Abstract
The number of atrial fibrillation (AF) catheter ablations performed annually has been increasing exponentially in the western countries in the last few years. This is clearly related to technological advancements, which have greatly contributed to the improvements in catheter ablation of AF. In particular, state-of-the-art electroanatomical mapping systems have greatly facilitated mapping processes and have enabled complex AF ablation strategies. In this review, we outline contemporary and upcoming electroanatomical key technologies focusing on new mapping tools and strategies in the context of AF catheter ablation.
Introduction
Atrial fibrillation (AF) constitutes the most common arrhythmia in clinical practice with prevalence estimates varying from 1% in the general population to 17% in octogenarians.[1] Rhythm control represents a therapeutic goal in patients, which are still symptomatic after rate control. Antiarrhythmic drugs (AADs) have long been the only means to maintain sinus rhythm. However, AADs are associated with limited efficacy and considerable side effects. Thus, interventional approaches have gained in importance. Catheter ablation is such a promising procedure, which - in the early days - focused on transferring surgical MAZE strategies into the EP lab by creating linear radiofrequency lesions in the right (and left) atrium. However, rather modest success rates and significant complication rates were observed. The discovery of recurrent focal activity as AF triggers, and the demonstration that the primary source is located within or near the pulmonary veins (PVs) whose elimination has the potential to abolish AF reinitiated enthusiasm for catheter-based ablation.[2-4] The technique of ablation has evolved from early attempts to target individual ectopic foci within the PV over segmental ostial PV isolation to wide circumferential ‘antral’ electrical disconnection by circumferential linear lesions around both ipsilateral PVs.[5] Recovered PV conduction is a dominant finding in the majority of patients with recurrences and can be successfully eliminated by gap closure within the encircling lines.[6,7] Nowadays, electrical isolation of the PVs is recommended as the cornerstone of AF catheter ablation.[8-10] Although more than one ablation session may be necessary in some patients, rates of long-term survival free from AF recurrences after circumferential PV isolation with or without elimination of non-PV triggers are relatively high in paroxysmal AF. However, procedures in patients with persistent and especially long-standing persistent AF have a lower long-term success rate.[11,12] At least in part, this may be explained by the fact that chronic forms of AF are very often associated with structurally diseased and remodeled atria requiring additional atrial myocardial substrate modifications.[13-14] As a consequence, many centers add some kind of substrate modification for all patients with (longstanding) persistent AF routinely. Established forms of substrate modification include left and right atrial defragmentation during AF (as described below) and/or linear ablations in the left atrium. These debulking linear lesions (e.g. roof line, mitral isthmus line) serve to avoid common postinterventional macroreentrant tachycardias like the roof-dependent or perimitral atrial flutter. Endpoints of AF catheter ablation are still a matter of debate. Whereas bidirectional PV isolation and verification of linear lesion completeness is common standard, ablation-induced AF slowing/termination and subsequent AF noninducibility are less clear.
At the end of the day, all current strategies require application of systematic lesion patterns with long linear lesions, which need to be electrically continuous, transmural, and irreversible at best. This goal means a major challenge for the operator, because effective catheter ablation in the LA/PV transition zone and anywhere else in the complex and individually variable anatomy of the human atrium is difficult, especially in a beating heart within a breathing thorax. Inaccuracies in catheter manipulation and lesion deployment may not only result in incomplete lines of electrical block, but may also cause collateral damage like pulmonary vein stenosis, perforation, phrenic nerve injury, and esophageal damage. In this context, fluoroscopy, which is still the basic tool to visualize catheter location and maneuvering, may only insufficiently demarcate critical targets, especially without contrast enhancement. Thus, it is generally understandable, that sole reliance on two-dimensional x-ray impedes complex ablation approaches and exposes patients and staff to significant amounts of ionizing radiation.
In the late 1990’s, electroanatomical mapping systems (EAMS) were introduced into clinical practice. Early technologies like the LocaLisa® system (Medtronic, Arden Hills, MN, USA) were capable of tracking intracardiac electrodes as well as tagging points in a 3D electrical field.[15] Reduced x-ray needs for all kinds of ablations were consistently observed.[16-19] However, the navigation system has been largely superseded, because of its inability to build surface geometries and to create electrophysiological maps. The Ensite Array® (Endocardial Solutions, St. Paul, MN, USA) uses a mesh of 64 coated wires spanned over a balloon forming more than 3,000 unipolar electrodes. In later generations the LocaLisa® technology has been integrated so that array and ablation catheter localization is achieved via the impedance-based tracking technology. More than 3000 “virtual” (non-contact) far-field signals are simultaneously superimposed on a reconstructed endocardial surface reconstruction allowing for high-density electrophysiologic maps from single beats. However, the system did not prevail for routine use, mainly because of its complexity, costs, and limitations like electrogram timing inaccuracies at distances more than 34 mm from the center of the array.[20] Nowadays, two EAMS have become the standard in electrophysiological practice: (1) the EnsiteNavX® system (St Jude Medical, St. Paul, MN, USA), incorporating a further development of the impedance-based Localisa navigation technology, and (2) the Carto® system (Biosense Webster, Baldwin Park, CA, USA). Since their introduction into clinical practice, these EAMS have seen continuous technical development in various aspects such as (multiple) catheter visualization, creation of chamber models, image integration, and mapping modalities.[21] In consideration of this, this review article outlines state-of-the-art features and derived strategies of these rapidly evolving EAMS technologies and outlines upcoming technologies in the context of AF ablation.
Description of established electroanatomical mapping technologies
Contact mapping
The fundamental concept of established EAMS consist of a precise non-fluoroscopic visualization of mapping catheters and a reconstruction of 3D volumes of interest (e.g. the left atrium) that are created by the manipulation of the mapping catheter. The resulting 3D reconstruction model is illustrated as a shell representing the cardiac structure of interest and can be more accurate in its representation by increasing the number of sampled points. The latest EAMS versions come with tools that enable fast and automated multi-point model creation during catheter movement. Multipolar catheters may additionally support rapid chamber reconstruction and mapping with individual anatomical locations such as His bundle, valvular annuli and other structures being marked or tagged within the model. Another feature of current EAMS is the simultaneous display of various diagnostic catheters and devices (e.g. esophageal probe) in real-time in relation to the 3D geometry. Additionally, electrical information at map points can be recorded and used for further analyses. The most established mapping techniques include color-coded display of the referenced electrical activation sequence known as “activation mapping”, and mapping of unipolar/bipolar electrograms as part of “fractionation mapping” and “voltage mapping” on the model surface.[22] Optional features allow for the measurement and display of electrical contact or the contact force at the electrode-tissue interface. The two most widely applied contemporary contact EAMS versions for AF ablation worldwide are Carto3® (Biosense Webster) and EnSiteNavX Velocity® (St Jude Medical).
The original Carto® system is principally based on three active weak magnetic fields (5x10-6 to 5x10-5 Tesla), generated by a 3-coil location pad placed underneath the patient’s thorax. Magnetic field strengths are measured with mini-sensors embedded in the catheter tip on a continuous basis providing information about the exact position and orientation of the sensor in space.[21] One sensor attached to the patient’s skin within the working space of interest serves as a location reference. Patient movement or dislocation of the location pad may lead to uncorrectable map shifts. Modern versions of Carto® System (Carto3®) integrate a hybrid of magnetic and current-based catheter localization technology that enables visualization of multiple catheters simultaneously without the need for fluoroscopy. For this, six electrode patches positioned at the patient’s back and chest continuously screen the current emitted at a unique frequency from different catheter electrodes. Localization of the non-magnetic electrodes can be calibrated by the detection of the magnetic sensor within the coordinate system in order to overcome distortions from non-uniform intrathoracic resistances. Other new development of the Carto3® system is the fast anatomical mapping (FAM) allowing the creation of detailed shells with all electrodes of a multipolar mapping catheter by moving it around in the chamber of interest. These representations of end-diastolic surfaces provide a much better reconstruction than the point-by-point maps in the earlier Carto® versions. Another development targeting the accuracy of surface reconstructions is accomplished by a unique type of respiratory gating in which varying thoracic impedances are measured throughout the respiratory cycle. The new developments in the current Carto3® version have already been shown beneficial in terms of fluoroscopy requirements, when compared to the older CartoXP® version.[23]
The other EAMS commonly used today is the EnsiteNavX® system. This system is based on the LocaLisa® technology and uses six skin electrode patches to create high frequency electric fields (approximately 8 kHz in the current version) in three orthogonal planes. The 3D-localization of conventional electrophysiology catheters is calculated based on an impedance gradient in relation to a reference electrode.[15] Calculations can be complicated by the body’s non-linear impedance, which is to some extent correctable by a process called field scaling.[15,24] In order to improve compensation for cardiac and respiratory motion artifacts, intra-cardiac reference catheters such as catheters placed at the relatively stable proximal coronary sinus are usually preferred over an extra-cardiac reference electrode. However, dislocation of the intra-cardiac reference catheter may lead to uncorrectable map shifts. It is an advantage of the EnSiteNavX® system over the Carto® system that it is architecturally open and allows for visualization of multiple catheters from different manufacturers.[25] Moreover, all electrodes of any catheter can be used simultaneously for a relatively quick reconstruction of cardiac chambers providing not only anatomical information but also electrophysiological mapping data, when the OneMap® tool is used.
