Abstract
Hypertrophic cardiomyopathy (HCM) is a genetic cardiovascular disease that predisposes individuals to the development of arrhythmias. The most common sustained arrhythmia is atrial fibrillation (AF). Compared with the general population, patients with HCM are more prone to the development of AF. To avoid embolic complications and the clinical deterioration caused by the development of AF in HCM, identifying patients with a tendency toward AF might affect the management of HCM. In this review, we evaluated the predictors of AF development in patients with HCM.
Keywords: Hypertrophic Cardiomyopathy, Atrial Fibrillation, Left Atrium, Predictors
Introduction
Hypertrophic cardiomyopathy (HCM) is the most common genetic cardiovascular disorder, with a prevalence of 1:500 in population-based studies.[1] Diagnosis is based on the demonstration of a hypertrophied left ventricle (LV) with a wall thickness of ≥15 mm that cannot be explained solely by the loading conditions. In most cases, a mutation in the gene that encodes a sarcomeric protein causes the disease, and it is inherited mostly as an autosomal dominant genetic trait.[2] The disease spectrum is wide, including an asymptomatic state, the development of symptoms of heart failure due to impaired diastolic functions or LV outflow (LVOT) obstruction, sudden cardiac death, progression to LV systolic dysfunction, atrial fibrillation (AF), and related embolic complications.[2]
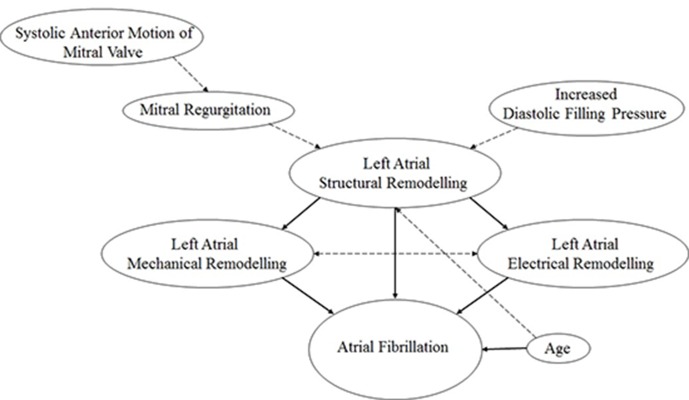
AF is the most common sustained arrhythmia in patients with HCM.[3] It occurs in ~1% of the general population,[4] but 20–30% of patients with HCM.[4-6] Approximately 2–3.8% of HCM patients are diagnosed with AF annually.[7-9] Since LV filling is dependent mostly on atrial contraction in HCM patients, AF is poorly tolerated by these patients since it reduces LV filling time and causes further impairment in LV diastole. Development of AF causes acute symptoms such as palpitations, dyspnea, and chest pain. The clinical worsening might be more prominent in those with LVOT obstruction and those with severe diastolic dysfunction. In these patients development of AF might cause hypotension, lightheadedness, presyncope, and syncope. By decreasing LV diastolic filling time during the tachycardia, AF may also provoke or worsen an LVOT gradient. A study investigating impact of AF on stroke displayed an obviously increased risk in the patients with AF compared with those in sinus rhythm.[5] AF is associated not only with an increased risk of stroke but also with an increased risk of advanced heart failure,[6,7] and stroke-related deaths6 in HCM population. AF was also proved to cause premature deaths in an Italian HCM cohort.[10] Therefore, understanding the predictors of AF and the management of these determinants before AF develops is important clinically. In this review, we evaluated the predictors of AF development in patients with HCM (Table 1 and Figure 1).
Table 1. Predictors of atrial fibrillation risk in hypertrophic cardiomyopathy.
