Abstract
The benefits of cardiac imaging are immense, and modern cardiac electrophysiology (EP) requires the extensive and versatile use of a variety of cardiac imaging and radiology-based techniques. In the cardiac electrophysiology lab, doses can range around a reference effective dose (ED) of 15 milliSievert corresponding to 750 chest x-rays for a cardiac radiofrequency ablation, ranging from less than 2 to > 60 mSv. The reference dose for a regular pacemaker or ICD implant is 4 mSv (range 1.4-17) and for a CRT implant is 22 mSv (range 2.2-95). Doses on the order of magnitude of 10-100 milliSievert (mSv) correspond to a low (albeit definite, not negligible) additional lifetime risk of fatal and non-fatal cancer from between 1 in 1000 (10 mSv) to 1 in 100 (100 mSv). The increasing use and complexity of cardiac electrophysiology techniques have not been matched by increasing awareness and knowledge by prescribers and practitioners. The protection of doctors is just as important as protection of patients. Most experienced (and most exposed) interventional cardiologists and electrophysiologists have an exposure per annum of around 5 mSv, two to three times higher than diagnostic radiologists, with a typical cumulative lifetime attributable risk on the order of magnitude of 1 cancer (fatal and non-fatal) per 100 exposed subjects. Operator dose per procedure correlates somewhat with the patient dose, but may be typically 1000 times lower depending upon the shielding employed (one unit of incidence scatter dose for the operator when 1000 units of incident dose are given to the patient). However, adequate radiation protection training and diligent protection can reduce this radiation exposure by 90%.
The priority given to radioprotection in every cardiology department is an effective strategy for primary prevention of cancer, a strong indicator of the quality of the cardiology division, and the most effective shielding for enhancing the safety of patients, doctors, and staff.
Keywords: Radiation, Risk, Electrophysiology
Introduction
Over the last 20 years, interventional electrophysiology (EP) has expanded significantly, in the field of diagnostic studies, ablations, and device implantation. Most of their interventions are performed under fluoroscopic guidance. Therefore, effective dose (ED) to patient of EP procedures can range anywhere from 1 to 100 milliSievert (mSv), equivalent to a radiological risk corresponding to 50 to 5000 chest x-rays. The occupational exposure of cardiac electrophysiologists can be two to three times higher than that of diagnostic radiologists.[1] The increasing use and complexity of EP techniques have not been matched by increasing awareness and knowledge by prescribers and practitioners. Most doctors – including cardiac electrophysiologists and invasive cardiologists – grossly underestimate the radiation doses for most commonly requested tests.[2,3] However, this knowledge is crucial for several reasons. First, the dose is proportional to long-term cancer risk, and therefore it is necessary to be aware of the dose in order to perform a proper risk-benefit assessment, quintessential for evaluating the appropriateness of any given test or procedure. Second, knowing the dose is necessary in order to apply dose optimization, intended to achieve the desired diagnostic information or therapeutic benefit with the lowest necessary dose. Third, radiation awareness is essential for better protection of cardiac electro-physiologists and staff (technicians and nurses), since simple radioprotection knowledge can reduce occupational exposure by tenfold, making one’s professional life longer and healthier. These are three excellent reasons to pursue a policy of radioprotection in the EP lab.
Deterministic And Stochastic Risks In The EP Lab
There are two main biological effects of radiation (Table 1): tissue reactions (deterministic effects), which occur when the radiation dose exceeds a specific threshold and become evident days to months after exposure as a predictable change in tissue occurs, and stochastic effects, which relate to the potential for future harm to the tissue and the body.[3,4]
Table 1. Biological effects of ionizing radiation.
| Tissue reactions (“deterministic”) | Chance damage(“probabilistic”) | |
|---|---|---|
| Dose level | Medium to high | Any |
| Latency period | Short (days or weeks) | Long (years) |
| Threshold dose | Yes | No |
| Biological mechanism | Predominantly cell death | Cell damage |
| Sample clinical effects | Skin lesions | Cancer |
Deterministic (tissue reaction) effects of most concern for patients and operators include skin injuries (reported in patients during long, repeated and complicated interventional procedures). The severity of tissue reactions, rather than probability of occurrence, is proportional to the dose imparted to the tissue. Patient skin injuries may occur when fluoroscopic procedures exceed 20 min, using high-contrast fluoroscopy mode, or 60 min in low-level fluoroscopy. Tissue injury following fluoroscopic guided procedures remains asymptomatic and is often unrecognized as it occurs weeks after the procedure. They usually occur on the patient’s back (where the x-rays are delivered) and many severe cases come to light only through litigation. A case is filed in the US courts every 4 to 5 weeks by patients who have suffered such injuries.