Image integration
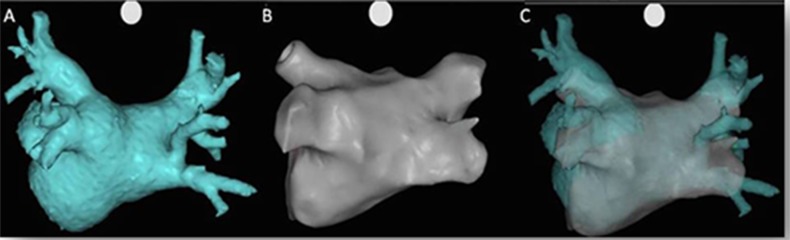
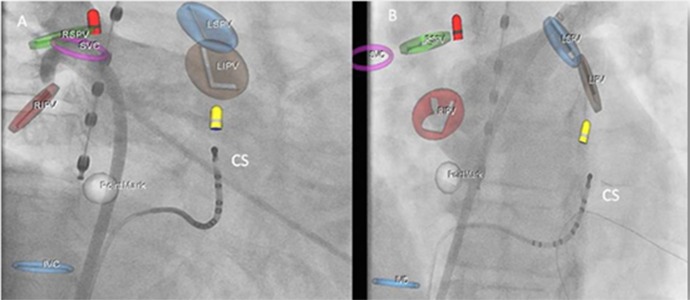
Image integration is used by many electrophysiologists for catheter ablation of AF in order to further increase the understanding of the patient’s complex atrial anatomy. It may enhance recognition of important anatomical variations, particularly concerning the pulmonary vein-atrial junction and the ridge between the left pulmonary veins and the left atrial appendage. In most cases, CT or MRI data, which were acquired prior to the procedure, are integrated in the EAMS. After image processing (segmentation), 3D images are either merged or fused with the 3D reconstructions Figure 1 with fusion usually requiring a more extensive registration process.[24] Utilization of intracardiac echocardiography (ICE) enables non-fluoroscopic real-time imaging allowing for visualization of mapping/ablation catheters, identification of various important anatomical structures (e.g. LA-PV junction, esophagus), guidance of transseptal puncture, monitoring catheter-tissue-contact, and early detection of complications such as pericardial effusion, thrombus formation, or tissue overheating (microbubble formation).[26-28] The most widely used ICE technology runs integrated in the Carto® system (CartoSound®, Biosense Webster). It uses a phased-array ultrasound tipped catheter consisting of a 64-element transducer (Sound[29] Star® Catheter, Biosense Webster). The high-resolution, multiple-frequency transducer (5-10 MHz) is incorporated into a 10F steerable catheter and provides 90° sector images with depth control. The CartoSound® module is capable of creating 3D models by combining multiple 2D ultrasound cross sections generated by the transducer.[30] The latter can be merged with segmented CT/MRI left atrial models.[29] The technology allows improvement in success and complication rates as well as shortening of LA catheter dwell and fluoroscopy times when compared with the fluoroscopy-only approach.[26] However, intracardiac ultrasound adds a non-negligible cost to the procedure, which has impeded widespread use of this technology. Another potential disadvantage is the requirement of an additional 11F sheath for transducer introduction, potentially raising the risk of femoral access complications.
Figure 1. A. Segmented CT model of the left atrium. B. Left atrial reconstruction created by the roving catheter using the FAM tool of CARTO3®. C. Merged LA model.
Clinical Benefit of EAMS use in AF Ablation
Comparative studies have shown that by means of the 3D EAMS both, radiation exposure and procedure duration can be significantly shortened versus conventional fluoroscopy-guided AF ablation procedures.[31,32] Small single-center studies comparing the two systems in AF ablation directly demonstrated similar clinical results, but advantages of Carto® over EnsiteNavX® in terms of fluoroscopy use and procedure durations.[33,34]
Further clinical benefits of image integration remain controversial. Retrospective comparative studies showed evidence of reduced fluoroscopy times, improved success rates and lower complication rates such as pulmonary vein stenosis.[35,36] These benefits, however, could not be entirely reproduced in prospective studies, particularly not the improved efficacy rates.[37] There are significant limitations of integration of virtual models, which require consideration. First, contemporary 3D models represent static representations of a moving organ and not all motion artifacts from the beating heart or respiration can currently be entirely compensated. Second, the different volume status during CT/MRI and during the procedure may result in mismatches of image integration. Further disadvantages relate to the additional radiation exposure due to CT scans, to potential kidney damage or allergic reactions induced by contrast agents, or to an additional logistic and economic burden. Despite these limitations, image integration is considered useful by many electrophysiologists and applied routinely.
Contact Force
Besides delivered power and catheter stability, adequate tissue contact by radiofrequency catheters are the variables needed to achieve durable and transmural lesions and to prevent complications secondary to excessive force. So far, electrophysiologists used signs of contact like the mechanical feedback at the catheter handle, observation of catheter manipulation on fluoroscopy, and rather inaccurate surrogate measures such as intracardiac electrograms and impedance changes during ablation.[38] Another optional technology, which has found its integration into EAMS relates to monitoring of electrode-tissue contact force. Currently, the SmartTouch® catheter (Biosense Webster), and since recently the TactiCath® Quartz catheter (St Jude Medical) provide continuous real-time measurements of contact force (scaled in grams), which is visualized in the EAMS. In the Carto® system, the contact force measurements and the force vector at the catheter tip are illustrated on the EAMS screen. Optionally, ablation points can be created dependent on the prespecified force-time integral[39] (VisiTag®). In the EnsiteNavX® system, contact force data and the direction of forces (axial or lateral) are depicted in a separate screen tab. The safety and effectiveness of the technologies have been evaluated both in prospective multicenter and smaller single-center studies. Energy delivery seem to be optimal in terms of efficacy (PV reconnection rate and clinical outcome), risks (steam pops, perforation, collateral thermal damage), and procedural parameters (procedural, ablation and fluoroscopy times), when contact forces are kept between 10 and 30g.[40-44]
Remote catheter navigation and EAMS
Both remote navigation systems are integrated with 3D EAMS. The Sensei® electromechanical navigation system (Hansen medical, Mountain View, CA, USA) is designed for integration with EnsiteNavX®, and the Niobe® magnetic navigation system (Stereotaxis, St. Louis, MO, USA) fully integrates with CartoRMT®, although use with EnsiteNavX® is feasible. In the robotic system, adjustments of the map orientation can be performed with a roller ball in the workstation simultaneously with controlling the catheter using the joystick. Coaxial forces applied to the catheter tip can be measured and displayed as a realtime waveform on the main screen as visual feedback of force (Intellisense® technology). The operator can set a warning level resulting in a colour change of the virtual catheter tip and the pressure waveform as well as a mechanical feedback alarm at the 3D control mouse. In the magnetic system, complete EAMS integration allows use of the computer mouse for both, moving the magnetic vector (and catheter) and controlling the map on the same window. Magnetic vector orientation is displayed on the map allowing for intuitive vector movements. Moreover, the display capabilities of the Odyssey system allow for simultaneous projection of mapping integrated in the fluoroscopy environment as well as magnetic navigation and ECG recordings. Recently, a meta-analysis that included 941 patients demonstrated that remote magnetic catheter navigation was associated with less periprocedural complications and with substantially less fluoroscopy time. However, clinical success rates were not superior to manual catheter navigation and total procedure times were longer.[45] The cost issue involving initial acquisition costs as well as disposable material costs – being additions to the overall cost of the procedure - continues to be a major concern.
Description of established mapping strategies
During the index procedure, anatomically-based PVI or empirical lesion sets usually do not require sophisticated mapping strategies. In these cases, EAMS are used to support continuous lesions deployment within the left atrium. Ring catheters usually confirm bidirectional block.
However, certain methods of substrate modification, or characterization of extra-PV foci and/or secondary atrial tachycardias as well as identification of conducting gaps within ablation lines at re-do procedures may require various mapping strategies supported by EAMS.[46-49]
Activation mapping
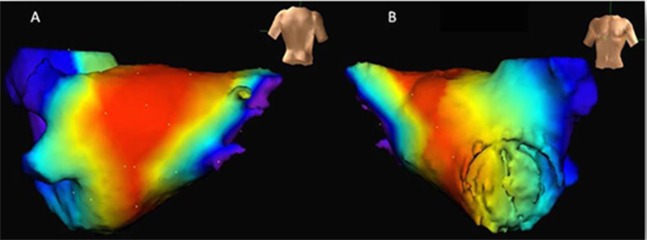
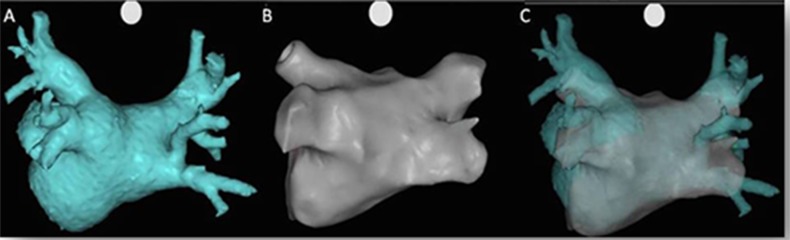
Activation mapping requires information about the timing of bipolar electrical signals of multiple surface points in relation to a stable reference signal (e.g. from the coronary sinus catheter). This process can be successfully shortened with the use of multielectrode catheters like the PentaRay® catheter (Biosense Webster). The activation sequence is then depicted in a color-coded fashion on the 3D model as an isochronal map (Figure 2). With this technique, focal or microreentry sources, as well as gaps within incomplete linear lesions can be easily localized. Macroreentrant tachycardias are more challenging to interpret and require the description of the complete tachycardia cycle length. In these situations, termination of the tachycardia by additional strategic ablation lesions requires consideration of anatomical (e.g. valves, vessels) and structural (e.g. scars, slow conduction zones) obstacles.[46,48]
Figure 2. Activation map of an atrial tachycardia depicted on a left atrial geometry created with the FAM tool of CARTO3® (anteroposterior view). The color-coded scale visualizes earlier activated regions (red/yellow color) in comparison to later activated (green/blue color) areas. In this case, an atrial focus is postulated at the roof of left atrium, adjacent to the left upper pulmonary vein.
Entrainment mapping
As mentioned above, interpretation of activation maps of macroreentry atrial tachycardias can be challenging, particularly for the identification of the leading circuit and critical isthmus sites. Entrainment mapping has been proven useful in characterizing reentry circuits, which can be applied in the context of electroanatomical mapping. To do so, a map of post-pacing intervals is displayed on the EAMS instead of the color-coded display of activation times. For this purpose, activation times are manually replaced by post-pacing intervals at all locations where entrainment maneuvers were successfully performed. In the final map, the reentry circuit is characterized by a route of “earliest” activation (Figure 3). Esato et al. studied 26 patients presenting with macroreentry atrial tachycardia. Color-coded 3D post-pacing interval maps resulted in accurate visualization of the reentrant circuit in all study patients. Strategic linear lesions were then placed in the right or left atrium in order to interrupt impulse propagation. A procedural success of 100% was reported, while 88% of patients remained free of any tachycardia recurrences during 10 months of follow-up.[50]
Figure 3. A map of post-pacing intervals is displayed on the electroanatomical model created by the EnSite NavX Velocity® system. Times are manually annotated and reflect the post-pacing intervals at all sites where entrainment maneuvers were successfully performed. In this case, red color portrays pathway of shortest post-pacing intervals closest to the reentry circuit. In the final map, the reentry circuit is characterized by a route of “earliest” activation depicting a roof-dependent atrial flutter (A. Posterior-anterior view, B. Anterior-posterior view.).
