Abstract
Background
In the general geriatric population, programs linking geriatric evaluation with interventions are effective for improving functional status and survival of the patients. Whether or not these interventions improve health related quality of life (HRQoL) or overall survival (OS) in older patients with cancer is not yet clear. Indeed, randomized data on the effect of such interventions on survival and HRQoL are rare and conflicting. We describe the rationale and design of a phase III multicenter trial aimed at assessing the efficacy of geriatric intervention in the management of elderly patients with cancer.
Methods/design
Approximately 1200 patients, 70 years and older, considered in need of a geriatric intervention based on the G8 screening tool will be randomized into two intervention arms. The ‘Usual-care’ arm involves standard oncological care based on pre-defined oncological protocols. In addition to the standard oncological care, the ‘Case-management’ arm involves a multidimensional geriatric assessment and interventions tailored for the patient. Efficacy will be assessed using a co-primary endpoint encompassing OS and HRQoL.
Discussion
This trial has been designed to assess whether focused geriatric case management can either improve OS or HRQoL in elderly cancer patients considered in need of geriatric assessment.
Trial registration
Clinicaltrials.gov ID: NCT02704832.
Keywords: Aged, Elderly, Cancer, Geriatric intervention, Case-management, Chemotherapy, Clinical trial
Background
As the worldwide population ages and progress in cancer treatment increases survival, improving the management of older patients with cancer has become a major public health issue. Significant progress has been made in recent years, and geriatric assessment tools with prognostic value to identify specific problems in the elderly cancer population have been developed and validated [1–4]. However, this approach takes time and skills to administer and interpret, and only a few teams in France can perform full geriatric assessment in routine practice for all elderly cancer patients. We have developed [5] and validated the G8 screening tool [3], a short, easy-to-administer screening tool to identify patients in need of comprehensive geriatric assessment (CGA) and specialized interventions. However, the impact of further geriatric interventions on elderly cancer patient outcomes has not yet been investigated.
A number of randomized trials on geriatric interventions have shown benefit in various aspects for older cancer patients such as physical activity levels or health related quality of life (HRQoL) (Table 1). Goodwin et al. reported that nurse case management had a positive impact on the management of elderly patients with breast cancer [6]. Morey et al., in a 12-month home-based study, reported the impact of physical activity in overweight, long-term cancer survivors older than 65 years of age. They reported gains in function scores, basic lower extremity function, dietary habits and an improvement in the overall HRQoL [7]. In another study, an improvement in lean mass, muscle strength, walk time and HRQoL was observed with a resistance and aerobic exercise program for 57 prostate cancer patients with a mean age of 70 years [8]. Gains in practice of two or more goal behaviors, exercise minutes per week, total fat, saturated fat, and body mass index (BMI) were observed for 443 patients with newly diagnosed loco-regional breast or prostate cancer after a 10-month program of tailored mailed print materials [9]. Geriatric intervention reduced the pain in frail elderly patients who underwent elective surgery for a solid tumor but did not have any significant effect on delirium, complications, length of stay, care dependency and HRQoL [10].
Table 1.
Literature review of geriatric intervention programs
| First author | Study design | N | Population | Mean age | Intervention | Primary end-point | Results |
|---|---|---|---|---|---|---|---|
| Bourdel-Marchasson [13] | Multicenter RCT* | 336 | Patients with solid tumor treated by chemotherapy at risk of malnutrition (17 ≤ MNA ≤ 23.5). | 78.0y | 3–6 months diet counselling intervention | 1-year mortality | - Early dietary counselling was efficient in increasing intake but had no beneficial effect on mortality. |
| Hempenius [10] | Multicenter RCT | 260 | Frail elderly patients undergoing elective surgery for a solid tumor | ≈77.5y | Geriatric liaison intervention | Postoperative delirium | - Intervention for frail elderly cancer patients receiving surgery to prevent post-operative delirium was not effective. |
| Demark-Wahnefried [34] | Multicenter international RCT (RENEW study) | 641 | Overweight long-term survivors (≥5 years) of colorectal, breast and prostate cancer | ≈73y | 12-month diet and exercise intervention via telephone counseling and print materials | Change in functional status (baseline/12-month and 24-month) Diet quality, BMI and physical activity |
- Significant change in functional status between intervention group and control group (p < 0.01): amelioration of functional decline in intervention group. Significant change in diet quality, physical activity and BMI (p < 0.01). |
| Morey [7] | Change in functional status (baseline/12 m) using the Medical Outcomes Study SF36 questionnaire, health-related QoL | - Significant change in physical function (p = 0.03) and QoL (p = 0.007) between groups. | |||||
| Lapid [35] | Subset geriatric analysis from stratified, two-group RCT | 33 | New advanced cancer diagnosis (5-year OS: 0–50 %) planned to receive radiotherapy | ≈72y | 4-week multidisciplinary QoL intervention | QoL measured with Spitzer uniscale and linear analogue self-assessment (LASA) at baseline and weeks 4, 8, and 27 | - Significant improvement in QoL (p < 0.05) at baseline, maintained at 4 and 8 weeks. |
| Rao [14] | Subset analysis from RCT [36] | 99 | Frail elderly cancer patients hospitalized on a medical or surgical ward (≥2 days) | ≈74y | Geriatric assessment and patient management by a geriatric attending physician and a social worker | 12-month survival and health-related QoL (after randomization), ADL, physical performance, health service utilization, and costs | - No significant effect on survival or QoL parameters. Positive effects of geriatric inpatient care on mental health and bodily pain (p < 0.05). Days of hospitalization and cost similar. |
| Goodwin [6] | Multicenter RCT | 335 | Older women (≥65y) newly (<2 months) diagnosed with breast cancer | ≈72y | 12-month nurse case management | Type and use of cancer-specific therapies received in the first 6 months after diagnosis. Patient satisfaction and arm function |
