Abstract
We sought to examine the existential challenges that cancer survivors may experience as they strive to make meaning, regain their self-identity, cope with fear of recurrence, and experience feelings of grief and guilt. Lymphoma survivors (n=429) completed the 2010 LIVESTRONG survey and provided responses about meaning, cancer worry, security, identity, grief, guilt, and perceived functional impairment due to these concerns. Most survivors (73−86%) endorsed existential concerns, with 30−39% reporting related perceived functional impairment. Concerns were associated with being female, younger, unmarried, and having undergone stem cell transplantation. Lymphoma survivors experience existential challenges that impact their life even years after diagnosis.
Keywords: lymphoma, existential, survivorship, meaning, worry
Background
Nearly 80,000 adults are diagnosed with lymphoma in the United States each year (American Cancer Society, 2014). Adult-onset lymphoma can carry a generally favorable prognosis, reflected in the growing population of lymphoma survivors (Baxi and Matasar, 2010); nevertheless, a lymphoma diagnosis exerts a substantial psychological impact due to the daunting challenges of treatment and transition to survivorship. A cancer diagnosis can lead not only to psychological distress but may have a more fundamental effect on core aspects of a person’s identity, and their perceptions about the meaning of life_and what the future might hold. Further, as survivorship progresses, patients are faced with the task of returning to their daily life that generally reflects a reordering of their life priorities (Little et al., 2002; Pascal and Endacott, 2010).
Several studies have documented the emotional impact of cancer diagnosis and its effects on health-related quality of life in lymphoma survivors (Jensen et al., 2013; Mols et al., 2007; Roper et al., 2009; Smith et al., 2010), but less is known about the existential aspects of this experience. Existential aspects, generally taken to include the meaning and purpose of life and the awareness of values in life, are important because they impact one’s sense of well-being and emotional distress levels (Henoch and Danielson, 2009; Vehling et al., 2012) and could affect decision making about current or future cancer care and health maintenance behaviors (Lee and Loiselle, 2012). Awareness of one’s potential death may spur the examination of one’s life (Lee, 2008; Willig, 2009). Equally important within the domain of existential concerns, personal identity can become altered due to illness, and one task of survivorship is to restore, preserve, or incorporate new aspects of identity into one’s sense of self (Little et al., 2002; Neimeyer et al., 2006). Existential challenges also include the experience of cancer-related anxiety and uncertainty about possible recurrence and metastatic disease (Pascal and Endacott, 2010).
A cancer diagnosis offers an opportunity for self-examination as well as potential changes in self-identity (Jim and Jacobsen, 2008; Zebrack, 2000). Zebrack’s (2000) model of cancer survivorship suggests that the experience of cancer leads to identity changes for the survivor, resulting in changes in self-concept. Cancer survivors may continuously experience cancer threat and the related potential for additional change and restructuring in their lives (Zebrack, 2000). Indeed, when people are faced with a highly stressful life event, such as cancer, most undertake efforts to make meaning, or some type of cognitive readjustment, so that the stressful experience can be integrated in to one’s larger belief system about their life and the world (Park, 2010); their coping style may affect their meaning making (Schmidt et al., 2011). The extent to which lymphoma survivors experience these existential processes of identity restructuring and meaning making and what factors (sociodemographic or clinical) are associated with these concerns are unknown. We examined the prevalence of existential concerns (loss of meaning, worry about cancer recurrence and death, perceptions of a lost sense of security in the future and a lost sense of identity, and grief and guilt about seeing other cancer patients die) using data from the 2010 LIVESTRONG Survey (Rechis et al., 2011). We also evaluated respondents’ perceptions of the impact of these concerns on their current daily lives as survivors. We expected that lymphoma survivors would experience existential concerns. We also expected, based on prior studies in lymphoma populations (Jensen et al., 2013; Smith et al., 2010), that younger survivors would report the most concerns. Finally, we anticipated that women would be more likely than men to report concerns, based on findings that women tend to experience more distress in response to cancer diagnosis (Hagedoorn et al., 2008).
Method
Participants
A total of 4286 post-treatment cancer survivors responded to the 2010 LIVESTRONG survey; the current study is focused on the 429 respondents who indicated that they were post-treatment adult-onset lymphoma survivors. Forty-three percent were Hodgkin lymphoma (HL) survivors and 57% were non-Hodgkin lymphoma (NHL) survivors.
