesive dressings. A study has shown the relative advantage of hydrocolloid dressings in patients with psoriasis as 47% of treated plaques resolved with 10 weekly applications of hydrocolloid dressing. The dressing was superior to twice daily application of potent topical steroid cream for 10 weeks.[35]
TOPICAL THERAPY
Emollients
Even if no medicated preparations are applied, psoriasis can be treated to some extent with emollients, especially in erythrodermic cases. The use of emollients is an internationally accepted standard adjunctive to treatment of psoriasis.[36] Two studies with aloe vera have reported conflicting results.[37] Hydration and emollients are valuable and inexpensive adjuncts to psoriasis treatment. Keeping psoriatic skin soft and moist minimizes the symptoms of itching and pain. The major role for emollients and moisturizers is their supportive role in normalizing hyperproliferation, differentiation, and apoptosis; furthermore, they also exert anti-inflammatory effects. Subsequently, an improved barrier function and stratum corneum hydration makes the epidermis more resistant to external stressors and irritation and reduces the induction of Koebner phenomena. Most of the emollients are lipid-rich (sometimes oily), and hence they are especially suitable in the intermediate phase and the chronic/remission phase of psoriasis. They may be combined with bath oils. The most effective are ointments such as petroleum jelly or thick creams, especially when applied immediately after a hydrating bath or shower. They also improve results with phototherapy provided applied in thin layer. In an open label study, once daily application of water in oil cream with once daily steroid cream was more effective than once daily or equal efficacy to twice daily corticosteroid cream.[38] According to another study emollients reduce itching, redness, soreness, and lesional extension in around one-third of patients;[39] oil based medications being more effective such as petrolatum and aquaphor. They do not cause irritation, atrophy, HPA axis suppression, staining, systemic side effects, and are safe for pregnant and lactating females. However, they might be messy, inconvenient to apply, and may lead to folliculitis.
SPECIAL CONDITIONS REQUIRING ADDITIONAL GENERAL MEASURES
The management of psoriasis in special conditions is done as below.[40]
Nail psoriasis
Physical maneuvers to improve nail appearance or comfort may be helpful for some patients. Patients can thin their nails by scraping them with a file or shaving them down with the edge of a glass slide. Thick toenails that are painful or interfere with footwear can be removed by a podiatrist.
Erythrodermic and pustular psoriasis
Rest and hospitalization can be used in concordance with emollients, wet dressings, and oatmeal baths.
Children
The immediate and long-term adverse effects of therapies for psoriasis are of particular concern in the pediatric population. Many agents used in the treatment of adult psoriasis have also been used for children. However, high quality studies on the efficacy and safety of therapies for psoriasis in children are limited.
Pregnant and lactating females
Studies suggest that pregnant women with psoriasis have increased risk of poor birth outcomes, including preterm births and preeclampsia.[41] Women with severe psoriasis were also found to have a higher incidence of low birth weight babies compared to those without the disease. Pregnant women should avoid psoriasis treatments altogether or use only the safest forms, including certain topical and ultraviolet B phototherapy during conception, pregnancy, and nursing. While nursing, it is important to exercise caution with treatments as systemic absorption through the skin may occur into the mother's milk. Topical steroids should not be used on the nipples. If a mother has psoriasis on her nipples, it is important to moisturize the nipples with emollients. Psoriasis on the nipple does not harm a nursing infant. However, it may cause enough discomfort to the mother to make breast-feeding difficult. Systemic medications should, however, be avoided when nursing because of the potential for passing the drugs’ active ingredients to the infant through the breast milk.
FACTORS AFFECTING QUALITY OF LIFE
Body surface area: Controversial association. Gelfand et al. showed that patients with more extensive skin involvement have greater reductions in QOL with female and young patients being affected the most.[42] Rakhesh et al. found that patients with PASI score more than 18 had higher physical disability and higher stress rating.[43] However, the study by Sampogna et al.[44] showed that poor correlation (0.1–0.3) existed between clinical severity and QOL measurements
Location:[45] psoriasis of hands and feet which may cause difficulty in performing daily chores, such as picking up things, sewing, and walking, and lesions on the exposed parts of the body or cosmetic disfigurement affects QOL more
Age and Sex:[43] Older age group and females are more severely affected
Symptoms such as itching and pain that interfere with basic functions such as self-care
Presence of associated psoriatic arthritis[46] or guttate forms
Other comorbidities
Duration of disease:[42] According to a study, duration of disease had no correlation with QOL measures demonstrating that patients do not necessarily adapt to their disease over time
Greater extent of skin involvement/higher DLQI are associated with decrements in income further impairing access to treatment.[42]
Tools to measure quality of life
These measures may be categorized as psoriasis-specific, skin specific, generic QOL measures, and “mixed” measures [Table 1]. Psoriasis-specific measures are the most sensitive, however, the more general measures facilitate comparisons across diseases. Use of these measures vary across different clinical controlled trials, examining effect of different pharmacological treatments on QOL of psoriasis patients.
