Abstract
Cryptosporidium spp. and Enterocytozoon bieneusi are two prevalent opportunistic pathogens in humans and animals. Currently, few data are available on genetic characterization of both pathogens in rabbits in China. The aim of the present study was to understand prevalence and genetic characterization of Cryptosporidium spp. and E. bieneusi in rabbits. We collected 215 fecal samples from 150 Rex rabbits and 65 New Zealand White rabbits on two different farms in Heilongjiang Province, China. Cryptosporidium spp. and E. bieneusi were tested by polymerase chain reaction (PCR) and sequencing the partial small subunit of ribosomal DNA (SSU rDNA) and the internal transcribed spacer (ITS) region of rDNA, respectively. Cryptosporidium was detected in 3.3% (5/150) of Rex rabbits and 29.2% (19/65) of New Zealand White rabbits. All the 24 Cryptosporidium isolates were identified as C. cuniculus. Enterocytozoon bieneusi was only found in 14.7% (22/150) of Rex rabbits. Five known genotypes: CHN-RD1 (n = 12), D (n = 3), Type IV (n = 2), Peru6 (n = 1), and I (n = 1), and three novel ones CHN-RR1 to CHN-RR3 (one each) were detected. By analyzing the 60-kDa glycoprotein (gp60) gene sequences of C. cuniculus isolates, three subtypes were obtained: VbA28 (n = 2), VbA29 (n = 16), and VbA32 (n = 3). All these three C. cuniculus subtypes were reported previously in humans. Four known E. bieneusi genotypes have been found to be present in humans. The three novel ones fell into zoonotic group 1. The results suggest zoonotic potential of C. cuniculus and E. bieneusi isolates in rabbits.
Keywords: rabbits, Cryptosporidium, Enterocytozoon bieneusi, ITS region, SSU rDNA, gp60 gene
Abstract
Cryptosporidium spp. et Enterocytozoon bieneusi sont deux agents pathogènes opportunistes répandus chez les humains et les animaux. Actuellement, peu de données sont disponibles sur la caractérisation génétique de ces deux agents pathogènes chez les lapins en Chine. Le but de la présente étude était de comprendre la prévalence et la caractérisation génétique des Cryptosporidium spp. et E. bieneusi chez les lapins. Nous avons recueilli 215 échantillons fécaux de 150 lapins Rex et 65 lapins blancs de Nouvelle Zélande dans deux fermes différentes dans la province du Heilongjiang, en Chine. Cryptosporidium spp. et E. bieneusi ont été testés par PCR et respectivement par séquençage partiel de la petite sous-unité de l’ADN ribosomal (SSU-ADNr) et de la région ITS de l’ADNr. Cryptosporidium a été détecté dans 3.3 % (5/150) des lapins Rex et 29.2 % (19/65) des lapins blancs de Nouvelle-Zélande. Tous les 24 isolats de Cryptosporidium ont été identifiés comme C. cuniculus. Enterocytozoon bieneusi n’a été trouvé que dans 14.7 % (22/150) des lapins Rex. Cinq génotypes connus : CHN-RD1 (n = 12), D (n = 3), Type IV (n = 2), Peru6 (n = 1) et I (n = 1), et trois nouveaux, CHN-RR1 à CHN-RR3 (un de chaque) ont été détectés. En analysant les séquences du gène de la glycoprotéine de 60 kDa (gp60) des isolats de C. cuniculus, trois sous-types ont été obtenus: VbA28 (n = 2), VbA29 (n = 16) et VBA32 (n = 3). Ces trois sous-types de C. cuniculus ont été rapportés auparavant chez l’homme. Quatre génotypes d’E. bieneusi connus ont été rapportés chez les humains. Les trois nouveaux appartiennent au groupe zoonotique 1. Les résultats suggèrent un potentiel zoonotique des isolats de C. cuniculus et E. bieneusi des lapins.
Introduction
Cryptosporidium spp. and Enterocytozoon bieneusi are obligate intracellular eukaryotes, and both of them can infect the intestine of hosts. Clinical symptoms of human disease caused by either Cryptosporidium or E. bieneusi are variable, ranging from asymptomatic infection or self-limiting diarrhea in healthy people to chronic or life-threatening diarrhea in immunocompromsied individuals [33, 48]. Besides humans, these microorganisms have also been found in numerous animal species [33, 41].
Cryptosporidium is a complex genus. To date, 30 Cryptosporidium species and more than 40 genotypes have been described, and among them, 20 Cryptosporidium species/genotypes have been reported in humans, with C. hominis and C. parvum responsible for the majority of infections [15, 23, 28, 41, 42]. For E. bieneusi, more than 240 ITS genotypes have been identified worldwide [18, 45], and at least 70 genotypes have been found in humans, with 33 genotypes being zoonotic [21, 33, 61]. In phylogenetic analysis, all the published genotypes belong to nine distinct groups. Group 1 is composed of the common zoonotic genotypes and groups 2–9 mostly contain host-adapted genotypes [14, 19, 33]. The findings of the same species/genotypes of the two pathogens in humans and animals support presumption of zoonotic potential [33, 41].
Currently, fumagillin is effective in the treatment of microsporidiosis caused by E. bieneusi [2], while nitazoxanide has an effect on cryptosporidiosis in non-HIV patients to a certain extent [41]. However, understanding Cryptosporidium and E. bieneusi epidemiology in different host species is still a key step to prevent Cryptosporidium and E. bieneusi infections in humans, particularly in determining the zoonotic potential of animal-derived isolates.
In China, Rex rabbits are one of the most common farmed animal species used for fur and meat production; and with the development of the fur industry in recent years, the number of Rex rabbits has been increasing. New Zealand White rabbits are mainly used for food production and experiments. The aim of the present study was to understand the prevalence of natural infection and genetic characterization of Cryptosporidium and E. bieneusi in Rex rabbits and New Zealand White rabbits. In addition, the zoonotic potential of Cryptosporidium and E. bieneusi isolates was assessed.