Procedure
From June 2010 through March 2011, LIVESTRONG fielded the online LIVESTRONG Survey for Post-Treatment Cancer Survivors (see (Rechis et al., 2011) for details on administration and a copy of the survey instrument). The survey was available on LIVESTRONG.org, and LIVESTRONG constituents (e.g., those who either received LIVESTRONG services or who participated in a prior LIVESTRONG event) were notified about the survey through emails, Twitter, and Facebook posts. Additionally, LIVESTRONG reached out to partner organizations (e.g., the American Cancer Society) and state cancer coalitions who shared information about the survey with their constituents. Finally, LIVESTRONG worked with National Cancer Institute Comprehensive Cancer Centers to share the survey with patients.
Measures
Existential challenges
Three sets of variables from the 2010 LIVESTRONG dataset were used to examine six existential challenges.
First, the survey included seven items from the Constructed Meaning Scale, a previously validated scale used in other cancer populations (Fife, 1995). These items were: I feel cancer is something I will never recover from; I feel cancer is serious but I will be able to return to life as it is was before my illness; I feel cancer has changed my life permanently so it will never be as good again; I feel that I have made a complete recovery from my illness; I feel that I am the same person I was before my illness; I feel that my experience with cancer has made me a better person; I feel that having cancer has interfered with my achievement of the most important goals I have set for myself. Respondents rated each item on a 1 (strongly disagree) to 4 (strongly agree) scale. Several of the statements were reverse-scored and the total score for all statements was summed where higher scores indicate more constructed meaning. The scale had adequate internal consistency in this sample (α = 0.73), given our goals of examining prevalence and correlates of respondent concerns (Graham and Naglieri, 2003). The original Constructed Meaning Scale has eight items (Fife, 1995); as only seven were included in the LIVESTRONG survey (missing item: I feel that my relationships with other people have not been negatively affected by my illness), we prorated scores to examine the equivalent of an eight-item scale so as to allow for better comparison of our results to other studies.
The second existential issue examined in the survey was cancer worry, assessed with three items: I have (a) been preoccupied with concerns about cancer;(b) worried about dying from cancer; and, (c) worried about cancer coming back. For each statement, respondents selected “yes” (coded as 1), “no” (coded as 0) and “don’t know.” For purposes of analysis, “don’t know” was coded as “no” (0). A summed scale score was created wherein higher scores meant more cancer worry (α = 0.65).
Finally, four items addressed existential issues related to security, identity, grief, and guilt. Respondents reported whether each of the following statements was true for them as a result of their experience with cancer: I have (a) lost a sense of security in my future; (b) felt that I have lost a sense of my identity; (c) felt grief about the death of other cancer patients; and, (d) felt guilt over the death of other cancer patients. Because these items each examine a distinct existential experience, they were considered individually. For each statement, respondents selected “yes” (coded as 1) “no” (coded as 0) and “don’t know.” “Don’t know” was coded as “no” (0). These items are derived from several years of work by the LIVESTRONG Foundation during which experts and survivors were consulted in a process of formative research to develop items that reflected the challenges people affected by cancer were facing when they presented to LIVESTRONG for services (Rechis et al., 2011).
Functional impairment
The degree to which the existential concerns of cancer worry, security, identity, grief, and guilt impacted respondents was assessed by asking respondents to what degree their activities were limited by these concerns in the past week (“a lot”, “a little”, “not at all” and “I don’t know”). This impairment question was asked with regard to cancer worry only if a respondent endorsed “yes” on at least one of the three cancer worry items. A second impairment question was asked if respondents endorsed at least one concern among those of security, identity, grief, or guilt. This impairment question was not asked in reference to items on the Constructed Meaning scale.
Sociodemographic characteristics
Gender, age, education level, marital status, and race/ethnicity were included in analyses.
Clinical characteristics
We examined respondents’ answers to questions regarding: type of lymphoma (Hodgkin or non-Hodgkin); time since diagnosis; type of treatment received (radiation or chemotherapy alone or combined); and whether they received a stem cell transplant.
Statistical analysis
Descriptive statistics were used to characterize the presence of existential challenges, as well as the sample’s sociodemographic and clinical characteristics. A log-transformed version of time since diagnosis was used in all analyses in order to normalize its skewed distribution prior to performing any statistical tests. Bivariate statistics descriptively characterized relationships between existential challenges and each of the sociodemographic and clinical characteristics, as well as the degree to which the three categories of existential challenges were interrelated. Finally, multivariate linear regression (for constructed meaning and cancer worry) and multivariate logistic regression (for the four grief or identity challenge items) were used to examine the unique associations of each of the sociodemographic and clinical characteristics with the existential challenges.