- More appropriate management for women receiving nurse case management (Breast-conserving surgery, adjuvant radiation, radiation therapy, axillary dissection and breast reconstruction surgery). Better arm function and higher satisfaction in intervention group. |
| McCorkle [15] | Single centerRCT | 375 | Old patients (≥60y) newly diagnosed with solid cancer | 60–92 | 4-week home-based case management by nurse | Length of survival | - Longer survival in intervention group than in usual care group (p = 0.001). Survival advantage for intervention group in late stage patients. |
| Galvao [8] | Two-arm single center RCT | 57 | Prostate cancer patient without bone metastases treated by AST (≥2 months) | ≈70y | 12-week progressive resistance and aerobic training (2/week) by an exercise physiologist | Muscle mass, strength, physical function, QoL | - Significant change in total body lean mass, muscle strength and endurance (p < 0.05). Change in QoL for general health (p = 0.022), vitality (p = 0.019) and physical health composite score (p = 0.02). |
*QoL quality of Life, RCT randomized controlled trial
Geriatric intervention has also been shown to increase overall survival (OS) in the general elderly population in randomized controlled trials (RCTs) [11, 12]. However, only few RCTs have investigated the impact specifically for elderly cancer patients, with conflicting results. Bourdel-Marchasson et al. [13] found no impact on 1-year mortality after a nutritional intervention, and in a sub-analysis of a larger trial, Rao et al. [14] found no difference in 1-year survival after geriatric case-management for elderly cancer patients. An improvement in survival was reported in an RCT involving case-management in the form of a one-month nurse intervention for post-surgical elderly cancer patients, including 375 patients older than 60 years, but this benefit was restricted to the sub-population of patients with advanced disease [15].
Overall, results from various studies suggest that geriatric interventions can potentially improve OS in elderly cancer patients. Although several attempts are being made to identify more patients at risk that require geriatric interventions, any OS or HRQoL benefits following these interventions has not yet been sufficiently demonstrated.
Our objective is to conduct a two-arm phase III trial to assess the efficacy of geriatric intervention in the management of elderly patients with cancer (targeted oncology domains: breast, colorectal, lung, prostate, bladder, ovary, lymphoma). The trial will be restricted to patients with an abnormal G8 screening tool score that are considered in need of a geriatric intervention. This trial protocol was developed in collaboration with two national research platforms (Cancer and Elderly Platform and Cancer and Quality of Life Platform). We present here the key elements of the trial: objectives, study design, target population, description of the interventions, evaluation criteria and statistical methods.
Methods/Design
Objectives
Primary objective
The primary objective of the trial is to compare the efficacy of two treatment strategies “usual care” and “Case-management intervention” in elderly cancer patients considered in need of a geriatric assessment (G8 score ≤ 14). Treatment strategies are defined as follows:
“Usual care”: Patients are treated according to ongoing standards in oncology.
“Case-management intervention”: Patients are treated according to ongoing standards in oncology as in the “Usual care” arm. In addition, patients receive geriatric assessments and interventions coordinated by a geriatrician and a trained nurse, and tailored for the patient.
The intervention content for each arm has been precisely defined by a panel of experts in geriatric oncology. Efficacy will be assessed using a co-primary endpoint encompassing OS and three targeted HRQoL dimensions (global health status, physical functioning and emotional functioning as measured using the European Organization for Research and Treatment of Cancer, EORTC, QLQ-C 30 questionnaire [16]). Specifically, efficacy of the “Case- management intervention” will be considered superior to that of “Usual care” if, at one year, compared to usual care, improvement is observed for OS or at least one of the targeted HRQoL dimensions. We provide additional details of the primary endpoint in evaluation criteria and sample size calculation sections.
Secondary objectives
Secondary objectives are three-fold. First, in the population of elderly cancer patients considered in need of a geriatric assessment (G8 score ≤ 14), we will compare the two treatment strategies in terms of additional endpoints: 6-month objective response, 1- and 3-year progression-free-survival (PFS) and OS, HRQoL dimensions other than those targeted for the primary endpoint, grade 3–4 toxicities, duration and number of hospitalizations, place of residence (home versus nursing home or hospital).
Second, we will focus on the population recruited in the intervention arm. Our objective is to provide a description of geriatric parameters (evolution over one year, as well as descriptive data at baseline, 6 and 12 months): functional status, nutritional status, depression status, physical capacities, number and type of prescribed geriatric interventions.
Third, while our main focus is on elderly cancer patients considered in need of a geriatric assessment (G8 score ≤ 14), we also intend to provide a brief description of patients with a normal G8-score. Vital status, place of residence and disease progression at one year will be described.
Overall study design
The efficacy of the treatment strategies “Usual care” and “Case-management intervention” will be assessed using a two-arm randomized multicenter trial, conducted in elderly cancer patients considered in need of a geriatric assessment (G8 score ≤ 14).
As additional objectives involve describing elderly cancer patients with a normal G8-score, a specific cohort will be built in parallel to the randomized trial. Patients initially screened for inclusion in the randomized trial but who will present with a G8 score ≤ 14 will be included in this parallel prospective cohort.
All elderly cancer patients treated at participating centers will first be screened with the G8 instrument (Appendix A). If the G8 score is altered (G8 score ≤ 14) then patients will be included in the main trial and randomized between “Usual care” and “Case-management intervention” (Fig. 1). For each arm, patients will be treated according to protocols specifically defined for this trial (See section “Description of the interventions”). If the resulting score is normal (G8 > 14) then patients will be included in the parallel cohort and treated according to the institution’s standard management process.
