Supplemental Digital Content is available in the text
Keywords: community-health-center–based intervention, hypertension, stroke, total death
Abstract
Background:
It is not fully clear whether the effect of short-term management in community can reduce the long-term risk of stroke
Objectives:
To evaluate whether short-term hypertension management is associated with long-term incidence of stroke and total death in community health centers in China.
Design:
Community controlled trail.
Participants:
Six community health centers (4 active, 2 control) in China, patients with hypertension.
Control arm:
Patients were treated with normally therapy method.
Active arm:
Patients were treated oriented by the Guideline for hypertension management.
Randomization:
Two centers (Hebei and Zhejiang) from the Hypertension Control in Community (HCC) Project, which was conducted from 2005 to 2008, were randomly selected for this study. Four thousand hypertensive patients from these centers, who were under management for one year in the baseline, were followed up in 2013. The electronic health record system (2005–2008) was used to identify 2000 hypertensive patients, who were not included in HCC but lived in comparable community health center in the same province, as the control group. All baseline and follow-up data were collected using standardized questionnaires for stroke outcomes.
Main outcome measures:
Stroke.
Results:
Of the 6000 participants, 3787 (63.1%) were eligible for analysis. At the time of follow-up, the average BP was kept in the lower level than that in baseline, and the control rate was 59.3%. After propensity-score matching, 110 strokes (2.0% vs 4.6%) and 141 deaths (1.4% vs 3.8%) were noted in the matched intervention and control groups (1078 pairs), respectively. Patients in the intervention group were less likely to experience a stroke or die than those in the control group (hazard ratio [HR] = 0.40, 95% confidence interval [CI]: 0.26–0.62, P < 0.01; HR = 0.50, 95% CI: 0.35–0.72, P < 0.01). The sensitivity analysis showed similar results.
Conclusions:
Short-term management of hypertension had a positive effect on the long-term risk reduction of death and stroke in hypertensive patients.
1. Introduction
Hypertension is the leading risk factor for cardiovascular disease,[1] associated with increased risk of coronary heart disease, stroke[2–4] and accounts for about 7.6 million deaths per year worldwide.[4] Currently, hypertension is most prevalent in the United states (29.0%),[5] Brazil (21%),[6] Turkey(30.3%),[7] and Arab countries (29.5%).[8] But only about half of the patients were under control in the United States[5] and Turkey.[7] Hypertension is also a common disease in China (26.7%),[9] affecting over 200 million patients alone,[10] but the control rate was only 11.2%.[9] It is the most important risk factor for premature death and stroke in China.[11,12] Stroke is the leading cause of adult disability in China,[13] and places a significant socioeconomic burden on patients and the health system.[11]
Effective blood pressure (BP) control significantly reduces the risk of stroke and death.[14–17] A recent meta-analysis by Sundström et al[16,18] showed that antihypertensive drugs reduce the incidence of stroke and death in patients with uncomplicated grade 1 hypertension. It was reported that BP reduction with short-term antihypertensive drugs treatment has long-term protective effects on target organs.[19,20] Although antihypertensive agents are the most effective agent to reduce BP level, behavioral intervention and self-care all are helpful to lower the BP.[21–23] However, few studies have evaluated the effect of short-term management of hypertension on the long-term incidence of stroke and total death in community health centers. The Hypertension Control in Communities (HCC) Project, described previously,[24] initiated intervention studies in community health centers (CHCs) across China between 2005 and 2010 to determine the effect of one-year, guideline-oriented management of hypertension at the community level. The control of hypertension in the community improved significantly after one year.[25] The present study was conducted to determine whether 1-year hypertension management is associated with an incidence of stroke or total death after the HCC Project ended more than 5 years ago.
2. Methods
One thousand CHCs across China were selected for the project between 2005 and 2010. Hypertensive patients were managed for at least 1 year by CHC doctors who were trained by the Chinese Guidelines for Hypertension Prevention and Control.[26] The protocol, which was based on the guidelines, was as follows: classification of hypertension, stratification of global risk, health education, lifestyle changes, and drug titration. Lifestyle changes included smoking cessation, moderation in drinking, exercise, weight loss, and reduction of salt and fat intake. All drugs were prescribed according to the doctors’ choices. The patients were followed up by the community doctors every 1, 2, or 3 months based on the risk stratification in the clinic (Supplementary Fig. S1).
