Abstract
Chronic kidney disease (CKD) has been identified as an important risk factor for new-onset atrial fibrillation (AF) and would significantly increase the risk of AF-related strokes. Stroke prevention in AF patients with CKD is a big challenge, especially for patients with end-stage renal disease (ESRD) undergoing long-term dialysis. In addition to an increase risk of stroke, renal dysfunction was also associated with a higher risk of hemorrhage due to dysregulation of coagulation and uremia-mediated platelet dysfunction. Therefore, the net clinical benefit balancing stroke risk reduction and increased risk of bleeding should be weighed carefully before initiating oral anti-coagulants for ESRD patients. Several studies investigating whether warfarin should be used for stroke prevention in AF patients with ESRD have been published and showed inconsistent results. Since none of these studies was a prospective and randomized trial, the best strategy for stroke prevention in AF patients with ESRD undergoing dialysis remained unknown and more data are necessary to answer this issue.
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and its prevalence is projected to continuously increase over the next few decades.[1] Asymptomatic AF was common (39.7%) in daily cardiology practice, being associated with elderly age and more comorbidities.[2] AF patients usually have several important comorbidities, such as hypertension, diabetes and heart failure, and “lone AF” is becoming uncommon.[3] The incidence of AF significantly increased when patients have more systemic diseases. In the previous study from Taiwan, the risk of new-onset AF increased from 0.77 per 1000 person-years for patients with a CHADS2 (congestive heart failure, hypertension, age ≥75, diabetes mellitus, and prior stroke or transient ischemic attack) score of 0 to 34.6 per 1000 person-years for those with a score of 6.[4] AF is an important risk factor of ischemic stroke with a worse prognosis and higher recurrence rate compared to that of non-AF related stroke.[5] The risk of AF-related stroke is not homogenous and mainly depends on the presence or absence of clinical risk factors. Several scoring systems, including CHADS2 and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age 65–74, female) schemes,[6,7] which incorporated clinical important factors have been developed to estimate the risk of stroke and guide anti-thrombotic therapies for AF patients.
Although renal dysfunction is not included in the CHADS2 or CHA2DS2-VASc schemes, it has been identified as an important risk factor for new-onset AF and would significantly increase the risk of AF-related strokes.[8-10] Moreover, renal dysfunction has been reported to be a significant predictor of in-hospital mortality in patients suffering a stroke.[11] The strategy about stroke prevention in AF patients with renal dysfunction, especially for those with end-stage renal disease (ESRD) undergoing dialysis, is complex. A substantially increased risk of bleeding with or without oral anticoagulants (OACs) is an important concern when treating these patients. In this review, we will focus on discussing the risk of AF, AF-related stroke and strategy for stroke prevention for patients with renal dysfunction and ESRD.
Risk of New-Onset AF in Patients with Renal Dysfunction
AF and renal dysfunction are frequently coexistent in the clinical practice. One-third of AF patients had stage III to V chronic kidney disease (CKD) with a glomerular filtration rate (GFR) lower than 60 mL/min/1.73m2 (Figure 1).[12-15] The prevalence of AF for subjects without CKD, and with stage 1 to 2, stage 3, and stage 4 to 5 CKD was 1.0%, 2.8%, 2.7% and 4.2%, respectively.[14] The prevalence of AF is much higher in ESRD patients undergoing maintenance hemodialysis which was reported to be 13-27%.[16-18] The risk of new-onset AF was also higher in patients with renal insufficiency compared to those without renal dysfunction. In a recent nationwide study from Taiwan which enrolled 404,703 patients without past history of AF (134,901 subjects each in control, CKD and ESRD groups), the incidence of AF increased from 5.0 per 1000 personyears for control subjects to 12.1 per 1000 person-years for ESRD patients (Figure 2).[19] Interestingly, the occurrence of AF was reported to be associated with increased risk of developing ESRD in adults with CKD with a hazard ratio (HR) of 1.67.[20] The mechanism behind the close relationship between CKD and AF may be multifactorial, including systemic inflammation, similar clinical risk factors for both conditions and modulation of the renin-angiotensin systems.[21,[22] In a recent study which enrolled 40 ESRD patients who have received implantations of implantable cardioverter defibrillators and undergone dialysis, device-detected AF occurred significantly more often on a dialysis day and especially during hemodialysis.[23] The finding suggested that the fluctuation of intra-vascular volume and electrolytes and activation of sympathetic nervous system may contribute the pathogenesis of AF development for ESRD patients.
Figure 1. Distributions of renal function in AF patients. One-third of AF patients had stage III to V chronic kidney disease with a glomerular filtration rate smaller than 60 mL/min/1.73m2. AF = atrial fibrillation. *The figure was modified from the figure by Hart et al. published in Can J Cardiol 2013.[15].