Mapping of complex fractionated atrial electrograms
Complex fractionated atrial electrograms (CFAEs) are defined as low voltage (≤0.15 mV) multiple potential signals with one or both of the following characteristics: (1) atrial EGMs composed of two deflections or more, and/or perturbations of the baseline with continuous deflection of a prolonged activation complex; (2) atrial EGMs with a very short cycle length (≤120 milliseconds), with or without multiple potentials. Miscellaneous mechanisms have been proposed to explain the genesis of CFAEs. In some cases, these mechanisms are thought to be related to factors which perpetuate AF, while in others they are considered to be passive consequences of rapid AF drivers originating e.g. in the PVs.[51] Supplementary ablation of CFAEs has been shown to improve outcomes preferentially in patients with persistent and long-lasting persistent AF.[32] At least in part, some of the beneficial effects of CFAE ablation may be mitigated by higher rates of post-procedural atrial tachycardias.[52] Contemporary EAMS integrate automated algorithms which enable acquisition of CFAEs and construction of corresponding maps.[53] So far, these algorithms for mapping of electroanatomical CFAEs have not yet been proven beneficial in terms of procedure time or clinical outcomes when compared to conventional CFAE mapping and ablation.[54]
Multipolar mapping and ablation of AF
Simultaneous multipolar ablation catheters have been proposed to simplify PV isolation. Recently, a new multipolar open-irrigated radiofrequency ablation catheter (nMARQ, Biosense-Webster) has been developed, which can be used with the Carto3® EAMS. The catheter is equipped with a circular or semilunar distal tip section that contains 10 platinum ring electrodes. A dedicated multi-channel radiofrequency energy generator delivers unipolar or bipolar radiofrequency energy over multiple electrodes. Feasibility and safety of ablation with the nMARQ® catheter has been shown in patients with paroxysmal AF.[55,56] However, issues regarding silent cerebral ischemia remain as observed with the nonirrigated duty-cycled bipolar and unipolar radiofrequency ablation PVAC® catheter (Medtronic, Minneapolis, MN, USA) remain to be addressed.[57,58]
New electroanatomical mapping developments and technologies
Mapping of high dominant frequencies
Experimental studies have demonstrated that AF may be driven by localized reentrant sources known as rotors and/or focal impulses, which result in a hierarchical distribution of frequencies throughout the atria. These rotors can be identified by high-resolution signal analysis of the Fourier power spectrum with its dominant frequency (DF).[59] Contemporary EAMS allow for the automated display of color-coded 3D DF maps. High DF sites are usually defined as sites demonstrating a 20% frequency gradient relative to the surrounding tissue, representing possible targets for ablation. Multiple DF sites are usually found in individual patients. In patients with paroxysmal AF, DF sources were more often found close to the PVs, whereas in permanent AF, DF sites were more often located in the atria. Regardless of the specific location, atrial activation by high-frequency sources results in inter-atrial DF gradients. Ablation of DF sites may result in significant slowing of AFCL, reduction of AF inducibility, and even AF termination most notably in patients with paroxysmal AF, with sinus rhythm maintenance predicted by elimination of preexisting left to right atrial DF gradients.[60,61] There is concern about the spatiotemporal stability of DF sites detected intra-procedurally, and consecutively about their role as fixed AF drivers. Thus, large-scale randomized clinical studies are warranted to determine the role of high DF ablation, as a stand-alone strategy or as an adjunct to PV isolation. In this regard, two novel technologies may contribute relevant findings: one is the use of modern body surface mapping technology, which may prove valuable in the non-invasive determination of AF mechanisms and preparation of ablation procedures.[62,63] The other is a novel computational approach to map stable sources as potential targets of AF ablation.
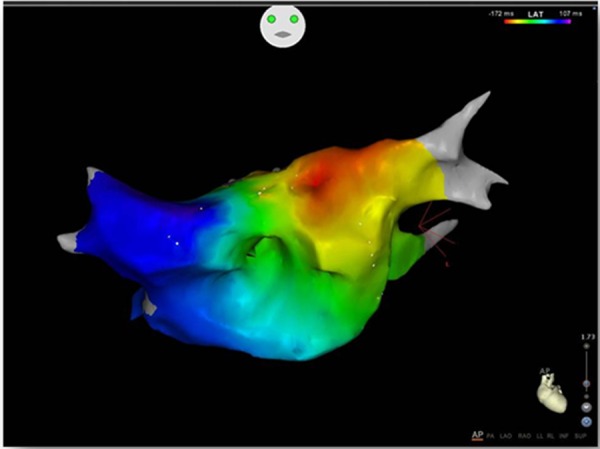
Focal Impulse and Rotor mapping and modulation
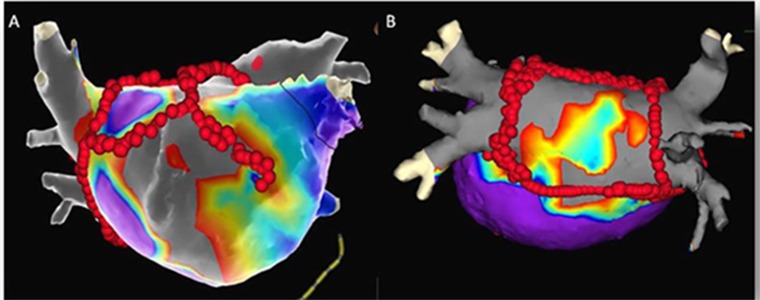
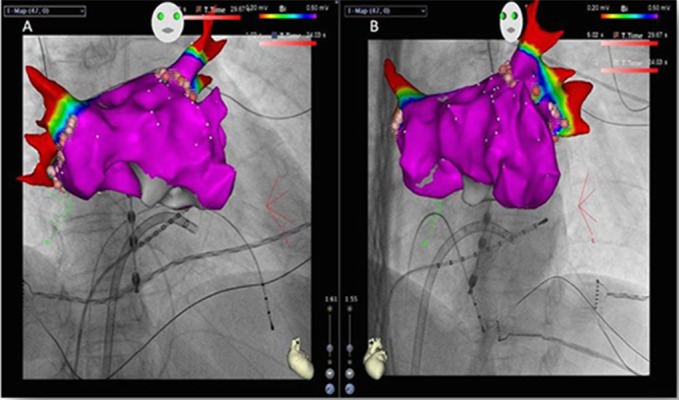
The concept of focal impulse and rotor modulation (FIRM) is a promising concept for substrate modification in AF patients.[64] For this technique, 64-pole basket catheters are used for panoramic left (and right) atrial mapping during AF. The RhythmView® mapping system (Topera, Menlo Park, CA, USA) is subsequently used to create AF propagation maps. Rotors are defined as stable and sustained spiral activation around a center of rotation, whereas focal impulses are defined by centrifugal activation from a source. Focal target zones are located by their electrode coordinates, where radiofrequency energy using a conventional ablation catheter is usually applied for 15–30 sec up to 10 min or achievement of AF termination or slowing. Due to the fact, that (EAMS-supported) PV isolation should follow, EnsiteNavX® or Carto® can be used to support FIRM. EAMS may then be used for nonfluoroscopic tracking of the basket catheters and simultaneous creation of atrial geometries (Figure 4), which may then be fused with 3D CT/MR images. Additionally, FIRM target and ablation sites can be marked within these models, which eliminates errors from basket catheter dislocation. Clinical studies have shown, that usually 2-3 rotors or focal impulses can be demonstrated in the vast majority of patients. Direct or coincidental FIRM on top of conventional PVI was able to improve mid-term and long-term AF ablation outcome.[64-66] However, similar to other technologies, which are used on top of conventional AF ablation, additional costs remain an issue.
Figure 4. Illustration of focal impulse and rotor modulation (FIRM) supported by conventional electroanatomical mapping system. Right and left atrial geometries created with EnsiteNavX Velocity® (modified anteroposterior view), the left atrial reconstruction being fused with a 3D reconstruction derived from computed tomography. The 64-polar basket catheter is visualized within the left atrium. Also shown: decapolar catheter in the coronary sinus (yellow), tip of ablation catheter within left superior PV (green), 3D marker points illustrating coronary sinus ostium (yellow) and FIRM ablation sites (blue, green).
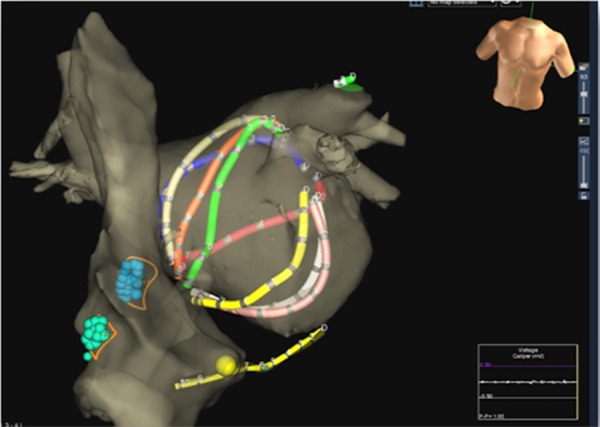
Voltage mapping and substrate imaging
Low-voltage areas (<0.5 mV) in the left atrium have been associated with endocardial scar and/or structural defects and their presence has been shown to result in impaired outcomes after PVI.[67-71] Targeting low-voltage zones by radiofrequency substrate modification similar to a substrate modification for unstable ventricular tachycardias may be a valuable therapeutic option. To evaluate this option, our group performed left atrial voltage maps in 178 AF patients and observed low-voltage areas outside the encircled pulmonary veins in 35% of patients with persistent AF and in 10% of patients with paroxysmal AF, preferentially in the septal, anterior, and posterior left atrium (Figure 5). All patients without low-voltage areas were left without further substrate modifications. One-year freedom of atrial arrhythmias was 62% in these patients without any low-voltage areas after a single procedure. A comparison group of 26 patients with low-voltage and PVI only had a one-year success rate of 23%. On the other hand, patients with low-voltage areas and strategic substrate modification targeting the low voltage areas had a 70% arrhythmia-free survival rate after one year.[72] These results may indicate that almost two thirds of all persistent AF patients may not require additional substrate modifications. Moreover, in patients with a structurally diseased left atrium, an individualized voltage-based substrate modification may compensate for the impaired outcomes, at least within a time-frame of one year. Prospective, randomized clinical studies are necessary to clarify the role of a voltage-based AF ablation in comparison to established strategies.