Table 1.
Tools to measure quality of life in psoriasis
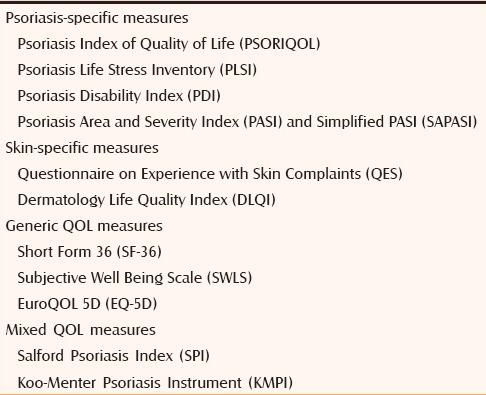
Psoriasis-specific measures
Psoriasis index of quality of life
The psoriasis index of quality of life (PSORIQOL) is a 25 dichotomous item instrument developed through interviews assessing capability of individual to satisfy their needs.
Psoriasis life stress inventory
The psoriasis life stress inventory (PLSI) is a 15-item questionnaire that provides a measure of psychosocial stress associated with coping with everyday events, with scores ranging from 0 to 45.
Psoriasis disability index
The psoriasis disability index (PDI) is a 15-item scale that specifically addresses self-reported disability in areas of daily activities, employment, personal relationships, leisure and treatment effects in everyday life.
Psoriasis area and severity index and simplified psoriasis area and severity index
PASI measures psoriasis severity clinically on the basis of body surface area involvement and erythema, scaling, and induration severity. The maximum score for PASI is 72. The simplified PASI is a simplified self-assessed scoring system.
Skin-specific measures
Questionnaire on experience with skin complaints
The short form of the questionnaire on experience with skin complaints (QES) with 23 items is a valid instrument for examination of social and psychic burdens of psoriasis, especially the stigmatization associated with this disease.
Dermatology life quality index
The DLQI is a self-reported questionnaire of 10 items (feelings, daily activities, leisure, work, personal relationships, and treatment) to measure HRQOL over the previous week in patients with skin diseases.
Generic quality of life measures
Short form 36 (SF-36)
The SF-36 health survey is a generic, 36-item, self-reported health status questionnaire assessing 8 domains of health status, namely, (1) physical activities; (2) social activities; (3) usual physical role activities; (4) bodily pain; (5) general mental health; (6) usual emotional role activities; (7) vitality; and (8) general health perceptions.
Subjective well-being scale
The subjective well-being scale (SWLS) is a validated short 5-item instrument designed to measure global life satisfaction and subjective well-being (SWB).
EuroQOL 5D
The EuroQOL 5D (EQ-5D) is a standardized generic instrument developed for describing and valuing health states. It is useful for health surveys and assessing outcomes related to treatment.
Mixed QOL measures
Salford psoriasis index
The Salford psoriasis index (SPI) is derived from combining a score of current severity of psoriasis based on the PASI, a score indicating psychosocial disability, and a score based on historical information (signs, psychosocial disability, interventions).
Koo-Menter psoriasis instrument
The Koo-Menter psoriasis instrument (KMPI) is a formal diagnostic algorithm for identifying patients with significant impact on QOL warranting systemic therapy and justifying treatment decisions for health care payers.
Recently, McKenna et al.[47] focused on generating a disease specific QOL instrument by developing questions after an extensive interview process leading to 25 and 20 question profiles specific to QOL issues for patients with psoriatic arthritis and psoriasis, respectively.