Materials
Ethics statement
Before beginning this study, we described the protocol to the farm managers and obtained their permission. In this study, only fecal samples of the farm animals were collected. Meanwhile, the study protocol was reviewed and approved by the Research Ethics Committee and the Animal Ethics Committee of Harbin Medical University. The work concerning animals strictly followed guidelines in accordance with the Regulations for the Administration of Affairs Concerning Experimental Animals.
Specimen collection
During the period from March 2015 to February 2016, a total of 215 rabbit fecal samples were collected from Heilongjiang Province, China, including 150 from Rex rabbits on a farm in Huaqiang Fur Breeding Base in Bayan County and 65 from New Zealand White rabbits on a farm in Huaxing Breeding Base of Rabbits in Harbin City. One fresh fecal specimen (approximately 15 g) of each animal was collected. All the fecal specimens were transported to our laboratory in a cooler with ice packs within 24 h and stored in refrigerators at 4 °C until molecular analysis. Rex rabbits and New Zealand White rabbits were collected from the two different farms, both accounting for approximately 5% of the total animals. Rex rabbits and New Zealand White rabbits were five or six and two or three months old, respectively. No apparent clinical signs of diarrhea were observed at the time of sampling.
DNA extraction
To reduce interference from crude fiber and impurities in rabbit manure, the fecal specimens were sieved and washed with distilled water by centrifugation for 10 min at 1500 g×. Genomic DNA was extracted from 180–200 mg washed fecal pellets using a QIAamp DNA Stool Mini Kit (QIAgen, Hilden, Germany) according to manufacturer-recommended procedures. DNA was eluted in 200 μL of AE buffer and stored at −20 °C in a freezer prior to polymerase chain reaction (PCR) analysis.
Cryptosporidium genotyping and subtyping
All genomic DNA samples were subjected to nested PCR targeting Cryptosporidium by amplification of an 830 bp nucleotide fragment of the small subunit (SSU) rDNA of Cryptosporidium. The primers and the cycling parameters in PCR analysis were used as previously described by Xiao et al. [52]. Subtyping of Cryptosporidium-positive samples was performed by nested PCR amplification of an approximately 800–850 bp fragment of the gp60 gene [1].
E. bieneusi genotyping
To identify the presence and genotypes of E. bieneusi, all the genomic DNA samples were subjected to nested PCR amplification of a 389 bp nucleotide fragment of the rDNA of E. bieneusi containing 76 bp of the 3′ end of SSU rDNA, 243 bp of the internal transcribed spacer (ITS) region, and 70 bp of the 5′ region of the large subunit (LSU) rDNA [7]. All the genotypes were named based on 243 bp of the ITS region of E. bieneusi according to the established nomenclature system [44].
Nucleotide sequencing and analyzing
All the secondary PCR products of the expected size were directly sequenced with primers used for the secondary PCR after being purified on an ABI PRISM 3730XL DNA Analyzer by Sinogeno- max Biotechnology Co. Ltd. (Beijing, China), using the BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, USA). Sequence accuracy was confirmed by two-directional sequencing and by sequencing a new PCR product if necessary for some DNA samples, from which novel nucleotide sequences were obtained. Nucleotide sequences obtained in the present study were subjected to BLAST searches (http://www.ncbi.nlm.nih.gov/blast/), and then aligned and analyzed with each other and reference sequences from GenBank using Clustal X 1.81 (http://www.clustal.org/).
Phylogenetic analysis
Phylogenetic relationships among subtypes of Cryptosporidium and genotypes of E. bieneusi determined in the present study with those presently available in public databases were explored using the Mega 5 program (http://www.megasoftware.net/) to construct two neighbor-joining trees based on the evolutionary distances calculated by the Kimura 2-parameter model. The reliability of the trees was assessed using the bootstrap analysis with 1000 replicates.
Results
Infection rates of Cryptosporidium and E. bieneusi
Cryptosporidium was detected in the two rabbit breeds by nested PCR amplification of the SSU rDNA. Infection rates of Cryptosporidium were 3.3% (5/150) and 29.2% (19/65) in Rex rabbits and New Zealand White rabbits, respectively. There was a significant difference in infection rates of Cryptosporidium between the two rabbit breeds by means of a χ2 test (χ2 = 30.67, p < 0.01) (Table 1).
Table 1.
Prevalences and genotypes/subtypes of C. cuniculus and E. bieneusi in rabbits.
| Host | Sample (n) |
C. cuniculus
|
E. bieneusi
|
||
|---|---|---|---|---|---|
| No. of positive (%) | Gp60 subtype (n) | No. of positive (%) | ITS genotypes (n) | ||
| Rex rabbits | 150 | 5 (3.3) | VbA32 (3) | 22 (14.7) | CHN-RD1 (12); D (3); Type IV (2); Peru6 (1); I (1); CHN-RR1 to CHN-RR3 (1 each) |
| New Zealand White rabbits | 65 | 19 (29.2) | VbA29 (16); VbA28 (2) | – | – |
Note: The bars denote negative results.
By amplifying the ITS region of the rDNA, E. bieneusi was detected in 14.7% (22/150) of Rex rabbits, and there was an absence of E. bieneusi in New Zealand White rabbits.