LA = Left atrium; LAEF = Left atrial ejection fraction
| Study | Variables | Cutoff values |
|---|---|---|
| Maron et al.18 | Age | ≥ 40 years |
| Olivotto et al.5 | LA diameter | > 45 mm |
| Maron et al.18 | LA end-diastolic volume | ≥ 118 mL |
| Tani et al.15 | LA volume index | ≥ 34 mL/cm2 |
| Maron et al.18 | LAEF | < 38 % |
| Ozdemir et al.22 | Maximun P-wave duration | > 134.5 ms |
| Cecchi et al.21 | Filtered P wave duration | ≥ 140 ms |
| Ozdemir et al.22 | P wave dispersion | > 52.5 ms |
Figure 1. Contributors and predictors of atrial fibrillation risk in hypertrophic cardiomyopathy.
Left Atrial Structural Remodeling
Left atrial (LA) enlargement is common in HCM. The LA is a thin-walled cardiac chamber that is exposed to LV end-diastolic pressure (LVEDP). In HCM, elevated LVEDP causes an increase in LA afterload; in response LA enlarges and secondary atrial myopathy is observed.[11] Atrial tissue fibrosis was observed in pathological specimens from HCM patients, which might have been a consequence of secondary atrial myopathy.[12] Fibrosis could impair the propagation of sinus impulses in atrial tissue and thereby play an important role in the development of AF.
The size of the LA is strongly associated with the development of AF in patients with HCM.[3] Although different thresholds for using the size of the LA to predict AF in HCM populations have been used in different trials, the most accepted LA size is ≥45 mm.[5,13] Guidelines from the European Society of Cardiology advised that 48-h ambulatory electrocardiogram (ECG) monitoring should be performed every 6–12 months to detect AF in patients who are in sinus rhythm (SR) and have an LA diameter ≥45 mm.[13] Regardless of whether AF attacks are paroxysmal or persistant and whether they cause symptoms or are asymptomatic, patients with documented AF should be administered anticoagulant therapy.[14] Although measuring LA diameter when assessing the susceptibility of patients for AF development is practical and used commonly in routine echocardiographic evaluations, calculating the LA volume index (LAVI) provides more information regarding LA remodeling than does measuring its diameter alone.[15,16] LAVI is also superior to measuring LA diameter for predicting AF in patients with HCM; specifically, a LAVI cutoff value of ≥34 mL/m2 was associated with the development of paroxysmal AF attacks.[15] Changes in the LA volume and related functions proceed according to the Frank-Starling mechanism in patients with HCM, which explains failure of LA function in response to larger LAVs in patients with HCM.[11,17] We demonstrated recently that LA functions were preserved until the LAVI reached 40 mL/m2, but that further increases in LAVI resulted in deteriorated LA functions.[11] These observations might lead to the more compherensive follow-up of patients with a LAVI of ≥ 40 mL/m2. Recently, Maron et al. suggested that an LA cutoff volume of ≥118 mL predicted the occurrence of AF with 71% sensitivity and 65% specificity in populations with HCM.[18] Therefore, LA functions and volumes should be evaluated compherensively to identify individuals at risk before the onset of AF. The prophylactic use of anticoagulants for stroke prevention in patients with LA dysfunction has not yet been investigated or recommended.
LA Mechanical Remodelling
Three phases of LA mechanical function occur during a cardiac cycle.[19] First, during ventricular systole the LA collects and stores blood to function as a “reservoir”, which is also named the LA total emptying fraction. Second, during the early phase of ventricular diastole the LA transfers blood passively into the LV to serve as a “conduit”, which is also named the LA passive emptying fraction. Third, the LA functions has a “contractile” function to push blood actively into the LV, which is also named the LA active emptying fraction or booster pump function.[19] The phasic functions of the LA have been used to predict the development of AF episodes in patients with HCM.[18] For example, Maron et al. used the LA total emptying fraction (expressed as LAEF <38%) to predict future clinical AF events. However, the authors did not evaluate the value of other two LA phasic functions for predicting the development of AF. Therefore, further data are needed.