The lens is a radiosensitive tissue, and thus cataract formation is the primary ocular complication associated with ionizing radiation exposure for both patients and doctors. Until recently, the dose threshold for radiation-induced lens opacities was considered 2 Gy for a single dose or 5 Gy for fractionated dose. Currently, radiation-induced cataract, previously thought to be deterministic (tissue reaction), is now recognized to be possibly stochastic in nature, occurring at a much lower radiation exposure level than previously thought. Indeed, several epidemiological studies showed an increased incidence of lens opacities at doses below 0.5 Gy. Accordingly, on April 21, 2011 the International Commission on Radiological Protection (ICRP) slashed the earlier dose limit of 150 mSv in a year for the lens of the eye, to the present 20 mSv in a year, averaged over a defined period of 5 years, with no single year exceeding 50 mSv. Eye cataracts, with the radiation-specific type of posterior sub-capsular opacities, can be observed in one-third of staff after 30 years of work – as a consequence of lack of specific protection and too-permissive limits allowed for the current generation of workers up to 2011.[5]
The stochastic effect of most concern is a carcinogenic effect (in both exposed patients and doctors). It occurs when the cell is modified by damage to its DNA but remains viable, the harm eventually being expressed through cell proliferation. Ionizing radiation damages DNA molecules either directly (though ionization of DNA molecule) or indirectly (through generation of free radicals and reactive oxygen species in the surrounding medium). Cancer may occur after a latency period of many years. Reducing the risk of cancer is at the core of the radioprotection system for patient and staff.
Radiation Doses
The radiation doses of common EP examinations are reported in Table 2. As a reference dose, a conventional chest radiography (single postero-anterior projection) corresponds to 0.02 mSv; a diagnostic coronary angiography to 7 mSv (range 2-16); a percutaneous coronary angioplasty to 15 mSv (7-57); a 64-slice coronary CT to 15 mSv (3-32) and a Sestamibi Myocardial Perfusion Scintigraphy to 9.4 mSv.
Table 2. Doses of common examinations in the EP lab.
AF: atrial fibrillation; AT: atrial tachycardia; VT: ventricular tachycardia; CRT: Cardiac Resynchronization therapy
| Cardiac electrophysiology | Effective dose (mSv) | Equivalent CXRs |
|---|---|---|
| Diagnostic EP studies | 3.2 (1.3–23.9) | 160 |
| Ablation procedure | 15.2 (1.6–59.6) | 760 |
| AF | 16.6 (6.6–59.2) | 830 |
| AT-AVNRT-AVRT | 4.4 (1.6–25) | 220 |
| VT | 12.5 (3 to ≥45) | 625 |
| Regular PM or ICD implant | 4 (1.4–17) | 200 |
| CRT implant | 22 (2.2–95) | 1100 |
On the display of the equipment, values are usually reported as a dose-area product (DAP) or Kerma-area products (KAP) indicating total energy impacting the patient for a given EP procedure. As a general rule, ED can be estimated approximately as follows: ED (mSv)= DAP (Gy x cm2) x 0.2 (mSv/Gy cm2). The conversion factor (from DAP to mSv) is age-specific, and increases with decreasing age (Table 3). Consequently, DAP quantity represents a relevant dosimetry index, the value of which should be optimized against the diagnostic reference level, which varies for each procedure and can be used as a tool to comply with the ALARA (As Low As Reasonably Achievable) principle.
Table 3. Conversion factors: from KAP to effective dose.
KAP: Kerma Area Product
| Radiology | |
|---|---|
| KAP in adults | mSv = KAP (Gy cm2) × 0.2 |
| KAP in 15-year-olds | mSv = KAP (Gy cm2) × 0.4 |
| KAP in 5-year-olds | mSv = KAP (Gy cm2) × 1.0 |
| KAP in 1-year-olds | mSv = KAP (Gy cm2) × 1.9 |
| KAP in newborns | mSv = KAP (Gy cm2) × 3.7 |
The introduction of non-radiology-based methods of cardiac mapping and co-registration of CMR images of the target structures (for instance, the left atrium) could dramatically reduce these doses. The many factors modulating the dose in the EP lab are summarized in Table 4 and can reduce the dose by a factor of 10 to 100.
Table 4. Factors modulating doses in the cardiac EP lab.