Cryptosporidium species and subtypes
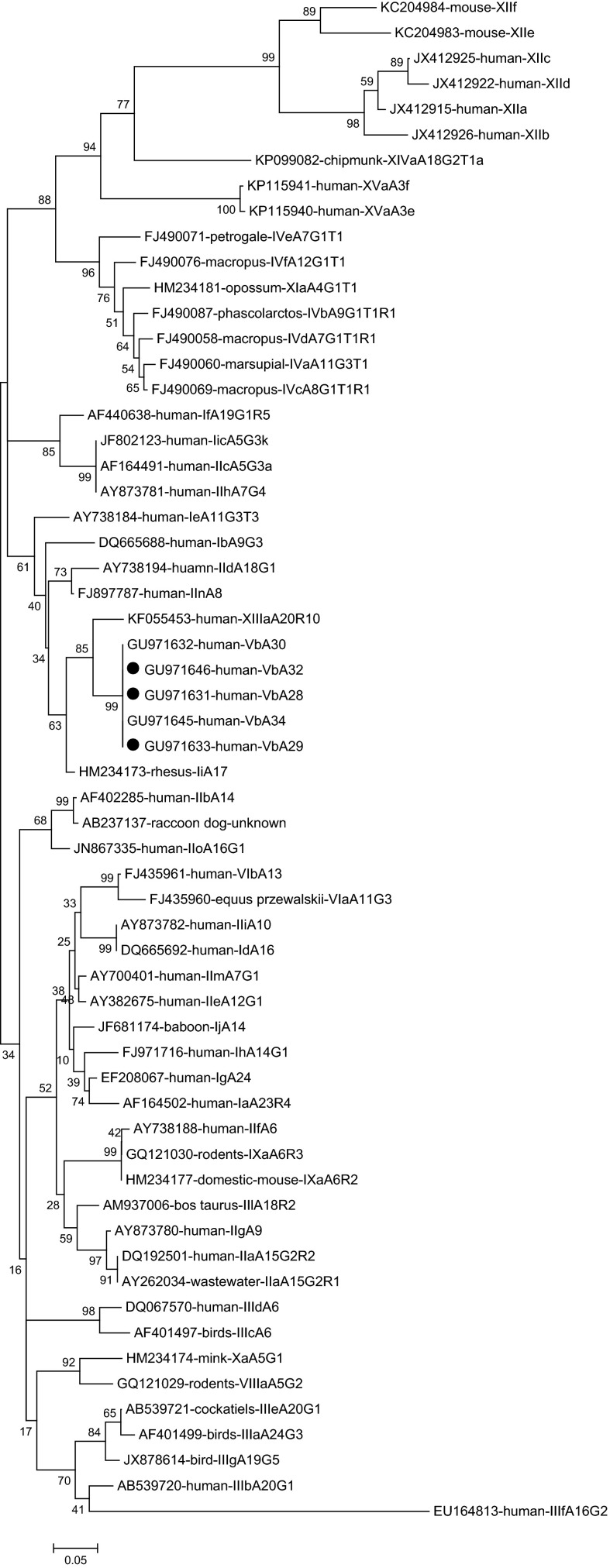
Analysis of 24 sequences of the SSU rDNA of Cryptosporidium showed that all the Cryptosporidium isolates were identical to each other and had 100% similarity with a C. cuniculus isolate from a rabbit (HQ397716). C. cuniculus-positive specimens were further subtyped by amplifying the gp60 gene. Only 21 C. cuniculus isolates produced the expected PCR product and were successfully sequenced. Three subtypes were observed according to established nomenclature [39]: VbA28 (n = 2), VbA29 (n = 16) and VbA32 (n = 3). Two subtypes VbA28 and VbA29 were identified in New Zealand White rabbits while one subtype VbA32 in Rex rabbits (Table 1). Phylogenetic analysis of the gp60 nucleotide sequences revealed that C. cuniculus subtypes VbA28, VbA29 and VbA32 fell into the same clade as C. erinacei subtype XIIIaA20R10, and were genetically close to C. parvum subtype families IId and IIn, and C. hominis subtype families Ib and Ii (Fig. 1).
Figure 1.
Phylogenetic relationship of gp60 subtypes of Cryptosporidium species/genotypes. The relationships between C. cuniculus subtypes identified in the present study and known subtypes of other Cryptosporidium species/genotypes deposited in the GenBank were inferred by a neighbor-joining analysis of gp60 gene sequences based on genetic distance by the Kimura 2-parameter model. The numbers on the branches are percent bootstrapping values from 1000 replicates. Each sequence is identified by its accession number, host origin, and subtype designation. The circles filled in black indicate the subtypes identified in this study.
E. bieneusi genotypes
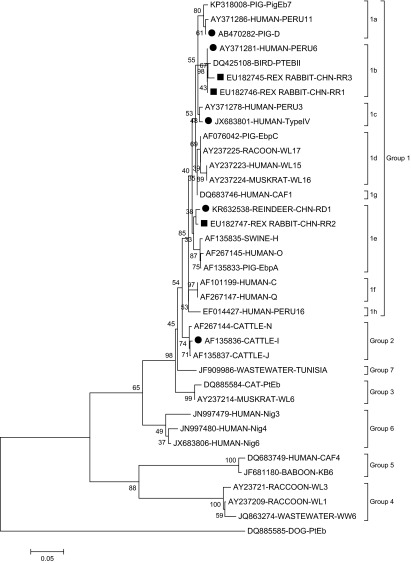
By nucleotide sequence analysis of the ITS region of the rDNA of E. bieneusi, eight genotypes were identified in the Rex rabbits, including five known genotypes (CHN-RD1, Type IV, Peru6, D, and I) and three novel ones (CHN-RR1, CHN-RR2, and CHN-RR3) (Table 1). Genotype CHN-RD1 was found in 54.5% (12/22) of E. bieneusi isolates, showing dominance. The remaining genotypes were all at a low frequency: 13.6% (3/22) for genotype D, 9.1% (2/22) for genotype Type IV, and 4.5% (1/22) for genotypes I, CHN-RR1, CHN-RR2, and CHN-RR3.
Genotype CHN-RR1 (KU182745) had two base deletions at nucleotide sites 51 and 52 of the ITS region. Genotypes CHN-RR2 (KU182746) and CHN-RR3 (KU182747) were observed to have one and two single-nucleotide polymorphisms compared to genotype G (AF135834) and genotype Peru6 (JF927955), respectively. In phylogenetic analysis, all the genotypes except genotype I (clustered into group 2) here belonged to zoonotic group 1: genotypes Peru6, CHN-RR1, and CHN-RR3 in subgroup 1b; genotype D in subgroup 1a; genotype Type IV in subgroup 1c; and genotypes CHN-RD1 and CHN-RR2 in subgroup 1e (Fig. 2).