This project was approved by the Fuwai Hospital and sub-centers’ Ethics Review Boards. All participants provided written informed consent.
2.1. Study population
Patients aged 18 to 79 years with hypertension diagnosed by the local hospital and who met the inclusion criteria by measuring BPs again before recruiting, were included in this study. Patients with any of the following were excluded: secondary hypertension; acute coronary syndrome or stroke less than 3 months ago; psychiatric illness; hearing difficulty; physical incapacitation; uncooperative behavior; or life expectancy of less than 1 year.
Two CHCs from the project were randomly selected from Hebei and Zhejiang (subcenters of the HCC project) and 4000 hypertensive patients, who were managed during 2005 to 2008, were followed up in 2013. An additional 2000 hypertensive patients were retrospectively selected as controls from the electronic health record systems (2005–2008) of the CHCs, which were not a part of the HCC program but had comparability in the economic development level and geographical position, in Hebei and Zhejiang as a control group (Supplementary Fig. S2). Baseline and follow-up data for the control and intervention groups was collected using standardized questionnaires in 2013.
2.2. Blood pressure measurement
BP was measured by trained doctors in clinics at each visit using a mercury sphygmomanometer with a cuff of appropriate size. The pressure at which the first Korotkoff sound appeared was taken as the systolic BP, and the pressure at which the Korotkoff sounds disappeared (fifth phase) was taken as the diastolic BP. The sitting BP was measured twice at 1-minute intervals and once after the patient had remained seated for 5 minutes.
2.3. Definitions
Hypertension was defined as a systolic BP of 140 mmHg or more, diastolic BP or 90 mmHg or more, or use of an antihypertensive drug. Smoking was defined as the use of at least one cigarette per day. Drinking was defined as consumption of at least 1 alcoholic beverage per week. Diabetes, myocardial infarction, angina, and stroke were self-reported at baseline; death and stroke information were collected using standardized case report forms. All suspected strokes were confirmed by an independent endpoint committee blinded to the study.
2.4. Statistical analysis
Descriptive data are presented as means (standard deviation) and proportions. Chi-squared tests and 2-tailed Student t tests were used to compare the baseline characteristics of the 2 groups.
Patients in the intervention group were matched with those in the control group to reduce bias using a 1:1 ratio with propensity scores. The propensity score for each patient was defined as the probability of experiencing stroke, death, or both using baseline data, such as age, gender, body mass index, smoking status, drinking status, systolic and diastolic BP, diabetes, and history of cardiovascular events. The patients were matched using 5:1 digit matching. The success of propensity scores in reducing bias was assessed by comparing the covariates between groups.
The difference in survival between the groups was assessed using the Kaplan–Meier method and log-rank test. Cox proportional hazards regression models were used to compare time to stroke or death for intervention versus control groups with hazard ratios (HRs) and 95% confidence intervals (CIs). Data was adjusted for age, gender, body mass index, smoking, drinking, systolic, and diastolic BP, diabetes, and history of cardiovascular disease.
Sensitivity analysis was performed to assess the robustness of results. Cox models were used after excluding 161 patients with cardiovascular diseases at baseline and 14 patients with stroke or death in the first year.
P values below 0.05 were considered statistically significant. Data was analyzed using the SAS software, version 9.2 (SAS Institute Inc., Cary, NC).