RAO: Right Anterior Oblique projection; LAO: left Anterior Oblique projection; KAP: Kerma Area Product; QC: quality control
| Lower doses | Higher doses | ||
|---|---|---|---|
| Operator-dependent | Operator background | Expert | Beginner |
| Training with the simulator | Yes | No | |
| Awareness | Radiation aware | Radiation unaware | |
| Written report | Includes KAP | Omits KAP | |
| Projection | RAO | AP or LAO | |
| Pulsed fluoroscopy | Low rate (≤ 6 fps) | High rate (> 12.5 fps) | |
| Cine duration | Short | Long | |
| Cine substitution by stored fluoroscopy | Yes | No | |
| Fluoroscopy during catheter withdrawal | No | Yes | |
| Collimation | Optimized, and adapted | Wide open, and fixed throughout the procedure | |
| Pelvic radiation | Avoided | During introduction and removal of the catheters | |
| Anesthesiologists/AP | Allowed to halt the procedure | Also exposed when in close proximity | |
| Patient-dependent | Body habitus | Lean | Obese |
| Arrhythmic lesion to be ablated | Supraventricular tachycardia | Atrial fibrillation or VT | |
| Technology-dependent | X-ray system | Tuned for the EP, inspected for QC and maintained | No specific EP settings, not tested, not maintained |
| Combination with the CT(pre-procedural/rotational) | No | Yes | |
| Non-fluoroscopic mapping systems) | Yes (Ensite; Carto; and Mediguide) | No | |
| Shielding | Above and below the table; cabin | Minimal, only above the table |
Protection Of Personnel
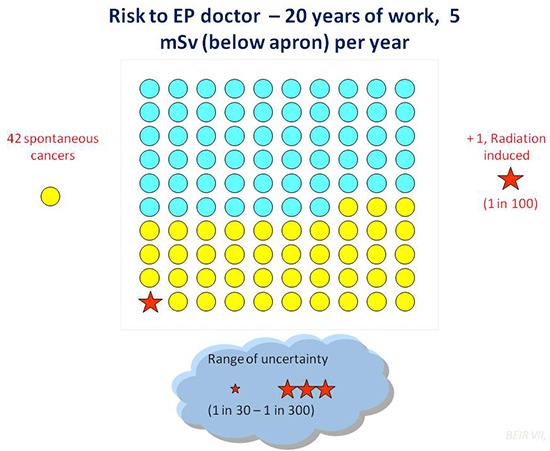
Protection of doctors is just as important as the protection of patients. Most experienced (and most exposed) cardiac electrophysiologists have an exposure per annum of around 5 mSv, two to three times higher than diagnostic radiologists, with a typical cumulative lifetime attributable risk on the order of magnitude of 1 cancer (fatal and non-fatal) per 100 exposed subjects.[6,7] The excess cancer risk may involve more exposed and less well protected organs, such as skin cancer, leukemia, breast cancer in females, and brain cancer.[8] More dose corresponds to greater cancer risk, and recent observational case series described a disproportionate number of tumors in the left side of the brain,[9] the region of the head known to be more exposed to radiation -twice as much compared to the right side.[10]
Operator dose per procedure correlates somewhat with the patient dose, but may be typically 1000 times lower depending upon the shielding employed (one unit of incidence scatter dose for the operator when 1000 units of incidence dose are given to the patient). However, adequate radiation protection training and diligent protection can reduce this radiation exposure by 90%.[10]
The Order Of Magnitude And Risks
A cumulative ED of 100 mSv may be reached by a patient after four ablation procedures plus two or three CT’s, with an extra-risk of cancer of 1 in 100 (Fig. 1). The same cumulative dose of 100 mSv can be reached by an experienced EP after 30 years of work (Fig. 2). This is a “population” risk, and the true individual risk is dictated – as always in medicine – by genetic and environmental factors. For instance, the average dose of 15 mSv confers a risk of one extra-cancer in every 750 exposed 50-year old male patients, but the risk is 38% higher in women, must be multiplied by 4 in children, and reduced by 50% in an 80-year-old man. The risk is higher in presence of some unfavorable polymorphisms of genes involved in DNA repair and in presence of other environmental carcinogens such as smoking. The risk can probably be reduced with chemoprotective strategies, for instance with anti-oxidant cocktails,[11] although the cost-benefit assessment of these strategies remains unsettled.