Figure 2.
Phylogenetic relationships of Enterocytozoon bieneusi genotype groups. The relationships between Enterocytozoon bieneusi genotypes identified in the present study and other known genotypes deposited in the GenBank were inferred by a neighbor-joining analysis of ITS sequences based on genetic distance by the Kimura 2-parameter model. The numbers on the branches are percent bootstrapping values from 1000 replicates. Each sequence is identified by its accession number, host origin, and genotype designation. The group terminology for the clusters is based on the work of Zhao et al. [60]. The squares and circles filled in black indicate novel and known genotypes identified in this study, respectively.
Discussion
In the present study, Cryptosporidium was identified in the two rabbit breeds, with overall prevalence of 11.2% (24/215). Epidemiological data indicate that Cryptosporidium has previously been identified in rabbits in Japan, with 30.3% (20/66) in dead juvenile animals and 3.33% (1/30) in healthy animals [47], and in Australia (6.8%; 12/176) [35] as well as in some areas of China:Sichuan (1.03%; 3/290), Heilongjiang (2.38%, 9/378), and Henan (3.4%, 37/1081) [30, 46, 55]. In fact, Cryptosporidium in farm rabbits is not often recognized due to a low prevalence and asymptomatic course of infection. However, there is an outbreak of massive mortality among farm rabbits associated with Cryptosporidium infection in Poland [20]. Here, E. bieneusi was only found in 14.7% (22/150) of Rex rabbits, and the prevalence was higher than that (0.94%; 4/426) reported in a recent study in China [57]. To our best knowledge, there are another two studies reporting E. bieneusi infections in rabbits, where only a small number of rabbits were involved [11, 13]. The present finding of Cryptosporidium and E. bieneusi in the asymptomatic rabbits emphasized the importance of epidemiological investigations of the two pathogens in these animals.
By sequence analysis of the partial SSU rDNA, all 24 PCR specimens positive for Cryptosporidium were identified as C. cuniculus. C. cuniculus is one of the zoonotic Cryptosporidium species, which has been strongly linked to human cryptosporidiosis [41]. Molecular epidemiological data of human cryptosporidiosis have presented increasing occurrence of C. cuniculus in humans in some regions/countries. It was even considered to be the third most common Cryptosporidium species in clinical patients with cryptosporidiosis during the 2007–2008 period in the UK [10], including a waterborne outbreak of human cryptosporidiosis caused by C. cuniculus from a wild rabbit entering a treated tank [9]. In fact, some sporadic human cases have been reported in Nigeria, Australia, France, and Spain [3, 22, 32, 34]. Currently, natural infection of C. cuniculus has only been reported in rabbits and humans, as well as a kangaroo [22]. Rabbits have been confirmed to be the main hosts of natural infection of C. cuniculus. To date, experimental infections have only been established in weanling rabbits (Oryctolagus cuniculus), immunosuppressed Mongolian gerbils (Meriones unguiculatus), and immunosuppressed adult Porton strain mice (Mus musculus) [40]. C. cuniculus seems to have a narrow host range. The true host range of C. cuniculus needs to be confirmed by subsequent molecular epidemiological studies of Cryptosporidium. Gp60 gene sequencing is the most commonly used tool for Cryptosporidium subtyping, aimed at identifying infection sources, investigating transmission dynamics, and understanding genetic diversity within and between Cryptosporidium species/genotypes as well as their taxonomy [41]. In the present study, gp60-based subtyping of C. cuniculus isolates was achieved and three subtypes were identified: VbA28, VbA29, and VbA32. The observation that all the three subtypes here have been detected in humans [10] suggests their significance in public health. Here, subtype VbA28 was found in rabbits for the first time. Actually, two different families (Va and Vb) have been described within C. cuniculus. To date, nine and 20 subtypes have been found in the two different subtype families, respectively [5, 9, 10, 20, 22, 30, 35, 36, 40, 46, 55] (Table 2). Based on the data summarized in Table 2, the subtypes in the Va family are mostly found in humans and occasionally seen in rabbits; in contrast, the subtypes in the Vb family appear to be more common in rabbits than in humans. By phylogenetic analysis, the subtypes in the Vb family fell into a clade with C. parvum and C. hominis (Fig. 1). In a previous phylogenetic analysis of the SSU rDNA and hsp70 genes, C. cuniculus was observed to be genetically most closely related to C. hominis, sharing 99.2% similarity with C. hominis at the SSU rDNA locus and 99.7% similarity with C. hominis at the hsp70 locus [43]. In another study, on the basis of a distance matrix derived from the alignment utilized herein to construct the phylogeny, C. cuniculus was reported to be genetically closest to C. parvum and C. hominis, sharing 98% similarity with each of them [35].
Table 2.
Subtypes of C. cuniculus in humans and rabbits worldwide.