Fig. 1.
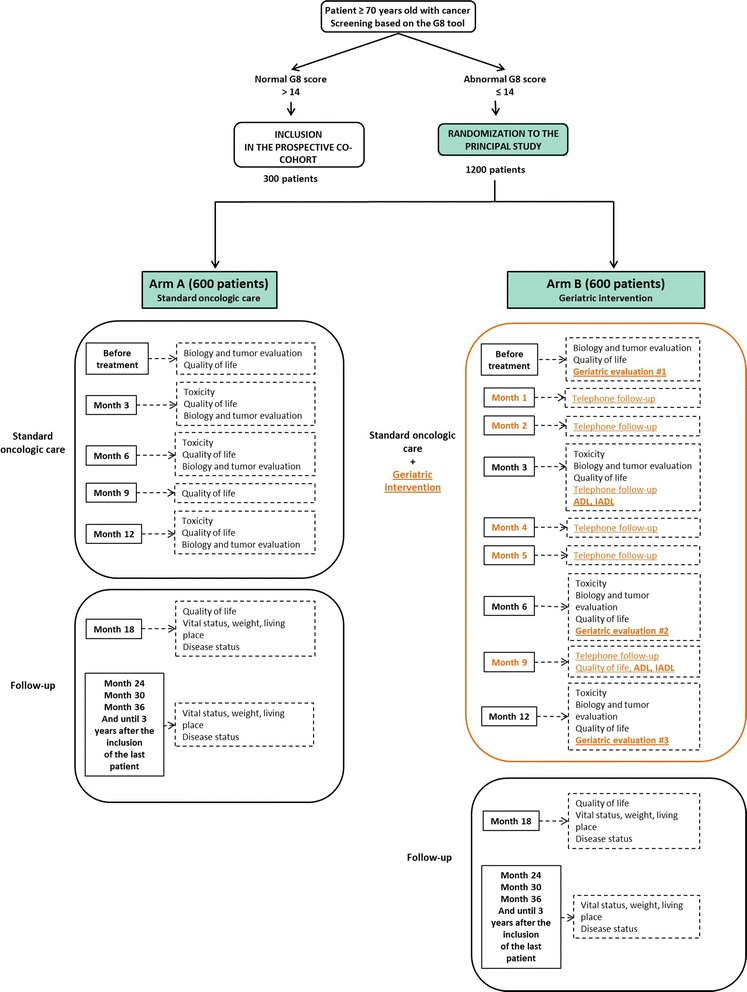
ᅟ
This study will be initially proposed to the 28 Regional Coordination Units for Geriatric Oncology accredited to the French National Cancer Institute across France, including Comprehensive Cancer Centers, teaching hospitals, public hospitals and private practices.
Data will be collected on an electronic case report form and directly input via the Internet. Data will be handled by online trial management software on the Internet; it will be transferred and monitored remotely in real-time. Similarly, randomization will proceed through internet-based software allowing rapid randomization at any time.
Eligibility criteria
This study will include patients 70 years and older. In addition, patients must meet the following criteria: performance status 0 to 3 (WHO), candidate to 1st line medical treatment (excluding best supportive care) of breast, colon, rectal, lung, prostate, bladder, or ovarian cancer and lymphomas (indolent and aggressive); excluding exclusive hormonotherapy (except prostate cancer); or, second line medical treatment (excluding Best Supportive Care) of breast, colon, rectal, prostate cancer, ovary and indolent lymphoma.
Exclusion criteria are life expectancy under 6 months, presence of any psychological, familial, sociological or geographical condition potentially hampering compliance with the study protocol and follow-up schedule, participation at the same time in another study in which investigational drugs are used, and patients who have already received two lines of treatment or for whom hormonal treatment (except for abiraterone acetate and enzalutamide in prostate cancer) or best supportive care is indicated.
Description of the interventions
All patients included in the randomized trial will receive cancer care according to ongoing standards in oncology. The content of this intervention has been precisely defined in a cancer care protocol by a panel of experts in geriatric oncology, and depending on the disease and stage. For patients specifically randomized in the “Case-management intervention”, intervention will, in addition, involve multidimensional geriatric assessments and case-management geriatric interventions tailored for the patient. Similarly, this specific geriatric intervention has been precisely defined in a geriatric care protocol by a panel of experts in geriatric oncology. We first describe the development process for the cancer care protocol and the geriatric care protocol followed by details of the content of each protocol.
Development of the standard cancer care and geriatric intervention plans
The objective of this preliminary phase is to propose protocols for both cancer care and geriatric care for patients included in the randomized trial in order to ensure homogeneous oncological care (across treatment arms and between investigational sites) as well as homogeneous interventions in geriatrics (within the arm “Case-management intervention” and between investigational sites). Firstly, although the trial is aimed at assessing the efficacy of the geriatric intervention, it is important to acknowledge that for same disease, several cancer treatment options can be proposed, and dose adjustments are expected. By providing a cancer care protocol, clinicians will have a specific list of cancer treatment options for which they will be able to select an option. Secondly, it is important to ensure that patients who will be randomized in the geriatric intervention arm will be followed-up and treated according to a standardized procedures (use of the same questionnaires, same decision rules to propose specific interventions, etc.), justifying the development of a geriatric care protocol.
To develop and validate the final version of both the cancer care and the geriatric care protocols, two independent committees were set up for each protocol: a writing committee and a peer-review committee. For the cancer care protocol, the writing committee led by an oncologist (CT) consisted of seven additional experts in each targeted oncology domain (breast, colo-rectal, lung, prostate, bladder, lymphoma, or ovarian cancer), and the validation committee included four oncologists and one geriatrician. For the geriatric care protocol, the writing committee consisted of two geriatricians (MR and OSJ) and one nurse qualified in geriatric oncology (MDZ), and the validation committee included one oncologist and four geriatricians. The complete list of experts constituting the committees is provided in Appendix B.