Figure 1. The dose-effect relationship between radiation exposure and cancer risk over background levels. The solid line indicates the epidemiological evidence, which is conclusive for doses > 50 mSv, and recently expanded with the publication of two medical cohorts of over 800,000 children who underwent CT in Australia and UK. The cumulative dose of 100 mSv corresponds to a 1% extra-risk of cancer over baseline and can be reached after three serial EP procedures and two CTs.

Figure 2. The risk model for the Biological Effects of Ionizing Radiation Committee VII for exposure to low-level radiation predict that about one (red star) out of 100 people would likely develop solid cancer or leukemia from an exposure of 100 mSv above background. About 42 additional people (yellow circles) in the same group would be expected to develop solid cancer or leukemia from other causes. Roughly half of these cancers would result in death. This dose of 100 mSv is reached by 5% of patients in a single cardiac ablation or coronary angiography procedure. [Modified and adapted from ref 6: BEIR VII Health Risks from Exposure to Low levels of Ionizing Radiation, Phase 2. dels-old.nas.edu/dels/rpt_briefs/beir_vii_final.pdf.].
The use of fluoroscopy during invasive fluoroscopy intervention (such as catheter radiofrequency ablation) is likely to result in a small increase in the lifetime risk of a fatal malignancy, and the most likely malignancies will be lung, bone marrow (leukemia) and the breast, the organs exposed to the maximum amount of radiation.[12]
The risk may be acceptable when flanked with a documented or expected benefit, but it is not negligible, and should be spelled out in the informed consent form before the procedure (Table 5). After the examination, the actual delivered dose should be stored in the patient’s and laboratory’s records. This simple process will gently force the doctor to learn what he/she should already know, enabling him/her to make more responsible choices.
Table 5. Terminology that should be used .
RCR: Royal College of Radiology. Adapted and modified from ref.[1]
| Investigation (example) | Effective dose range | Additional lifetime risk of fatal and non-fatal cancer | RCR symbolic representation | Proposed risk term |
|---|---|---|---|---|
| CXR | <0.1 mSv | 1 in 1 million to 1 in 100 000 |

|
Negligible |
| Abdominal X-ray | 0.1-1 mSv | 1 in 100 000 to 1 in 10 000 |


|
Minimal |
| Chest CT | 1-10 mSv | 1 in 10 000 to 1 in 1 000 |



|
Very low |
| PCI | 10-100 mSv | 1 in 1 000 to 1 in 100 |




|
Low |
Novel Opportunities In The EP Lab
The challenges of radioprotection in the EP lab opens exciting new opportunities for the clinician, the researcher, and the pharma and technology industries, in a perspective that will rapidly positively impact on both patients and doctors.
For the clinician, the advent and diffusion of near-zero fluoroscopy techniques will soon lead to a dramatic reduction in delivered doses to patients and also to the operator.
For the researcher, it is essential to move from the current evidence-poor to an evidence-rich milieu, with data directly linking radiation exposure to cancer and non-cancer (including arterial and brain premature aging) effects in our patients and in ourselves as exposed population. In particular, the EP community should play a proactive role in collecting new evidence. In the USA, the Multispecialty Occupational Health Group network triggered a cohort mortality study comparing cancer and other serious disease outcomes (including cardiovascular disease) in 44,000 physicians performing fluoroscopically guided procedures (including interventional cardiologists, cardiac electrophysiologists, radiologists, neuroradiologists and others). In Italy, the Healthy Cath Lab study is organized by the Italian National Research Council – Institute of Clinical Physiology with endorsement by the Italian Society of Invasive Cardiology.[4] The Italian study population will involve 500 exposed interventional cardiologists and staff (technicians and nurses) evaluated by a molecular epidemiology approach to assess “early warning signs” of brain and vascular aging (Table 6). The EP community might decide to join in, since the safety issue is vital for EP doctors and patients.
Table 6. Ongoing studies on interventional cardiologists and electrophysiologists.
NIH: National Institute of Health; NCI: National Cancer Institute
| Main funding | NIH and NCI | Italian CNR National Research Council – IFC, Institute of Clinical Physiology |
|---|---|---|
| Scientific Societies endorsement | Multispecialty Occupational Health Group | Italian Society of Invasive Cardiology (GISE) |
| Enrolled population |
|
|
| Endpoint | Epidemiological clinical endpoints (cancer, cataract, vascular events) | Surrogate biomarkers of genetic, vascular, reproductive, neurocognitive effect |
For the industry, there is growing interest not only in new techniques with near-zero exposure based on non-fluoroscopic navigation, but also for new textile materials for better and more ergonomic shielding for patients and doctors, also based on novel alloys and nano-technology.