LA Electrical Remodelling
Sinus impulses spread homogenously in the atrial myocardium. The distribution of discontinuous and heterogeneous sinus impulse propagations, an increased dispersion of atrial refractories, and fragmentation of intra-atrial conduction could cause atrial reentry. Two electrocardiographic parameters might provide data regarding the distribution properties of impulses: P wave duration (Pdur), and P-wave dispersion (PWD).[20] The value of Pdur for predicting the development of AF in a HCM cohort was assessed by Cecchi et al.[21] They demonstrated that measuring a Pdur of ≥140 msn in the sinus rhythm using high resolution signal-averaged electrocardiography identified patients with HCM who were likely to develop AF with sensitivity, specificity, and positive-predictive accuracy values of 56%, 83%, and 66%, respectively.[21] Measuring Pdur is a non-invasive technique, but it is not practical for use in routine clinical evaluations. Instead, measuring the maximum P wave duration (Pmax) and PWD using surface 12-lead ECGs is more practical. Ozdemir et al. assessed the value of these two parameters in patients with HCM. They reported that a Pmax of >134.5 ms separated HCM patients with and without AF with a sensitivity of 92%, specificity of 89%, and a positive predictive value of 80%.[22] A PWD of >52.5 ms separated HCM patients with AF from those without AF with a sensitivity of 96%, a specificity of 91%, and a positive predictive accuracy of 84%.[22] In addition, assessing both electrocardiographic parameters as well as atrial electromechanical dyssynchrony using echocardiography[23] helps to identify prolonged atrial conduction noninvasively. A chronically elevated LV filling pressure in patients with HCM might cause secondary atrial myopathy,[11] which contributes to atrial dyssynchrony and a prolonged PWD;[24] however, a study assessing the predictive value of atrial dyssynchrony for the development of AF in a population with HCM has not yet been reported.
Previously, the association between LA electrical and mechanical remodelling in HCM patients with sinus rhythm was investigated. Negative correlations between LA total emptying fraction (LA reservoir function) and PWD and atrial dyssynchrony were shown in these patients.[24] No association between LA active emptying fraction and LA electrical remodelling was detected. The LA total emptying fraction was related to AF development,[18] however; the value of LA active emptying fraction in predicting AF development in HCM population was not assessed in a follow up study.
Genetic Factors
The tendency of some families with HCM to development of AF and incidence of AF in patients with small LA (LA diameter ≤40 mm) have raised suspicions about the genetic inheritance of AF in patients with HCM.[3] This hypothesis is supported indirectly by observations that a specific myosin heavy-chain mutation (Arg663His) increased the risk of developing AF.[25] A study of 24 patients with Arg663His mutations revealed that there was a high prevalence of AF. Specifically, 47% of these individuals developed AF over a 7-year follow-up period.[25] In addition to sarcomeric gene mutations, a group of non-sarcomeric genes have been investigated to assess the genetic predisposition of individuals with HCM to develop AF. The possible role of aldosterone in atrial structural and electrical remodelling, increasing collagen biosynthesis, and cardiomyocyte apoptosis attracted attention toward genes in the renin angiotensin aldosterone system (RAAS).[26] Belenkov et al. investigated different polymorphisms in various RAAS genes in patients HCM, and showed that 1166/ polymorphisms of AGTR1 was a predictor of AF development, whereas −344 / polymorphisms of CYP11B2 had no association with AF development.[27] However, a recent study that analyzed a Caucasian population with HCM showed a role of the –344T>C CYP11B2 gene polymorphism in the secretion of serum aldosterone, and suggested a link between this polymorphism and AF development in HCM patients.[9] Therefore, further data are needed to better understanding the role of the RAAS genes in predicting AF in HCM.
Age
Age is a well-known predictor of AF in the general population.[28] Increased age also contributes to the development of AF in HCM;[18] however, there is also evidence that a large number of HCM patients aged <60 years also developed AF.[29] For example, one study reported that AF developed in a wide age range of patients (19–82 years) with HCM.[3] Our previous report explaining that the presence of LA appendage dysfunction in sinus rhythm was independent of age in a HCM cohort also raised concerns over the need for additional AF predictors that could be used in relatively young HCM population.[30] Olivotto et al. reported that an age at diagnosis of >50 years was a predictor of AF in a multivariate analysis that included LA diameter, functional class, maximum LA wall thickness, and the presence of ≥30 mmHg gradient in LVOT; however, LV filling pressure was not studied.[5] Recently, Maron et al. reported an age threshold of ≥40 years for predicting AF in their HCM cohort.[17] A late diagnosis of HCM might be associated with a long duration of exposure to a high LV filling pressure. Taken together, these findings suggest that increased age contributes to the development of AF in HCM patients. Nevertheless, more studies are needed to identify young patients at risk of developing AF for the early management of these patients.
