Abstract
Laparoscopic right hemicolectomy with extracorporeal anastomosis is a widely used procedure; several authors have published their approach to intracorporeal anastomosis. In this paper, we present an approach developed by us and compare short-term outcomes with those of extracorporeal anastomosis in colon cancer patients.
Retrospective review of colon cancer patients treated with laparoscopic right hemicolectomy either with intracorporeal anastomosis (TLG group) or extracorporeal anastomosis (LG group) at the Zhangjiagang Hospital Affiliated to Soochow University between January 2011 and October 2015. Operative and postoperative data are compared.
Around 85 patients underwent laparoscopic hemicolectomy (56 TLG and 29 LG) during the reference period for this study. Age, gender, body mass index (BMI), stage of cancer, operation time, number of lymph nodes harvested, and length of hospital stay were comparable between the 2 groups. In the TLG group, the ileocolic anastomosis time was significantly shorter (9.9–15.5 minutes vs 13.5–18.2 minutes in LG; P < 0.001), the mean intraoperative blood loss was lower (83.2 mL [range, 56.5–100.5 mL] vs 93.3 mL [range, 75.8 – 110.3 mL]; P < 0.001), the recovery of bowel function was faster (P < 0.001), and the postoperative pain score was lower (P < 0.001) as compared to that in the LG group. Complications in the LG group included wound infection (4 patients), obstruction (1), and postoperative bleeding complications (1); however, only 1 patient developed complication (wound infection) in the TLG group.
Total laparoscopic right hemicolectomy with 3-step stapled intracorporeal anastomosis for colon cancer is a safe and reliable procedure. Its advantages include short anastomosis time, less intraoperative blood loss, less postoperative pain, and early bowel function recovery.
Keywords: 3-step ileocolic anastomosis, colon cancer, total laparoscopy
1. Introduction
Laparoscopic surgery has gained wide acceptance and has been increasingly performed over the years. The first case of laparoscopic right hemicolectomy for colon cancer was reported in 1991.[1] Benefits of laparoscopic surgery over open surgery for colon cancer are well documented. These include less blood loss, lower perioperative morbidity, lower incidence of wound infection and incision hernia, less postoperative pain, early recovery of bowel function, shorter hospital stay, earlier return to work, and comparable survival.[2–4] Despite these advantages, laparoscopic colectomy is technically challenging and warrants intensive structured training to minimize conversion to open surgery and associated complications.[5]
Several variations of the procedure have been described.[6,7] Among these, ileocolic anastomosis is one of the most essential steps of the operation, which is performed using an extracorporeal or intracorporeal approach. The extracorporeal anastomotic technique is similar to that performed during open surgery and is utilized more frequently.[8,9] It requires greater mobilization and exteriorization of the bowel through the abdominal incision for further steps. Hence, the intracorporeal anastomosis is a suitable alternative that allows completion of the anastomosis without any externalization of the bowel. However, this technique limits the ability to choose an extraction site, which is usually a small midline incision. In addition, problems with intestinal alignment after extraction are known to occur. The first report of total laparoscopic right hemicolectomy with intracorporeal anastomosis was published in 2003.[10] A recent review of laparoscopic right hemicolectomies performed with either intracorporeal or extracorporeal anastomoses demonstrated comparable outcomes in terms of incidence of anastomotic leaks, overall postoperative morbidity, and 30-day postoperative mortality.[11] Intracorporeal anastomosis has been shown to reduce wound-related complications, facilitate early restoration of bowel function, and improve cosmesis.[12,13] However, definitive evidence on the effect of the type of anastomosis on short-term outcomes of right hemicolectomy, especially with respect to anastomotic leaks and short-term morbidity, is still awaited.[14–17]
Total laparoscopic right hemicolectomy is being routinely performed at our center for treatment of both benign and neoplastic conditions since several years. We carried out hemicolectomy with a 3-step stapled intracorporeal isoperistalic ileocolic anastomosis in 56 colon cancer cases with good short-term outcomes. Herein, we present our approach and compare the short-term outcomes with those of extracorporeal fashion in a Chinese population. We aim to provide valuable information to this field for better clinical practice.