Another instrument “utilities” has been developed for skin diseases which permit interpretation between various diseases and populations. It measures the willingness of patients to trade disease free status for the remainder of their lives in exchange for a reduction in their lifespan.[48]
However, despite availability of all these scores, PASI score is the most extensively studied psoriasis clinical severity score and the most thoroughly validated according to methodological validation criteria.[49]
A prospective multicentre study comparing Skindex-29, DLQI, PDI, and Medical Outcome Study SF 36 showed that Skindex-29 had a weak but significant correlation with clinical severity with minimal floor effect; SF-36 was more sensitive than the other instruments.[50]
According to Food and drug administration (FDA) guidelines, establishing the reliability, validity, and responsiveness of these scores is necessary for their use in clinical studies. Reliability refers to the accuracy of a measure, whereas validity refers to the extent the measure actually is measuring what it purports to measure. Responsiveness refers to the capability to detect changes in the clinical status of patients or other relevant outcomes measures. Minimum important difference (MID) refers to the smallest difference in score, which patients perceive as beneficial and which necessitates a change in patient's management.[51]
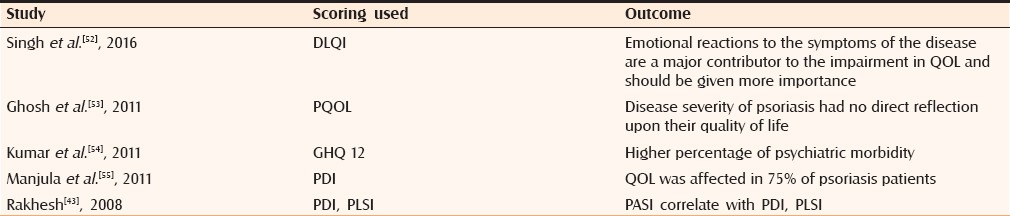
Based on this study, the DLQI is a psychometrically sound and responsive measure of psoriasis-specific outcomes and most comprehensively captures the impact of clinical signs and symptoms on patient's well-being. Table 2 summarizes various studies conducted in India about QOL.
Table 2.
Studies conducted in India regarding quality of life
Clinical utility of quality of life scores
QOL in dermatology is measured for clinical, research, audit, and for political and financial purposes and management decisions. Guidelines promulgated by the British Association of Dermatologists[51] for the use of biologics in psoriasis indicate that eligible patients must have a PASI score of at least 10 and a score on the DLQI of greater than 10.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Finlay AY, Kelly SE. Psoriasis - An index of disability. Clin Exp Dermatol. 1987;12:8–11. doi: 10.1111/j.1365-2230.1987.tb01844.x. [DOI] [PubMed] [Google Scholar]
- 2.Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel EJ. Quantifying the harmful effects of psoriasis on health related quality of life. J Am Acad Dermatol. 2002;4:512–8. doi: 10.1067/mjd.2002.122755. [DOI] [PubMed] [Google Scholar]
- 3.Hrehorów E, Salomon J, Matusiak L, Reich A, Szepietowski JC. Patients with psoriasis feel stigmatized. Acta Derm Venereol. 2012;92:67–72. doi: 10.2340/00015555-1193. [DOI] [PubMed] [Google Scholar]
- 4.Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4:35. doi: 10.1186/1477-7525-4-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finlay AY, Coles EC. The effect of severe psoriasis on the quality of life of 369 patients. Br J Dermatol. 1995;132:236–44. doi: 10.1111/j.1365-2133.1995.tb05019.x. [DOI] [PubMed] [Google Scholar]
- 6.Fortune DG, Richards HL, Griffiths CE. Psychologic factors in psoriasis: Consequences, mechanisms, and interventions. Dermatol Clin. 2005;23:681–94. doi: 10.1016/j.det.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Basra MK, Hussain S. Application of the dermatology life quality index in clinical trials of biologics for psoriasis. Chin J Integr Med. 2012;18:179–85. doi: 10.1007/s11655-012-1007-0. [DOI] [PubMed] [Google Scholar]