Figure 5. Voltage map projected on a 3D model of the left atrium after registration of a segmented CT geometry, created by the EnSite NavX Velocity® System. Gray areas correspond to scar (electrograms amplitudes <0.2 mV), purple areas correspond to normal voltage amplitude >0.5 mV, red/yellow colors depict areas with reduced (low) electrograms voltage amplitudes: 0.2-0.5 mV. Strategic radiofrequency lesions have been placed (red dots) after circumferential pulmonary vein isolation in order to prevent left atrial macro-reentrant tachycardias having their critical isthmus sites within the low voltage zones (left), or to exclude diseased atrial tissue (box lesions, right).
As mentioned earlier, scarred and fibrotic and/or diseased (remodeled) atrial tissue may also be identified by MRI late gadolinium enhancement (LGE).[69] Recently, the DECAAF study demonstrated that atrial tissue fibrosis estimated by LGE MRI pre-procedurally was an independent AF recurrence factor in patients ablated for AF.[68] Arrhythmia recurrence was related to LGE burden, ranging from 15% for stage 1 fibrosis (<10% of the atrial wall) to 69% for stage 4 fibrosis (≥30% of the atrial wall) after 1-2 years. Integration of LGE data into electroanatomical maps for targeted substrate modification represents a promising ablation strategy, either for the index procedure or for redo procedures requiring gap detection.[73-75]
Ripple Mapping
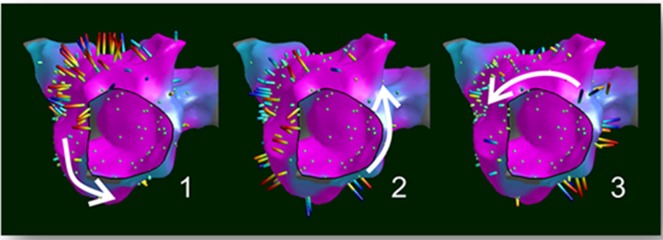
The automated mapping algorithms integrated in contemporary EAMS can be susceptible to annotation and interpolation errors. Even manual point-by-point verification of annotated points is prone to incorrect judgment regarding signal selection, inappropriate selection of the window-of-interest or the presence of fragmented, double-potentials or areas of very-low continuous potentials where annotation can be challenging. Furthermore, many of these informative electrogram characteristics are lost when a single timing point is assigned to generate activation maps. Ripple Mapping is a novel technique that displays electrogram time-voltage data simultaneously as dynamic bars on CARTO surface shells to overcome these limitations.[76] Electrograms are visualized on the 3D geometries as color bars corresponding to 3D coordinates, changing colors and dimensions according to the voltage-time relationship, time-gated to a pre-selected electrogram used as reference (Figure 6). Differentiation of these bars based on time gives the operator the impression of a “wave-like” movement of the propagation, without any manual or automatic annotations. The feasibility of “ripple mapping” for rapid diagnosis of atrial tachycardias has been reported recently, demonstrating higher diagnostic accuracy compared to conventional 3D activation mapping.[77] A current limitation of this approach is the fact, that maps are generated offline and post-processing can take time. In conclusion, ripple mapping has the potential to simplify electroanatomical mapping and to minimize operator-dependence. However, the extent to which this technology will be incorporated into “real-time” application will require prospective evaluation and head-to-head comparison with other mapping modules.
Figure 6. Electroanatomical ripple map (Carto3R, postprocessed) illustrating counterclockwise perimitral atrial flutter at three different time points of the tachycardia cycle (1-3, taken from a movie). Electrograms do not require manual annotation and are displayed as dynamic bars protruding from the surface changing in length and color depending on the local electrogram voltage-time relationship (Courtesy of Nick Linton, Imperial College Healthcare NHS Trust, London, UK).
Integrated use of non-fluoroscopic and fluoroscopic techniques
A major limitation of established EAMS is the absence of direct flow of imaging information from the x-ray system. The MediGuide® Technology (St Jude Medical) has overcome this constraint by using electromagnetic tracking and small (<1 mm) sensors embedded in a multitude of medical devices such as wires, sheaths, and catheters to enable tracking over pre-recorded fluoroscopy loops. With the integration of the electromagnetic transmitters to the x-ray flat-panel detector, fluoroscopy and magnetic tracking are automatically aligned within the 3D working space. This combination allows real-time non-fluoroscopic visualization of sensor position and orientation on pre-recorded loops. The system displays two screens simultaneously, allowing for a virtual biplane 3D sensor visualization (Figure 7). A reference sensor on the patient’s chest supports compensation of motion artifacts, and the electrocardiogram (ECG) is used to adapt the speed of the cine-loop display. Integration of MediGuide® tracking data into the Ensite NavX® system improves its compensation for field distortions, enabling creation of very accurate chamber reconstructions. For AF catheter ablation in particular, catheters with sensors at their distal tips are used and left atrial angiographies instead of native fluoroscopy loops serve as the environment for non-fluoroscopic tracking. Comparative studies have shown significant reduction in fluoroscopy requirements when MediGuide is used supplementary to Ensite NavX®. After a steep learning curve, less than 3 minutes of fluoroscopy time, mainly used for the transseptal puncture, is currently used to complete an entire AF ablation procedure without any negative impacts on procedure time, efficacy and safety.[78-80]
Figure 7. Snapshot of two simultaneously displayed MediGuide® screens showing the left atrial mapping process during catheter ablation of atrial fibrillation. Sensors at the tip of various catheters are projected in real-time on pre-recorded loops (red tip for mapping catheter, yellow tip for coronary sinus catheter). Left (right anterior oblique view): Background movie showing semi-selective pulmonary vein angiography of the right upper pulmonary vein. Right (left anterior oblique view): Pre-recorded semi-selective left upper pulmonary vein angiography was chosen as the background for non-fluoroscopic sensor tracking. Various markers were set with the MediGuide® system (RSPV, RIPV, LSPV, and LIPV for ostia of right/left superior/inferior pulmonary veins; SVC, IVC for superior/inferior caval vein; PointMark for oval fossa). At the time of recording the background loops, the transseptal sheath, coronary sinus catheter (CS), and esophageal probe were already in place.
A module for the integration of electroanatomical mapping and x-ray images/movies has also been developed for the Carto3® system (Carto UniVu®), similar to the technology that has already been used for remote catheter navigation (Navigant®, Stereotaxis). Communication between the x-ray system and the EAMS on the hardware level allow co-registration of real-time electromagnetic mapping within the fluoroscopic environment. Simultaneous display of two different projections allows for a virtual biplane view (Figure 8). Anecdotal experiences have shown potential to significantly reduce fluoroscopy use. However, clinical studies are needed to further define the clinical value of this new development.
Figure 8. Left atrial reconstruction created with CARTO UniVu,® RAO and LAO projections. Following registration of the x-ray system to the EAMS, multiple fluoroscopy snapshots can be recorded. The reconstructed 3D model is then projected and auto-registered into the fluoroscopic environment. In this example, a 3D voltage map has been created. Red color indicates areas with absence of signals due to low-voltage/scar. In this case, no potentials are found within the pulmonary veins after wide atrial isolation. Purple color indicates areas of ‘healthy’ left atrium with voltage amplitudes above 0.5 mV.
Automatic high-resolution mapping
Very recently, a novel EAMS (Rhythmia Mapping®, Boston Scientific, Marlborough, Massachusetts, USA) received FDA clearance and CE mark approval. The mapping system uses a specially-designed mini basket array with 8 splines, each containing 8 electrodes attached to a bi-directional deflectable catheter (IntellaMap Orion® High Resolution Mapping Catheter). Similar to the CARTO3® technology, the RHYTHMIA® system uses a hybrid of magnetic with one sensor at the catheter tip and impedance-based tracking with all 64 electrodes for catheter navigation and geometry creation. The major advantage of the system is the rapid and automatic acquisition of high-resolution electroanatomical contact maps without the need for extensive manual annotation (Figure 9). For this purpose, the system selects cardiac beats considering stability of cycle length, timing, location, and the respiratory cycle. Far-field components are reduced by combining unipolar and bipolar electrograms. Nakagawa et al. evaluated the features of the system in a feasibility study involving electroanatomical mapping in canine models.[81] Right atrial electroanatomical activation maps with more than 4,000 electrograms were created within 7 minutes (medians). Furthermore, the low noise level in the system of 0.01 mV allowed the recording of very low-amplitude potentials indicative of scarred atrial myocardium. Complete linear lesions after radiofrequency ablation, as well gaps within incomplete lines were accurately detected with minor manual corrections. In another study, the technology has been used in a porcine model for detailed assessment of sinus node activation.[82] Application of this technology in patients will elucidate the utility of the system in a clinical setting.
Figure 9. 3D models of porcine right and left atria created with Rhythmia Mapping® System (left: modified posterior-anterior view, right: left anterior oblique view). A color-coded sinus rhythm activation map is depicted showing earliest activation in red. More than 4,000 electrograms were taken and automatically analyzed from >400 beats within less than 7 minutes using the basket catheter.
Conclusion
There is no doubt, that the introduction and advances of electroanatomical mapping systems have paved the way to facilitate PV isolation and to serve as a prerequisite for more complex substrate modification and for successful treatment of diverse primary or postinterventional atrial tachycardias. Carto® and EnsiteNavX®, which are fundamentally dissimilar in terms of tracking technology, are successfully used in the context of AF ablation and have evolved as the standard EAMS today. A variety of useful tools (optional in part) have been developed and EAMS-based strategies have emerged recently. Principally, these novelties raise a claim to make procedures shorter, easier, less dependent on fluoroscopy, safer, and last but not least more effective. All of these goals should at best be achieved with reasonable costs. Image integration is well established in many labs and results in less fluoroscopy use. Due to improved awareness of the individual anatomy, prevention of complications like pulmonary vein stenosis or esophageal thermal damage may be expected, but has not yet been proven. Precise autoregistration of 3D models may represent another important step forward towards reduction of procedure duration. Activation mapping using (multielectrode) catheters as well as entrainment mapping already belongs to the standard armamentarium for ablation of complex substrates today. Innovative mapping approaches like ripple mapping may someday allow experienced operators to create maps of complex atrial tachycardias without assisting experts. Fluoroscopy-integrated electroanatomical mapping enables the operator to perform catheter ablation of (even complex) AF cases with a minimum use of ionizing radiation. Similar effects have been found for remote navigation systems. However, these technologies require cost-intensive hardware installations. Therefore, further development of these technologies should enter the next stage to improve efficacy and lower risks of the procedure. An open design resulting the applicability on other fluoro-intensive interventions (like left ventricular lead implantation in cardiac resynchronization therapy) may serve as another argument for such a technology.