2. Methods
2.1. Patients
We retrospectively reviewed the medical records of 85 patients who underwent total laparoscopic right hemicolectomy with use of either 3-step isoperistalic intracorporeal anastomosis or laparoscopic assisted right hemicolectomy with extracorporeal anastomosis performed at our department between January 2011 and October 2015. Written informed consent was obtained from all patients. In addition to routine investigations, computed tomography (CT) of chest, abdomen and pelvis, positron emission tomography-computed tomography (PET-CT), and colonoscopy was performed in all patients as part of preoperative work-up.
Patients who had cancer of ileocecum, ascending colon, or hepatic flexure of colon in the absence of invasion of the serous layer or metastases were included in the analysis. Patients with prior history of abdominal surgery, previous malignancy or those who had psychiatric disorders or severe organ dysfunction such as severe cardiopulmonary disorders were excluded.
Patient demographics, preoperative and operative data, and outcomes were included in the analysis. Key variables of interest included age, sex, body mass index (BMI), preoperative diagnosis, duration of surgery, duration of ileocolic anastomosis, intraoperative blood loss, total length of hospital stay, postoperative duration of intestinal function recovery, postoperative pain, and incidence of postoperative in-hospital complications (infection, obstruction, and bleeding). Pathological data, including tumor-node-metastasis (TNM) stage and the number of nodes dissected, were also reviewed. All pathological data fell into the category of T1–3NxM0. The pain evaluation method was as described elsewhere.[18]
2.2. Ethics
This study was approved by the Ethics Committee at the Zhangjiagang Hospital Affiliated to Soochow University. Written informed consent was obtained from each participant.
2.3. Surgical technique
Preoperative bowel preparation, intravenous antibiotics, and nutritional status monitoring was performed in all patients. Patients were administered general anesthesia and placed in supine position. The surgeon and the second assistant surgeon who held the camera stood on the left side of the patient, the first assistant surgeon stood on the right side of the patient. Pneumoperitoneum was set up by use of the Veress needle at the umbilicus and the abdomen insufflated with carbon dioxide (CO2) gas to a pressure of 14 mm Hg. A 10 mm Trocar was placed 3 cm below the umbilicus for visualization, and a 12 mm Trocar inserted under the lower rib margin on the left middle axillary line to serve as the main working port. After adequate insufflation and trocar placement, the abdomen was inspected for any obvious metastatic lesions or any other abnormality. The ileocolic vessels were identified and elevated, and the peritoneum was incised laterally to the ileocolic vessels and superior mesenteric vein. Ileocolic vessels and the right colic vessels were dissected and ligated at the vascular pedicles. The retroperitoneal plane was further developed in Toldt's space using a medial-to-lateral and inferior-to-superior approach, passing duodenum and pancreas anteriorly and ascending colon and transverse colon posteriorly. The colic branch of the gastrocolic vessels was also ligated during dissection. The right lateral peritoneum was then incised, and the terminal ileum and ascending colon were completely mobilized. Once the right colon was fully mobilized along the lateral attachments, the hepatic flexure was mobilized via dissection and division of hepatocolic ligament and greater omentum. The intra-mesenteric lymphatic tissue was simultaneously removed when mobilization of the right mesocolon was completed.
Next step was ileocolic anastomosis. For laparoscopic assisted right hemicolectomy with extracorporeal anastomosis group (LG), a midline supraumbilical 4 to 8 cm incision was made for bowel extraction. The terminal ileum and right hemicolon were resected, and a side-to-side stapled anastamosis performed. After completion of the anastomosis, the fascia at the extraction site was closed and reinspection of the peritoneal cavity was carried out. The drainage tube was routinely placed in the right upper quadrant.
In patients undergoing total laparoscopic right hemicolectomy with isoperistalic stapled intracorporeal anastomosis, ileal mesentery and mesocolon were fully liberated using an ultrasound knife to reach the target resection margin prior to anastomosis. The anastomosis was a 3-step procedure. First, a linear cutting stapler (PSE60A, Johnson & Johnson, Inc., New Brunswick, New Jersey, USA) was used to divide the transverse colon (Fig. 1A). In the second step, the ileum and transverse colon were aligned in parallel in an isoperistaltic pattern. An anterior wall colostomy was made 10 cm distal to the transected transverse colon and an enterotomy with 1 cm incision was performed on the ileum. Two jaws of the endoscopic stapler were then inserted into the bowels respectively. The stapler was fired and withdrawn, and a side-to-side anastomosis created (Fig. 1B). In the third step, the common enterotomy was closed with the stapler and the terminal ileum finally divided for completion of the 3-step anastomosis (Fig. 1C). The drainage tubes were positioned after specimen bagging and extraction, and total laparoscopic right hemicolectomy with 3-step intracorporeal isoperistalic ileocolic anastomosis was completed (Fig. 1D).