- 8.Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: Results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137:280–4. [PubMed] [Google Scholar]
- 9.Pearce DJ, Singh S, Balkrishnan R, Kulkarni A, Fleischer AB, Feldman SR. The negative impact of psoriasis on the workplace. J Dermatolog Treat. 2006;17:24–8. doi: 10.1080/09546630500482886. [DOI] [PubMed] [Google Scholar]
- 10.Gupta MA, Schork NJ, Gupta AK, Kirkby S, Ellis CN. Suicidal ideation in psoriasis. Int J Dermatol. 1993;32:188–90. doi: 10.1111/j.1365-4362.1993.tb02790.x. [DOI] [PubMed] [Google Scholar]
- 11.Jager ME, van de Kerkhof PC, de Jong EM, Seyger MM. A cross-sectional study using the Children's Dermatology Life Quality Index (CDLQI) in childhood psoriasis: Negative effect on quality of life and moderate correlation of CDLQI with severity scores. Br J Dermatol. 2010;163:1099–101. doi: 10.1111/j.1365-2133.2010.09993.x. [DOI] [PubMed] [Google Scholar]
- 12.Lebwohl MG, Van de Kerkhof P. Psoriasis. In: Lebwohl MG, Heymann WR, Jones JB, Coulson I, editors. Treatment of skin disease: Comprehensive therapeutic Strategies. 2nd ed. New York: Mosby International; 2002. pp. 533–43. [Google Scholar]
- 13.Janowski K, Steuden S, Pietrzak A, Krasowska D, Kaczmarek L, Gradus I, et al. Social support and adaptation to the disease in men and women with psoriasis. Arch Dermatol Res. 2012;304:421–32. doi: 10.1007/s00403-012-1235-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diagnosis and management of psoriasis and psoriatic arthritis. [Last accessed on 2012 Jun 02]. Available from: www.sign.ac.uk/guidelines .
- 15.Reich K, Mrowietz U. Treatment goals in psoriasis. J Dtsch Dermatol Ges. 2007;5:566–74. doi: 10.1111/j.1610-0387.2007.06343.x. [DOI] [PubMed] [Google Scholar]
- 16.Heller MM, Lee ES, Koo JY. Stress as an Influencing Factor in Psoriasis. [Last accessed on 2012 Jun 02]. Available from: www.Skin Therapy letter.com . [PubMed]
- 17.Pakran J, Riyaz N, Nandakumar G. determinants of quality of life in psoriasis patients: A cluster analysis of 50 patients. Indian J Dermatol. 2011;56:689. doi: 10.4103/0019-5154.91830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fortune DG, Main CJ, O’Sullivan TM, Griffiths CE. Quality of life in patients with psoriasis: The contribution of clinical variables and psoriasis-specific stress. Br J Dermatol. 1997;137:755–60. [PubMed] [Google Scholar]
- 19.Fortune DG, Richards HL, Griffiths CE. Psychologic factors in psoriasis: Consequences, mechanisms, and interventions. Dermatol Clin. 2005;23:681–94. doi: 10.1016/j.det.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 20.Wolters M. Diet and Psoriasis: Experimental Data and Clinical Evidence. Br J Dermatol. 2005;153:706–14. doi: 10.1111/j.1365-2133.2005.06781.x. [DOI] [PubMed] [Google Scholar]
- 21.Schena D, Chieregato GC, de Gironcoli M, Girelli D, Olivieri O, Stanzial AM, et al. Increased erythrocyte membrane arachidonate and platelet malondialdehyde (MDA) production in psoriasis: Normalization after fish-oil. Acta Derm Venereol. 1989;146(Suppl):42–4. [PubMed] [Google Scholar]
- 22.Collier PM, Ursell A, Zaremba K, Payne CM, Staughton RC, Sanders T. Effect of regular consumption of oily fish compared with white fish on chronic plaque psoriasis. Eur J Clin Nutr. 1993;47:251–4. [PubMed] [Google Scholar]
- 23.Wilkinson DI. Do dietary supplements of fish oils improve psoriasis? Cutis. 1990;46:334–6. [PubMed] [Google Scholar]
- 24.Mayser P, Mrowietz U, Arenberger P, Buchvald J, Christophers E, Jablonska S, et al. Omega-3 fatty acidbased lipid infusion in patients with chronic plaque psoriasis: Results of a double-blind, randomized, placebo-controlled, multicenter trial. J Am Acad Dermatol. 1998;38:539–47. doi: 10.1016/s0190-9622(98)70114-8. [DOI] [PubMed] [Google Scholar]