Enhanced efficacy remains one of the most important goals of future advances in ablation tools. In this regard, improvements in energy delivery and ablation strategy play a major role, whereas the EAMS may rather have an indirect, permissive role. Contact force monitoring seems to be a promising application with reasonable additive costs. Innovative strategies like voltage-based left atrial substrate modification possess the potential of increased efficacy, although not yet proven in prospective studies. Scar-based strategies may additionally benefit from scar visualization by image integration (i.e. delayed enhancement MRI) in the future. Novel systems capable of automated high-density mapping may prove valuable for electrogram-based ablation strategies (voltage or CFAE).
Ultimately, transferring the patient into the MRI suite for AF therapy represents a desirable future task. The potential to visualize the anatomy, to identify pathomorphology, to monitor lesion development, to detect complications, and to track the catheters simultaneously in real-time in a fluoroscopy-free environment is an exciting project.[83]
Disclosure
S.R. and P.S. have received modest lecture honoraria and congress sponsoring from St. Jude Medical and Biosense. A.B. has received modest lecture honoraria and congress sponsoring from Boston Scientific. G.H. has received modest lecture honoraria from St. Jude Medical, and Biosense and is a member of the Biosense and St. Jude Medical advisory board.
References
- Reardon M, Camm A J. Atrial fibrillation in the elderly. Clin Cardiol. 1996 Oct;19 (10):765–75. doi: 10.1002/clc.4960191003. [DOI] [PubMed] [Google Scholar]
- Jaïs P, Haïssaguerre M, Shah D C, Chouairi S, Gencel L, Hocini M, Clémenty J. A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation. 1997 Feb 4;95 (3):572–6. doi: 10.1161/01.cir.95.3.572. [DOI] [PubMed] [Google Scholar]
- Haïssaguerre M, Marcus F I, Fischer B, Clémenty J. Radiofrequency catheter ablation in unusual mechanisms of atrial fibrillation: report of three cases. J. Cardiovasc. Electrophysiol. 1994 Sep;5 (9):743–51. doi: 10.1111/j.1540-8167.1994.tb01197.x. [DOI] [PubMed] [Google Scholar]
- Haïssaguerre M, Jaïs P, Shah D C, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Métayer P, Clémenty J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 1998 Sep 3;339 (10):659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- Arentz Thomas, Weber Reinhold, Bürkle Gerd, Herrera Claudia, Blum Thomas, Stockinger Jochem, Minners Jan, Neumann Franz Josef, Kalusche Dietrich. Small or large isolation areas around the pulmonary veins for the treatment of atrial fibrillation? Results from a prospective randomized study. Circulation. 2007 Jun 19;115 (24):3057–63. doi: 10.1161/CIRCULATIONAHA.107.690578. [DOI] [PubMed] [Google Scholar]
- Ouyang Feifan, Antz Matthias, Ernst Sabine, Hachiya Hitoshi, Mavrakis Hercules, Deger Florian T, Schaumann Anselm, Chun Julian, Falk Peter, Hennig Detlef, Liu Xingpeng, Bänsch Dietmar, Kuck Karl-Heinz. Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation. 2005 Jan 18;111 (2):127–35. doi: 10.1161/01.CIR.0000151289.73085.36. [DOI] [PubMed] [Google Scholar]
- Ouyang Feifan, Tilz Roland, Chun Julian, Schmidt Boris, Wissner Erik, Zerm Thomas, Neven Kars, Köktürk Bulent, Konstantinidou Melanie, Metzner Andreas, Fuernkranz Alexander, Kuck Karl-Heinz. Long-term results of catheter ablation in paroxysmal atrial fibrillation: lessons from a 5-year follow-up. Circulation. 2010 Dec 7;122 (23):2368–77. doi: 10.1161/CIRCULATIONAHA.110.946806. [DOI] [PubMed] [Google Scholar]
- Calkins Hugh, Kuck Karl Heinz, Cappato Riccardo, Brugada Josep, Camm A John, Chen Shih-Ann, Crijns Harry J G, Damiano Ralph J, Davies D Wyn, DiMarco John, Edgerton James, Ellenbogen Kenneth, Ezekowitz Michael D, Haines David E, Haissaguerre Michel, Hindricks Gerhard, Iesaka Yoshito, Jackman Warren, Jalife Jose, Jais Pierre, Kalman Jonathan, Keane David, Kim Young-Hoon, Kirchhof Paulus, Klein George, Kottkamp Hans, Kumagai Koichiro, Lindsay Bruce D, Mansour Moussa, Marchlinski Francis E, McCarthy Patrick M, Mont J Lluis, Morady Fred, Nademanee Koonlawee, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Packer Douglas L, Pappone Carlo, Prystowsky Eric, Raviele Antonio, Reddy Vivek, Ruskin Jeremy N, Shemin Richard J, Tsao Hsuan-Ming, Wilber David. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012 Apr;14 (4):528–606. doi: 10.1093/europace/eus027. [DOI] [PubMed] [Google Scholar]
- Camm A John, Lip Gregory Y H, De Caterina Raffaele, Savelieva Irene, Atar Dan, Hohnloser Stefan H, Hindricks Gerhard, Kirchhof Paulus. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012 Nov;33 (21):2719–47. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014 Dec 2;64 (21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Elayi Claude S, Verma Atul, Di Biase Luigi, Ching Chi Keong, Patel Dimpi, Barrett Conor, Martin David, Rong Bai, Fahmy Tamer S, Khaykin Yaariv, Hongo Richard, Hao Steven, Pelargonio Gemma, Dello Russo Antonio, Casella Michela, Santarelli Pietro, Potenza Domenico, Fanelli Raffaele, Massaro Raimondo, Arruda Mauricio, Schweikert Robert A, Natale Andrea. Ablation for longstanding permanent atrial fibrillation: results from a randomized study comparing three different strategies. Heart Rhythm. 2008 Dec;5 (12):1658–64. doi: 10.1016/j.hrthm.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Oral Hakan, Knight Bradley P, Tada Hiroshi, Ozaydin Mehmet, Chugh Aman, Hassan Sohail, Scharf Christoph, Lai Steve W K, Greenstein Radmira, Pelosi Frank, Strickberger S Adam, Morady Fred. Pulmonary vein isolation for paroxysmal and persistent atrial fibrillation. Circulation. 2002 Mar 5;105 (9):1077–81. doi: 10.1161/hc0902.104712. [DOI] [PubMed] [Google Scholar]
- Hunter R J, Berriman T J, Diab I, Baker V, Finlay M, Richmond L, Duncan E, Kamdar R, Thomas G, Abrams D, Dhinoja M, Sporton S, Earley M J, Schilling R J. Long-term efficacy of catheter ablation for atrial fibrillation: impact of additional targeting of fractionated electrograms. Heart. 2010 Sep;96 (17):1372–8. doi: 10.1136/hrt.2009.188128. [DOI] [PubMed] [Google Scholar]
- O'Neill Mark D, Wright Matthew, Knecht Sébastien, Jaïs Pierre, Hocini Mélèze, Takahashi Yoshihide, Jönsson Anders, Sacher Frédéric, Matsuo Seiichiro, Lim Kang Teng, Arantes Leonardo, Derval Nicolas, Lellouche Nicholas, Nault Isabelle, Bordachar Pierre, Clémenty Jacques, Haïssaguerre Michel. Long-term follow-up of persistent atrial fibrillation ablation using termination as a procedural endpoint. Eur. Heart J. 2009 May;30 (9):1105–12. doi: 10.1093/eurheartj/ehp063. [DOI] [PubMed] [Google Scholar]
- Wittkampf F H, Wever E F, Derksen R, Wilde A A, Ramanna H, Hauer R N, Robles de Medina E O. LocaLisa: new technique for real-time 3-dimensional localization of regular intracardiac electrodes. Circulation. 1999 Mar 16;99 (10):1312–7. doi: 10.1161/01.cir.99.10.1312. [DOI] [PubMed] [Google Scholar]
- Kesek Milos, Wallenius Niklas, Rönn Folke, Höglund Niklas, Jensen Steen. Reduction of fluoroscopy duration in radiofrequency ablation obtained by the use of a non-fluoroscopic catheter navigation system. Europace. 2006 Dec;8 (12):1027–30. doi: 10.1093/europace/eul127. [DOI] [PubMed] [Google Scholar]
- Rolf Sascha, Holzmeister Johannes, Fruehwirth Marcel, Haverkamp Wilhelm. Idiopathic left ventricular tachycardia: procedural and fluoroscopy time saving ablation using LocaLisa navigation system. J. Cardiovasc. Electrophysiol. 2006 Feb;17 (2):214–5. doi: 10.1111/j.1540-8167.2005.00304.x. [DOI] [PubMed] [Google Scholar]
- Kirchhof Paulus, Loh Peter, Eckardt Lars, Ribbing Michael, Rolf Sascha, Eick Olaf, Wittkampf Fred, Borggrefe Martin, Breithardt G G ünter, Haverkamp Wilhelm. A novel nonfluoroscopic catheter visualization system (LocaLisa) to reduce radiation exposure during catheter ablation of supraventricular tachycardias. Am. J. Cardiol. 2002 Aug 1;90 (3):340–3. doi: 10.1016/s0002-9149(02)02481-5. [DOI] [PubMed] [Google Scholar]
- Macle Laurent, Jaïs Pierre, Scavée Christophe, Weerasooriya Rukshen, Hocini Mélèze, Shah Dipen C, Raybaud Florence, Choi Kee-Joon, Clémenty Jacques, Haïssaguerre Michel. Pulmonary vein disconnection using the LocaLisa three-dimensional nonfluoroscopic catheter imaging system. J. Cardiovasc. Electrophysiol. 2003 Jul;14 (7):693–7. doi: 10.1046/j.1540-8167.2003.03012.x. [DOI] [PubMed] [Google Scholar]