Left Ventricular Outflow Obstruction
Confounding data have been reported in studies that assessed the effect of LVOT obstruction or the magnitude of the gradient in LVOT on AF development. The largest retrospective singlecenter study designed to characterize the prevalence, clinical, and echocardiographic correlates of AF included 3023 patients with HCM who remained in SR and 650 HCM patients with AF, and revealed that AF was less common in patients with an obstructive HCM phenotype.[31] In contrast, Autore et al. suggested that a higher proportion of patients with LVOT obstruction developed either paroxysmal or chronic AF compared with those without LVOT obstruction during follow-up.[32] The discrepancy in these studies might be caused by the dynamic state of the LVOT gradient, rather than the constant state observed in aortic stenosis. It is not possible to estimate the duration and magnitude of the LVOT gradient that an HCM patient is exposed throughout their life because of the dynamic nature of the LVOT obstruction. As such, it is controversial whether LVOT obstruction contributes to LA remodelling.[33-35] A more severe LVOT gradient causes more a severe systolic anterior motion of mitral valve, which results in a more severe mitral regurgitation36[36] that might cause LA function to deteriorate. It could be concluded that the contribution of LVOT obstruction to LA remodelling might be caused by the resultant mitral regurgitation as a result of the systolic anterior motion of the mitral leaflets. Therefore, predicting the development of AF using the duration and degree of mitral regurgitation might be valuable.
Myocardial Fibrosis
Myocardial fibrosis is a known predictor of ventricular arrythmias in patients with HCM.[37] However, a study investigating pathological specimens of HCM patients with and without AF reported that a greater proportion of myocardial fibrosis in the LV was observed in individuals with AF compared with those without AF, suggesting that the severity of myocardial fibrosis is related to the development of AF in HCM.[38] It is possible that myocardial fibrosis contributes to the development of AF by increasing LV stiffness and elevating LV end-diastolic pressure. However, limited data are available, and larger studies are needed.
Higher levels of brain natriuretic peptide (BNP) are detected in HCM patients with AF compared with those in SR.[31] The predictive value of BNP for the development of AF has not been investigated in a large study. The levels of the N-terminal portion of pro-BNP (NT-pro-BNP) were related to the failure of LA reservoir function.11 In addition, an impaired LA reservoir function was related to the development of AF in HCM patients.[17] This suggests that BNP might predict AF development in HCM. However, in a study evaluating the relationship between the prevelance of AF and the levels of high-sensitive cardiac troponin T (hs-cTnT) and BNP in obstructive HCM, hs-cTnT, but not BNP, levels were related to the prevalence of AF.[39] Moreover, hs-cTnT levels were significantly higher in patients with persistent AF compared with in those with paroxysmal AF or in those without AF. The leakage of troponin from dying atrial myocytes and during AF-induced myocardial ischemia were suggested as the sources of troponin release in HCM.[39] Therefore, larger studies are needed to assess the potential of routine biomarker measurements in clinical practice to identify HCM patients that are likely to developAF.
Conclusions
It is important to recognize HCM patients who are more prone to the development of AF early to avoid the devastating consequences of AF. LA remodeling remains the cornerstone for predicting AF. ECG also identifies patients with prolonged atrial conduction. In addition, increased age contributes to AF development. Assessing all these predictors on an individual basis and the close follow-up of patients with multiple risk factors before the embolic complications of AF occur might be useful. A risk scoring system for both sudden cardiac death and the development of AF that involves the above predictors might be helpful for the primary prevention of AF in HCM patients.
Disclosure
None.