- 25.Rucevic I, Perl A, Barisic-Drusko V, Adam-Perl M. The role of the low energy diet in psoriasis vulgaris treatment. Coll Antropol. 2003;27(Suppl 1):41–8. [PubMed] [Google Scholar]
- 26.Naldi L, Parazzini F, Peli L, Chatenoud L, Cainelli T. Dietary factors and the risk of psoriasis. Results of an Italian case–control study. Br J Dermatol. 1996;134:101–6. [PubMed] [Google Scholar]
- 27.Poikolainen K, Karvonen J, Pukkala E. Excess mortality related to alcohol and smoking among hospital-treated patients with psoriasis. Arch Dermatol. 1999;135:1490–3. doi: 10.1001/archderm.135.12.1490. [DOI] [PubMed] [Google Scholar]
- 28.Michaelsson G, Gerdén B, Hagforsen E, Nilsson B, Pihl-Lundin I, Kraaz W, et al. Psoriasis patients with antibodies to gliadin can be improved by a gluten-free diet. Br J Dermatol. 2000;142:44–51. doi: 10.1046/j.1365-2133.2000.03240.x. [DOI] [PubMed] [Google Scholar]
- 29.Fairris GM, Lloyd B, Hinks L, Perkins PJ, Clayton BE. The effect of supplementation with selenium and vitamin E in psoriasis. Ann Clin Biochem. 1989;26:83–8. doi: 10.1177/000456328902600113. [DOI] [PubMed] [Google Scholar]
- 30.Baker H, Comaish JS. Is vitamin B12 of value in psoriasis? Br Med J. 1962;2:1729–30. doi: 10.1136/bmj.2.5321.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stucker M, Memmel U, Hoffmann M, Hartung J, Altmeyer P. Vitamin B12 cream containing avocado oil in the therapy of plaque psoriasis. Dermatology. 2001;203:141–7. doi: 10.1159/000051729. [DOI] [PubMed] [Google Scholar]
- 32.Naldi L. Cigarette smoking and psoriasis. Clin Dermatol. 1998;16:571–4. doi: 10.1016/s0738-081x(98)00040-6. [DOI] [PubMed] [Google Scholar]
- 33.Erisksson MO, Hagforsen E, Lundin IP, Michaelsson G. Palmoplantar pustulosis: A clinical and immunohistological study. Br J Dermatol. 1998;138:390–8. doi: 10.1046/j.1365-2133.1998.02113.x. [DOI] [PubMed] [Google Scholar]
- 34.Gupta MA, Schork NJ, Gupta AK, Ellis CN. Alcohol intake and treatment responsiveness of psoriasis: A prospective study. J Am Acad Dermatol. 1993;28:730–2. doi: 10.1016/0190-9622(93)70101-x. [DOI] [PubMed] [Google Scholar]
- 35.Freidman SJ. Management of psoriasis vulgaris with a hydrocolloid occlusive dressing. Arch Dermatol. 1987;123:1046–52. [PubMed] [Google Scholar]
- 36.Lebwohl MG, Van de Kerkhof P. Psoriasis. In: Lebwohl MG, Heymann WR, Jones JB, Coulson I, editors. Treatment of skin disease: Comprehensive therapeutic Strategies. 2nd ed. New York: Mosby International; 2002. pp. 533–43. [Google Scholar]
- 37.Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 3. Guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60:643–59. doi: 10.1016/j.jaad.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 38.Watsky KL, Freize L, Leneveu MC, Wenck HA, Lefell DJ. Water in oil emollients as steroid sparing adjunctive therapy in the treatment of psoriasis. Cutis. 1199;50:383–6. [PubMed] [Google Scholar]
- 39.Greaves MW, Weinstein GD. Treatment of psoriasis. N Engl J Med. 1995;332:581–8. doi: 10.1056/NEJM199503023320907. [DOI] [PubMed] [Google Scholar]
- 40.Schiener R, Brockow T, Franke A, Salzer B, Peter RU, Resch KL. Bath PUVA and saltwater baths followed by UV-B phototherapy as treatments for psoriasis: A randomized controlled trial. Arch Dermatol. 2007;143:586. doi: 10.1001/archderm.143.5.586. [DOI] [PubMed] [Google Scholar]
- 41.Greaves MW, Weinstein GD. Treatment of psoriasis. N Engl J Med. 1995;332:581–8. doi: 10.1056/NEJM199503023320907. [DOI] [PubMed] [Google Scholar]