- Earley Mark J, Abrams Dominic J R, Sporton Simon C, Schilling Richard J. Validation of the noncontact mapping system in the left atrium during permanent atrial fibrillation and sinus rhythm. J. Am. Coll. Cardiol. 2006 Aug 1;48 (3):485–91. doi: 10.1016/j.jacc.2006.04.069. [DOI] [PubMed] [Google Scholar]
- Gepstein L, Hayam G, Ben-Haim S A. A novel method for nonfluoroscopic catheter-based electroanatomical mapping of the heart. In vitro and in vivo accuracy results. Circulation. 1997 Mar 18;95 (6):1611–22. doi: 10.1161/01.cir.95.6.1611. [DOI] [PubMed] [Google Scholar]
- Knackstedt Christian, Schauerte Patrick, Kirchhof Paulus. Electro-anatomic mapping systems in arrhythmias. Europace. 2008 Nov;10 Suppl 3 ():iii28–34. doi: 10.1093/europace/eun225. [DOI] [PubMed] [Google Scholar]
- Scaglione Marco, Biasco Luigi, Caponi Domenico, Anselmino Matteo, Negro Andrea, Di Donna Paolo, Corleto Antonella, Montefusco Antonio, Gaita Fiorenzo. Visualization of multiple catheters with electroanatomical mapping reduces X-ray exposure during atrial fibrillation ablation. Europace. 2011 Jul;13 (7):955–62. doi: 10.1093/europace/eur062. [DOI] [PubMed] [Google Scholar]
- Govil Ashul, Calkins Hugh, Spragg David D. Fusion of imaging technologies: how, when, and for whom? J Interv Card Electrophysiol. 2011 Dec;32 (3):195–203. doi: 10.1007/s10840-011-9616-7. [DOI] [PubMed] [Google Scholar]
- Eitel Charlotte, Hindricks Gerhard, Dagres Nikolaos, Sommer Philipp, Piorkowski Christopher. EnSite Velocity cardiac mapping system: a new platform for 3D mapping of cardiac arrhythmias. Expert Rev Med Devices. 2010 Mar;7 (2):185–92. doi: 10.1586/erd.10.1. [DOI] [PubMed] [Google Scholar]
- Marrouche Nassir F, Martin David O, Wazni Oussama, Gillinov A Marc, Klein Allan, Bhargava Mandeep, Saad Eduardo, Bash Dianna, Yamada Hirotsugu, Jaber Wael, Schweikert Robert, Tchou Patrick, Abdul-Karim Ahmad, Saliba Walid, Natale Andrea. Phased-array intracardiac echocardiography monitoring during pulmonary vein isolation in patients with atrial fibrillation: impact on outcome and complications. Circulation. 2003 Jun 3;107 (21):2710–6. doi: 10.1161/01.CIR.0000070541.83326.15. [DOI] [PubMed] [Google Scholar]
- Biermann Jürgen, Bode Christoph, Asbach Stefan. Intracardiac Echocardiography during Catheter-Based Ablation of Atrial Fibrillation. Cardiol Res Pract. 2012;2012:921746. doi: 10.1155/2012/921746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asbach Stefan, Biermann Jürgen, Bode Christoph, Faber Thomas S. Early Heparin Administration Reduces Risk for Left Atrial Thrombus Formation during Atrial Fibrillation Ablation Procedures. Cardiol Res Pract. 2011;2011:615087. doi: 10.4061/2011/615087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura Masaomi, Sasaki Shingo, Owada Shingen, Horiuchi Daisuke, Sasaki Kenichi, Itoh Taihei, Ishida Yuji, Kinjo Takahiko, Okumura Ken. Validation of accuracy of three-dimensional left atrial CartoSound™ and CT image integration: influence of respiratory phase and cardiac cycle. J. Cardiovasc. Electrophysiol. 2013 Sep;24 (9):1002–7. doi: 10.1111/jce.12170. [DOI] [PubMed] [Google Scholar]
- Tops Laurens F, Schalij Martin J, den Uijl Dennis W, Abraham Theodore P, Calkins Hugh, Bax Jeroen J. Image integration in catheter ablation of atrial fibrillation. Europace. 2008 Nov;10 Suppl 3 ():iii48–56. doi: 10.1093/europace/eun235. [DOI] [PubMed] [Google Scholar]
- Estner Heidi Luise, Deisenhofer Isabel, Luik Armin, Ndrepepa Gjin, von Bary Christian, Zrenner Bernhard, Schmitt Claus. Electrical isolation of pulmonary veins in patients with atrial fibrillation: reduction of fluoroscopy exposure and procedure duration by the use of a non-fluoroscopic navigation system (NavX). Europace. 2006 Aug;8 (8):583–7. doi: 10.1093/europace/eul079. [DOI] [PubMed] [Google Scholar]
- Rotter Martin, Takahashi Yoshihide, Sanders Prashanthan, Haïssaguerre Michel, Jaïs Pierre, Hsu Li-Fern, Sacher Fréderic, Pasquié Jean-Luc, Clementy Jacques, Hocini Mélèze. Reduction of fluoroscopy exposure and procedure duration during ablation of atrial fibrillation using a novel anatomical navigation system. Eur. Heart J. 2005 Jul;26 (14):1415–21. doi: 10.1093/eurheartj/ehi172. [DOI] [PubMed] [Google Scholar]
- Liu Xu, Wang Xin-hua, Gu Jia-ning, Zhou Li, Qiu Jian-hua. Electroanatomical systems to guided circumferential pulmonary veins ablation for atrial fibrillation: initial experience from comparison between the Ensite/NavX and CARTO system. Chin. Med. J. 2005 Jul 20;118 (14):1156–60. [PubMed] [Google Scholar]
- Khaykin Yaariv, Oosthuizen Richard, Zarnett Lauren, Wulffhart Zaev A, Whaley Bonnie, Hill Carol, Giewercer David, Verma Atul. CARTO-guided vs. NavX-guided pulmonary vein antrum isolation and pulmonary vein antrum isolation performed without 3-D mapping: effect of the 3-D mapping system on procedure duration and fluoroscopy time. J Interv Card Electrophysiol. 2011 Apr;30 (3):233–40. doi: 10.1007/s10840-010-9538-9. [DOI] [PubMed] [Google Scholar]
- Kistler Peter M, Rajappan Kim, Jahngir Mohammed, Earley Mark J, Harris Stuart, Abrams Dominic, Gupta Dhiraj, Liew Reginald, Ellis Stephen, Sporton Simon C, Schilling Richard J. The impact of CT image integration into an electroanatomic mapping system on clinical outcomes of catheter ablation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2006 Oct;17 (10):1093–101. doi: 10.1111/j.1540-8167.2006.00594.x. [DOI] [PubMed] [Google Scholar]
- Martinek Martin, Nesser Hans-Joachim, Aichinger Josef, Boehm Gernot, Purerfellner Helmut. Impact of integration of multislice computed tomography imaging into three-dimensional electroanatomic mapping on clinical outcomes, safety, and efficacy using radiofrequency ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2007 Oct;30 (10):1215–23. doi: 10.1111/j.1540-8159.2007.00843.x. [DOI] [PubMed] [Google Scholar]
- Kistler Peter M, Rajappan Kim, Harris Stuart, Earley Mark J, Richmond Laura, Sporton Simon C, Schilling Richard J. The impact of image integration on catheter ablation of atrial fibrillation using electroanatomic mapping: a prospective randomized study. Eur. Heart J. 2008 Dec;29 (24):3029–36. doi: 10.1093/eurheartj/ehn453. [DOI] [PubMed] [Google Scholar]
- Nakagawa Hiroshi, Kautzner Josef, Natale Andrea, Peichl Petr, Cihak Robert, Wichterle Dan, Ikeda Atsushi, Santangeli Pasquale, Di Biase Luigi, Jackman Warren M. Locations of high contact force during left atrial mapping in atrial fibrillation patients: electrogram amplitude and impedance are poor predictors of electrode-tissue contact force for ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2013 Aug;6 (4):746–53. doi: 10.1161/CIRCEP.113.978320. [DOI] [PubMed] [Google Scholar]
- Shah Dipen C, Lambert Hendrik, Nakagawa Hiroshi, Langenkamp Arne, Aeby Nicolas, Leo Giovanni. Area under the real-time contact force curve (force-time integral) predicts radiofrequency lesion size in an in vitro contractile model. J. Cardiovasc. Electrophysiol. 2010 Sep;21 (9):1038–43. doi: 10.1111/j.1540-8167.2010.01750.x. [DOI] [PubMed] [Google Scholar]
- Yokoyama Katsuaki, Nakagawa Hiroshi, Shah Dipen C, Lambert Hendrik, Leo Giovanni, Aeby Nicolas, Ikeda Atsushi, Pitha Jan V, Sharma Tushar, Lazzara Ralph, Jackman Warren M. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ Arrhythm Electrophysiol. 2008 Dec;1 (5):354–62. doi: 10.1161/CIRCEP.108.803650. [DOI] [PubMed] [Google Scholar]
- Reddy Vivek Y, Shah Dipen, Kautzner Josef, Schmidt Boris, Saoudi Nadir, Herrera Claudia, Jaïs Pierre, Hindricks Gerhard, Peichl Petr, Yulzari Aude, Lambert Hendrik, Neuzil Petr, Natale Andrea, Kuck Karl-Heinz. The relationship between contact force and clinical outcome during radiofrequency catheter ablation of atrial fibrillation in the TOCCATA study. Heart Rhythm. 2012 Nov;9 (11):1789–95. doi: 10.1016/j.hrthm.2012.07.016. [DOI] [PubMed] [Google Scholar]
- Stabile Giuseppe, Solimene Francesco, Calò Leonardo, Anselmino Matteo, Castro Antonello, Pratola Claudio, Golia Paolo, Bottoni Nicola, Grandinetti Giuseppe, De Simone Antonio, De Ponti Roberto, Dottori Serena, Bertaglia Emanuele. Catheter-tissue contact force for pulmonary veins isolation: a pilot multicentre study on effect on procedure and fluoroscopy time. Europace. 2014 Mar;16 (3):335–40. doi: 10.1093/europace/eut262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura Masaomi, Sasaki Shingo, Owada Shingen, Horiuchi Daisuke, Sasaki Kenichi, Itoh Taihei, Ishida Yuji, Kinjo Takahiko, Tomita Hirofumi, Okumura Ken. Comparison of lesion formation between contact force-guided and non-guided circumferential pulmonary vein isolation: a prospective, randomized study. Heart Rhythm. 2014 Jun;11 (6):984–91. doi: 10.1016/j.hrthm.2014.03.019. [DOI] [PubMed] [Google Scholar]