Once the protocols were drafted by the writing committee, they were sent to the peer-review committee for assessment and comments with a standardized questionnaire consisting of seven questions on the clarity, appropriateness and applicability of the proposed protocols. Members provided a formal and advisory opinion on content and form of the initial version of the guidelines. Minor modifications to the protocols were incorporated following the review. Final documents were then redistributed to the writing committees for validation. This review process was an essential quality assurance step and the final document was circulated to all participating investigators of the trial and will serve as a reference document.
Description of the intervention for the arm ‘Usual care’
Patients will be treated according to the cancer care protocol, which provides, for each cancer site, a list of treatment options as well as guidelines for dose modifications and adverse event management. The complete cancer care protocol is available upon request.
Patients will be followed-up by the oncologist for three years after randomization. Baseline assessment includes clinical examination, laboratory tests (hematology, biochemistry and/or creatinine clearance), disease history and treatments, tumor assessment, and HRQoL assessment (QLQ-C30 and ELD-14). Quarterly visits by the oncologist during the first year will include a clinical examination, laboratory tests, tumor assessment, and HRQoL assessment (QLQ-C30 and ELD-14 questionnaires). Patients will then be seen every semester during the second and third years during which data on disease progression, HRQoL and vital status will be collected.
Description of the intervention for the arm “Case-management intervention”
Patients will be treated according to the oncological standards, as defined in the cancer care protocol. Patients’ follow-up with their oncologist will be identical to that of patients in the ‘Usual care’ arm. In addition, intervention will also involve case-management geriatric interventions tailored for the patient. The geriatric care protocol provides a full description of the case-management process which includes CGAs, telephone follow-ups by the nurse and patient file reviews by the geriatrician and the nurse.
The patient will be seen by the geriatrician and the nurse for CGA at baseline (after randomization and before treatment initiation), as well as 6 and 12 months after randomization. The CGA will include the following: questionnaires completed with the nurse (Activities of Daily Living (ADL) [17], Instrumental ADL (IADL), Mini Mental State Examination (MMSE) [18], Mini Nutritional Assessment (MNA) [19], Geriatric Depression Scale (GDS-15) [20], EORTC QLQ-C 30 [16] and the Elderly Cancer Patients version (EORTC QLQ- ELD14) [21]); social evaluation including mode of living, professional help, social situation; geriatric clinical consultation including Timed Up and Go (TUG) [22], Short Performance Physical battery (SPPB [23]), weight loss, subjective health, falls in last 12 months, co-morbidities, other medical treatment, pain (numerical scale) and sleep patterns; geriatric patient management plan defined by nurse and geriatrician. The geriatric management plan establishing any necessary interventions will be defined by the nurse and the geriatrician across eleven intervention areas according to the predefined rules in the geriatric care protocol. Table 2 presents a summary of these interventions for the eleven intervention areas: modification of therapy, balancing chronic diseases, pain treatment, nutritional intervention, physical activity, physiotherapy, psychological support, prevention of further cognitive impairment, treatment of sleeping disorders, assistance, and home help. For illustration, with regards to nutritional intervention, weight loss over the last three and six months should be assessed and the MNA questionnaire should be completed. The patient will be considered at risk of malnutrition in case of MNA score between 17 and 23.5 and in such case, advice on increasing dietary uptake (use of food pyramid adapted for elderly patients) should be provided as presented in the geriatric protocol. On the other hand, in case of an MNA score below 17, weight loss greater than 5% over the last three months or 10% over the last six months, then the patient will be considered malnourished, and should be referred to a dietician.
Table 2.
Proposed geriatric interventions defined in protocol according to the eleven areas and screening tools used
| Area | Indication | Intervention |
|---|---|---|
| Modification of therapy | Polypharmacy | • Re-evaluate treatment indications (with general practitioner), optimize treatment according to elderly patient protocols. |
| • Use the STOPP-START* tool as a reference [37, 38]. | ||
| Balancing chronic diseases | CIRS-G* Grade ≥ 3, | • Adaptation of therapy. |
| arterial hypertension, diabetes, arthritis, or sensory problems | • Other non-drug interventions such as dietary advice, devices. | |
| • Referral to specialist doctor. | ||
| Pain treatment | Pain >1 on numeric scale | • Drug: WHO levels 1–3 antalgic treatment |
| • Non-drug: physiotherapy, devices | ||
| Nutritional intervention | Malnutrition (MNA* ≤ 17) | • Referral to dietician (nutritional supplements, artificial nutrition, etc.) |
| Weight loss ≥5 % over 3 m, or ≥10 % over 6 m | ||
| At risk of malnutrition - 17 < MNA ≤ 23.5 | • Advice on increasing dietary uptake (use of food pyramid adapted for elderly patients) | |
| Physical activity | Sedentary or at risk of falls | • Recommend daily walk, walking upstairs, carrying groceries |
| Physiotherapy | Difficulty with walking and balance (TUG*, and SPPB*). Fall in the last 12 m, weight loss, muscle loss | • Prescribe physiotherapy for muscular reinforcement Work on balance, and getting up from lying down position |
| • Prescribe walking aids | ||
| Psychological support | GDS* ≥ 6 | • Consultation with psychologist or psychiatrist |
| Apparent anxiety (clinical assessment) | ||
| Antecedent of depression | ||
| Prevention of further cognitive impairment | MMSE* < 24 | • Behavioral monitoring during chemotherapy |
| • Prevention of confusion [39] | ||
| Treatment for sleeping disorders | Positive screening score on adapted Epworth scale [40] | • Introduction, modification or discontinuation of treatment by hypnosis according to STOPP and START recommendations [37, 38] |
| Assistance | Social fragility identified (absence of social support) | • Ask patient directly if help is needed |
| • Refer to a social worker | ||
| Home help | Difficulties performing daily tasks such as grooming, housework | • Prescribe support within the home (nursing, physiotherapy, housecleaner, etc.) |
*STOPP-START Screening Tool of Older persons’ prescriptions, CIRS-G Cumulative Illness Rating Scale for Geriatrics, MNA Mini Nutritional Assessment, TUG Timed Up and Go, SPPB Short Performance Physical battery, GDS Geriatric Depression Scale, MMSE Mini mental state examination
Telephone follow-ups by the nurse will take place on a monthly basis for the first semester, then every three months up to one year, or after any event, such as hospitalization, or change of residence to nursing home. The following information should be recorded: clinical status of the patient including factors assessed at the 1-month review, any toxicity to treatment, social assistance in place, and coordination of future consultations.