- 42.Gelfand JM, Feldman SR, Stern RS, Thomas J, Rolstad T, Margolis DJ. Determinants of quality of life in patients with psoriasis: A study from the US population. J Am Acad Dermatol. 2004;51:704–8. doi: 10.1016/j.jaad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 43.Rakhesh SV, D’Souza M, Sahai A. Quality of life in psoriasis: A study from south India. Indian J Dermatol Venereol Leprol. 2008 Nov-Dec;74(6):600–6. doi: 10.4103/0378-6323.45101. [DOI] [PubMed] [Google Scholar]
- 44.Sampogna F, Chren MM, Melchi CF, Pasquini P, Tabolli S, Abeni D, et al. Age, gender, quality of life and psychological distress in patients hospitalized with psoriasis. Br J Dermatol. 2006;154:325–31. doi: 10.1111/j.1365-2133.2005.06909.x. [DOI] [PubMed] [Google Scholar]
- 45.Fortune DG, Main CJ, O’Sullivan TM, Griffiths CE. Quality of life in patients with psoriasis: The contribution of clinical variables and psoriasis-specific stress. Br J Dermatol. 1997;137:755–60. [PubMed] [Google Scholar]
- 46.Rosen CF, Mussani F, Chandran V, Eder L, Thavaneswaran A, Gladman DD. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology. 2012;51:571–6. doi: 10.1093/rheumatology/ker365. [DOI] [PubMed] [Google Scholar]
- 47.McKenna SP, Cook SA, Whalley D, Doward LC, Richards HL, Griffiths CE, Van Assche D. Development of the PSORIQoL, a psoriasis specific measure of quality of life designed for use in clinical practice and trials. Br J Dermatol. 2003;149:323–31. doi: 10.1046/j.1365-2133.2003.05492.x. [DOI] [PubMed] [Google Scholar]
- 48.Chen SC, Bayoumi AM, Soon SL, Aftergut K, Cruz P, Sexton SA, et al. A catalog of dermatology utilities: A measure of the burden of skin diseases. J Investig Dermatol Symp Proc. 2004;9:160–8. doi: 10.1046/j.1087-0024.2003.09112.x. [DOI] [PubMed] [Google Scholar]
- 49.Puzenat E, Bronsard V, Prey S, Gourraud PA, Aractingi S, Bagot M, et al. What are the best outcome measures for assessing plaque psoriasis severity? A systematic review of the literature. J Eur Acad Dermatol Venereol. 2010;24:10–6. doi: 10.1111/j.1468-3083.2009.03562.x. [DOI] [PubMed] [Google Scholar]
- 50.Fernandez-Peñas P, Jones-Caballero M, Espallardo O, García-Díez A. Comparison of Skindex-29, Dermatology Life Quality Index, Psoriasis Disability Index and Medical Outcome Study Short Form 36 in patients with mild to severepsoriasis. Br J Dermatol. 2012;166:884–7. doi: 10.1111/j.1365-2133.2012.10806.x. [DOI] [PubMed] [Google Scholar]
- 51.Shikiar R, Willian MK, Okun MM, Thompson CS, Revicki DA. The validity and responsiveness of three quality of life measures in the assessment of psoriasis patients: Results of a phase II study. Health Qual Life Outcomes. 2006;4:1. doi: 10.1186/1477-7525-4-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh SM, Narang T, Dogra S, Verma AK, Gupta S, Handa S. An analysis of dermatological quality-of-life scores in relation to psychiatric morbidity in psoriasis. Indian Dermatol Online J. 2016;7:208–9. doi: 10.4103/2229-5178.182371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shankar V, Ghosh S, Ghosh K, Chaudhuri U. PASI and PQOL-12 score in psoriasis: Is there any correlation. Indian J Dermatol. 2011;56:287–9. doi: 10.4103/0019-5154.82482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumar S, Kachhawha D, Das Koolwal G, Gehlot S, Awasthi A. Psychiatric morbidity in psoriasis patients: A pilot study. Indian J Dermatol Venereol Leprol. 2011;77:625. doi: 10.4103/0378-6323.84074. [DOI] [PubMed] [Google Scholar]
- 55.Manjula VD, Sreekiran S, Saril PS, Sreekanth MP. A study of psoriasis and quality of life in a tertiary care teaching hospital of Kottayam, Kerala. Indian J Dermatol. 2011;56:403–6. doi: 10.4103/0019-5154.84767. [DOI] [PMC free article] [PubMed] [Google Scholar]