3. Results
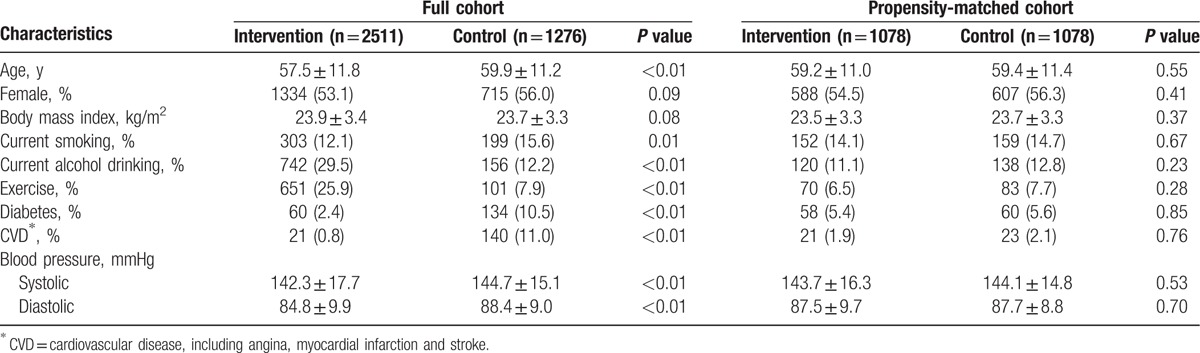
Of the 6000 study participants, 3787 (63.1%) were eligible for analyses: 2511 in the intervention and 1276 in the control group. The average BP was 142.3/84.8 mmHg in the intervention group and 144.7/88.4 mmHg in the control group (P < 0.01). There were significant differences in cardiovascular risk factors between the 2 groups. After propensity score matching, there were 1078 participants in each group, and the characteristics of the participants in both groups were similar (P > 0.05, Table 1).
Table 1.
Characteristics of the patients at baseline.
In the intervention group, the average BP reduction was 11.5/4.7 mmHg after 1 year of management, whereby the control rate reached near 65%. At the time of follow-up, the average BP was kept lower than that in baseline, and the control rate was 59.3% (Fig. 1).
Figure 1.
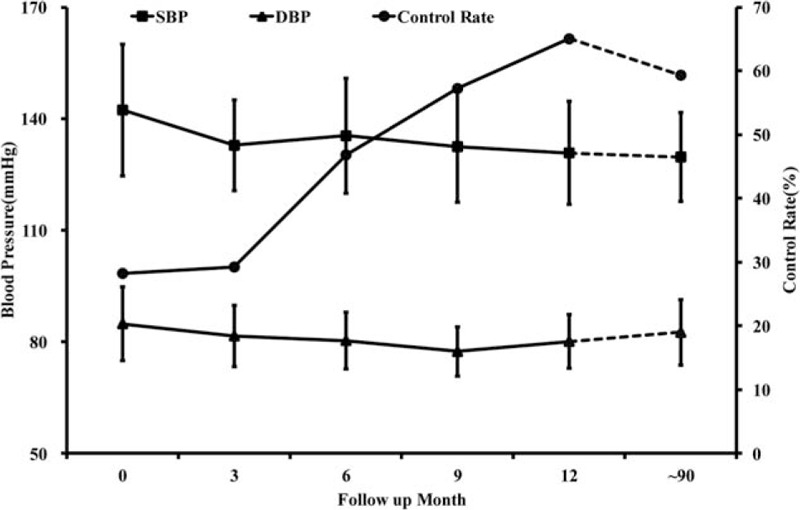
Average level of blood pressure and the control rate for patients under management. DBP = diastolic blood pressure, SBP = systolic blood pressure.
Patients in the intervention group were significantly less likely to have a stroke (1.9% vs 2.9%; HR = 0.34, 95% CI: 0.23–0.49, P < 0.01) or die (1.3% vs 3.8%; HR = 0.49, 95% CI: 0.35–0.68, P < 0.01) than those in the control group. After propensity score matching, 110 strokes (2.0% vs 4.6%) and 141 deaths (1.4% vs 3.8%) occurred in the matched intervention and control pairs (n = 1078).
Patients in the intervention group were less likely to experience a stroke during follow-up than those in the control group (HR = 0.40, 95% CI: 0.26–0.62, P < 0.01, Fig. 2A); as well as death (HR = 0.50, 95% CI: 0.35–0.72, P < 0.01, Fig. 2B).
Figure 2.