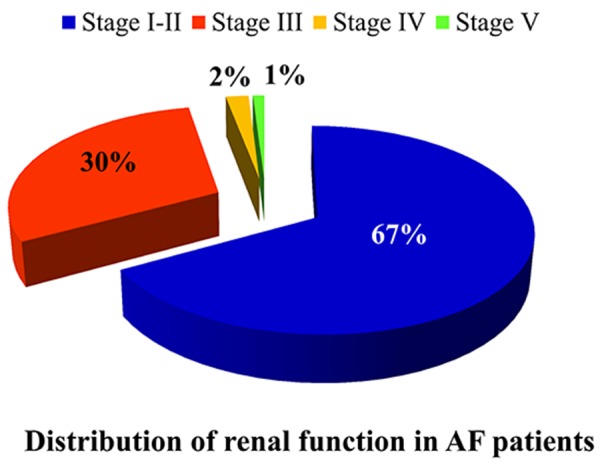
Figure 2. Incidence of new-onset AF among control subjects and patients with CKD and ESRD undergoing dialysis. The incidence of AF increased from 5.0 per 1000 person-years for control subjects to 12.1 per 1000 person-years for ESRD patients. AF = atrial fibrillation; CKD = chronic kidney disease; ESRD = end-stage renal disease. *The data used in the figure were from the paper by Liao et al. published in Kidney Int. 2014.[19].

Renal Dysfunction and Risk of Ischemic Stroke in AF
Several studies have demonstrated that renal dysfunction was an important risk factor of ischemic stroke in AF patients. In the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) study, 676 thromboembolic events occurred during the follow up of 33,165 person-years among 10,980 AF patients without use of OACs. The risk of thromboembolic events was 39% greater if estimated GFR (eGFR) fell below 45 mL/min/1.73m2 compared to an eGFR > 60 mL/min/1.73m2.[12] A recent meta-analysis performed by Zeng et al. which analyzed 18 studies involving 538,479 patients has demonstrated that AF patients with eGFR <60 mL/min/1.73m2 compared with those with eGFR ≥60 mL/min/1.73m2 experienced a significantly increased risk for developing thromboembolic events (relative risk, 1.62 [95% confidence interval = 1.40-1.87; P<0.001]). The annual rate of thromboembolic events increased by 0.41% (95% confidence interval = 0.17%-0.65%) for a 10 mL/min/1.73m2 decrease in renal function.[24] In a recent Danish registry study of 132,372 individuals with AF, 3,587 individuals had CKD, which was associated with increased risk of both ischemic stroke and bleeding.[8] In ROCKET-AF (Rivaroxaban Once-daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation), 14,264 patients with nonvalvular AF and estimated GFR ≥ 30 mL/min were randomized to rivaroxaban or dose-adjusted warfarin, reduced creatinine clearance was a strong, independent predictor of stroke and systemic embolism, second only to prior stroke or transient ischemic attack.[25] In our previous study which enrolled 547 AF patients after catheter ablation, renal dysfunction, defined as an eGFR < 60 mL/ min/1.73 m2 was an important risk factor of ischemic stroke even among patients with a CHA2DS2-VASc score of 0-1.[26]
Although renal dysfunction has been demonstrated to be a significant risk factor of ischemic stroke in AF patients, the question to be answered is whether adding renal dysfunction into the scoring systems, such as CHADS2 and CHA2DS2-VASc scores, could improve the accuracy of stroke prediction. A scoring system, named R2CHADS2, which incorporates the components of the CHADS2 score and awards 2 points for renal dysfunction, was derived from the subjects enrolled in ROCKET AF trial and validated among participants in ATRIA study.[25] The authors demonstrated that R2CHADS2 scheme could improve net reclassification index by 6.2% compared with CHA2DS2-VASc and by 8.2% compared with CHADS2.[25] However, in another study performed by Roldán et al. which enrolled 978 AF patients under warfarin treatment in Spain, adding renal dysfunction (1 point if eGFR was 30-60 ml/ min, and 2 points if eGFR was < 30 ml/min) to the CHADS2 and CHA2DS2-VASc stroke risk scores did not independently add predictive information.[27] Banerjee et al. investigated this issue among participants in the Loire Valley Atrial Fibrillation Project and found that renal impairment was not an independent predictor of ischemic stroke in patients with AF and did not significantly improve the predictive ability of the CHADS2 or CHA2DS2-VASc scores.[28] In 2 studies which compared R2CHADS2 and CHA2DS2-VASc scores among AF patients post catheter ablation, R2CHADS2 was not superior to CHA2DS2-VASc in predicting thromboembolism.[29,30] Besides, the CHA2DS2-VASc score could further differentiate thromboembolic risk in the low-risk strata based on R2CHADS2 score and may be superior in the subgroup with AF recurrences.[29]
Another new scoring system, named ATRIA score, which included renal dysfunction (eGFR < 45 ml/min or end-stage renal disease) and proteinuria in the model was derived from the ATRIA cohort.31 The ATRIA score ranged from 0 to 15, and it was stratified into low (0 to 5 points), moderate (6 points), and high (7 to 15 points) risk categories to fit annualized event rates of <1%, 1% to <2%, and ≥2% per year, respectively.[31] In the ATRIA cohort, the C-index was greater and net reclassification improvement was positive comparing the ATRIA score with the CHADS2 or CHA2DS2-VASc scores. However, in a recent study from Taiwan which analyzed 186,570 AF patients without antithrombotic therapies, the CHA2DS2-VASc score performed better than ATRIA score in predicting ischemic stroke as assessed by c-indexes (0.698 vs. 0.627, respectively; p < 0.0001). The CHA2DS2-VASc score also improved the net reclassification index by 11.7% compared with ATRIA score (p < 0.0001).32 Importantly, the study demonstrated that the patients categorized as low-risk by use of the ATRIA score (score 0-5) were not necessarily lowrisk, and the annual stroke rates can be as high as 2.95% at 1-year follow-up and 2.84% at 15-year follow-up. In contrast, patients with a CHA2DS2-VASc score of 0 had a truly low risk of ischemic stroke, with an annual stroke rate of approximately 1%.[32] Another study using the Danish registry database showed similar findings as that observed in Taiwan AF cohort.[33] Based on these findings of studies mentioned above, adding renal dysfunction into the CHA2DS2- VASc score may not be able to improve the accuracy for predicting ischemic stroke.