References
- Maron B J, Gardin J M, Flack J M, Gidding S S, Kurosaki T T, Bild D E. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995 Aug 15;92 (4):785–9. doi: 10.1161/01.cir.92.4.785. [DOI] [PubMed] [Google Scholar]
- Richard Pascale, Charron Philippe, Carrier Lucie, Ledeuil Céline, Cheav Theary, Pichereau Claire, Benaiche Abdelaziz, Isnard Richard, Dubourg Olivier, Burban Marc, Gueffet Jean-Pierre, Millaire Alain, Desnos Michel, Schwartz Ketty, Hainque Bernard, Komajda Michel. Hypertrophic cardiomyopathy: distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Circulation. 2003 May 6;107 (17):2227–32. doi: 10.1161/01.CIR.0000066323.15244.54. [DOI] [PubMed] [Google Scholar]
- Maron Barry J, Olivotto Iacopo, Bellone Pietro, Conte Maria Rosa, Cecchi Franco, Flygenring Björn P, Casey Susan A, Gohman Thomas E, Bongioanni Sergio, Spirito Paolo. Clinical profile of stroke in 900 patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2002 Jan 16;39 (2):301–7. doi: 10.1016/s0735-1097(01)01727-2. [DOI] [PubMed] [Google Scholar]
- Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 9;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- Olivotto I, Cecchi F, Casey S A, Dolara A, Traverse J H, Maron B J. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001 Nov 20;104 (21):2517–24. doi: 10.1161/hc4601.097997. [DOI] [PubMed] [Google Scholar]
- Nistri Stefano, Olivotto Iacopo, Betocchi Sandro, Losi Maria Angela, Valsecchi Grazia, Pinamonti Bruno, Conte Maria Rosa, Casazza Franco, Galderisi Maurizio, Maron Barry J, Cecchi Franco. Prognostic significance of left atrial size in patients with hypertrophic cardiomyopathy (from the Italian Registry for Hypertrophic Cardiomyopathy). Am. J. Cardiol. 2006 Oct 1;98 (7):960–5. doi: 10.1016/j.amjcard.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Maron Barry J, McKenna William J, Danielson Gordon K, Kappenberger Lukas J, Kuhn Horst J, Seidman Christine E, Shah Pravin M, Spencer William H, Spirito Paolo, Ten Cate Folkert J, Wigle E Douglas. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J. Am. Coll. Cardiol. 2003 Nov 5;42 (9):1687–713. doi: 10.1016/s0735-1097(03)00941-0. [DOI] [PubMed] [Google Scholar]
- Guttmann Oliver P, Rahman M Shafiqur, O'Mahony Constantinos, Anastasakis Aris, Elliott Perry M. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart. 2014 Mar;100 (6):465–72. doi: 10.1136/heartjnl-2013-304276. [DOI] [PubMed] [Google Scholar]
- Orenes-Piñero E, Hernández-Romero D, Romero-Aniorte A I, Martínez M, García-Honrubia A, Caballero L, Garrigos-Gómez N, Andreu-Cayuelas J M, González J, Feliu E, Climent V, Nicolás-Ruiz F, De La Morena G, Valdés M, Lip G Y H, Marín F. Prognostic value of two polymorphisms in non-sarcomeric genes for the development of atrial fibrillation in patients with hypertrophic cardiomyopathy. QJM. 2014 Aug;107 (8):613–21. doi: 10.1093/qjmed/hcu046. [DOI] [PubMed] [Google Scholar]
- Cecchi F, Olivotto I, Montereggi A, Santoro G, Dolara A, Maron B J. Hypertrophic cardiomyopathy in Tuscany: clinical course and outcome in an unselected regional population. J. Am. Coll. Cardiol. 1995 Nov 15;26 (6):1529–36. doi: 10.1016/0735-1097(95)00353-3. [DOI] [PubMed] [Google Scholar]