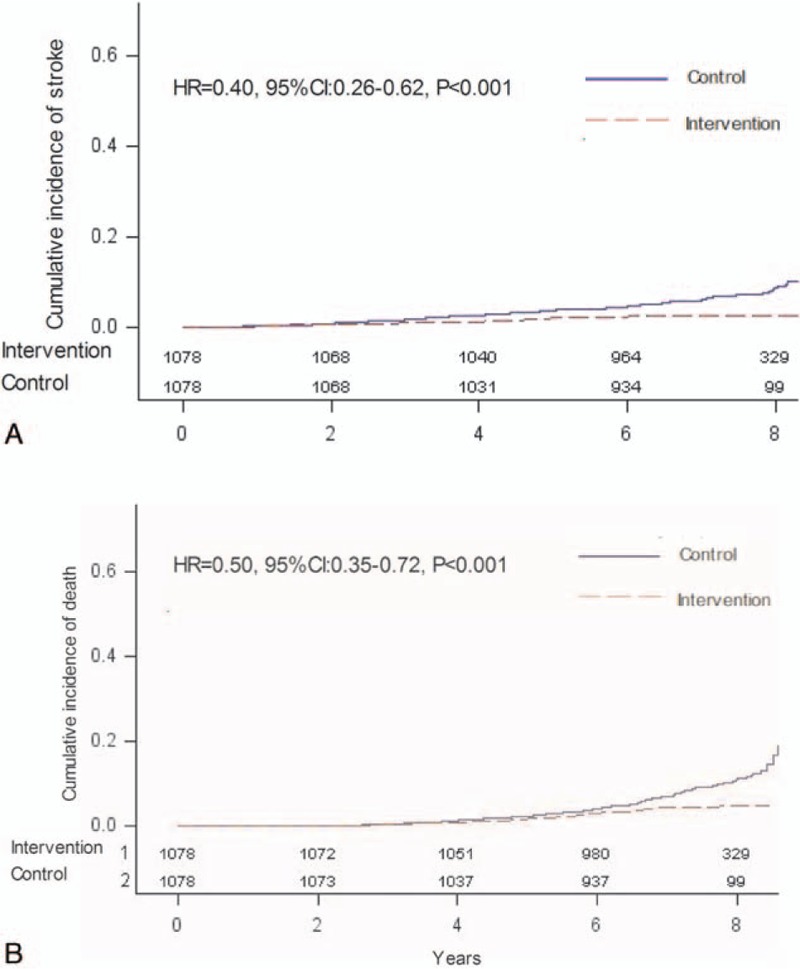
(A) Cumulative hazard curves for the primary composite endpoint for stroke. Time-to-event curves of stroke in control and intervention cohort. B. Cumulative hazard curves for the primary composite endpoint for total death. Time-to-event curves of total death in control and intervention cohort. CI = confidence interval, HR = hazard ratio.
The adjusted HRs for sensitivity analyses was similar to those of the entire group and propensity-score matched participants (Fig. 3).
Figure 3.

HRs for stroke and total death among the intervention group versus control group. ∗Exclusion of 161 hypertensive patients with cardiovascular diseases at baseline. #Exclusion of 14 hypertensive patients occurred deaths or strokes in the first year of follow-up. Adjusted HR: adjusted for age, gender, body mass index, smoking, alcohol drinking, baseline systolic and diastolic BP, diabetes, and history of CV diseases. CI = confidence interval, HR = hazard ratio.
4. Discussion
This is the first study to evaluate the long-term effects of a short multifaceted intervention on clinical outcomes in hypertensive patients in CHCs. The effect of short-term treatment of hypertension on the incidence of stroke and total death were studied more than 5 years after the project. After a median follow-up of 7.3 years, there was a 60% decrease in strokes and a 50% decrease in total deaths in the intervention group relative to the control group.
Many interventions were used in this project, with the 4 most prominent being health promotion through media, health education, training healthcare staff, and the implementation of treatment guidelines.[27] Studies have shown that interventions involving health education and training of healthcare providers can help patients better understand their diseases, change their health behaviors, and adhere to treatment. This may lead to significant improvement in health outcomes, including BP reduction.[28–35] These findings were also seen in the Community-Based Cardiovascular Risk Factors Intervention Strategies (CORFIS) study in Malaysia and a community-based intervention study in the United States.[21,36] Chen et al[37] found health education in combination with other interventions reduces stroke death by 74.3% and all-stroke morbidity by 54.7%.