- Marijon Eloi, Fazaa Samia, Narayanan Kumar, Guy-Moyat Benoit, Bouzeman Abdeslam, Providencia Rui, Treguer Frederic, Combes Nicolas, Bortone Agustin, Boveda Serge, Combes Stephane, Albenque Jean-Paul. Real-time contact force sensing for pulmonary vein isolation in the setting of paroxysmal atrial fibrillation: procedural and 1-year results. J. Cardiovasc. Electrophysiol. 2014 Feb;25 (2):130–7. doi: 10.1111/jce.12303. [DOI] [PubMed] [Google Scholar]
- Proietti Riccardo, Pecoraro Valentina, Di Biase Luigi, Natale Andrea, Santangeli Pasquale, Viecca Maurizio, Sagone Antonio, Galli Alessio, Moja Lorenzo, Tagliabue Ludovica. Remote magnetic with open-irrigated catheter vs. manual navigation for ablation of atrial fibrillation: a systematic review and meta-analysis. Europace. 2013 Sep;15 (9):1241–8. doi: 10.1093/europace/eut058. [DOI] [PubMed] [Google Scholar]
- Chang Shih-Lin, Lin Yenn-Jiang, Tai Ching-Tai, Lo Li-Wei, Tuan Ta-Chuan, Udyavar Ameya R, Hu Yu-Feng, Chiang Shuo-Ju, Wongcharoen Wanwarang, Tsao Hsuan-Ming, Ueng Kwo-Chang, Higa Satoshi, Lee Pi-Chang, Chen Shih-Ann. Induced atrial tachycardia after circumferential pulmonary vein isolation of paroxysmal atrial fibrillation: electrophysiological characteristics and impact of catheter ablation on the follow-up results. J. Cardiovasc. Electrophysiol. 2009 Apr;20 (4):388–94. doi: 10.1111/j.1540-8167.2008.01358.x. [DOI] [PubMed] [Google Scholar]
- Gerstenfeld Edward P, Callans David J, Dixit Sanjay, Russo Andrea M, Nayak Hemal, Lin David, Pulliam Ward, Siddique Sultan, Marchlinski Francis E. Mechanisms of organized left atrial tachycardias occurring after pulmonary vein isolation. Circulation. 2004 Sep 14;110 (11):1351–7. doi: 10.1161/01.CIR.0000141369.50476.D3. [DOI] [PubMed] [Google Scholar]
- Gerstenfeld Edward P, Marchlinski Francis E. Mapping and ablation of left atrial tachycardias occurring after atrial fibrillation ablation. Heart Rhythm. 2007 Mar;4 (3 Suppl):S65–72. doi: 10.1016/j.hrthm.2007.01.024. [DOI] [PubMed] [Google Scholar]
- Mesas Cézar E, Pappone Carlo, Lang Christopher C E, Gugliotta Filippo, Tomita Takeshi, Vicedomini Gabriele, Sala Simone, Paglino Gabriele, Gulletta Simone, Ferro Amedeo, Santinelli Vincenzo. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: electroanatomic characterization and treatment. J. Am. Coll. Cardiol. 2004 Sep 1;44 (5):1071–9. doi: 10.1016/j.jacc.2004.05.072. [DOI] [PubMed] [Google Scholar]
- Esato Masahiro, Hindricks Gerhard, Sommer Philipp, Arya Arash, Gaspar Thomas, Bode Kerstin, Bollmann Andreas, Wetzel Ulrike, Hilbert Sebastian, Kircher Simon, Eitel Charlotte, Piorkowski Christopher. Color-coded three-dimensional entrainment mapping for analysis and treatment of atrial macroreentrant tachycardia. Heart Rhythm. 2009 Mar;6 (3):349–58. doi: 10.1016/j.hrthm.2008.12.013. [DOI] [PubMed] [Google Scholar]
- Miyamoto Koji, Tsuchiya Takeshi, Nagamoto Yasutsugu, Yamaguchi Takanori, Narita Sumito, Ando Shin-Ichi, Hayashida Kiyoshi, Tanioka Yoshito, Takahashi Naohiko. Characterization of bipolar electrograms during sinus rhythm for complex fractionated atrial electrograms recorded in patients with paroxysmal and persistent atrial fibrillation. Europace. 2010 Apr;12 (4):494–501. doi: 10.1093/europace/euq033. [DOI] [PubMed] [Google Scholar]
- Wu Shao-Hui, Jiang Wei-Feng, Gu Jun, Zhao Liang, Wang Yuan-Long, Liu Yu-Gang, Zhou Li, Gu Jia-Ning, Xu Kai, Liu Xu. Benefits and risks of additional ablation of complex fractionated atrial electrograms for patients with atrial fibrillation: a systematic review and meta-analysis. Int. J. Cardiol. 2013 Oct 25;169 (1):35–43. doi: 10.1016/j.ijcard.2013.08.083. [DOI] [PubMed] [Google Scholar]
- Hunter Ross J, Diab Ihab, Thomas Glyn, Duncan Edward, Abrams Dominic, Dhinoja Mehul, Sporton Simon, Earley Mark J, Schilling Richard J. Validation of a classification system to grade fractionation in atrial fibrillation and correlation with automated detection systems. Europace. 2009 Dec;11 (12):1587–96. doi: 10.1093/europace/eup351. [DOI] [PubMed] [Google Scholar]
- Verma Atul, Novak Paul, Macle Laurent, Whaley Bonnie, Beardsall Marianne, Wulffhart Zaev, Khaykin Yaariv. A prospective, multicenter evaluation of ablating complex fractionated electrograms (CFEs) during atrial fibrillation (AF) identified by an automated mapping algorithm: acute effects on AF and efficacy as an adjuvant strategy. Heart Rhythm. 2008 Feb;5 (2):198–205. doi: 10.1016/j.hrthm.2007.09.027. [DOI] [PubMed] [Google Scholar]
- Zellerhoff Stephan, Daly Matthew, Lim Han S, Denis Arnaud, Komatsu Yuki, Jesel Laurence, Derval Nicolas, Sacher Frédéric, Cochet Hubert, Knecht Sébastien, Yiem Sunthareth, Hocini Mélèze, Haïssaguerre Michel, Jaïs Pierre. Pulmonary vein isolation using a circular, open irrigated mapping and ablation catheter (nMARQ): a report on feasibility and efficacy. Europace. 2014 Sep;16 (9):1296–303. doi: 10.1093/europace/euu133. [DOI] [PubMed] [Google Scholar]
- Scaglione Marco, Caponi Domenico, Anselmino Matteo, Di Clemente Francesca, Blandino Alessandro, Ferraris Federico, Di Donna Paolo, Ebrille Elisa, Halimi Franck, Leclercq Jean F, Iunco Costanza, Vaudagna Carloeugenio, Cesarani Federico, Gaita Fiorenzo. Pulmonary vein isolation with a new multipolar irrigated radiofrequency ablation catheter (nMARQ™): feasibility, acute and short-term efficacy, safety, and impact on postablation silent cerebral ischemia. J. Cardiovasc. Electrophysiol. 2014 Dec;25 (12):1299–305. doi: 10.1111/jce.12500. [DOI] [PubMed] [Google Scholar]
- Gaita Fiorenzo, Leclercq Jean François, Schumacher Burghard, Scaglione Marco, Toso Elisabetta, Halimi Franck, Schade Anja, Froehner Steffen, Ziegler Volker, Sergi Domenico, Cesarani Federico, Blandino Alessandro. Incidence of silent cerebral thromboembolic lesions after atrial fibrillation ablation may change according to technology used: comparison of irrigated radiofrequency, multipolar nonirrigated catheter and cryoballoon. J. Cardiovasc. Electrophysiol. 2011 Sep;22 (9):961–8. doi: 10.1111/j.1540-8167.2011.02050.x. [DOI] [PubMed] [Google Scholar]
- Herrera Siklódy Claudia, Deneke Thomas, Hocini Mélèze, Lehrmann Heiko, Shin Dong-In, Miyazaki Shinsuke, Henschke Susanne, Fluegel Peter, Schiebeling-Römer Jochen, Bansmann Paul M, Bourdias Thomas, Dousset Vincent, Haïssaguerre Michel, Arentz Thomas. Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J. Am. Coll. Cardiol. 2011 Aug 9;58 (7):681–8. doi: 10.1016/j.jacc.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Sanders Prashanthan, Berenfeld Omer, Hocini Mélèze, Jaïs Pierre, Vaidyanathan Ravi, Hsu Li-Fern, Garrigue Stéphane, Takahashi Yoshihide, Rotter Martin, Sacher Fréderic, Scavée Christophe, Ploutz-Snyder Robert, Jalife José, Haïssaguerre Michel. Spectral analysis identifies sites of high-frequency activity maintaining atrial fibrillation in humans. Circulation. 2005 Aug 9;112 (6):789–97. doi: 10.1161/CIRCULATIONAHA.104.517011. [DOI] [PubMed] [Google Scholar]
- Atienza Felipe, Almendral Jesús, Jalife José, Zlochiver Sharon, Ploutz-Snyder Robert, Torrecilla Esteban G, Arenal Angel, Kalifa Jérôme, Fernández-Avilés Francisco, Berenfeld Omer. Real-time dominant frequency mapping and ablation of dominant frequency sites in atrial fibrillation with left-to-right frequency gradients predicts long-term maintenance of sinus rhythm. Heart Rhythm. 2009 Jan;6 (1):33–40. doi: 10.1016/j.hrthm.2008.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haïssaguerre Michel, Sanders Prashanthan, Hocini Mélèze, Hsu Li-Fern, Shah Dipen C, Scavée Christophe, Takahashi Yoshihide, Rotter Martin, Pasquié Jean-Luc, Garrigue Stéphane, Clémenty Jacques, Jaïs Pierre. Changes in atrial fibrillation cycle length and inducibility during catheter ablation and their relation to outcome. Circulation. 2004 Jun 22;109 (24):3007–13. doi: 10.1161/01.CIR.0000130645.95357.97. [DOI] [PubMed] [Google Scholar]
- Cochet Hubert, Dubois Rémi, Sacher Frédéric, Derval Nicolas, Sermesant Maxime, Hocini Mélèze, Montaudon Michel, Haïssaguerre Michel, Laurent François, Jaïs Pierre. Cardiac arrythmias: multimodal assessment integrating body surface ECG mapping into cardiac imaging. Radiology. 2014 Apr;271 (1):239–47. doi: 10.1148/radiol.13131331. [DOI] [PubMed] [Google Scholar]