- Tülüce Kamil, Yakar Tülüce Selcen, Yavuzgil Oğuz, İsayev Elnur, Bilgin Murat, Akyıldız Akçay Filiz, Nalbantgil Sanem, Özerkan Filiz. The left atrial phasic functions and the relationship with plasma N-terminal pro-B-type natriuretic peptide levels and symptomatic states in patients with hypertrophic cardiomyopathy. Anadolu Kardiyol Derg. 2014 Dec;14 (8):719–27. doi: 10.5152/akd.2014.5101. [DOI] [PubMed] [Google Scholar]
- Varnava A M, Elliott P M, Sharma S, McKenna W J, Davies M J. Hypertrophic cardiomyopathy: the interrelation of disarray, fibrosis, and small vessel disease. Heart. 2000 Nov;84 (5):476–82. doi: 10.1136/heart.84.5.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott Perry M, Anastasakis Aris, Borger Michael A, Borggrefe Martin, Cecchi Franco, Charron Philippe, Hagege Albert Alain, Lafont Antoine, Limongelli Giuseppe, Mahrholdt Heiko, McKenna William J, Mogensen Jens, Nihoyannopoulos Petros, Nistri Stefano, Pieper Petronella G, Pieske Burkert, Rapezzi Claudio, Rutten Frans H, Tillmanns Christoph, Watkins Hugh. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014 Oct 14;35 (39):2733–79. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014 Dec 2;64 (21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Tani Tomoko, Tanabe Kazuaki, Ono Miwa, Yamaguchi Kazuto, Okada Midori, Sumida Toshiaki, Konda Toshiko, Fujii Yoko, Kawai Junichi, Yagi Toshikazu, Sato Masatake, Ibuki Motoaki, Katayama Minako, Tamita Koichi, Yamabe Kenji, Yamamuro Atsushi, Nagai Kunihiko, Shiratori Kenichi, Morioka Shigefumi. Left atrial volume and the risk of paroxysmal atrial fibrillation in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2004 Jun;17 (6):644–8. doi: 10.1016/j.echo.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Tsang Teresa S M, Abhayaratna Walter P, Barnes Marion E, Miyasaka Yoko, Gersh Bernard J, Bailey Kent R, Cha Stephen S, Seward James B. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J. Am. Coll. Cardiol. 2006 Mar 7;47 (5):1018–23. doi: 10.1016/j.jacc.2005.08.077. [DOI] [PubMed] [Google Scholar]
- Bauer Fabrice, Shiota Takahiro, White Richard D, Lever Harry M, Qin Jian Xin, Drinko Jeannie, Martin Maureen, Tsujino Hiroyuki, Sitges Marta, Kim Yong Jin, Thomas James D. Determinant of left atrial dilation in patients with hypertrophic cardiomyopathy: a real-time 3-dimensional echocardiographic study. J Am Soc Echocardiogr. 2004 Sep;17 (9):968–75. doi: 10.1016/j.echo.2004.05.018. [DOI] [PubMed] [Google Scholar]
- Maron Barry J, Haas Tammy S, Maron Martin S, Lesser John R, Browning Joseph A, Chan Raymond H, Olivotto Iacopo, Garberich Ross F, Schwartz Robert S. Left atrial remodeling in hypertrophic cardiomyopathy and susceptibility markers for atrial fibrillation identified by cardiovascular magnetic resonance. Am. J. Cardiol. 2014 Apr 15;113 (8):1394–400. doi: 10.1016/j.amjcard.2013.12.045. [DOI] [PubMed] [Google Scholar]
- Blume Gustavo G, Mcleod Christopher J, Barnes Marion E, Seward James B, Pellikka Patricia A, Bastiansen Paul M, Tsang Teresa S M. Left atrial function: physiology, assessment, and clinical implications. Eur J Echocardiogr. 2011 Jun;12 (6):421–30. doi: 10.1093/ejechocard/jeq175. [DOI] [PubMed] [Google Scholar]