One-year effects of the project HCC, in which many CHCs’ data have been pooled in previous studies, and results have shown the average BP to have a significant reduction and the control rate rose markedly.[25] Five years after the project ended, the positive effects remained detectable: the average BP was still lower than that in the baseline, and the control rate was near 59%. There was a 60% decrease in deaths from stroke and 50% decrease in overall death in the intervention group compared with the control group. One of the reasons for this may have been that the training and supervising forced doctors to improve and retain their practices after the program ended. Another reason was the patients’ attitude, behavior, and knowledge of prevention for hypertension were improved after 1-year management, and it helped to improve the compliance. This indicated that hypertension management in the community level, even short term intervention, can produce a positive effect for cardiovascular disease prevention. If it continues for a long time, the effect should become more pronounced.
Hypertension is highly prevalent in China and worldwide. Patients with hypertension have poor awareness, treatment, and control.[38,39] Guidelines are still not being adequately implemented by the doctors in their practice.[40] Public health efforts are, therefore, urgently required in order to improve BP control. Standardized CHC-based management of hypertension appears to be a good choice for China and possibly other developing countries.
The present study has several limitations. First, there were significant differences in the baseline data between the groups. Although propensity scoring and sensitivity analyses were carried out, important confounders may have been missed. Second, the study is limited by the limitations of the health record system. It was not possible to adjust for all factors that affect the risk of stroke, such as lipid status, hypertension, or family history. Third, the doctors’ practices were not evaluated during and after the program, and it was not clear whether their practices were retained at the time of follow-up. The rate of lost to follow up was near 30%, this maybe have biased the result assessment, although it was reported that a loss to follow-up of 22% would not bias conclusions.[41] Finally, ascertainment bias may have affected the results. For example, some strokes may have been missed if they led immediately to death.
In conclusion, this study was limited by the lost rate of follow up and applying propensity score model retrospectively. However, the results clearly indicated that one-year management of hypertension in the community level could lead to a marked reduction in stroke and total death. Improving hypertension management in community health centers has the potential for improving cardiovascular disease prevention.
Supplementary Material
Footnotes
Abbreviations: BP = blood pressure, CHCs = community health centers, CI = confidence interval, HCC = Hypertension Control in Community, HR = hazard ratio.
The authors have no conflicts of interest to declare.
Supplemental Digital Content is available for this article.
References
- [1].Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001;345:1291–7. [DOI] [PubMed] [Google Scholar]
- [3].Dregan A, Stewart R, Gulliford MC. Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing 2013;42:338–45. [DOI] [PubMed] [Google Scholar]
- [4].Lawes CM, Vander Hoorn S, Rodgers A. International Society of H. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–8. [DOI] [PubMed] [Google Scholar]
- [5].Yoon SS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011-2014. NCHS Data Brief 2015;1–8. [PubMed] [Google Scholar]
- [6].Unger A, Felzemburgh RD, Snyder RE, et al. Hypertension in a Brazilian urban slum population. J Urban Health 2015;92:446–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sengul S, Akpolat T, Erdem Y, et al. Changes in hypertension prevalence, awareness, treatment, and control rates in Turkey from 2003 to 2012. J Hypertens 2016;34:1208–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tailakh A, Evangelista LS, Mentes JC, et al. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci 2014;16:126–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003-2012. Int J Cardiol 2015;184:637–44. [DOI] [PubMed] [Google Scholar]
- [10].Hu SS, Kong LZ, Gao RL, et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci 2012;25:251–6. [DOI] [PubMed] [Google Scholar]
- [11].Sun H, Zou X, Liu L. Epidemiological factors of stroke: a survey of the current status in china. J Stroke 2013;15:109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation 2005;112:1651–62. [DOI] [PubMed] [Google Scholar]