Results
Descriptive statistics
Table 1 shows the descriptive and bivariate statistics for the study sample. Respondents averaged 44 years old and about 7 years post-diagnosis. Just over half (55.9%) of the sample was female, most were married or partnered (64%), White (87.1%), and had a college education. Nearly half (45.7%) received both chemotherapy and radiation while the remainder had just one of the two (205 had chemotherapy with no radiation and 28 had radiation with no chemotherapy); 12.4% had undergone a stem cell transplant.
Table 1.
Descriptive and Bivariate Statistics (n=429).
| Variable | Mean (SD) or % |
Constructed Meaning†
(Mean score or r) |
Cancer Worry†
(Mean count or r) |
|
|---|---|---|---|---|
| Sociodemographic and clinical variables | ||||
| Agea | (years) | 44.2 (12.7) Range = 18-78 |
−0.01 | −0.17** |
| Gender | Male | 44.1 | 23.0 | 1.7 |
| Female | 55.9 | 22.6 | 1.8 | |
| Marital Statusb |
Married/Partnered | 64.0 | 23.1* | 1.7 |
| Unmarried | 36.0 | 22.2 | 1.7 | |
| Educationc | Less than college | 18.1 | 21.8 | 1.7 |
| Some college | 25.1 | 22.9 | 1.8 | |
| College degree | 32.2 | 22.9 | 1.7 | |
| Graduate degree | 24.6 | 23.1 | 1.7 | |
| Race/Ethnicityc | White | 87.1 | 22.8 | 1.7 |
| Non-white | 12.9 | 23.1 | 1.9 | |
| Type of lymphoma | Hodgkin | 47.3 | 22.8 | 1.7 |
| Non-Hodgkin | 52.7 | 22.7 | 1.7 | |
| Treatment | Solo treatment | 54.3 | 22.9 | 1.7 |
| Combined treatment | 45.7 | 22.6 | 1.8 | |
| Stem cell transplant | Yes | 12.4 | 21.5* | 1.9 |
| No | 87.6 | 22.9 | 1.7 | |
| Time since diagnosisd | (years) | 7.0 (7.4) | 0.07 | −0.15* |
| Existential challenges | ||||
| Constructed Meaning total scorea | (mean score) | 22.8 (4.1) Range = 9.1-32.0 |
||
| Cancer worry countc | (mean count) | 1.7 (1.0) Range = 0-3 |
−0.38** | |
| Lost sense of security | % “yes” | 51.7 | −0.45** | 0.46** |
| Lost sense of identitye | % “yes” | 25.6 | −0.36** | 0.23** |
| Grief over others’deathse | % “yes” | 70.4 | −0.10* | 0.23** |
| Guilt over others’ deathsf | % “yes” | 38.7 | −0.23** | 0.27** |
Missing for one respondent;
Missing for seven respondents;
Missing for 10 respondents;
Missing for 22 respondents ;
Missing for three respondents;
Missing for five respondents;
Higher scores meaning more constructed meaning or more cancer worry;
p<0.05;
p<0.01
Regarding existential challenges, the average score on the Constructed Meaning scale was 22.8, which is in the upper half of the range, indicating notable concerns. The average score on the cancer worry scale was 1.7, reflecting endorsement of more than one of three cancer worry items. More than half of respondents endorsed I have lost a sense of security in my future (51.7%) and I have felt grief about the death of other cancer patients (70.4%). About one-quarter endorsed I have felt that I have lost a sense of my identity, and 38.7% endorsed I have felt guilt over the death of other cancer patients.