Stroke Prevention in AF Patients with Non-Dialysis Dependent CKD
Stroke prevention in AF patients with CKD is a big challenge, especially for ESRD patients undergoing long-term dialysis. Renal dysfunction is associated with both increased risk of stroke and hemorrhage (HR = 1.27) due to dysregulation of coagulation and uremia-mediated platelet dysfunction.[34] The registry study from Denmark showed the benefit of vitamin K antagonist (VKA) therapy on ischemic stroke/systemic thromboembolism outcomes in the setting of CKD, although both VKA and aspirin were associated with an increased risk of bleeding.[8] A recent study demonstrated that VKAs have poor efficacy and safety profiles in patients with non-dialysis dependent severe CKD (eGFR < 30ml/min) compared to patient with moderate renal impairment (eGFR 30-60ml/min) or normal renal function.[35] Patients with severe CKD were at high risk of stroke and major bleeding during VKA treatment compared with those without renal impairment, HR = 2.75 and 1.66, or with moderate CKD, HR = 3.93 and 1.86, respectively.[35] Importantly, variability of International Normalized Ratios during the entire treatment period significantly increased with each stage of CKD compared to control, suggesting that patients with CKD tended to have unstable anticoagulant control with VKAs.[35] Recently, Jun et al. further demonstrated that reduced kidney function was associated with an increased risk of major bleeding among older adults with AF starting warfarin; excess risks from reduced eGFR were most pronounced during the first 30 days of treatment.[36]
The non-VKA oral anticoagulants (NOACs) have changed the landscape of stroke prevention in AF by offering physicians and patients a safer and more convenient choice compared to warfarin. However, patients with an eGFR < 30 min/mL were excluded from the trials of dabigatran (The Randomized Evaluation of Long-Term Anti-coagulation Therapy <RE-LY>) and rivaroxaban (ROCKETAF). [37,38] In the trial of apixaban (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation < ARISTOTLE>), a small percentage of patients (1.5%) with an eGFR < 30 min/mL have been enrolled.[39] Therefore, apixaban is the only NOACs which could be used for patients with stage IV CKD. Unlike dabigatran whose excretion largely depends on renal route (~80%), the majority of apixaban was excreted by liver (~73%), and therefore the accumulation of apixaban in CKD patients may not be a serious concern. In the subgroup analysis of ARISTOTLE trial, apixaban treatment reduced the rate of stroke, death, and major bleeding, regardless of renal function.[40] Besides, patients with an eGFR < 50 mL/min seemed to have the greatest reduction in major bleeding with apixaban compared to warfarin.[40] However, there is no head-to-head study comparing the efficacy and safety of different NOACs, whether apixaban is a favorable choice of NOACs in patients with renal impairment remains uncertain.
Stroke Prevention in AF Patients with ESRD Undergoing Dialysis
The optimal strategy for stroke prevention in AF patients with ESRD undergoing dialysis is unclear. Internationally, warfarin prescribing patterns for hemodialysis patients with AF vary widely in the world, from 2% in Germany to as high as 37% in Canada.[41] Even in Canada, a national survey of nephrologists showed that most respondents were consistently uncertain about warfarin use for AF in ESRD patients, particularly because of uncertainty on how best to balance the prevention of ischemic stroke against bleeding risk.[42] Patients with ESRD undergoing dialysis were excluded in the generation and validation of stroke risk calculator scores, such as CHADS2 and CHA2DS2-VASc scores. The uncertainty about how to predict stroke risk among ESRD patients makes it even more difficult for clinical physicians to make decisions about stroke prevention. Until recently, the usefulness of CHADS2 and CHA2DS2-VASc scores in predicting ischemic stroke was validated in a nationwide study from Taiwan which analyzed more than 10,000 AF patients with ESRD undergoing dialysis.[43] Similar to general AF population without ESRD, the CHA2DS2-VASc score performed better than CHADS2 and was also able to further refine risk stratification among patients with a CHADS2 score of 0 or 1.[44,45]
The next question is how to treat these patients regarding stroke prevention. During hemodialysis sessions, patients would receive heparin for anticoagulation and its effect can be prolonged a few hours after the procedure which could increase the risk of bleeding. Table 1 summarized 6 published studies investigating whether warfarin or aspirin should be used for stroke prevention in AF patients with ESRD.[34,41,46-49] These studies showed inconsistent results with 4 of them did not demonstrate benefits of warfarin use for stroke prevention in ESRD patients undergoing dialysis. One study performed by Bonde et al. using Danish registry database showed that warfarin use was associated with a reduced risk of mortality among ESRD patients, but the risk of combined endpoint with fatal stroke or fatal bleeding was similar between users and non-users.[49] The only one study which demonstrated that warfarin use can provide net clinical benefits balancing ischemic stroke, hemorrhagic stroke and death was performed by Friberg et al.[34] In this study, 13,435 patients with renal failure (3,766 under warfarin use) were identified from Swedish Patient registry based on the disease or procedure codes. The authors demonstrated that patients with both AF and renal failure will probably benefit most from having the same treatment as is recommended for other patients with AF, without setting a higher or lower threshold for treatment.[34] Since these studies showed different results and none of them was a prospective and randomized trial, the best strategy for stroke prevention in AF patients with ESRD undergoing dialysis remained unknown and more data are necessary to answer this issue.