Patient file reviews will take place after telephone follow-ups and will involve the geriatrician, the nurse and the oncologist in order to review how the geriatric interventions in place are progressing, and assess the need for further interventions according to the predefined rules (Table 2).
To standardize care in the “Case-Management arm”, a two-day training for nurses will be organized. Two nurses per investigating center will participate in the training which will be mandatory before the center can accrue. During this training session, nurses will be trained to perform the telephone follow-ups with patients.
Description of the intervention for patients included in the parallel cohort
Patients with a normal G8 score will be included in the parallel cohort and treated according to the institution’s standard management process.
Evaluation criteria
Although OS is a usual endpoint to assess treatment efficacy in RCTs, it may not be sufficient to assess the treatment benefit in an elderly population. The effect on HRQoL should also be considered, since it may be as important as (and sometimes more than) duration of life for this population [24, 25]. Efficacy will be assessed using a co-primary endpoint encompassing OS and three targeted HRQoL dimensions including global health status, physical functioning and emotional functioning as measured using the EORTC QLQ-C 30 questionnaire [16]. Specifically, efficacy of the “case-management intervention” will be considered superior to that of “usual care” at one year, if there is a significant clinical improvement in OS without a significant deterioration in at least one of the targeted HRQoL dimensions, or if there is a significant clinical improvement in at least one of the targeted HRQoL dimension without a significant difference in OS.
OS is defined as the delay between the date of randomization and the date of death. If the absolute difference in OS at one year is at least 10% greater, then we will consider it as a significant improvement in the OS. For HRQoL, the three targeted dimensions will be assessed using the EORTC QLQ-C 30 questionnaire [16]. Dimensions will be scored according to the EORTC manual [26]. Each dimension will be scored ranging from 0 to 100 and a difference of 10 points or greater will be considered to be clinically significant [27]. If there is a major improvement in at least one of the three scales, without deterioration of the other two, then we will consider as a significant improvement in HRQoL. Secondary endpoints include PFS defined as the delay between the date of randomization and the date of progression or death whichever occurs first. Progression, as well as objective response, will be defined as per the RECIST criteria for solid tumors [28] or the Cheson criteria for lymphomas [29]. HRQoL dimensions other than those targeted for the primary efficacy endpoints will similarly be assessed based on the EORTC scoring manual, and the EORTC ELD-14 module will be assessed following published guidelines [30]. For each of the HRQoL dimensions, time until definitive deterioration (TUDD) will be investigated and defined based on a recent publication [31]. Toxicities will be graded according to the NCI-CTC v4.3 classification. For geriatric questionnaires (G8, ADL, IADL, MNA, MMSE, GDS-15, CIRS-G, TUG), cut-off scores used to define abnormal scores are those reported in the corresponding literature and summarized in Soubeyran et al. [3].
Statistical methods
Randomization
For the phase III trial, randomization will be performed on an individual basis based on a 1:1 allocation ratio. Randomization will be stratified by investigational site, treatment line (first or second), and type of cancer (breast, colon, rectal or prostate cancer versus bladder, ovarian, or lung cancer or lymphoma). Because of the number of strata foreseen, randomization by minimization will be implemented [32].
Sample size
Sample size was estimated for the randomized trial. For the null hypothesis we assumed no difference in OS and no difference in the three targeted HRQoL dimensions between the two intervention arms. Alternative hypotheses were two-fold: improvement in OS or improvement in HRQoL. The 5% two-sided type-1 error rate was therefore split between the two alternative hypotheses with 2% for OS and 1% for each of the three HRQoL dimensions. Sample size improvement for testing improvement in OS assumed the following hypotheses: 2% (two-sided) type-1 error rate, 85% power, anticipated 1-year 50% OS rate in the ‘usual care’ group [13], 60% expected 1-year 60% OS rate in the “Case-management” arm (ie anticipated hazard ratio, HR = 0.74). These hypotheses led to an estimated sample size of 1096 subjects (548 per group; 486 events) needed to detect a difference in OS (log-rank test). Sample size for testing improvement in HRQoL was based on a 3% (two-sided) type-1 error. If the intervention is effective, we expect that it will allow us to detect, at one year, a mean difference of 10 points or more for at least one of the three targeted HRQoL scores (common standard deviation of 20 points). Each of the three scales will be independently tested. Five hundred and forty eight subjects per group (as needed for OS comparison) will provide sufficient power (>90%) for independently testing the three HRQoL scales at 1% (2-group t-tests of equal means – common variance).
To anticipate for non-assessable subjects (10%), 1200 patients need to be randomized (ie with G8 score ≤ 14). Based on previous research [5] about 80% of the patients are expected to have positive G8, thus 1500 patients need to be screened for inclusion in the randomized trial.