| Host | Country | Va family | Vb family | Ref. |
|---|---|---|---|---|
| Human | Australia | VbA25 | [22] | |
| UK | VaA9; VaA11; VaA18; VaA19; VaA21; VaA22; VaA23 | VbA20; VbA22; VbA25; VbA26; VbA28; VbA29; VbA30; VbA32; VbA33; VbA34; VbA36; VbA37 | [10, 40] | |
| VaA18; VaA22 | [9] | |||
| VaA18; VaA22; VaA23; VaA32 | [5] | |||
| Rabbit | Australia | VbA23R3; VbA26R4 | [35] | |
| VbA22R4; VbA23R3; VbA24R3; VbA25R4; VbA26R4 | [36] | |||
| China | VaA31 | [30] | ||
| VbA21; VbA32 | [55] | |||
| VbA36; VbA35; VbA29 | [46] | |||
| VbA28, VbA29 and VbA32 | This study | |||
| Czech Republic | VaA19 | [9] | ||
| Poland | VbA24 | [20] | ||
| UK | VaA18 | [9] |
By sequence analysis of the ITS region of the rDNA, eight genotypes were identified out of 22 E. bieneusi isolates, including five known and three novel isolates (Table 1). Genotype CHN-RD1 showed predominance in Rex rabbits (54.5%; 12/22). This genotype was originally detected in reindeers living in the northeast forest region of Great Hinggan Mountains, China [29]. The other four known genotypes (Type IV, Peru6, D, and I) have previously been found in both humans and animals, suggesting possible zoonotic transmission from Rex rabbits to humans [33, 45]. Genotypes D and Type IV are currently the two most common genotypes diagnosed in human cases of microsporidiosis caused by E. bieneusi [33]. Genotype D has the widest geographical distribution and animal host range [45, 60]. In China, both genotypes have been identified in children, and in HIV-positive and HIV-negative patients [50, 51, 53]. Meanwhile, they have also been found in nonhuman primates, pigs, deer, foxes, raccoon dogs, dogs, cats, rabbits, squirrels, chinchillas, snakes, Siberian tigers, lions, hippopotamus, common cranes, a red-crowned crane, a Fischer’s lovebird, and some other captive wildlife, as well as in wastewater and lake water [12, 16–18, 24–27, 38, 54, 58, 59, 61, 63]. Compared to genotypes D and Type IV, genotypes Peru6 and I have a small number and a limited geographical area in human cases infected with E. bieneusi, with the former only found in Peru and Portugal [4, 8, 31, 49], and the latter only in China [56]. In China, to date, genotype Peru6 has been identified in sheep and goats, reindeers, red-crowned cranes, ducks, geese, and pigeons, as well as in wastewater [25, 29, 62, 63]; genotype I has been found in nonhuman primates, cats, a chicken, pigeons, pigs, and golden takins [13, 16, 17, 37, 39, 59, 60].
In a phylogenetic analysis, all the three novel genotypes fell into zoonotic group 1. Group 1 is reported to contain 94% of the published ITS sequences of E. bieneusi and almost all the human-pathogenic genotypes are in this group [33]. Thus, the novel genotypes obtained here may have a large zoonotic potential.
In the present study, it was observed that there were only 241 bp in the ITS region of novel genotype CHN-RR1. In fact, length variation of the ITS region of the rDNA of E. bieneusi has been found: 241 bp for genotypes CHN3, CHN4 and CHN5 from children in China [56], and 242 bp for genotype CAF4 from a human in Gabon [6]. The ITS region is 243 bp in length for the vast majority of E. bieneusi genotypes.
Conclusion
Our present study demonstrated an occurrence of C. cuniculus and E. bieneusi in rabbits in Heilongjiang Province, China. All the C. cuniculus subtypes have previously been reported in humans. All the known E. bieneusi genotypes except CHN-RD1 are human-pathogenic, with all the novel ones falling into zoonotic group 1. The facts above suggest zoonotic potential of C. cuniculus and E. bieneusi isolates in these animals. It is therefore necessary to make farmers and veterinarians aware of the potential for zoonotic transmission of cryptosporidiosis and microsporidiosis as a result of close contact with infected rabbits.
Conflict of interest
The authors declare that they have no conflict of interest in relation with this paper.
Acknowledgments
This work was supported partially by the Chinese Special Program for Scientific Research of Public Health (No. 201502021) and the Heilongjiang Province Education Bureau (No.12531266).
Cite this article as: Yang Z, Zhao W, Shen Y, Zhang W, Shi Y, Ren G, Yang D, Ling H, Yang F, Liu A & Cao J: Subtyping of Cryptosporidium cuniculus and genotyping of Enterocytozoon bieneusi in rabbits in two farms in Heilongjiang Province, China. Parasite, 2016, 23, 52.
References
- 1. Alves M, Xiao L, Sulaiman I, Lal AA, Matos O, Antunes F. 2003. Subgenotype analysis of Cryptosporidium isolates from humans, cattle, and zoo ruminants in Portugal. Journal of Clinical Microbiology, 41(6), 2744–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anane S, Attouchi H. 2010. Microsporidiosis: epidemiology, clinical data andtherapy. Gastroentérologie Clinique et Biologique, 34(8–9), 450–464. [DOI] [PubMed] [Google Scholar]
- 3. ANOFEL Cryptosporidium National Network. 2010. Laboratory-based surveillance for Cryptosporidium in France, 2006–2009. Euro Surveillance, 15(33), 19642. [PubMed] [Google Scholar]
- 4. Bern C, Kawai V, Vargas D, Rabke-Verani J, Williamson J, Chavez-Valdez R, Xiao L, Sulaiman I, Vivar A, Ticona E, Navincopa M, Cama V, Moura H, Secor WE, Visvesvara G, Gilman RH. 2005. The epidemiology of intestinal microsporidiosis in patients with HIV/AIDS in Lima Peru. Journal of Infectious Diseases, 191(10), 1658–1664. [DOI] [PubMed] [Google Scholar]