Figure 1.
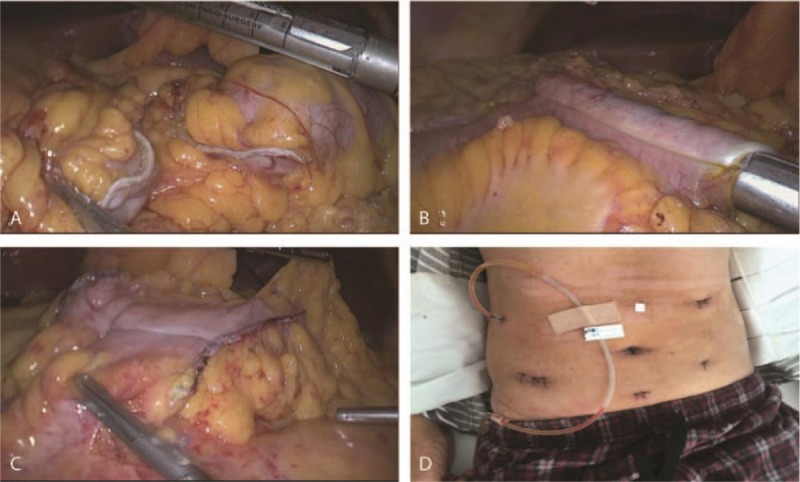
(A) A linear cutting stapler (PSE60A, Johnson & Johnson) was utilized to divide the transverse colon; (B) the ileum and transverse colon were aligned in parallel in an isoperistaltic pattern. A colostomy and an enterotomy were performed, respectively. The stapler was inserted, fired, and withdrawn, and a side-to-side anastomosis established; (C) the common enterotomy was closed with the stapler and the terminal ileum divided; (D) drainage tubes were applied as per need after specimen bagging and extraction.
2.4. Statistical analyses
Statistical analyses were performed using Graphpad software Prism6 (GraphPad Software, Inc., San Diego, CA, USA). Quantitative variables are expressed as mean ± standard error of the mean (SEM) or mean ± standard deviation (SD); between-group differences were assessed using a 2-tailed, unpaired Student t test. Categorical variables are analyzed using the Pearson χ2 or Fisher exact test. Statistical significance was defined as a P value <0.05.
3. Results
3.1. Demographics
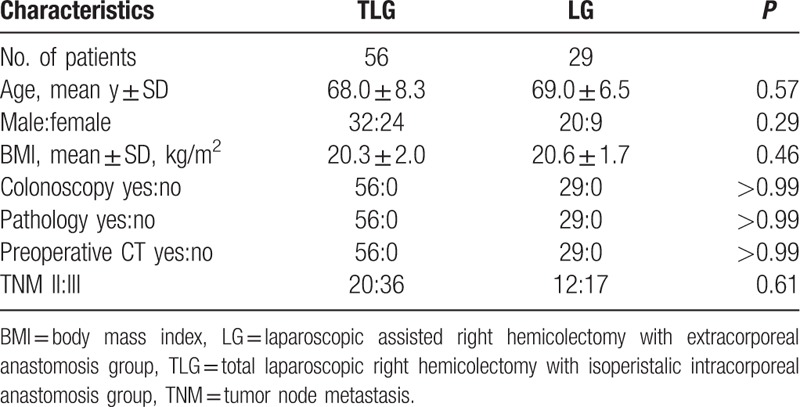
A total of 85 (52 men and 33 women) patients had undergone laparoscopic right hemicolectomy between January 2011 and October 2015; 56 patients underwent total laparoscopic right hemicolectomy with 3-step isoperistalic stapled intracorporeal anastomosis (referred to as TLG), whereas 29 patients underwent laparoscopic assisted right hemicolectomy with extracorporeal anastomosis (LG). All 85 patients had undergone preoperative colonoscopy, CT, and/or PET-CT and had definite pathology reports. No significant between-group difference was observed with respect to baseline characteristics such as mean age, gender, BMI, and TNM stage (Table 1).
Table 1.