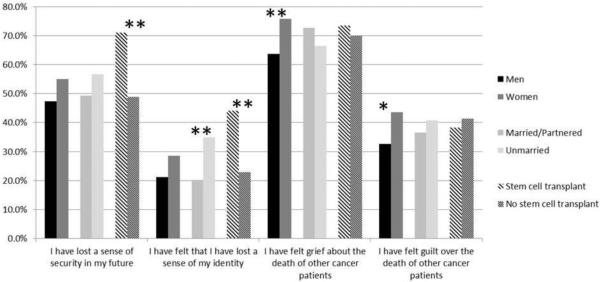
Bivariate associations between Constructed Meaning, cancer worry, and sociodemographic and clinical characteristics are also shown in Table 1. Figure 1 shows bivariate relationships between sociodemographic and clinical characteristics with issues related to security, identity, grief, and guilt. Age, gender, marital status, time since diagnosis, and receipt of a stem cell transplant were all associated with existential challenges in bivariate analyses (all p<0.05). Specifically, younger respondents reported more cancer worry and were more likely to report identity challenges, though older respondents were more likely to report grief, and survivors further from time of diagnosis reported less cancer worry, were less likely to report challenges with respect to their sense of security, but were more likely to report experiencing grief and guilt over the loss of other cancer survivors (data not shown). Married respondents had higher Constructed Meaning scores than unmarried respondents and survivors who underwent a stem cell transplant had lower Constructed Meaning scores than those who did not.
Figure 1.
The Percentage of Respondents Who Endorsed Existential Challenges by Sociodemographic and Clinical Variables.
* p<0.05; ** p<0.01
Table 1 also shows the bivariate relationships among Constructed Meaning, cancer worry, and the remaining existential challenges, which were all moderately related in expected ways: higher Constructed Meaning was associated with lower cancer worry and lower probability of endorsing security, identity, grief, or guilt challenges; higher cancer worry was associated with a higher probability of endorsing security, identity, grief, or guilt challenges; and endorsing any of security, identity, grief, or guilt challenges was associated with a higher likelihood of endorsing the others, except that identity challenges were not associated with grief.
Multivariate analyses
Table 2 shows the multivariate linear regression models; Table 3 shows the logistic models. In the multivariate linear regression model of Constructed Meaning, marital status and having had a stem cell transplant had significant unique associations with Constructed Meaning. Specifically, unmarried respondents (standardized β=−0.14; p=0.01) and respondents who had received a stem cell transplant (standardized β=−0.13; p=0.01) had lower Constructed Meaning scale scores than married respondents or those who had not undergone transplant. For cancer worry, lower worry was significantly associated with being older (standardized β=−0.13; p=0.04) and being further from time of diagnosis (standardized β=−0.16; p=0.01).
Table 2.
Multivariate Linear Regressions of Constructed Meaning and Cancer Worry.
| Constructed Meaning (Model Adjusted R = 0.23) F(11,372)=1.90; p=0.04 |
Cancer worry (Model Adjusted R = 0.25) F(11,381)=2.26; p=0.01 |
||||
|---|---|---|---|---|---|
| Standardized β | p | Standardized β | p | ||
| Age | (years) | −.04 | 0.47 | −.13 | 0.04 |
| Gender | Male | reference | 0.51 | reference | 0.45 |
| Female | −.03 | .04 | |||
| Marital Status |
Married/ Partnered |
reference | 0.01 | reference | 0.40 |
| Unmarried | −.14 | −.04 | |||
| Education | Less than college | −.15 | 0.02 | −.02 | 0.81 |
| Some college | −.05 | 0.46 | −.03 | 0.61 | |
| College degree | −.05 | 0.49 | −.05 | 0.43 | |
| Graduate degree | reference | reference | |||
| Race/Ethnicity | White | reference | 0.86 | reference | 0.11 |
| Non-white | −.01 | .08 | |||
| Type of lymphoma | Hodgkin | reference | 0.93 | reference | 1.0 |
| Non-Hodgkin | −.01 | .00 | |||
| Treatment | Solo treatment | reference | 0.64 | reference | 0.56 |
| Combined treatment | −.03 | .03 | |||
| Stem cell transplant | Yes | −.13 | 0.01 | .06 | 0.27 |
| No | reference | reference | |||
| Time since diagnosis | (years) | .06 | .31 | −.16 | 0.01 |
Table 3.