- 5. Bouzid M, Tyler KM, Christen R, Chalmers RM, Elwin K, Hunter PR. 2010. Multi-locus analysis of human infective Cryptosporidium species and subtypes using ten novel genetic loci. BMC Microbiology, 10, 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Breton J, Bart-Delabesse E, Biligui S, Carbone A, Seiller X, Okome-Nkoumou M, Nzamba C, Kombila M, Accoceberry I, Thellier M. 2007. New highly divergent rRNA sequence among biodiverse genotypes of Enterocytozoon bieneusi strains isolated from humans in Gabon and Cameroon. Journal of Clinical Microbiology, 45(8), 2580–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buckholt MA, Lee JH, Tzipori S. 2002. Prevalence of Enterocytozoon bieneusi in swine: an 18-month survey at a slaughterhouse in Massachusetts. Applied and Environmental Microbiology, 68(5), 2595–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cama VA, Pearson J, Cabrera L, Pacheco L, Gilman R, Meyer S, Ortega Y, Xiao L. 2007. Transmission of Enterocytozoon bieneusi between a child and guinea pigs. Journal of Clinical Microbiology, 45(8), 2708–2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chalmers RM, Robinson G, Elwin K, Hadfield SJ, Xiao L, Ryan U, Modha D, Mallaghan C. 2009. Cryptosporidium sp. rabbit genotype, a newly identified human pathogen. Emerging Infectious Diseases, 15(5), 829–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chalmers RM, Elwin K, Hadfield SJ, Robinson G. 2011. Sporadic human cryptosporidiosis caused by Cryptosporidium cuniculus, United Kingdom, 2007–2008. Emerging Infectious Diseases, 17(3), 536–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. del Aguila C, Izquierdo F, Navajas R, Pieniazek NJ, Miró G, Alonso AI, Da Silva AJ, Fenoy S. 1999. Enterocytozoon bieneusi in animals: rabbits and dogs as new hosts. Journal of Eukaryotic Microbiology, 46(5), 8S–9S. [PubMed] [Google Scholar]
- 12. Deng L, Li W, Yu X, Gong C, Liu X, Zhong Z, Xie N, Lei S, Yu J, Fu H, Chen H, Xu H, Hu Y, Peng G. 2016. First report of the human-pathogenic Enterocytozoon bieneusi from red-bellied tree squirrels (Callosciurus erythraeus) in Sichuan, China. PLoS One, 11(9), e0163605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Galván-Díaz AL, Magnet A, Fenoy S, Henriques-Gil N, Haro M, Gordo FP, Millán J, Miró G, del Águila C, Izquierdo F. 2014. Microsporidia detection and genotyping study of human pathogenic E. bieneusi in animals from Spain. PLoS One, 9(3), e92289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guo Y, Alderisio KA, Yang W, Cama V, Feng Y, Xiao L. 2014. Host specificity and source of Enterocytozoon bieneusi genotypes in a drinking source watershed. Applied and Environmental Microbiology, 80(1), 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holubová N, Sak B, Horčičková M, Hlásková L, Květoňová D, Menchaca S, McEvoy J, Kváč M. 2016. Cryptosporidium avium n. sp. (Apicomplexa: Cryptosporidiidae) in birds. Parasitology Research, 115(6), 2243–2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Karim MR, Dong H, Yu F, Jian F, Zhang L, Wang R, Zhang S, Rume FI, Ning C, Xiao L. 2014. Genetic diversity in Enterocytozoon bieneusi isolates from dogs and cats in China: host specificity and public health implications. Journal of Clinical Microbiology, 52(9), 3297–3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karim MR, Wang R, Dong H, Zhang L, Li J, Zhang S, Rume FI, Qi M, Jian F, Sun M, Yang G, Zou F, Ning C, Xiao L. 2014. Genetic polymorphism and zoonotic potential of Enterocytozoon bieneusi from nonhuman primates in China. Applied and Environmental Microbiology, 80(6), 1893–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Karim MR, Yu F, Li J, Li J, Zhang L, Wang R, Rume FI, Jian F, Zhang S, Ning C. 2014. First molecular characterization of enteric protozoa and the human pathogenic microsporidian, Enterocytozoon bieneusi, in captive snakes in China. Parasitology Research, 113(8), 3041–3048. [DOI] [PubMed] [Google Scholar]
- 19. Karim MR, Dong H, Li T, Yu F, Li D, Zhang L, Li J, Wang R, Li S, Li X, Rume FI, Ning C. 2015. Predomination and new genotypes of Enterocytozoon bieneusi in captive nonhuman primates in zoos in China: high genetic diversity and zoonotic significance. PLoS One, 10(2), e0117991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaupke A, Kwit E, Chalmers RM, Michalski MM, Rzeżutka A. 2014. An outbreak of massive mortality among farm rabbits associated with Cryptosporidium infection. Research in Veterinary Science, 97(1), 85–87. [DOI] [PubMed] [Google Scholar]
- 21. Khanduja S, Ghoshal U, Agarwal V, Pant P, Ghoshal UC. 2016. Identification andgenotyping of Enterocytozoon bieneusi among human immunodeficiency virus infected patients. Journal of Infection and Public Health, pii, S1876-0341(16)00016-2. [DOI] [PubMed]
- 22. Koehler AV, Whipp MJ, Haydon SR, Gasser RB. 2014. Cryptosporidium cuniculus – new records in human and kangaroo in Australia. Parasites & Vectors, 7, 492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kváč M, Havrdová N, Hlásková L, Daňková T, Kanděra J, Ježková J, Vítovec J, Sak B, Ortega Y, Xiao L, Modrý D, Chelladurai JR, Prantlová V, McEvoy J. 2016. Cryptosporidium proliferans n. sp. (Apicomplexa: Cryptosporidiidae): molecular and biological evidence of cryptic species within gastric Cryptosporidium of Mammals. PLoS One, 11(1), e0147090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li J, Qi M, Chang Y, Wang R, Li T, Dong H, Zhang L. 2015. Molecular characterization of Cryptosporidium spp., Giardia duodenalis, and Enterocytozoon bieneusi in captive wildlife at Zhengzhou Zoo, China. Journal of Eukaryotic Microbiology, 62(6), 833–839. [DOI] [PubMed] [Google Scholar]