Table 1. Summary of the studies investigating the treatments for stroke prevention in AF patients with ESRD.
| Author (year) | Study design | Patient number | Main findings |
|---|---|---|---|
| Wizemann et al.[41] (2010) | Longitudinal cohort | ESRD patients undergoing hemodialysis – Age < 65 years: 1,001 Age 66-75 years: 1,137 Age >75 years: 1,107 | Warfarin use could not prevent stroke in patients younger than 75 years. Warfarin use was associated with a higher risk of stroke for patients older than 75 years (HR = 2.17; 95% CI = 1.04-4.53). |
| Winkelmayer et al.[46] (2011) | Longitudinal cohort | ESRD patients undergoing hemodialysis - 237 warfarin users and 948 propensity-matched nonusers over 2287 person-years of follow-up | The occurrence of ischemic stroke was similar (HR = 0.92; 95% CI = 0.61-1.37), whereas warfarin users experienced twice the risk of hemorrhagic stroke (HR = 2.38; 95% CI = 1.15- 4.96). |
| Shah et al. (2014)[47] | Population-based retrospective cohort ICD codes-based study | 1,626 dialysis patients (46% under warfarin use) | Warfarin use, in comparison with no-warfarin use, was not associated with a lower risk for stroke (HR = 1.14; 95% CI = 0.78–1.67) but was associated with a 44% higher risk for bleeding (HR = 1.44; 95% CI = 1.13–1.85). Propensity score–adjusted analyses yielded similar results. |
| Friberg et al. (2014)[34] | Population-based retrospective cohort ICD codes-based study | 13,435 AF patients with renal failure with or without long-term dialysis (3,766 with warfarin use) | Most patients with renal failure benefited from warfarin treatment, despite their high bleeding risk. The incidence of the combined endpoint ischemic or hemorrhagic stroke or death was lower among those who used warfarin than among those who did not use warfarin (HR = 0.76, 95% CI = 0.72-0.80). |
| Chen et al. (2014)[48] | Population-based retrospective cohort ICD codes-based study | Propensity-matched analysis for ESRD patients undergoing dialysis – Control (n = 840) versus warfarin (n = 250) versus anti-platelet drugs (n = 840) | Anti-platelet or warfarin treatment could not lower the risk of ischemic stroke in patients with ESRD |
| Bonde et al. (2014)[49] | Population-based retrospective cohort ICD codes-based study | 1,728 ESRD patients undergoing renal replacement therapy | In patients receiving renal replacement therapy with a CHA2DS2-VASc score > 2, warfarin was associated with lower risk of all-cause death (HR = 0.85, 95% CI = 0.72 to 0.99). However, the use of warfarin was not associated with a lower risk of fatal stroke or fatal bleeding (HR = 1.30, 95% CI = 0.77-2.20). |
Conclusions
In summary, renal dysfunction was a risk factor of new-onset AF and was associated with an increased risk of ischemic stroke in AF patients. Although several studies were published regarding the use of warfarin in AF patients with ESRD undergoing dialysis, more data are necessary to understand whether warfarin use has net clinical benefits considering stroke risk reduction and major bleeding in this special population..
Disclosures
None.