Patient demographic and baseline characteristics.
3.2. Surgical parameters
There were no significant differences between the 2 groups with respect to the operation time, number of lymph node clearance, and total length of hospital stay (P = 0.42, P = 0.54, P = 0.29, respectively; Table 2). In the TLG group, the mean duration of ileocolic anastomosis was shorter (13.06 ± 0.182 minutes [range 9.9–15.5 minutes] vs 15.59 ± 0.238 minutes [range 13.5–18.2 minutes]; P < 0.001) and the mean intraoperative blood loss lower (83.21 mL [range 56.5–100.5 mL] vs 93.39 mL [range 75.8–110.3 mL] than that in the LG group. Although the operation time was similar in the 2 groups, there was a statistically significant shorter time to intestinal function recovery with the 3-step intracorporeal anastomosis (P < 0.001). Moreover, patients in the TLG group had significantly decreased postoperative pain scores (P < 0.001 vs LG group) (Table 2 and Fig. 2).
Table 2.
Comparison of surgical data between the 2 groups.
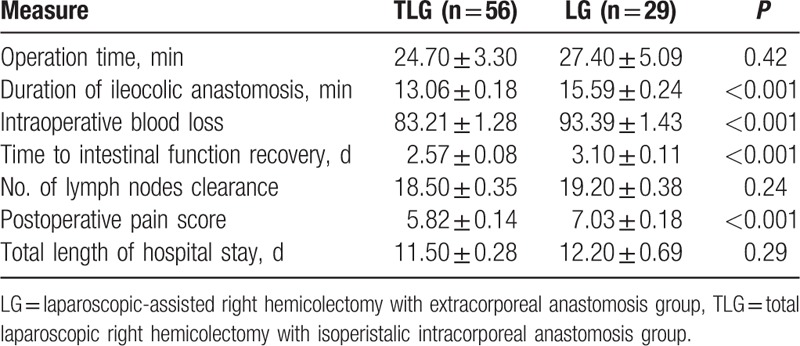
Figure 2.
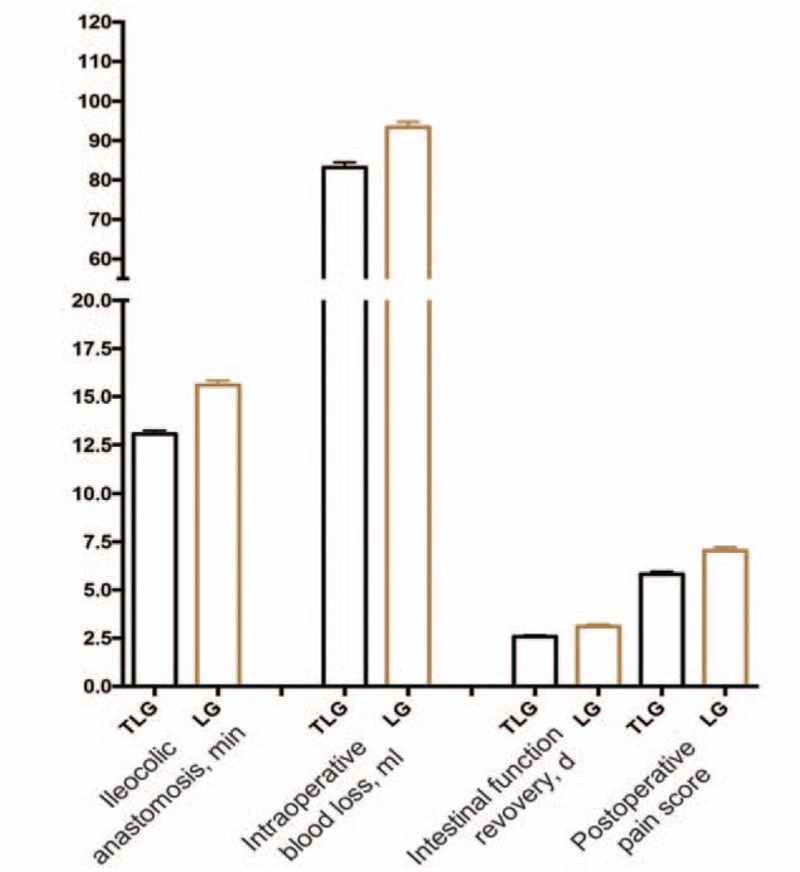
A comparison of the operative and postoperative data. The errors bars represent the standard error of the mean (SEM). SEM = standard error of the mean.