Logistic Regression Models of Security, Identity, Grief, and Guilt Challenges.
|
Odds of
reporting security concern *R2=0.07 X2=26.00; p<0.01 |
Odds of
reporting identity concern *R2=0.06 X2=24.21; p=0.01 |
||||
| OR (95% CI) | p | OR (95% CI) | p | ||
| Age | (years) | 0.99 (0.97, 1.10) | 0.25 | 0.99 (0.97, 1.01) | 0.26 |
| Gender | Male | reference | reference | ||
| Female | 1.33 (0.87, 2.04) | 0.19 | 1.29 (0.79, 2.12) | 0.32 | |
| Marital status | Married/partnered | reference | Reference | ||
| Unmarried | 1.41 (0.90, 2.20) | 0.14 | 2.01 (1.22,3.30) | <0.01 | |
| Education | Less than college | 0.83 (0.43, 1.59) | 0.57 | 0.95 (0.46, 1.96) | 0.90 |
| Some college | 0.70 (0.38, 1.29) | 0.26 | 0.72 (0.36-1.44) | 0.35 | |
| College degree | 0.55 (0.31, 0.98) | 0.04 | 0.71 (0.37, 1.36) | 0.30 | |
| Graduate degree | reference | 0.22 | reference | 0.65 | |
| Race/Ethnicity | White | reference | reference | ||
| Non-white | 1.02 (0.54, 1.98) | 0.94 | 0.63 (0.28, 1.40) | 0.26 | |
| Type of lymphoma | Hodgkin | reference | reference | ||
| Non-Hodgkin | 1.48 (0.91, 2.4) | 0.11 | 1.04 (0.60, 1.82) | 0.90 | |
| Treatment | Solo treatment | reference | reference | ||
| Combined treatment | 0.57 (0.57, 1.36) | 0.88 | 0.90 (0.55, 1.49) | 0.68 | |
| Stem cell transplant | Yes | 3.09 (1.56, 6.13) | <0.01 | 2.6 (1.36, 4.97) | <0.01 |
| No | reference | reference | |||
| Time since diagnosis | (years) | 0.75 (0.42, 1.31) | 0.31 | 0.85 (0.44, 1.62) | 0.62 |
|
Odds of
reporting security concern *R2=0.07 X2=26.00; p<0.01 |
Odds of
reporting identity concern *R2=0.06 X2=24.21; p=0.01 |
||||
| OR (95% CI) | p | OR (95% CI) | p | ||
| Age | (years) | 1.10 (0.99, 1.04) | 0.23 | 0.98 (0.96, 1.00) | 0.06 |
| Gender | Male | reference | reference | ||
| Female | 2.03 (1.28, 3.23) | <0.01 | 1.77 (1.13, 2.78) | 0.01 | |
| Marital status | Married/partnered | reference | reference | ||
| Unmarried | 0.77 (0.48, 1.24) | 0.28 | 1.04 (0.66, 1.65) | 0.87 | |
| Education | Less than college | 2.01 (0.97, 4.14) | 0.06 | 1.39 (0.72, 2.70) | 0.33 |
| Some college | 1.71 (0.89, 3.28) | 0.11 | 0.98 (0.57, 1.87) | 0.95 | |
| College degree | 1.27 (0.69, 2.32) | 0.44 | 1.03 (0.57, 1.87) | 0.93 | |
| Graduate degree | reference | 0.20 | reference | 0.70 | |
| Race/Ethnicity | White | reference | reference | ||
| Non-white | 1.03 (0.52, 2.02) | 0.94 | 0.88 (0.45, 1.72) | 0.71 | |
| Type of lymphoma | Hodgkin | reference | reference | ||
| Non-Hodgkin | 1.10 (0.66, 1.85) | 0.71 | 1.31 (0.79, 2.16) | 0.3 | |
| Treatment | Solo treatment | reference | reference | ||
| Combined treatment | 1.07 (0.67, 1.71) | 0.79 | 1.35 (0.86, 2.11) | 0.19 | |
| Stem cell transplant | Yes | 1.16 (0.59, 2.28) | 0.67 | 1.13 (0.60, 2.13) | 0.71 |
| No | reference | reference | |||
| Time since diagnosis | (years) | 1.95 (1.06, 3.6) | 0.03 | 2.26 (1.24, 4.11) | <0.01 |
Cox & Snell
In the logistic models of security, identity, grief, and guilt concerns, gender, marital status, having received a stem cell transplant, and time since diagnosis were each associated with significantly higher odds of reporting at least one of these existential challenges. Women had significantly higher odds of reporting challenges with grief (OR=2.03; p<0.01) and guilt (OR=1.77; p=0.01). Unmarried respondents had significantly higher odds of reporting identity challenges (OR=2.01; p<0.01). For clinical variables, the odds of reporting security (OR=3.09; p<0.01) and identity (OR=2.60; p<0.01) concerns were significantly higher for those who underwent stem cell transplant, and the odds of reporting experiencing grief or guilt over the death of other cancer survivors was significantly increased as time since diagnosis increased (OR=1.95 for grief; p<0.05; OR=2.26 for guilt; p<0.01).