- Dilaveris P E, Gialafos E J, Sideris S K, Theopistou A M, Andrikopoulos G K, Kyriakidis M, Gialafos J E, Toutouzas P K. Simple electrocardiographic markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am. Heart J. 1998 May;135 (5 Pt 1):733–8. doi: 10.1016/s0002-8703(98)70030-4. [DOI] [PubMed] [Google Scholar]
- Cecchi F, Montereggi A, Olivotto I, Marconi P, Dolara A, Maron B J. Risk for atrial fibrillation in patients with hypertrophic cardiomyopathy assessed by signal averaged P wave duration. Heart. 1997 Jul;78 (1):44–9. doi: 10.1136/hrt.78.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozdemir Ozcan, Soylu Mustasa, Demir Ahmet Duran, Topaloglu Serkan, Alyan Omer, Turhan Hasan, Bicer Asuman, Kutuk Emine. P-wave durations as a predictor for atrial fibrillation development in patients with hypertrophic cardiomyopathy. Int. J. Cardiol. 2004 Apr;94 (2-3):163–6. doi: 10.1016/j.ijcard.2003.01.001. [DOI] [PubMed] [Google Scholar]
- Sakabe K, Fukuda N, Fukuda Y, Morishita S, Shinohara H, Tamura Y. Interatrial dyssynchrony on tissue Doppler imaging predicts progression to chronic atrial fibrillation in patients with non-valvular paroxysmal atrial fibrillation. Heart. 2009 Jun;95 (12):988–93. doi: 10.1136/hrt.2008.152561. [DOI] [PubMed] [Google Scholar]
- Tuluce Kamil, Ozerkan Filiz, Yakar Tuluce Selcen, Yavuzgil Oguz, Gurgun Cemil, Bilgin Murat, Kahya Eren Nihan, Kocabas Ugur, Nalbantgil Sanem, Soydas Cinar Cahide. Relationships between P wave dispersion, atrial electromechanical delay, left atrial remodeling, and NT-proBNP levels, in patients with hypertrophic cardiomyopathy. Cardiol J. 2015;22 (1):94–100. doi: 10.5603/CJ.a2014.0025. [DOI] [PubMed] [Google Scholar]
- Gruver E J, Fatkin D, Dodds G A, Kisslo J, Maron B J, Seidman J G, Seidman C E. Familial hypertrophic cardiomyopathy and atrial fibrillation caused by Arg663His beta-cardiac myosin heavy chain mutation. Am. J. Cardiol. 1999 Jun 17;83 (12A):13H–18H. doi: 10.1016/s0002-9149(99)00251-9. [DOI] [PubMed] [Google Scholar]
- Tsai Chia-Ti, Chiang Fu-Tien, Tseng Chuen-Den, Hwang Juey-Jen, Kuo Kuan-Ting, Wu Cho-Kai, Yu Chih-Chieh, Wang Yi-Chih, Lai Ling-Ping, Lin Jiunn-Lee. Increased expression of mineralocorticoid receptor in human atrial fibrillation and a cellular model of atrial fibrillation. J. Am. Coll. Cardiol. 2010 Feb 23;55 (8):758–70. doi: 10.1016/j.jacc.2009.09.045. [DOI] [PubMed] [Google Scholar]
- Belenkov Yu N, Privalova E V, Kaplunova V Yu, Stambol'skiĭ D V, Fomin A A. [Analysis of morpho-functional parameters of the heart and polymorphisms of Renin-Angiotensin-aldosterone system genes in patients with different variants of the course of hypertrophic cardiomyopathy]. Kardiologiia. 2010;50 (6):27–34. [PubMed] [Google Scholar]
- Benjamin E J, Levy D, Vaziri S M, D'Agostino R B, Belanger A J, Wolf P A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994 Mar 16;271 (11):840–4. [PubMed] [Google Scholar]
- Losi Maria-Angela, Betocchi Sandro, Aversa Mariano, Lombardi Raffaella, Miranda Marianna, D'Alessandro Gianluigi, Cacace Alessandra, Tocchetti Carlo-Gabriele, Barbati Giovanni, Chiariello Massimo. Determinants of atrial fibrillation development in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 2004 Oct 1;94 (7):895–900. doi: 10.1016/j.amjcard.2004.06.024. [DOI] [PubMed] [Google Scholar]