References
- Tse Hung-Fat, Wang Yong-Jun, Ahmed Ai-Abdullah Moheeb, Pizarro-Borromeo Annette B, Chiang Chern-En, Krittayaphong Rungroj, Singh Balbir, Vora Amit, Wang Chun-Xue, Zubaid Mohammad, Clemens Andreas, Lim Paul, Hu Dayi. Stroke prevention in atrial fibrillation--an Asian stroke perspective. Heart Rhythm. 2013 Jul;10 (7):1082–8. doi: 10.1016/j.hrthm.2013.03.017. [DOI] [PubMed] [Google Scholar]
- Boriani Giuseppe, Laroche Cecile, Diemberger Igor, Fantecchi Elisa, Popescu Mircea Ioachim, Rasmussen Lars Hvilsted, Sinagra Gianfranco, Petrescu Lucian, Tavazzi Luigi, Maggioni Aldo P, Lip Gregory Y H. Asymptomatic atrial fibrillation: clinical correlates, management, and outcomes in the EORP-AF Pilot General Registry. Am. J. Med. 2015 May;128 (5):509–18.e2. doi: 10.1016/j.amjmed.2014.11.026. [DOI] [PubMed] [Google Scholar]
- Chiang Chern-En, Zhang Shu, Tse Hung Fat, Teo Wee Siong, Omar Razali, Sriratanasathavorn Charn. Atrial fibrillation management in Asia: from the Asian expert forum on atrial fibrillation. Int. J. Cardiol. 2013 Mar 20;164 (1):21–32. doi: 10.1016/j.ijcard.2011.12.033. [DOI] [PubMed] [Google Scholar]
- Chao Tze-Fan, Liu Chia-Jen, Chen Su-Jung, Wang Kang-Ling, Lin Yenn-Jiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Wu Tsu-Juey, Chen Tzeng-Ji, Chen Shih-Ann. CHADS2 score and risk of new-onset atrial fibrillation: a nationwide cohort study in Taiwan. Int. J. Cardiol. 2013 Sep 30;168 (2):1360–3. doi: 10.1016/j.ijcard.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Lin H J, Wolf P A, Kelly-Hayes M, Beiser A S, Kase C S, Benjamin E J, D'Agostino R B. Stroke severity in atrial fibrillation. The Framingham Study. Stroke. 1996 Oct;27 (10):1760–4. doi: 10.1161/01.str.27.10.1760. [DOI] [PubMed] [Google Scholar]
- Gage B F, Waterman A D, Shannon W, Boechler M, Rich M W, Radford M J. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001 Jun 13;285 (22):2864–70. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- Lip Gregory Y H, Nieuwlaat Robby, Pisters Ron, Lane Deirdre A, Crijns Harry J G M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010 Feb;137 (2):263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- Olesen Jonas Bjerring, Lip Gregory Y H, Kamper Anne-Lise, Hommel Kristine, Køber Lars, Lane Deirdre A, Lindhardsen Jesper, Gislason Gunnar Hilmar, Torp-Pedersen Christian. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N. Engl. J. Med. 2012 Aug 16;367 (7):625–35. doi: 10.1056/NEJMoa1105594. [DOI] [PubMed] [Google Scholar]
- Guo Yutao, Wang Haijun, Zhao Xiaoning, Zhang Yu, Zhang Dexian, Ma Jingling, Wang Yutang, Lip Gregory Y H. Relation of renal dysfunction to the increased risk of stroke and death in female patients with atrial fibrillation. Int. J. Cardiol. 2013 Sep 30;168 (2):1502–8. doi: 10.1016/j.ijcard.2012.12.099. [DOI] [PubMed] [Google Scholar]
- Providência Rui, Barra Sérgio, Paiva Luís. Chronic renal disease is associated with stroke and thromboembolism in atrial fibrillation independently from gender. Int. J. Cardiol. 2013 Oct 3;168 (3):3106–7. doi: 10.1016/j.ijcard.2013.04.072. [DOI] [PubMed] [Google Scholar]
- Fabbian Fabio, Gallerani Massimo, Pala Marco, De Giorgi Alfredo, Salmi Raffaella, Dentali Francesco, Ageno Walter, Manfredini Roberto. Association between in-hospital mortality and renal dysfunction in 186,219 patients hospitalized for acute stroke in the Emilia-Romagna region of Italy. Angiology. 2014 Nov;65 (10):906–10. doi: 10.1177/0003319713512017. [DOI] [PubMed] [Google Scholar]
- Go Alan S, Fang Margaret C, Udaltsova Natalia, Chang Yuchiao, Pomernacki Niela K, Borowsky Leila, Singer Daniel E. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. 2009 Mar 17;119 (10):1363–9. doi: 10.1161/CIRCULATIONAHA.108.816082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooiman J, van de Peppel W R, van der Meer F J M, Huisman M V. Incidence of chronic kidney disease in patients with atrial fibrillation and its relevance for prescribing new oral antithrombotic drugs. J. Thromb. Haemost. 2011 Aug;9 (8):1652–3. doi: 10.1111/j.1538-7836.2011.04347.x. [DOI] [PubMed] [Google Scholar]