- [13].Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology 2013;81:264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Siragy HM. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitors or calcium channel blocker vs diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Curr Hypertens Rep 2003;5:293–4. [DOI] [PubMed] [Google Scholar]
- [16].Sundstrom J, Arima H, Jackson R, et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med 2015;162:184–91. [DOI] [PubMed] [Google Scholar]
- [17].Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [18].Franklin SS, Jacobs MJ, Wong ND, et al. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 2001;37:869–74. [DOI] [PubMed] [Google Scholar]
- [19].Pettinger WA, Lee HC, Reisch J, et al. Long-term improvement in renal function after short-term strict blood pressure control in hypertensive nephrosclerosis. Hypertension 1989;13:766–72. [DOI] [PubMed] [Google Scholar]
- [20].Daniels SR. Short-term trials and long-term effects. Science 2001;293:2392–4. [DOI] [PubMed] [Google Scholar]
- [21].Low WH, Seet W, SR A, et al. Community-based cardiovascular Risk Factors Intervention Strategies (CORFIS) in managing hypertension: a pragmatic non-randomised controlled trial. Med J Malaysia 2013;68:129–35. [PubMed] [Google Scholar]
- [22].Boulware LE, Daumit GL, Frick KD, et al. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med 2001;21:221–32. [DOI] [PubMed] [Google Scholar]
- [23].Kennedy A, Reeves D, Bower P, et al. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomised controlled trial. J Epidemiol Community Health 2007;61:254–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang Z, Wang X, Chen Z, et al. Hypertension control in community health centers across China: analysis of antihypertensive drug treatment patterns. Am J Hypertens 2014;27:252–9. [DOI] [PubMed] [Google Scholar]
- [25].Wang ZW, Wang X, Zhang LF, et al. [Hypertension Control in Communities (HCC): evaluation result of blood pressure management among hypertensive]. Zhonghua Liu Xing Bing Xue Za Zhi 2010;31:1–4. [PubMed] [Google Scholar]
- [26].People’ s Medical Publishing House, Chinese guidelines for prevention treatment of hypertension. Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. Revised ed. 20052005. [Google Scholar]
- [27].van de Vijver S, Oti S, Addo J, et al. Review of community-based interventions for prevention of cardiovascular diseases in low- and middle-income countries. Ethn Health 2012;17:651–76. [DOI] [PubMed] [Google Scholar]
- [28].Kar SS, Thakur JS, Jain S, et al. Cardiovascular disease risk management in a primary health care setting of north India. Indian Heart J 2008;60:19–25. [PubMed] [Google Scholar]
- [29].Almeida-Pittito B, Hirai AT, Sartorelli DS, et al. Impact of a 2-year intervention program on cardiometabolic profile according to the number of goals achieved. Braz J Med Biol Res 2010;43:1088–94. [DOI] [PubMed] [Google Scholar]
- [30].Huang S, Hu X, Chen H, et al. The positive effect of an intervention program on the hypertension knowledge and lifestyles of rural residents over the age of 35 years in an area of China. Hypertens Res 2011;34:503–8. [DOI] [PubMed] [Google Scholar]
- [31].Saounatsou M, Patsi O, Fasoi G, et al. The influence of the hypertensive patient's education in compliance with their medication. Public Health Nurs 2001;18:436–42. [DOI] [PubMed] [Google Scholar]
- [32].Lu CH, Tang ST, Lei YX, et al. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health 2015;15:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Jeffery RW, Wing RR, Thorson C, et al. Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. J Consult Clin Psychol 1998;66:777–83. [DOI] [PubMed] [Google Scholar]
- [34].Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med 2006;145:165–75. [DOI] [PubMed] [Google Scholar]
- [35].Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ 2009;87:39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Zoellner J, Thomson JL, Landry AS, et al. Improvements in blood pressure among undiagnosed hypertensive participants in a community-based lifestyle intervention, Mississippi, 2010. Prev Chronic Dis 2014;11:E53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chen J, Wu X, Gu D. Hypertension and cardiovascular diseases intervention in the capital steel and iron company and Beijing Fangshan community. Obes Rev 2008;9suppl 1:142–5. [DOI] [PubMed] [Google Scholar]
- [38].Gao Y, Chen G, Tian H, et al. Prevalence of hypertension in china: a cross-sectional study. PLoS One 2013;8:e65938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet 2012;380:611–9. [DOI] [PubMed] [Google Scholar]
- [40].Karbach U, Schubert I, Hagemeister J, et al. Physicians’ knowledge of and compliance with guidelines: an exploratory study in cardiovascular diseases. Dtsch Arztebl Int 2011;108:61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Solberg TK, Sorlie A, Sjaavik K, et al. Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop 2011;82:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