- Yakar Tuluce Selcen, Kayikcioglu Meral, Tuluce Kamil, Yilmaz Meral Gulsum, Ozdogan Oner, Aydın Mehmet, Hasdemir Can. Assessment of left atrial appendage function during sinus rhythm in patients with hypertrophic cardiomyopathy: transesophageal echocardiography and tissue doppler study. J Am Soc Echocardiogr. 2010 Nov;23 (11):1207–16. doi: 10.1016/j.echo.2010.08.016. [DOI] [PubMed] [Google Scholar]
- Siontis Konstantinos C, Geske Jeffrey B, Ong Kevin, Nishimura Rick A, Ommen Steve R, Gersh Bernard J. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high-risk population. J Am Heart Assoc. 2014 Jun;3 (3):e001002. doi: 10.1161/JAHA.114.001002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autore Camillo, Bernabò Paola, Barillà Caterina Stella, Bruzzi Paolo, Spirito Paolo. The prognostic importance of left ventricular outflow obstruction in hypertrophic cardiomyopathy varies in relation to the severity of symptoms. J. Am. Coll. Cardiol. 2005 Apr 5;45 (7):1076–80. doi: 10.1016/j.jacc.2004.12.067. [DOI] [PubMed] [Google Scholar]
- Anwar Ashraf M, Soliman Osama I I, Nemes Attila, Geleijnse Marcel L, ten Cate Folkert J. An integrated approach to determine left atrial volume, mass and function in hypertrophic cardiomyopathy by two-dimensional echocardiography. Int J Cardiovasc Imaging. 2008 Jan;24 (1):45–52. doi: 10.1007/s10554-007-9224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Hua, Woo Anna, Monakier Daniel, Jamorski Michal, Fedwick Katie, Wigle E Douglas, Rakowski Harry. Enlarged left atrial volume in hypertrophic cardiomyopathy: a marker for disease severity. J Am Soc Echocardiogr. 2005 Oct;18 (10):1074–82. doi: 10.1016/j.echo.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Paulus W J. Natriuretic peptides to probe haemodynamic overload in hypertrophic cardiomyopathy. Eur. Heart J. 2001 Aug;22 (15):1249–51. doi: 10.1053/euhj.2000.2562. [DOI] [PubMed] [Google Scholar]
- Yu E H, Omran A S, Wigle E D, Williams W G, Siu S C, Rakowski H. Mitral regurgitation in hypertrophic obstructive cardiomyopathy: relationship to obstruction and relief with myectomy. J. Am. Coll. Cardiol. 2000 Dec;36 (7):2219–25. doi: 10.1016/s0735-1097(00)01019-6. [DOI] [PubMed] [Google Scholar]
- Adabag A Selcuk, Maron Barry J, Appelbaum Evan, Harrigan Caitlin J, Buros Jacqueline L, Gibson C Michael, Lesser John R, Hanna Constance A, Udelson James E, Manning Warren J, Maron Martin S. Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 2008 Apr 8;51 (14):1369–74. doi: 10.1016/j.jacc.2007.11.071. [DOI] [PubMed] [Google Scholar]
- Yamaji K, Fujimoto S, Yutani C, Ikeda Y, Mizuno R, Hashimoto T, Nakamura S. Does the progression of myocardial fibrosis lead to atrial fibrillation in patients with hypertrophic cardiomyopathy? Cardiovasc. Pathol. 2002 Jan 5;10 (6):297–303. doi: 10.1016/s1054-8807(01)00086-2. [DOI] [PubMed] [Google Scholar]
- Nakamura Shunichi, Takano Hitoshi, Matsuda Junya, Chinen Daigo, Kitamura Mitsunobu, Murai Koji, Asai Kuniya, Yasutake Masahiro, Takayama Morimasa, Shimizu Wataru. Prognostic values of highly sensitive cardiac troponin T and B-type natriuretic peptide for clinical features in hypertrophic obstructive cardiomyopathy: a cross-sectional study. BMJ Open. 2014;4 (9):e005968. doi: 10.1136/bmjopen-2014-005968. [DOI] [PMC free article] [PubMed] [Google Scholar]