- Haissaguerre Michel, Hocini Meleze, Denis Arnaud, Shah Ashok J, Komatsu Yuki, Yamashita Seigo, Daly Matthew, Amraoui Sana, Zellerhoff Stephan, Picat Marie-Quitterie, Quotb Adam, Jesel Laurence, Lim Han, Ploux Sylvain, Bordachar Pierre, Attuel Guillaume, Meillet Valentin, Ritter Philippe, Derval Nicolas, Sacher Frederic, Bernus Olivier, Cochet Hubert, Jais Pierre, Dubois Remi. Driver domains in persistent atrial fibrillation. Circulation. 2014 Aug 12;130 (7):530–8. doi: 10.1161/CIRCULATIONAHA.113.005421. [DOI] [PubMed] [Google Scholar]
- Narayan Sanjiv M, Krummen David E, Shivkumar Kalyanam, Clopton Paul, Rappel Wouter-Jan, Miller John M. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J. Am. Coll. Cardiol. 2012 Aug 14;60 (7):628–36. doi: 10.1016/j.jacc.2012.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan Sanjiv M, Baykaner Tina, Clopton Paul, Schricker Amir, Lalani Gautam G, Krummen David E, Shivkumar Kalyanam, Miller John M. Ablation of rotor and focal sources reduces late recurrence of atrial fibrillation compared with trigger ablation alone: extended follow-up of the CONFIRM trial (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation). J. Am. Coll. Cardiol. 2014 May 6;63 (17):1761–8. doi: 10.1016/j.jacc.2014.02.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan Sanjiv M, Krummen David E, Clopton Paul, Shivkumar Kalyanam, Miller John M. Direct or coincidental elimination of stable rotors or focal sources may explain successful atrial fibrillation ablation: on-treatment analysis of the CONFIRM trial (Conventional ablation for AF with or without focal impulse and rotor modulation). J. Am. Coll. Cardiol. 2013 Jul 9;62 (2):138–47. doi: 10.1016/j.jacc.2013.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahnkopf Christian, Badger Troy J, Burgon Nathan S, Daccarett Marcos, Haslam Thomas S, Badger Christopher T, McGann Christopher J, Akoum Nazem, Kholmovski Eugene, Macleod Rob S, Marrouche Nassir F. Evaluation of the left atrial substrate in patients with lone atrial fibrillation using delayed-enhanced MRI: implications for disease progression and response to catheter ablation. Heart Rhythm. 2010 Oct;7 (10):1475–81. doi: 10.1016/j.hrthm.2010.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrouche Nassir F, Wilber David, Hindricks Gerhard, Jais Pierre, Akoum Nazem, Marchlinski Francis, Kholmovski Eugene, Burgon Nathan, Hu Nan, Mont Lluis, Deneke Thomas, Duytschaever Mattias, Neumann Thomas, Mansour Moussa, Mahnkopf Christian, Herweg Bengt, Daoud Emile, Wissner Erik, Bansmann Paul, Brachmann Johannes. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014 Feb 5;311 (5):498–506. doi: 10.1001/jama.2014.3. [DOI] [PubMed] [Google Scholar]
- Oakes Robert S, Badger Troy J, Kholmovski Eugene G, Akoum Nazem, Burgon Nathan S, Fish Eric N, Blauer Joshua J E, Rao Swati N, DiBella Edward V R, Segerson Nathan M, Daccarett Marcos, Windfelder Jessiciah, McGann Christopher J, Parker Dennis, MacLeod Rob S, Marrouche Nassir F. Detection and quantification of left atrial structural remodeling with delayed-enhancement magnetic resonance imaging in patients with atrial fibrillation. Circulation. 2009 Apr 7;119 (13):1758–67. doi: 10.1161/CIRCULATIONAHA.108.811877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma Atul, Wazni Oussama M, Marrouche Nassir F, Martin David O, Kilicaslan Fethi, Minor Stephen, Schweikert Robert A, Saliba Walid, Cummings Jennifer, Burkhardt J David, Bhargava Mandeep, Belden William A, Abdul-Karim Ahmad, Natale Andrea. Pre-existent left atrial scarring in patients undergoing pulmonary vein antrum isolation: an independent predictor of procedural failure. J. Am. Coll. Cardiol. 2005 Jan 18;45 (2):285–92. doi: 10.1016/j.jacc.2004.10.035. [DOI] [PubMed] [Google Scholar]
- Yamaguchi Takanori, Tsuchiya Takeshi, Nagamoto Yasutsugu, Miyamoto Koji, Murotani Kenta, Okishige Kaoru, Takahashi Naohiko. Long-term results of pulmonary vein antrum isolation in patients with atrial fibrillation: an analysis in regards to substrates and pulmonary vein reconnections. Europace. 2014 Apr;16 (4):511–20. doi: 10.1093/europace/eut265. [DOI] [PubMed] [Google Scholar]
- Rolf Sascha, Kircher Simon, Arya Arash, Eitel Charlotte, Sommer Philipp, Richter Sergio, Gaspar Thomas, Bollmann Andreas, Altmann David, Piedra Carlos, Hindricks Gerhard, Piorkowski Christopher. Tailored atrial substrate modification based on low-voltage areas in catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014 Oct;7 (5):825–33. doi: 10.1161/CIRCEP.113.001251. [DOI] [PubMed] [Google Scholar]
- McGann Christopher J, Kholmovski Eugene G, Oakes Robert S, Blauer Joshua J E, Daccarett Marcos, Segerson Nathan, Airey Kelly J, Akoum Nazem, Fish Eric, Badger Troy J, DiBella Edward V R, Parker Dennis, MacLeod Rob S, Marrouche Nassir F. New magnetic resonance imaging-based method for defining the extent of left atrial wall injury after the ablation of atrial fibrillation. J. Am. Coll. Cardiol. 2008 Oct 7;52 (15):1263–71. doi: 10.1016/j.jacc.2008.05.062. [DOI] [PubMed] [Google Scholar]
- Taclas Jason E, Nezafat Reza, Wylie John V, Josephson Mark E, Hsing Jeff, Manning Warren J, Peters Dana C. Relationship between intended sites of RF ablation and post-procedural scar in AF patients, using late gadolinium enhancement cardiovascular magnetic resonance. Heart Rhythm. 2010 Apr;7 (4):489–96. doi: 10.1016/j.hrthm.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisbal Felipe, Guiu Esther, Cabanas-Grandío Pilar, Berruezo Antonio, Prat-Gonzalez Susana, Vidal Bárbara, Garrido Cesar, Andreu David, Fernandez-Armenta Juan, Tolosana Jose María, Arbelo Elena, de Caralt Teresa M, Perea Rosario J, Brugada Josep, Mont Lluís. CMR-guided approach to localize and ablate gaps in repeat AF ablation procedure. JACC Cardiovasc Imaging. 2014 Jul;7 (7):653–63. doi: 10.1016/j.jcmg.2014.01.014. [DOI] [PubMed] [Google Scholar]
- Linton Nick W F, Koa-Wing Michael, Francis Darrel P, Kojodjojo Pipin, Lim Phang Boon, Salukhe Tushar V, Whinnett Zachary, Davies D Wyn, Peters Nicholas S, O'Neill Mark D, Kanagaratnam Prapa. Cardiac ripple mapping: a novel three-dimensional visualization method for use with electroanatomic mapping of cardiac arrhythmias. Heart Rhythm. 2009 Dec;6 (12):1754–62. doi: 10.1016/j.hrthm.2009.08.038. [DOI] [PubMed] [Google Scholar]
- Jamil-Copley Shahnaz, Linton Nick, Koa-Wing Michael, Kojodjojo Pipin, Lim Phang Boon, Malcolme-Lawes Louisa, Whinnett Zachary, Wright Ian, Davies Wyn, Peters Nicholas, Francis Darrel P, Kanagaratnam Prapa. Application of ripple mapping with an electroanatomic mapping system for diagnosis of atrial tachycardias. J. Cardiovasc. Electrophysiol. 2013 Dec;24 (12):1361–9. doi: 10.1111/jce.12259. [DOI] [PubMed] [Google Scholar]
- Rolf Sascha, John Silke, Gaspar Thomas, Dinov Boris, Kircher Simon, Huo Yan, Bollmann Andreas, Richter Sergio, Arya Arash, Hindricks Gerhard, Piorkowski Christopher, Sommer Philipp. Catheter ablation of atrial fibrillation supported by novel nonfluoroscopic 4D navigation technology. Heart Rhythm. 2013 Sep;10 (9):1293–300. doi: 10.1016/j.hrthm.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Rolf Sascha, Sommer Philipp, Gaspar Thomas, John Silke, Arya Arash, Hindricks Gerhard, Piorkowski Christopher. Ablation of atrial fibrillation using novel 4-dimensional catheter tracking within autoregistered left atrial angiograms. Circ Arrhythm Electrophysiol. 2012 Aug 1;5 (4):684–90. doi: 10.1161/CIRCEP.112.971705. [DOI] [PubMed] [Google Scholar]
- Sommer Philipp, Rolf Sascha, Piorkowski Christopher, Gaspar Thomas, Huo Yan, Piedra Carlos, Richter Sergio, Bollmann Andreas, Arya Arash, Hindricks Gerhard. Nonfluoroscopic catheter visualization in atrial fibrillation ablation: experience from 375 consecutive procedures. Circ Arrhythm Electrophysiol. 2014 Oct;7 (5):869–74. doi: 10.1161/CIRCEP.114.001542. [DOI] [PubMed] [Google Scholar]
- Nakagawa Hiroshi, Ikeda Atsushi, Sharma Tushar, Lazzara Ralph, Jackman Warren M. Rapid high resolution electroanatomical mapping: evaluation of a new system in a canine atrial linear lesion model. Circ Arrhythm Electrophysiol. 2012 Apr;5 (2):417–24. doi: 10.1161/CIRCEP.111.968602. [DOI] [PubMed] [Google Scholar]
- Bollmann Andreas, Hilbert Sebastian, John Silke, Kosiuk Jedrzej, Hindricks Gerhard. Insights from preclinical ultra high-density electroanatomical sinus node mapping. Europace. 2015 Mar;17 (3):489–94. doi: 10.1093/europace/euu276. [DOI] [PubMed] [Google Scholar]
- Piorkowski Christopher, Grothoff Matthias, Gaspar Thomas, Eitel Charlotte, Sommer Philipp, Huo Yan, John Silke, Gutberlet Matthias, Hindricks Gerhard. Cavotricuspid isthmus ablation guided by real-time magnetic resonance imaging. Circ Arrhythm Electrophysiol. 2013 Feb;6 (1):e7–10. doi: 10.1161/CIRCEP.112.973719. [DOI] [PubMed] [Google Scholar]