Functional impairment
Of those respondents who had endorsed at least one worry concern (86% of sample), nearly a third (30%) indicated that their activities had been limited by this concern in the past week. Similarly, the majority of respondents (73%) endorsed at least one concern among security, identity, grief, and guilt. Of these respondents, 39% reported that their activities had been limited by this concern over the past week.
Discussion
The majority of lymphoma survivors reported having existential concerns due to their cancer diagnosis, even years later. Most survivors (86%) endorsed at least some cancer worry and 73% endorsed at least one concern related to identity, security, grief, or guilt. In terms of the real-life impact of such concerns, of those respondents who endorsed either worry or concern of identity, security, grief, or guilt, about a third (30%-39%) indicated that their current life was directly affected by that concern. These results suggest that existential concerns are not only common among lymphoma survivors, but have the potential to impact their daily lives for years afterwards.
Lymphoma survivors reported an average score on the Constructed Meaning Scale of 22.8 which suggests that lymphoma survivors experience enhanced meaning in their lives, in the range reported for other types of cancer (e.g., mean of 24 in prostate cancer survivors (Steginga et al., 2004); mean of 21 in colorectal cancer survivors (Chambers et al., 2012); mean of 19.6 in recurrent ovarian cancer survivors (Ponto et al., 2010). It is possible that survivors gained a sense of resilience and strength due to having survived cancer (Chambers et al., 2012; Diemling et al., 2007).
We identified several sociodemographic and clinical characteristics related to our six existential concerns outcome variables. Women were more likely to report concerns of grief and guilt. Being married or partnered appeared to offer some protection against loss of identity and lower meaning, perhaps because being part of a committed couple may allow the maintenance of an important aspect of a survivor’s identity (e.g., that of spouse or partner) after diagnosis. Further, being part of a dyad may buffer against stress in general (Geise-Davis et al, 2012).
In terms of treatment, respondents receiving stem cell transplantation reported lower levels of meaning and were more likely to endorse both security and identity concerns; this is in line with other findings of existential concerns in stem cell transplant recipients (Rusiewicz et al., 2008; Somerfield et al., 1996). Stem cell transplantation is one of the most serious cancer treatments; complications (e.g., infections, cardiovascular disease) can be life threatening and disruptive, and can occur long after transplantation (Gunasekaran et al., 2012). It is therefore understandable that respondents receiving transplantation would struggle with existential concerns of security and identity as it is likely more difficult to preserve these due to this protracted experience. We found that older respondents worried less about cancer, similar to other cancer populations (Myers et al., 2013; Phillips et al., 2013). It may be that for older patients, cancer diagnosis is more developmentally normative than for younger persons (Zebrack and Butler, 2012). Finally, those who were further out from diagnosis reported less worry, perhaps due to knowledge about improved survival odds, which come with surviving cancer after the first few years. However, those further out from diagnosis also were more likely to report feeling grief and guilt over the deaths of other survivors. This may reflect simply that more time since diagnosis gives more time to lose people, or could bring up a lingering question in lymphoma survivors of “why am I still here?”
The interpretation of these results is limited by several factors, including the cross-sectional nature of the survey which precludes ascertaining temporal relationships. We cannot determine the impact of disease stage on our outcomes as stage was not assessed. Further, some of our outcome variables were single items, which introduces possible measurement concerns; multi-item measures were not available in the survey. Finally, given the voluntary, online nature of the 2010 LIVESTRONG survey, the lymphoma survivors completing this survey may not be necessarily representative of lymphoma survivors in general.
In conclusion, lymphoma survivors experience existential challenges which are impactful even years after diagnosis. Survivor characteristics most related to existential concerns (for example, being female and younger) could allow supportive services provided by pastoral care or mental health professionals to be targeted to these subgroups. It is important that health care providers become aware of these concerns, even in long-term survivors, so that they may be addressed (Leung and Esplen, 2010). Although often overlooked in psychological interventions for cancer patients (Lindemalm et al., 2012), some evidence suggests that addressing existential concerns in cancer populations in general (Breitbart et al., 2012), and specifically in lymphoma survivor populations, would likely contribute to improved well-being and quality of life (Henoch and Danielson, 2009).