3.3. Complications
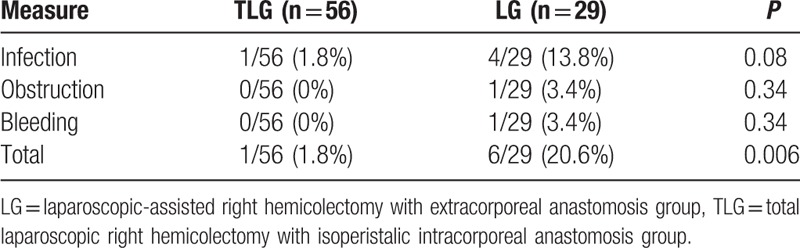
Postoperative complications in LG were: wound infection (13.8%; N = 4), bowel obstruction (3.4%; N = 1), and postoperative bleeding (3.4%; N = 1). All these complications were treated promptly and resolved with supportive medication or secondary surgical interventions. Only 1 case developed wound infection in the TLG group. There was no obvious difference in each subtype of complications between the groups. (Table 3) However, the overall complication rate was significantly lower in the TLG group as compared to that in the LG group (P = 0.006).
Table 3.
Comparison of postoperative complications of the 2 groups.
None of the patients in the study required conversion to open surgery during laparoscopic surgery. No anatomical bowel leakage, hernia, or severe organ dysfunction such as cardiopulmonary disorders occurred after surgery. There was no mortality in either group.
4. Discussion
Numerous reports have demonstrated that laparoscopy outweighs open operation in terms of postoperative pain, recovery, morbidity, length of hospital stay, and cosmesis.[19,20] Though seemingly challenging, laparoscopic right hemicolectomy has developed considerably in the past 20 years. In 2004, Senagore et al[9] described their operative technique for laparoscopic right hemicolectomy which involved intracorporeal mobilization of colon and vessel ligation, whereas bowel resection and anastomosis were performed extracorporeally. The technique required a larger abdominal incision and exteriorization of the bowel to create adequate tension-free environment for ileocolic anastomosis. However, the mesentery is liable to be heavily twisted in this process thereby increasing the risk for potential anastomotic leak and longer period for bowel function recovery.[21] The procedure is risky in patients with a short mesentery.
Total laparoscopic right hemicolectomy with intracorporeal anastomosis was developed to overcome these limitations.[10] This technique has gradually gained recognition and popularity in the past 10 years. Moreover, the technique is feasible and safe even in obese patients.[22] In 2008, Bergamaschi et al[23] described their operative technique with intracorporeal anastomosis, in which all steps were performed intracorporeally, but the anastomosis was hand-sewn. Neutzling et al[24] demonstrated several inherent advantages of the stapler approach over handsewn techniques in colorectal anastomosis surgery, regardless of the level of anastomosis. In 2010, Ho reported his own experience of total laparoscopic right hemicolectomy with stapled intracorporeal ileocolic anastomosis.[7] His approach still requires intracorporeal suturing as stay stitches for the sake of safe stapler application. Recently, robotic intracorporeal ileocolic anastomosis has been reported with high cost being the main disadvantage.[25]
In this article, we present our approach to total laparoscopic right hemicolectomy with stapled intracorporeal anastomosis for colon cancer. A total of 56 patients (TLG group) underwent this procedure over a period of 4 years with optimal outcomes.
The procedure was performed in a medial-to-lateral fashion. After adequate mobilization of terminal ileum and right colon and vessel ligations, the stapled ileocolic anastomosis technique consists of following 3 steps: first, the transverse colon is divided by a linear cutting stapler (PSE60A, Johnson & Johnson) (Fig. 1A). Second, the ileum and transverse colon are aligned in parallel in an isoperistaltic pattern to create a side-to-side stapled anastomosis (Fig. 1B). Third, the common enterotomy was closed with the stapler and the terminal ileum was finally divided for completion of the 3-step anastomosis (Fig. 1C). Our approach is similar to that of Ho in general but is much simpler and convenient to perform. Since we aligned the terminal ileum and transverse colon in an isoperistaltic manner, the anastomosis was close to normal physiological conditions.