Since 20% are expected to have normal G8 score, about 300 patients will be included in the parallel cohort. Following our previous experience with the ONCODAGE validation study [3] which included 1668 patients over 18 months, we expect that 800 patients will be screened each year, leading to an expected inclusion period of 1.5 to 2 years. To reach all endpoints, three years of follow-up are required, giving total study duration of 5 years.
Statistical analyses
For the randomized trial, different analysis sets will be defined including the intent-to-treat (ITT) population (all randomized patients included and analyzed according to the allocated intervention), modified ITT population (mITT: all randomized patients with baseline HRQoL included and analyzed according to the allocated intervention) and per protocol population (PP: eligible patients and analyzed according to the intervention actually received). These three populations will be described according to the following characteristics: compliance with eligibility criteria, epidemiological characteristics, clinical and laboratory characteristics, treatment characteristics, and HRQoL. For the co-primary endpoints, the primary analysis will be conducted in the mITT population, with sensitivity analyses conducted in the PP population. OS will first be compared based on a log-rant test stratified on randomization factors (2% type 1 error rate). Additional analyses will be conducted including Cox regression modeling to provide an estimate of the effect size of the intervention, after checking for underlying model assumptions. For each targeted HRQoL dimension, a t-test assuming common variances will be conducted (1% type 1 error rate). Sensitivity analyses assuming a mean difference of 5 points or more for at least one of the targeted HRQoL scores will be conducted. In addition, variance analysis will be conducted for adjustment on randomization factors and additional covariates. Other endpoints will be analyzed using standard statistical techniques. PFS will be analyzed using the same methods as for OS. Censoring mechanisms for the analysis of TUDD will follow recommendations from Bonnetain et al. [28]. With regards to HRQoL data, missing data analysis will be performed to determine the missing data profile. Longitudinal models will be fitted to provide a description of the HRQoL over time and investigate effect of the intervention. For patients treated in the “Case-Management” arm, the analysis of geriatric parameters will involve summary statistics presented at various time-points as well longitudinal analysis to investigate trends over time.
Monitoring and ethical considerations
The trial has been approved by the regional ethics committee (Comité de Protection des Personnes Sud-Ouest et Outre Mer III) and by the National Agency for Security of Medical and Health products (ANSM) and has been registered (Trial registration number: 2015-A01417-42). All patients will provide informed consent (both for the randomized trial and prospective cohort) and will be free to withdraw their consent at any time.
The study will be supervised and monitored continuously by a steering committee consisting of the principal investigator (oncologist), a coordinating geriatrician, a pharmacist in charge of the pharmacovigilance, a biostatistician, a data manager and the coordinating clinical research assistant. This committee will ensure the implementation and regular follow-up of the study, patient protection, ethical conduct of trial and evaluation of benefit/risk ratio. The scientific committee will include the steering committee as well as additional geriatrics, medical oncology, public health and biostatistics specialists. It will be responsible for validation modifications of the study protocol and reviewing scientific findings during the course of the study, providing patient protection, ethical conduct of trial and evaluation of benefit/risk ratio. An independent data monitoring committee (IDMC) has been foreseen and will be set up at least once during the course of the study.
Discussion
Currently, the G8 is recommended for systematic use in France [33] to identify patients requiring increased clinical attention up to full geriatric assessment, and potentially a geriatric intervention plan. This generates a certain cost, for the CGA and for the geriatric interventions proposed, yet the gains in survival or HRQoL of these geriatric interventions have not yet been demonstrated. The current evidence to suggest that geriatric interventions have a positive impact on survival and HRQoL in elderly cancer patients is limited and conflicting, and randomized controlled trial data in this specific context are required.
The current study protocol proposes a two-arm randomized comparison trial of usual cancer care versus usual cancer care combined with geriatric intervention, in a group of elderly patients across multiple centers in France. Our randomized trial offers an innovative approach introducing a co-primary endpoint including both OS and HRQoL. This methodology integrates the HRQoL dimension in addition to life span, which may reflect elderly people expectations.
As such, we propose to compare efficacy using a co-primary endpoint encompassing OS and specific dimensions of HRQoL at one year – this is the first time this elderly-specific endpoint has been proposed in this context.
Acknowledgements
The authors thank Pippa McKelvie-Sebileau and Dr. Ravi Nookala of Institut Bergonié for medical writing services.
Funding
We received funding for this study from the French Ministry of Health (grant numbers: INCa-DGOS_8536 and INCa-DGOS_5500).
Availability of data and materials
Not applicable.
Authors’ contributions
Conception and Design: PS, CT, CB, FB, OSJ, SM-P, MR, M-DZ. Manuscript Writing: PS, CB, CC, SM-P, MR, AG. All authors approved the final article for submission.
Competing interests
The authors declare no competing interests.
Consent to publish
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the Agence National de Securité du Medicament et des produits de santé (ANSM), French Ministry of Health, Reference number 151610B-12.
Abbreviations
- ADL
Activities of daily living
- BMI
Body mass index
- CGA
Comprehensive geriatric assessment
- EORTC
The European Organization for Research and Treatment of Cancer
- GDS
Geriatric depression scale
- HR
Hazard ratio
- HRQoL
Health related quality of life
- IADL
Instrumental activities of daily living
- IDMC
Independent data monitoring committee
- ITT
Intent-to-treat
- mITT
Modifiedodified intent-to-treat
- MMSE
Mini mental state examination
- MNA
Mini nutritional assessment
- OS
Overall survival
- PFS
Progression-free survival
- RCTs
Randomized control trials
- SPPB
Short performance physical battery
- TUDD
Time until definitive deterioration
- TUG
Timed up and go
Appendix
Appendix A
Table 3.