Acknowledgments
This research was supported by funding from the LIVESTRONG Foundation and Grants K23CA149082 and P30 CA047904 from the National Cancer Institute.
References
- American Cancer Society Cancer facts & figures. 2014 Available at www.cancer.org (accessed 30 October 2014)
- Baxi SS, Matasar MJ. State-of-the-art issues in Hodgkin’s lymphoma survivorship. Current Oncology Reports. 2010;12:366–373. doi: 10.1007/s11912-010-0123-2. [DOI] [PubMed] [Google Scholar]
- Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. Journal of Clinical Oncology. 2012;30:1304–1309. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers S, Baade P, Meng X, et al. Survivor identity after colorectal cancer: Antecedents, prevalence and outcomes. Psycho-Oncology. 2012;21:962–969. doi: 10.1002/pon.1991. [DOI] [PubMed] [Google Scholar]
- Diemling GT, Bowman KF, Wagner LJ. Cancer survivorship and identity among long-term survivors. Cancer Investigations. 2007;25:758–765. doi: 10.1080/07357900600896323. [DOI] [PubMed] [Google Scholar]
- Fife BL. The measurement of meaning in illness. Social Science & Medicine. 1995;40:1021–1028. doi: 10.1016/0277-9536(94)00174-r. [DOI] [PubMed] [Google Scholar]
- Geise-Davis J, Waller A, Carlson LE, et al. Screening for distress, the 6th vital sign: Common problems in cancer outpatients over one year in usual care: associations with marital status, sex, and age. BMC Cancer. 2012;12:441. doi: 10.1186/1471-2407-12-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JR, Naglieri JA. Handbook of Psychology, Vol 10: Assessment Psychology. Wiley; Hoboken, NJ: 2003. 2003. [Google Scholar]
- Gunasekaran U, Agarwal N, Jagasia MH, et al. Endocrine complications in long-term survivors after allogeneic stem cell transplant. Seminars in Hematology. 2012;49:66–72. doi: 10.1053/j.seminhematol.2011.10.010. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, SSanderman R, Bolks HN, et al. Distress in couples coping with cancer: a meta-analysis and cirtical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Henoch I, Danielson E. Existential concerns among patients with cancer and interventions to meet them: an integrative literature review. Psycho-oncology. 2009;18:225–236. doi: 10.1002/pon.1424. [DOI] [PubMed] [Google Scholar]
- Jensen RE, Arora NK, Bellizzi KM, et al. Health-related quality of life among survivors of aggressive non-hodgkin lymphoma. Cancer. 2013:672–680. doi: 10.1002/cncr.27781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jim HS, Jacobsen PB. Posttraumatic stress and posttraumatic growth in cancer survivorship: A review. The Cancer Journal. 2008;14:414–419. doi: 10.1097/PPO.0b013e31818d8963. [DOI] [PubMed] [Google Scholar]
- Lee V. The existential plight of cancer: meaning making as a concrete approach to the intangible search for meaning. Support Care Cancer. 2008;16:779–785. doi: 10.1007/s00520-007-0396-7. [DOI] [PubMed] [Google Scholar]
- Lee V, Loiselle CB. The salience of existential concerns across the cancer control continuum. Palliative & Support Care. 2012;10:12–133. doi: 10.1017/S1478951511000745. [DOI] [PubMed] [Google Scholar]
- Leung D, Esplen MJ. Alleviating existential distress of cancer patients: Can relational ethics guide clinicians? European Journal of Cancer Care. 2010;19:30–38. doi: 10.1111/j.1365-2354.2008.00969.x. [DOI] [PubMed] [Google Scholar]
- Lindemalm C, Granstam-Bjorneklett H, Bergkvist L, et al. Existential aspects are neglected in the evaluation of support-intervention in breast cancer patients. Acta Oncologica. 2012:807–809. doi: 10.3109/0284186X.2012.681699. [DOI] [PubMed] [Google Scholar]
- Little M, Paul K, Jordens CFC, et al. Survivorship and discourses of identity. Psycho-Oncology. 2002;11:170–178. doi: 10.1002/pon.549. [DOI] [PubMed] [Google Scholar]
- Mols F, Aaronson NK, Vingerhoets AJJM, et al. Quality of life among longer-term non-hodgkin lymphoma survivors. Cancer. 2007;109:1659–1667. doi: 10.1002/cncr.22581. [DOI] [PubMed] [Google Scholar]