No significant differences were observed between the 2 groups with respect to operation time, number of lymph node clearance, and total length of hospital stay. However, with the help of stapler, the duration of the ileocolic anastomosis was significantly shorter in the TLG group. Many factors could affect the duration of the anastomotic procedure including the patient's BMI, surgeon's skills, and the procedure itself among others. In this study, there was no significant difference between the 2 groups with respect to BMI and surgeon's skills. Therefore, it is likely that the proposed 3-step method itself was technically easier and more feasible. The time spent making the midline incision for bowel extraction, locating the resection sites, and immobilizing the bowels for performing anastomosis in the LG group was spared in the 3-step approach. In line with previous reports,[16] the intraoperative blood loss was less, and bowel function recovery was faster. Postoperative recovery of bowel function recovery is associated with operation time, use of anesthetics, bowel exposure time, and surgical trauma. Obviously, bowel function recovery would be faster in TLG because of short exposure time during operation and less surgical trauma. Moreover, these patients complained less postoperative pain than patients in the LG group. No major complications such as anatomical bowel leakage, hernia, or severe organ dysfunction occurred in both groups. However, the 3-step technique was associated with a lower overall postoperative complication rate.
Our analysis suggests that the total laparoscopic right hemicolectomy with stapled 3-step anastomosis technique is safe to perform and better than hemicolectomy with extracorporeal anastomosis in several aspects. Although we only assessed the use of this technique in colon cancer patients, the technique should be suitable for inflammatory bowel disease, arteriovenous malformations, obstruction, Crohn's disease (and complications), ischemia, and any other condition that requires intestinal resection with appropriate modifications.[26]
We chose colon cancer patients as our study population; therefore, it is critical to review the preoperative planning, colonoscopy report and CT scans judiciously to localize the tumor precisely. Other than tattooing of the lesion with India ink prior to surgery,[27] we routinely place 3 titanium clips to serve as landmarks adjacent to the tumor during colonoscopy examination and biopsy for better tumor localization during surgery. This not only helps avoid inadvertent mishandling of the tumor mass but also ensures that no tumor lesion is missed.
Intraoperative bleeding is a potential complication of total laparoscopic right hemicolectomy procedure. Therefore, unnecessary traction should be avoided and the middle colic vessels taken good care of. Prior to bowel resection, the terminal ileum and colon requires appropriate mobilization, which requires good anatomical orientation of the surgeon so as not to injure duodenum and other organs. When closing the common enterotomy, we recommend the stapler be bent to a 90-degree angle to prevent anastomotic stricture or anastomotic insufficiency. According to the most recent follow up data, there was no evidence of stricture formation at the site of the last stapler, though in some patients the follow up duration is less than 1 year.
In conclusion, we found total laparoscopic right hemicolectomy with 3-step stapled intracorporeal anastomosis for colon cancer to be a safe, reliable, and convenient procedure that offers benefits of short anastomosis time, less surgical trauma, flexibility in the selection of specimen extraction site, less postoperative pain, and earlier bowel recovery. We believe that this technique should be considered by every laparoscopic surgeon.
Footnotes
Abbreviations: BMI = body mass index, CO2 = carbon dioxide, CT = computed tomography, LG = laparoscopic-assisted right hemicolectomy with extracorporeal anastomosis group, PET-CT = positron emission tomography-computed tomography, SD = standard deviation, SEM = standard error of the mean, TLG = total laparoscopic right hemicolectomy with isoperistalic intracorporeal anastomosis group, TNM = tumor-node-metastasis.