- Baber Usman, Howard Virginia J, Halperin Jonathan L, Soliman Elsayed Z, Zhang Xiao, McClellan William, Warnock David G, Muntner Paul. Association of chronic kidney disease with atrial fibrillation among adults in the United States: REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Circ Arrhythm Electrophysiol. 2011 Feb;4 (1):26–32. doi: 10.1161/CIRCEP.110.957100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart Robert G, Eikelboom John W, Brimble K Scott, McMurtry M Sean, Ingram Alistair J. Stroke prevention in atrial fibrillation patients with chronic kidney disease. Can J Cardiol. 2013 Jul;29 (7 Suppl):S71–8. doi: 10.1016/j.cjca.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Vázquez E, Sánchez-Perales C, Borrego F, Garcia-Cortés M J, Lozano C, Guzmán M, Gil J M, Borrego M J, Pérez V. Influence of atrial fibrillation on the morbido-mortality of patients on hemodialysis. Am. Heart J. 2000 Dec;140 (6):886–90. doi: 10.1067/mhj.2000.111111. [DOI] [PubMed] [Google Scholar]
- Bozbas Huseyin, Atar Ilyas, Yildirir Aylin, Ozgul Aliseydi, Uyar Murathan, Ozdemir Nurhan, Muderrisoglu Haldun, Ozin Bulent. Prevalence and predictors of arrhythmia in end stage renal disease patients on hemodialysis. Ren Fail. 2007;29 (3):331–9. doi: 10.1080/08860220701191237. [DOI] [PubMed] [Google Scholar]
- Genovesi Simonetta, Pogliani Daniela, Faini Andrea, Valsecchi Maria G, Riva Alessandra, Stefani Francesca, Acquistapace Irene, Stella Andrea, Bonforte Giuseppe, DeVecchi Amedeo, DeCristofaro Vincenzo, Buccianti Gherardo, Vincenti Antonio. Prevalence of atrial fibrillation and associated factors in a population of long-term hemodialysis patients. Am. J. Kidney Dis. 2005 Nov;46 (5):897–902. doi: 10.1053/j.ajkd.2005.07.044. [DOI] [PubMed] [Google Scholar]
- Liao Jo-Nan, Chao Tze-Fan, Liu Chia-Jen, Wang Kang-Ling, Chen Su-Jung, Lin Yenn-Jiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Chung Fa-Po, Chen Tzeng-Ji, Chen Shih-Ann. Incidence and risk factors for new-onset atrial fibrillation among patients with end-stage renal disease undergoing renal replacement therapy. Kidney Int. 2015 Jun;87 (6):1209–15. doi: 10.1038/ki.2014.393. [DOI] [PubMed] [Google Scholar]
- Bansal Nisha, Fan Dongjie, Hsu Chi-yuan, Ordonez Juan D, Marcus Greg M, Go Alan S. Incident atrial fibrillation and risk of end-stage renal disease in adults with chronic kidney disease. Circulation. 2013 Feb 5;127 (5):569–74. doi: 10.1161/CIRCULATIONAHA.112.123992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shlipak Michael G, Fried Linda F, Crump Casey, Bleyer Anthony J, Manolio Teri A, Tracy Russell P, Furberg Curt D, Psaty Bruce M. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003 Jan 7;107 (1):87–92. doi: 10.1161/01.cir.0000042700.48769.59. [DOI] [PubMed] [Google Scholar]
- Reinecke Holger, Brand Eva, Mesters Rolf, Schäbitz Wolf-Rüdiger, Fisher Marc, Pavenstädt Hermann, Breithardt Günter. Dilemmas in the management of atrial fibrillation in chronic kidney disease. J. Am. Soc. Nephrol. 2009 Apr;20 (4):705–11. doi: 10.1681/ASN.2007111207. [DOI] [PubMed] [Google Scholar]
- Buiten M S, de Bie M K, Rotmans J I, Gabreëls B A, van Dorp W, Wolterbeek R, Trines S A, Schalij M J, Jukema J W, Rabelink T J, van Erven L. The dialysis procedure as a trigger for atrial fibrillation: new insights in the development of atrial fibrillation in dialysis patients. Heart. 2014 May;100 (9):685–90. doi: 10.1136/heartjnl-2013-305417. [DOI] [PubMed] [Google Scholar]
- Zeng Wu-Tao, Sun Xiu-Ting, Tang Kai, Mei Wei-Yi, Liu Li-Juan, Xu Qing, Cheng Yun-Jiu. Risk of thromboembolic events in atrial fibrillation with chronic kidney disease. Stroke. 2015 Jan;46 (1):157–63. doi: 10.1161/STROKEAHA.114.006881. [DOI] [PubMed] [Google Scholar]
- Piccini Jonathan P, Stevens Susanna R, Chang YuChiao, Singer Daniel E, Lokhnygina Yuliya, Go Alan S, Patel Manesh R, Mahaffey Kenneth W, Halperin Jonathan L, Breithardt Günter, Hankey Graeme J, Hacke Werner, Becker Richard C, Nessel Christopher C, Fox Keith A A, Califf Robert M. Renal dysfunction as a predictor of stroke and systemic embolism in patients with nonvalvular atrial fibrillation: validation of the R(2)CHADS(2) index in the ROCKET AF (Rivaroxaban Once-daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) and ATRIA (AnTicoagulation and Risk factors In Atrial fibrillation) study cohorts. Circulation. 2013 Jan 15;127 (2):224–32. doi: 10.1161/CIRCULATIONAHA.112.107128. [DOI] [PubMed] [Google Scholar]
- Chao Tze-Fan, Tsao Hsuan-Ming, Ambrose Kibos, Lin Yenn-Jiang, Lin Wei-Shiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Suenari Kazuyoshi, Li Cheng-Hung, Hartono Beny, Chang Hung-Yu, Chung Fa-Po, Hanafy Dicky A, Lin Wen-Yu, Chen Shih-Ann. Renal dysfunction and the risk of thromboembolic events in patients with atrial fibrillation after catheter ablation--the potential role beyond the CHA₂DS₂-VASc score. Heart Rhythm. 2012 Nov;9 (11):1755–60. doi: 10.1016/j.hrthm.2012.06.039. [DOI] [PubMed] [Google Scholar]