- Myers SB, Manne SL, Kissane DW, et al. Social-cognitive processes associated with fear of recurrence among women newly diagnosed with gynecological cancers. Gynecologic Oncology. 2013;128:120–127. doi: 10.1016/j.ygyno.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neimeyer RA, Herrero O, Botella L. Chaos to coherence: Psychotherapeutic integration of traumatic loss. Journal of Constructivist Psychology. 2006;19:127–145. [Google Scholar]
- Park C. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136:257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Pascal J, Endacott R. Ethical and existential challenges associated with a cancer diagnosis. Journal of Medical Ethics. 2010;36:279–283. doi: 10.1136/jme.2009.034942. [DOI] [PubMed] [Google Scholar]
- Phillips KM, McGinty HL, Gonzalez BD, et al. Factors associated with breast cancer worry 3 years after completion of adjuvant treatment. Psycho-Oncology. 2013;22:936–939. doi: 10.1002/pon.3066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponto JA, Ellington L, Mellon S, et al. Predictors of adjustment and growth in women with recurrent ovarian cancer. Oncology Nursing Forum. 2010;37:357–364. doi: 10.1188/10.ONF.357-364. [DOI] [PubMed] [Google Scholar]
- Rechis R, Reynolds KA, Beckjord EB, et al. “I learned to live with it” is not good enough: Challenges reported by post-treatment cancer survivors in the LIVESTRONG Surveys. LIVESTRONG; Austin, TX: 2011. [Google Scholar]
- Roper K, McDermott K, Cooley ME, et al. Health-related quality of life in adults with hodkin’s disease. Cancer Nursing. 2009;32:E1–E17. doi: 10.1097/NCC.0b013e3181aa4a33. [DOI] [PubMed] [Google Scholar]
- Rusiewicz A, DuHamel KN, Burkhalter J, et al. Psychological distress in long-term survivors of hematopoietic stem cell transplantation. Psycho-Oncology. 2008;17:329–337. doi: 10.1002/pon.1221. [DOI] [PubMed] [Google Scholar]
- Schmidt SD, Blank TO, Bellizzi KM, et al. The relationship of coping strategies, social support, and attachment style with posttraumatic growth in cancer survivors. Journal of Health Psychology. 2011;17:1033–1040. doi: 10.1177/1359105311429203. [DOI] [PubMed] [Google Scholar]
- Smith SK, Crespi CM, Petersen L, et al. The impact of cancer and quality of life for post-treatment non-Hodgkin lymphoma survivors. Psycho-oncology. 2010;19:1259–1267. doi: 10.1002/pon.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerfield MR, Curbow B, Wingard JR, et al. Coping with the physical and psychosocial sequelae of bone marrow transplantation among long-term survivors. Journal of Behavioral Medicine. 1996;19:163–184. doi: 10.1007/BF01857605. [DOI] [PubMed] [Google Scholar]
- Steginga S, Occhipinti S, Gardiner RA, et al. Prospective study of men’s psychological and decision-related adjustment after treatment for localized prostate cancer. Urology. 2004;63:751–756. doi: 10.1016/j.urology.2003.11.017. [DOI] [PubMed] [Google Scholar]
- Vehling S, Lehmann C, Oechsle K, et al. Is advanced cancer associated with demoralization and lower global meaning? The role of tumor stage and physical problems in explaining existential distress in cancer patients. Psycho-Oncology. 2012;21:54–63. doi: 10.1002/pon.1866. [DOI] [PubMed] [Google Scholar]
- Willig C. “Unlike a rock, a tree, a horse or an angel…” Reflections on the struggle for meaning through writing during the process of cancer diagnosis. Journal of Health Psychology. 2009;14:181–189. doi: 10.1177/1359105308100202. [DOI] [PubMed] [Google Scholar]
- Zebrack BJ. Cancer survivor identity and quality of life. Cancer Practice. 2000;8:238–242. doi: 10.1046/j.1523-5394.2000.85004.x. [DOI] [PubMed] [Google Scholar]
- Zebrack B, Butler M. Context of understanding psychosocial outcomes and behavior among adolescents and young adults with cancer. Journal of National Comprehensive Cancer Network. 2012;10:1151–1156. doi: 10.6004/jnccn.2012.0118. [DOI] [PubMed] [Google Scholar]