- 25. Li N, Xiao L, Wang L, Zhao S, Zhao X, Duan L, Guo M, Liu L, Feng Y. 2012. Molecular surveillance of Cryptosporidium spp., Giardia duodenalis, and Enterocytozoon bieneusi by genotyping and subtyping parasites in wastewater. PLoS Neglected Tropical Diseases, 6(9), e1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li W, Li Y, Song M, Lu Y, Yang J, Tao W, Jiang Y, Wan Q, Zhang S, Xiao L. 2015. Prevalence and genetic characteristics of Cryptosporidium, Enterocytozoon bieneusi and Giardia duodenalis in cats and dogs in Heilongjiang province, China. Veterinary Parasitology, 208(3–4), 125–134. [DOI] [PubMed] [Google Scholar]
- 27. Li W, Deng L, Yu X, Zhong Z, Wang Q, Liu X, Niu L, Xie N, Deng J, Lei S, Wang L, Gong C, Zhou Z, Hu Y, Fu H, Xu H, Geng Y, Peng G. 2016. Multilocus genotypes and broad host-range of Enterocytozoon bieneusi in captive wildlife at zoological gardens in China. Parasites & Vectors, 9(1), 395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li X, Pereira MD, Larsen R, Xiao C, Phillips R, Striby K, McCowan B, Atwill ER. 2015. Cryptosporidium rubeyi n. sp. (Apicomplexa: Cryptosporidiidae) in multiple Spermophilus ground squirrel species, International Journal for Parasitology. Parasites and Wildlife, 4(3), 343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu W, Nie C, Zhang L, Wang R, Liu A, Zhao W, Li H. 2015. First detection and genotyping of Enterocytozoon bieneusi in reindeers (Rangifer tarandus): a zoonotic potential of ITS genotypes. Parasites & Vectors, 8, 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liu X, Zhou X, Zhong Z, Chen W, Deng J, Niu L, Wang Q, Peng G. 2014. New subtype of Cryptosporidium cuniculus isolated from rabbits by sequencing the Gp60 gene. Journal of Parasitology, 100(4), 532–536. [DOI] [PubMed] [Google Scholar]
- 31. Lobo ML, Xiao L, Antunes F, Matos O. 2012. Microsporidia as emerging pathogens and the implication for public health: a 10-year study on HIV-positive and -negative patients. International Journal for Parasitology, 42(2), 197–205. [DOI] [PubMed] [Google Scholar]
- 32. Martínez-Ruiz R, de Lucio A, Fuentes I, Carmena D. 2016. Autochthonous Cryptosporidium cuniculus infection in Spain: first report in a symptomatic paediatric patient from Madrid. Enfermedades Infecciosas y Microbiología Clínica, 34(8), 532–534. [DOI] [PubMed] [Google Scholar]
- 33. Matos O, Lobo ML, Xiao L. 2012. Epidemiology of Enterocytozoon bieneusi infection in Humans. Journal of Parasitology Research, 2012, 981424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Molloy SF, Smith HV, Kirwan P, Nichols RA, Asaolu SO, Connelly L, Holland CV. 2010. Identification of a high diversity of Cryptosporidium species genotypes and subtypes in a pediatric population in Nigeria. The American Journal of Tropical Medicine and Hygiene, 82(4), 608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nolan MJ, Jex AR, Haydon SR, Stevens MA, Gasser RB. 2010. Molecular detection of Cryptosporidium cuniculus in rabbits in Australia. Infection, Genetics and Evolution, 10(8), 1179–1187. [DOI] [PubMed] [Google Scholar]
- 36. Nolan MJ, Jex AR, Koehler AV, Haydon SR, Stevens MA, Gasser RB. 2013. Molecular-based investigation of Cryptosporidium and Giardia from animals in water catchments in southeastern Australia. Water Research, 47(5), 1726–1740. [DOI] [PubMed] [Google Scholar]
- 37. Pirestani M, Sadraei J, Forouzandeh M. 2013. Molecular characterization and genotyping of Human related microsporidia in free-ranging and captive pigeons of Tehran, Iran. Infection, Genetics and Evolution, 20, 495–499. [PubMed] [Google Scholar]
- 38. Qi M, Luo N, Wang H, Yu F, Wang R, Huang J, Zhang L. 2015. Zoonotic Cryptosporidium spp. and Enterocytozoon bieneusi in pet chinchillas (Chinchilla lanigera) in China. Parasitology International, 64(5), 339–341. [DOI] [PubMed] [Google Scholar]
- 39. Reetz J, Rinder H, Thomschke A, Manke H, Schwebs M, Bruderek A. 2002. First detection of the microsporidium Enterocytozoon bieneusi in non-mammalian hosts (chickens). International Journal for Parasitology, 32(7), 785–787. [DOI] [PubMed] [Google Scholar]
- 40. Robinson G, Wright S, Elwin K, Hadfield SJ, Katzer F, Bartley PM, Hunter PR, Nath M, Innes EA, Chalmers RM. 2010. Re-description of Cryptosporidium cuniculus Inman and Takeuchi, 1979 (Apicomplexa: Cryptosporidiidae): morphology, biology and phylogeny. International Journal for Parasitology, 40(13), 1539–1548. [DOI] [PubMed] [Google Scholar]
- 41. Ryan U, Fayer R, Xiao L. 2014. Cryptosporidium species in humans and animals: current understanding and research needs. Parasitology, 141(13), 1667–1685. [DOI] [PubMed] [Google Scholar]
- 42. Ryan U, Paparini A, Tong K, Yang R, Gibson-Kueh S, O’Hara A, Lymbery A, Xiao L. 2015. Cryptosporidium huwi n. sp. (Apicomplexa: Eimeriidae) from the guppy (Poecilia reticulata). Experimental Parasitology, 150, 31–35. [DOI] [PubMed] [Google Scholar]