The G8 screening test
| Items | Possible answers (score) | |
|---|---|---|
| A | Has food intake declined over the past 3 months due to loss of appetite, digestive problems, chewing or swallowing difficulties? | 0 : severe decrease in food intake |
| 1 : moderate decrease in food intake | ||
| 2 : no decrease in food intake | ||
| B | Weight loss during the last 3 months | 0 : weight loss > 3 kg |
| 1 : does not know | ||
| 2 : weight loss between 1 and 3 kgs | ||
| 3 : no weight loss | ||
| C | Mobility | 0 : bed or chair bound |
| 1 : able to get out of bed/chair but does not go out | ||
| 2 : goes out | ||
| E | Neuropsychological problems | 0 : severe dementia or depression |
| 1 : mild dementia or depression | ||
| 2 : no psychological problems | ||
| F | Body Mass Index (BMI (weight in kg)/(height in m2) | 0 : BMI < 19 |
| 1 : BMI = 19 to BMI < 21 | ||
| 2 : BMI = 21 to BMI < 23 | ||
| 3 : BMI = 23 and > 23 | ||
| H | Takes more than 3 medications per day | 0 : yes |
| 1 : no | ||
| P | In comparison with other people of the same age, how does the patient consider his/her health status? | 0 : not as good |
| 0.5 : does not know | ||
| 1 : as good | ||
| 2 : better | ||
| Age | 0 : >85 | |
| 1 : 80–85 | ||
| 2 : <80 | ||
| Total Score | 0–17 |
Appendix B: Writing and Validation Committees of the Cancer Care Protocol
Writing Committee: Catherine Terret (Medical Oncologist, Lyon, Chair), Thomas Aparicio (Gastro-enterologist, Paris), Etienne Brain (Medical Oncologist, Paris), Camille Chakiba (Medical Oncologist, Bordeaux), Stéphane Culine (Medical Oncologist, Paris), Gilles Freyer (Medical Oncologist, Lyon), Caroline Lalet (Central Clinical Research Assistant, Bordeaux), Hervé Le Caer (Pneumologist, Draguignan), Loic Mourey (Medical Oncologist, Toulouse), Pierre Soubeyran (Medical Oncologist, Bordeaux).
Validation Committee: Leila BENGRINE-LEFEVRE (Medical Oncologist, Dijon), Emmanuelle BOURBOULOUX (Medical Oncologist, Nantes), Nicole TUBIANA-MATHIEU (Medical Oncologist, Limoges), Simon VALERO (Geriatrician, Poitiers).
Appendix C: Writing and Validation Committees of the Geriatric Care Protocol
Writing Committee: Muriel Rainfray (Geriatrician, Bordeaux, Co-Chair), Olivier St Jean (Geriatrician, Paris, Co-Chair), Camille Chakiba (Medical Oncologist, Bordeaux), Caroline Lalet (Central Clinical Research Assistant, Bordeaux), Marie-Dominique Zwolakowski (Advanced Practice Nurse, Bordeaux).
Validation Committee: Laurent Balardy (Geriatrician, Toulouse), Laurence CRISTOL-DALSTEIN (Geriatrician, Montpellier), Jean-Yves NIEMIER (Geriatrician, Nancy), Frédérique Retornaz (Geriatrician, Marseille), Véronique SERVENT (Medical Oncologist, Lille).
Contributor Information
Pierre Soubeyran, Phone: +33 (5) 56 33 32 69, Email: p.Soubeyran@bordeaux.unicancer.fr.
Catherine Terret, Email: catherine.terret@lyon.unicancer.fr.
Carine Bellera, Email: C.Bellera@bordeaux.unicancer.fr.
Franck Bonnetain, Email: franck.bonnetain@univ-fcomte.fr.
Olivier Saint Jean, Email: olivier.saint-jean@egp.aphp.fr.
Angéline Galvin, Email: Angeline.Galvin@isped.u-bordeaux2.fr.
Camille Chakiba, Email: camille.chakiba@gmail.com.
Marie-Dominique Zwolakowski, Email: M.Zwolakowski@bordeaux.unicancer.fr.
Simone Mathoulin-Pélissier, Email: S.Mathoulin@bordeaux.unicancer.fr.
Muriel Rainfray, Email: muriel.rainfray@chu-bordeaux.fr.