J-CT and S-SW contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1991;1:144–50. [PubMed] [Google Scholar]
- [2].Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet (London, England) 2002;359:2224–9. [DOI] [PubMed] [Google Scholar]
- [3].Buunen M, Veldkamp R, Hop WC, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 2009;10:44–52. [DOI] [PubMed] [Google Scholar]
- [4].Veldkamp R, Kuhry E, Hop WC, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 2005;6:477–84. [DOI] [PubMed] [Google Scholar]
- [5].Stein S, Stulberg J, Champagne B. Learning laparoscopic colectomy during colorectal residency: what does it take and how are we doing? Surg Endosc 2012;26:488–92. [DOI] [PubMed] [Google Scholar]
- [6].Bergamaschi R. Laparoscopic right hemicolectomy with intracorporeal anastomosis: letter to the “How I do it” article by Y.-H. Ho. Tech Coloproctol 2010;14:359–63. Techniques in coloproctology 2011; 15(3): 359-360. [DOI] [PubMed] [Google Scholar]
- [7].Ho YH. Laparoscopic right hemicolectomy with intracorporeal anastomosis. Tech Coloproctol 2010;14:359–63. [DOI] [PubMed] [Google Scholar]
- [8].Young-Fadok TM, Nelson H. Laparoscopic right colectomy: five-step procedure. Dis Colon Rectum 2000;43:267–71. [DOI] [PubMed] [Google Scholar]
- [9].Senagore AJ, Delaney CP, Brady KM, et al. Standardized approach to laparoscopic right colectomy: outcomes in 70 consecutive cases. J Am Coll Surg 2004;199:675–9. [DOI] [PubMed] [Google Scholar]
- [10].Casciola L, Ceccarelli G, Di Zitti L, et al. Laparoscopic right hemicolectomy with intracorporeal anastomosis. Technical aspects and personal experience. Minerva Chirurgica 2003;58:621–7. [PubMed] [Google Scholar]
- [11].Cirocchi R, Trastulli S, Farinella E, et al. Intracorporeal versus extracorporeal anastomosis during laparoscopic right hemicolectomy — systematic review and meta-analysis. Surg Oncol 2013;22:1–3. [DOI] [PubMed] [Google Scholar]
- [12].Pascual M, Salvans S, Pera M. Laparoscopic colorectal surgery: current status and implementation of the latest technological innovations. World J Gastroenterol 2016;22:704–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Milone M, Elmore U, Di Salvo E, et al. Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 2015;29:2314–20. [DOI] [PubMed] [Google Scholar]
- [14].Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS 2009;13:312–7. [PMC free article] [PubMed] [Google Scholar]
- [15].Grams J, Tong W, Greenstein AJ, et al. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc 2010;24:1886–91. [DOI] [PubMed] [Google Scholar]
- [16].Scatizzi M, Kroning KC, Borrelli A, et al. Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg 2010;34:2902–8. [DOI] [PubMed] [Google Scholar]
- [17].Carnuccio P, Jimeno J, Pares D. Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol 2014;18:5–12. [DOI] [PubMed] [Google Scholar]
- [18].Jian-Cheng T, Bo Z, Jian F, et al. Delta-shaped gastroduodenostomy in fully laparoscopic distal gastrectomy: a retrospective study. Medicine 2015;94:e1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kavanagh DO, Gibson D, Moran DC, et al. Short-term outcomes following laparoscopic resection for colon cancer. Int J Colorectal Dis 2011;26:361–8. [DOI] [PubMed] [Google Scholar]
- [20].Tan WS, Chew MH, Lim IA, et al. Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis 2012;27:773–80. [DOI] [PubMed] [Google Scholar]
- [21].Feroci F, Lenzi E, Kroning KC, et al. Feasibility and effectiveness of laparoscopic right colectomy with extracorporeal anastomosis. Minerva Chirurgica 2011;66:41–8. [PubMed] [Google Scholar]
- [22].Blumberg D. Laparoscopic colectomy performed using a completely intracorporeal technique is associated with similar outcome in obese and thin patients. Surg Laparosc Endosc Percutaneous Tech 2009;19:57–61. [DOI] [PubMed] [Google Scholar]
- [23].Bergamaschi R, Schochet E, Haughn C, et al. Standardized laparoscopic intracorporeal right colectomy for cancer: short-term outcome in 111 unselected patients. Dis Colon Rectum 2008;51:1350–5. [DOI] [PubMed] [Google Scholar]
- [24].Neutzling CB, Lustosa SA, Proenca IM, et al. Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev 2012;2: CD003144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Morpurgo E, Contardo T, Molaro R, et al. Robotic-assisted intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech A 2013;23:414–7. [DOI] [PubMed] [Google Scholar]
- [26].Maartense S, Dunker MS, Slors JF, et al. Laparoscopic-assisted versus open ileocolic resection for Crohn's disease: a randomized trial. Ann Surg 2006;243:143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Arteaga-Gonzalez I, Martin-Malagon A, Fernandez EM, et al. The use of preoperative endoscopic tattooing in laparoscopic colorectal cancer surgery for endoscopically advanced tumors: a prospective comparative clinical study. World J Surg 2006;30:605–11. [DOI] [PubMed] [Google Scholar]