- 43. Ryan U, Xiao L, Read C, Zhou L, Lal AA, Pavlasek I. 2003. Identification of novel Cryptosporidium genotypes from the Czech Republic. Applied and Environmental Microbiology, 69(7), 4302–4307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Santín M, Fayer R. 2009. Enterocytozoon bieneusi genotype nomenclature based on the internal transcribed spacer sequence: a consensus. Journal of Eukaryotic Microbiology, 56(1), 34–38. [DOI] [PubMed] [Google Scholar]
- 45. Santín M, Fayer R. 2011. Microsporidiosis: Enterocytozoon bieneusi in domesticated and wild animals. Research in Veterinary Science, 90(3), 363–371. [DOI] [PubMed] [Google Scholar]
- 46. Shi K, Jian F, Lv C, Ning C, Zhang L, Ren X, Dearen TK, Li N, Qi M, Xiao L. 2010. Prevalence, genetic characteristics, and zoonotic potential of Cryptosporidium species causing infections in farm rabbits in China. Journal of Clinical Microbiology, 48(9), 3263–3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shiibashi T, Imai T, Sato Y, Abe N, Yukawa M, Nogami S. 2006. Cryptosporidium infection in juvenile pet rabbits. Journal of Veterinary Medical Science, 68(3), 281–282. [DOI] [PubMed] [Google Scholar]
- 48. Sponseller JK, Griffiths JK, Tzipori S. 2014. The evolution of respiratory Cryptosporidiosis: evidence for transmission by inhalation. Clinical Microbiology Reviews, 27(3), 575–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sulaiman IM, Bern C, Gilman R, Cama V, Kawai V, Vargas D, Ticona E, Vivar A, Xiao L. 2003. A molecular biologic study of Enterocytozoon bieneusi in HIV-infected patients in Lima, Peru. Journal of Eukaryotic Microbiology, 50(Suppl), 591–596. [DOI] [PubMed] [Google Scholar]
- 50. Wang L, Xiao L, Duan L, Ye J, Guo Y, Guo M, Liu L, Feng Y. 2013. Concurrent infections of Giardia duodenalis, Enterocytozoon bieneusi, and Clostridium difficile in children during a cryptosporidiosis outbreak in a pediatric hospital in China. PLoS Neglected Tropical Diseases, 7(9), e2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang L, Zhang H, Zhao X, Zhang L, Zhang G, Guo M, Liu L, Feng Y, Xiao L. 2013. Zoonotic Cryptosporidium species and Enterocytozoon bieneusi genotypes in HIV-positive patients on antiretroviral therapy. Journal of Clinical Microbiology, 51(2), 557–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Xiao L, Morgan UM, Limor J, Escalante A, Arrowood M, Shulaw W, Thompson RC, Fayer R, Lal AA. 1999. Genetic diversity within Cryptosporidium parvum and related Cryptosporidium species. Applied and Environmental Microbiology, 65(8), 3386–3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Yang J, Song M, Wan Q, Li Y, Lu Y, Jiang Y, Tao W, Li W. 2014. Enterocytozoon bieneusi genotypes in children in Northeast China and assessment of risk of zoonotic transmission. Journal of Clinical Microbiology, 52(12), 4363–4367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ye J, Xiao L, Ma J, Guo M, Liu L, Feng Y. 2012. Anthroponotic enteric parasites in monkeys in public park, China. Emerging Infectious Diseases, 18(10), 1640–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhang W, Shen Y, Wang R, Liu A, Ling H, Li Y, Cao J, Zhang X, Shu J, Zhang L. 2012. Cryptosporidium cuniculus and Giardia duodenalis in rabbits: genetic diversity and possible zoonotic transmission. PLoS One, 7(2), e31262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang X, Wang Z, Su Y, Liang X, Sun X, Peng S, Lu H, Jiang N, Yin J, Xiang M, Chen Q. 2011. Identification and genotyping of Enterocytozoon bieneusi in China. Journal of Clinical Microbiology, 49(5), 2006–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zhang XX, Jiang J, Cai YN, Wang CF, Xu P, Yang GL, Zhao Q. 2016. Molecular characterization of Enterocytozoon bieneusi in domestic rabbits (Oryctolagus cuniculus) in Northeastern China. The Korean Journal of Parasitology, 54(1), 81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zhang Z, Huang J, Karim MR, Zhao J, Dong H, Ai W, Li F, Zhang L, Wang R. 2015. Zoonotic Enterocytozoon bieneusi genotypes in Père David’s deer (Elaphurus davidianus) in Henan, China. Experimental Parasitology, 155, 46–48. [DOI] [PubMed] [Google Scholar]
- 59. Zhao GH, Du SZ, Wang HB, Hu XF, Deng MJ, Yu SK, Zhang LX, Zhu XQ. 2015. First report of zoonotic Cryptosporidium spp., Giardia intestinalis and Enterocytozoon bieneusi in golden takins (Budorcas taxicolor bedfordi). Infection, Genetics and Evolution, 34, 394–401. [DOI] [PubMed] [Google Scholar]
- 60. Zhao W, Zhang W, Yang F, Cao J, Liu H, Yang D, Shen Y, Liu A. 2014. High prevalence of Enterocytozoon bieneusi in asymptomatic pigs and assessment of zoonotic risk at the genotype level. Applied and Environmental Microbiology, 80(12), 3699–3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhao W, Zhang W, Yang Z, Liu A, Zhang L, Yang F, Wang R, Ling H. 2015. Correction: Genotyping of Enterocytozoon bieneusi in Farmed Blue Foxes (Alopex lagopus) and Raccoon Dogs (Nyctereutes procyonoides) in China. PLoS One, 10(11), e0143992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Zhao W, Zhang W, Yang D, Zhang L, Wang R, Liu A. 2015. Prevalence of Enterocytozoon bieneusi and genetic diversity of ITS genotypes in sheep and goats in China. Infection, Genetics and Evolution, 32, 265–270. [DOI] [PubMed] [Google Scholar]
- 63. Zhao W, Yu S, Yang Z, Zhang Y, Zhang L, Wang R, Zhang W, Yang F, Liu A. 2016. Genotyping of Enterocytozoon bieneusi (Microsporidia) isolated from various birds in China. Infection, Genetics and Evolution, 40, 151–154. [DOI] [PubMed] [Google Scholar]