- Roldán V, Marín F, Manzano-Fernandez S, Fernández H, Gallego P, Valdés M, Vicente V, Lip G Y H. Does chronic kidney disease improve the predictive value of the CHADS2 and CHA2DS2-VASc stroke stratification risk scores for atrial fibrillation? Thromb. Haemost. 2013 May;109 (5):956–60. doi: 10.1160/TH13-01-0054. [DOI] [PubMed] [Google Scholar]
- Banerjee Amitava, Fauchier Laurent, Vourc'h Patrick, Andres Christian R, Taillandier Sophie, Halimi Jean Michel, Lip Gregory Y H. Renal impairment and ischemic stroke risk assessment in patients with atrial fibrillation: the Loire Valley Atrial Fibrillation Project. J. Am. Coll. Cardiol. 2013 May 21;61 (20):2079–87. doi: 10.1016/j.jacc.2013.02.035. [DOI] [PubMed] [Google Scholar]
- Kornej Jelena, Hindricks Gerhard, Kosiuk Jedrzej, Arya Arash, Sommer Philipp, Husser Daniela, Rolf Sascha, Richter Sergio, Piorkowski Christopher, Gaspar Thomas, Lip Gregory Y H, Bollmann Andreas. Renal dysfunction, stroke risk scores (CHADS2, CHA2DS2-VASc, and R2CHADS2), and the risk of thromboembolic events after catheter ablation of atrial fibrillation: the Leipzig Heart Center AF Ablation Registry. Circ Arrhythm Electrophysiol. 2013 Oct;6 (5):868–74. doi: 10.1161/CIRCEP.113.000869. [DOI] [PubMed] [Google Scholar]
- Chao Tze-Fan, Lin Yenn-Jiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Liao Jo-Nan, Chung Fa-Po, Hsieh Ming-Hsiung, Chen Shih-Ann. R2CHADS2 score and thromboembolic events after catheter ablation of atrial fibrillation in comparison with the CHA2DS2-VASc score. Can J Cardiol. 2014 Apr;30 (4):405–12. doi: 10.1016/j.cjca.2014.01.005. [DOI] [PubMed] [Google Scholar]
- Singer Daniel E, Chang Yuchiao, Borowsky Leila H, Fang Margaret C, Pomernacki Niela K, Udaltsova Natalia, Reynolds Kristi, Go Alan S. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J Am Heart Assoc. 2013 Jun;2 (3):e000250. doi: 10.1161/JAHA.113.000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao Tze-Fan, Liu Chia-Jen, Wang Kang-Ling, Lin Yenn-Jiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Chen Tzeng-Ji, Lip Gregory Y H, Chen Shih-Ann. Using the CHA2DS2-VASc score for refining stroke risk stratification in 'low-risk' Asian patients with atrial fibrillation. J. Am. Coll. Cardiol. 2014 Oct 21;64 (16):1658–65. doi: 10.1016/j.jacc.2014.06.1203. [DOI] [PubMed] [Google Scholar]
- Lip Gregory Y H, Nielsen Peter Brønnum, Skjøth Flemming, Lane Deirdre A, Rasmussen Lars Hvilsted, Larsen Torben Bjerregaard. The value of the European society of cardiology guidelines for refining stroke risk stratification in patients with atrial fibrillation categorized as low risk using the anticoagulation and risk factors in atrial fibrillation stroke score: a nationwide cohort study. Chest. 2014 Nov;146 (5):1337–46. doi: 10.1378/chest.14-0533. [DOI] [PubMed] [Google Scholar]
- Friberg Leif, Benson Lina, Lip Gregory Y H. Balancing stroke and bleeding risks in patients with atrial fibrillation and renal failure: the Swedish Atrial Fibrillation Cohort study. Eur. Heart J. 2015 Feb 1;36 (5):297–306. doi: 10.1093/eurheartj/ehu139. [DOI] [PubMed] [Google Scholar]
- Kooiman Judith, van Rein Nienke, Spaans Bas, van Beers Koen A J, Bank Jonna R, van de Peppel Wilke R, Sol Antonio Iglesias del, Cannegieter Suzanne C, Rabelink Ton J, Lip Gregory Y H, Klok Frederikus A, Huisman Menno V. Efficacy and safety of vitamin K-antagonists (VKA) for atrial fibrillation in non-dialysis dependent chronic kidney disease. PLoS ONE. 2014;9 (5):e94420. doi: 10.1371/journal.pone.0094420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun Min, James Matthew T, Manns Braden J, Quinn Robert R, Ravani Pietro, Tonelli Marcello, Perkovic Vlado, Winkelmayer Wolfgang C, Ma Zhihai, Hemmelgarn Brenda R. The association between kidney function and major bleeding in older adults with atrial fibrillation starting warfarin treatment: population based observational study. BMJ. 2015;350 ():h246. doi: 10.1136/bmj.h246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly Stuart J, Ezekowitz Michael D, Yusuf Salim, Eikelboom John, Oldgren Jonas, Parekh Amit, Pogue Janice, Reilly Paul A, Themeles Ellison, Varrone Jeanne, Wang Susan, Alings Marco, Xavier Denis, Zhu Jun, Diaz Rafael, Lewis Basil S, Darius Harald, Diener Hans-Christoph, Joyner Campbell D, Wallentin Lars. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009 Sep 17;361 (12):1139–51. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- Patel Manesh R, Mahaffey Kenneth W, Garg Jyotsna, Pan Guohua, Singer Daniel E, Hacke Werner, Breithardt Günter, Halperin Jonathan L, Hankey Graeme J, Piccini Jonathan P, Becker Richard C, Nessel Christopher C, Paolini John F, Berkowitz Scott D, Fox Keith A A, Califf Robert M. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011 Sep 8;365 (10):883–91. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- Granger Christopher B, Alexander John H, McMurray John J V, Lopes Renato D, Hylek Elaine M, Hanna Michael, Al-Khalidi Hussein R, Ansell Jack, Atar Dan, Avezum Alvaro, Bahit M Cecilia, Diaz Rafael, Easton J Donald, Ezekowitz Justin A, Flaker Greg, Garcia David, Geraldes Margarida, Gersh Bernard J, Golitsyn Sergey, Goto Shinya, Hermosillo Antonio G, Hohnloser Stefan H, Horowitz John, Mohan Puneet, Jansky Petr, Lewis Basil S, Lopez-Sendon Jose Luis, Pais Prem, Parkhomenko Alexander, Verheugt Freek W A, Zhu Jun, Wallentin Lars. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011 Sep 15;365 (11):981–92. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- Hohnloser Stefan H, Hijazi Ziad, Thomas Laine, Alexander John H, Amerena John, Hanna Michael, Keltai Matyas, Lanas Fernando, Lopes Renato D, Lopez-Sendon Jose, Granger Christopher B, Wallentin Lars. Efficacy of apixaban when compared with warfarin in relation to renal function in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur. Heart J. 2012 Nov;33 (22):2821–30. doi: 10.1093/eurheartj/ehs274. [DOI] [PubMed] [Google Scholar]
- Wizemann Volker, Tong Lin, Satayathum Sudtida, Disney Alex, Akiba Takashi, Fissell Rachel B, Kerr Peter G, Young Eric W, Robinson Bruce M. Atrial fibrillation in hemodialysis patients: clinical features and associations with anticoagulant therapy. Kidney Int. 2010 Jun;77 (12):1098–106. doi: 10.1038/ki.2009.477. [DOI] [PubMed] [Google Scholar]
- Juma Salima, Thomson Benjamin K A, Lok Charmaine E, Clase Catherine M, Blake Peter G, Moist Louise. Warfarin use in hemodialysis patients with atrial fibrillation: decisions based on uncertainty. BMC Nephrol. 2013;14 ():174. doi: 10.1186/1471-2369-14-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao Tze-Fan, Liu Chia-Jen, Wang Kang-Ling, Lin Yenn-Jiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Chung Fa-Po, Liao Jo-Nan, Chen Tzeng-Ji, Lip Gregory Y H, Chen Shih-Ann. Incidence and prediction of ischemic stroke among atrial fibrillation patients with end-stage renal disease requiring dialysis. Heart Rhythm. 2014 Oct;11 (10):1752–9. doi: 10.1016/j.hrthm.2014.06.021. [DOI] [PubMed] [Google Scholar]
- Chao Tze-Fan, Lin Yenn-Jiang, Tsao Hsuan-Ming, Tsai Chin-Feng, Lin Wei-Shiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Suenari Kazuyoshi, Li Cheng-Hung, Hartono Beny, Chang Hung-Yu, Ambrose Kibos, Wu Tsu-Juey, Chen Shih-Ann. CHADS(2) and CHA(2)DS(2)-VASc scores in the prediction of clinical outcomes in patients with atrial fibrillation after catheter ablation. J. Am. Coll. Cardiol. 2011 Nov 29;58 (23):2380–5. doi: 10.1016/j.jacc.2011.08.045. [DOI] [PubMed] [Google Scholar]
- Olesen Jonas Bjerring, Torp-Pedersen Christian, Hansen Morten Lock, Lip Gregory Y H. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0-1: a nationwide cohort study. Thromb. Haemost. 2012 Jun;107 (6):1172–9. doi: 10.1160/TH12-03-0175. [DOI] [PubMed] [Google Scholar]
- Winkelmayer Wolfgang C, Liu Jun, Setoguchi Soko, Choudhry Niteesh K. Effectiveness and safety of warfarin initiation in older hemodialysis patients with incident atrial fibrillation. Clin J Am Soc Nephrol. 2011 Nov;6 (11):2662–8. doi: 10.2215/CJN.04550511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah Mitesh, Avgil Tsadok Meytal, Jackevicius Cynthia A, Essebag Vidal, Eisenberg Mark J, Rahme Elham, Humphries Karin H, Tu Jack V, Behlouli Hassan, Guo Helen, Pilote Louise. Warfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysis. Circulation. 2014 Mar 18;129 (11):1196–203. doi: 10.1161/CIRCULATIONAHA.113.004777. [DOI] [PubMed] [Google Scholar]
- Chen Jien-Jiun, Lin Lian-Yu, Yang Yao-Hsu, Hwang Juey-Jen, Chen Pau-Chung, Lin Jiunn-Lee. Anti-platelet or anti-coagulant agent for the prevention of ischemic stroke in patients with end-stage renal disease and atrial fibrillation--a nation-wide database analyses. Int. J. Cardiol. 2014 Dec 20;177 (3):1008–11. doi: 10.1016/j.ijcard.2014.09.140. [DOI] [PubMed] [Google Scholar]
- Bonde Anders Nissen, Lip Gregory Y H, Kamper Anne-Lise, Hansen Peter Riis, Lamberts Morten, Hommel Kristine, Hansen Morten Lock, Gislason Gunnar Hilmar, Torp-Pedersen Christian, Olesen Jonas Bjerring. Net clinical benefit of antithrombotic therapy in patients with atrial fibrillation and chronic kidney disease: a nationwide observational cohort study. J. Am. Coll. Cardiol. 2014 Dec 16;64 (23):2471–82. doi: 10.1016/j.jacc.2014.09.051. [DOI] [PubMed] [Google Scholar]