References
- 1.Extermann M, Green T, Tiffenberg G, Rich C. Validation of the Senior Adult Oncology Program (SAOP) 2 screening questionnaire. Crit Rev Oncol Hematol. 2009;69(2):183–5. doi: 10.1016/j.critrevonc.2008.11.001. [DOI] [Google Scholar]
- 2.Hamaker ME, Jonker JM, de Rooij SE, et al. Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: a systematic review. Lancet Oncol. 2012;13(10):e437–e444. doi: 10.1016/S1470-2045(12)70259-0. [DOI] [PubMed] [Google Scholar]
- 3.Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE prospective multicenter cohort study. PLoS One. 2014;9(12):e115060. doi: 10.1371/journal.pone.0115060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saliba D, Elliott M, Rubenstein LZ, et al. The vulnerable elders survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49(12):1691–9. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 5.Bellera CA, Rainfray M, Mathoulin-Pelissier S, et al. Screening older cancer patients: first evaluation of the G-8 geriatric screening tool. Ann Oncol. 2012;23:2166–72. doi: 10.1093/annonc/mdr587. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin JS, Satish S, Anderson ET, Nattinger AB, Freeman JL. Effect of nurse case management on the treatment of older women with breast cancer. J Am Geriatr Soc. 2003;51(9):1252–9. doi: 10.1046/j.1532-5415.2003.51409.x. [DOI] [PubMed] [Google Scholar]
- 7.Morey MC, Snyder DC, Sloane R, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA. 2009;301(18):1883–91. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galvao DA, Taaffe DR, Spry N, Joseph D, Newton RU. Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial. J Clin Oncol. 2010;28(2):340–7. doi: 10.1200/JCO.2009.23.2488. [DOI] [PubMed] [Google Scholar]
- 9.Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25(19):2709–18. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- 10.Hempenius L, Slaets JP, Van AD, et al. Outcomes of a geriatric liaison intervention to prevent the development of postoperative delirium in frail elderly cancer patients: report on a multicentre, randomized, controlled trial. PLoS One. 2013;8(6):e64834. doi: 10.1371/journal.pone.0064834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubenstein LZ, Josephson KR, Wieland GD, et al. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med. 1984;311(26):1664–70. doi: 10.1056/NEJM198412273112604. [DOI] [PubMed] [Google Scholar]
- 12.Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342(8878):1032–6. doi: 10.1016/0140-6736(93)92884-V. [DOI] [PubMed] [Google Scholar]
- 13.Bourdel-Marchasson I, Blanc-Bisson C, Doussau A, et al. Nutritional advice in older patients at risk of malnutrition during treatment for chemotherapy: a two-year randomized controlled trial. PLoS One. 2014;9(9):e108687. doi: 10.1371/journal.pone.0108687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao AV, Hsieh F, Feussner JR, Cohen HJ. Geriatric evaluation and management units in the care of the frail elderly cancer patient. J Gerontol A Biol Sci Med Sci. 2005;60(6):798–803. doi: 10.1093/gerona/60.6.798. [DOI] [PubMed] [Google Scholar]
- 15.McCorkle R, Strumpf NE, Nuamah IF, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. J Am Geriatr Soc. 2000;48(12):1707–13. doi: 10.1111/j.1532-5415.2000.tb03886.x. [DOI] [PubMed] [Google Scholar]
- 16.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 17.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A Standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 19.Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15(2):116–22. doi: 10.1016/S0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- 20.Sheikh J, Yesavage JA. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–71. doi: 10.1300/J018v05n01_09. [DOI] [Google Scholar]
- 21.Johnson C, Fitzsimmons D, Gilbert J, et al. Development of the European Organisation for Research and Treatment of Cancer quality of life questionnaire module for older people with cancer: The EORTC QLQ-ELD15. Eur J Cancer. 2010;46(12):2242–52. doi: 10.1016/j.ejca.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67(6):387–9. [PubMed] [Google Scholar]
- 23.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.M221. [DOI] [PubMed] [Google Scholar]
- 24.Pallis AG, Ring A, Fortpied C, et al. EORTC workshop on clinical trial methodology in older individuals with a diagnosis of solid tumors. Ann Oncol. 2011;22(8):1922–6. doi: 10.1093/annonc/mdq687. [DOI] [PubMed] [Google Scholar]
- 25.Wildiers H, Mauer M, Pallis A, et al. End points and trial design in geriatric oncology research: a joint European organisation for research and treatment of cancer—Alliance for Clinical Trials in Oncology—International Society Of Geriatric Oncology position article. J Clin Oncol. 2013;31(29):3711–8. doi: 10.1200/JCO.2013.49.6125. [DOI] [PubMed] [Google Scholar]
- 26.Fayers P, Bottomley A. Quality of life research within the EORTC 2014;the EORTC QLQ-C30. Eur J Cancer;38:125–33. [DOI] [PubMed]
- 27.Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16(1):139–44. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 28.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 29.Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25(5):579–86. doi: 10.1200/JCO.2006.09.2403. [DOI] [PubMed] [Google Scholar]
- 30.Wheelwright S, Darlington AS, Fitzsimmons D, et al. International validation of the EORTC QLQ-ELD14 questionnaire for assessment of health-related quality of life elderly patients with cancer. Br J Cancer. 2013;109(4):852–8. doi: 10.1038/bjc.2013.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bonnetain F, Dahan L, Maillard E, et al. Time until definitive quality of life score deterioration as a means of longitudinal analysis for treatment trials in patients with metastatic pancreatic adenocarcinoma. Eur J Cancer. 2010;46(15):2753–62. doi: 10.1016/j.ejca.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 32.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31(1):103–15. doi: 10.2307/2529712. [DOI] [PubMed] [Google Scholar]
- 33.http://www.e-cancer.fr/Expertises-et-publications/Catalogue-des-publications/Suivi-du-dispositif-de-prise-en-charge-et-de-recherche-clinique-en-oncogeriatrie-Etat-des-lieux-au-1er-janvier-2015. 2015. Ref Type: Online Source
- 34.Demark-Wahnefried W, Morey MC, Sloane R, et al. Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. J Clin Oncol. 2012;30(19):2354–61. doi: 10.1200/JCO.2011.40.0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lapid MI, Rummans TA, Brown PD, et al. Improving the quality of life of geriatric cancer patients with a structured multidisciplinary intervention: a randomized controlled trial. Palliat Support Care. 2007;5(2):107–14. doi: 10.1017/S1478951507070174. [DOI] [PubMed] [Google Scholar]
- 36.Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346(12):905–12. doi: 10.1056/NEJMsa010285. [DOI] [PubMed] [Google Scholar]
- 37.Lang PO, Hasso Y, Belmin J, et al. STOPP-START: adaptation of a French language screening tool for detecting inappropriate prescriptions in older people. Can J Public Health. 2009;100(6):426–31. doi: 10.1007/BF03404338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83. doi: 10.5414/CPP46072. [DOI] [PubMed] [Google Scholar]
- 39.Inouye SK, Bogardus ST, Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–76. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 40.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