Finally, the patient will benefit from these innovations, since in the end radiation doses will drop and the benefit will remain the same, making the EP lab a safer place.[5]
Conclusion
The advent of radioprotection culture in the EP lab is a unique opportunity for today’s generation of professionals, who have the responsibility to change time-honored practices that increase the risk to patients and to us without any benefit. The key messages are simple and direct:
Attention to radioprotection is one aspect – and not the least important – of good practice of EP.
Protecting the patient from an unjustified or unoptimized dose is the best way to protect yourself and your staff.
Before the exam, both you and the patient should know the expected delivered dose (which is directly proportional to the long-term risk).
During the exam, make every effort to keep the dose as low as possible.
After the exam, write the dose down in the records. You and your patient need to know it, because short-term (weeks or months) deterministic (skin ulcers) and long-term (years or decades) stochastic (cancer) risk depend on it.
And finally: a smart EP cannot be afraid of radiation, but must be very afraid of radiation unawareness.
Disclosures
None.
References
- 1.Picano Eugenio, Vañó Eliseo, Rehani Madan M, Cuocolo Alberto, Mont Lluis, Bodi Vicente, Bar Olivier, Maccia Carlo, Pierard Luc, Sicari Rosa, Plein Sven, Mahrholdt Heiko, Lancellotti Patrizio, Knuuti Juhani, Heidbuchel Hein, Di Mario Carlo, Badano Luigi P. The appropriate and justified use of medical radiation in cardiovascular imaging: a position document of the ESC Associations of Cardiovascular Imaging, Percutaneous Cardiovascular Interventions and Electrophysiology. Eur. Heart J. 2014 Mar;35 (10):665–72. doi: 10.1093/eurheartj/eht394. [DOI] [PubMed] [Google Scholar]
- 2.Correia Maria Joao, Hellies Arianna, Andreassi Maria Grazia, Ghelarducci Bruno, Picano Eugenio. Lack of radiological awareness among physicians working in a tertiary-care cardiological centre. Int. J. Cardiol. 2005 Sep 1;103 (3):307–11. doi: 10.1016/j.ijcard.2004.08.070. [DOI] [PubMed] [Google Scholar]
- 3.Kim Candice, Vasaiwala Samip, Haque Faizul, Pratap Kiran, Vidovich Mladen I. Radiation safety among cardiology fellows. Am. J. Cardiol. 2010 Jul 1;106 (1):125–8. doi: 10.1016/j.amjcard.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 4.Picano Eugenio, Vano Eliseo. Radiation exposure as an occupational hazard. EuroIntervention. 2012 Oct;8 (6):649–53. doi: 10.4244/EIJV8I6A101. [DOI] [PubMed] [Google Scholar]
- 5.Heidbuchel Hein, Wittkampf Fred H M, Vano Eliseo, Ernst Sabine, Schilling Richard, Picano Eugenio, Mont Lluis, Jais Pierre, de Bono Joseph, Piorkowski Christopher, Saad Eduardo, Femenia Francisco. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014 Jul;16 (7):946–64. doi: 10.1093/europace/eut409. [DOI] [PubMed] [Google Scholar]
- 6.BEIR VII Health Risks from Exposure to Low Levels of Ionizing Radiation, Phase 2. . http://www.nap.edu/openbook.php?isbn=030909156X. 2014;0:0–0. [PubMed] [Google Scholar]
- 7.Venneri Lucia, Rossi Francesco, Botto Nicoletta, Andreassi Maria Grazia, Salcone Nicoletta, Emad Ahmed, Lazzeri Mauro, Gori Cesare, Vano Eliseo, Picano Eugenio. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council's Biological Effects of Ionizing Radiation VII Report. Am. Heart J. 2009 Jan;157 (1):118–24. doi: 10.1016/j.ahj.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Linet Martha S, Kim Kwang Pyo, Miller Donald L, Kleinerman Ruth A, Simon Steven L, Berrington de Gonzalez Amy. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat. Res. 2010 Dec;174 (6):793–808. doi: 10.1667/RR2014.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roguin Ariel. CardioPulse. Radiation in cardiology: can't live without it! : using appropriate shielding, keeping a distance as safely as possible and reducing radiation time are essential principles for radiation reduction. Eur. Heart J. 2014 Mar;35 (10):599–600. doi: 10.1093/eurheartj/ehu025. [DOI] [PubMed] [Google Scholar]
- 10.Vañó E, González L, Guibelalde E, Fernández J M, Ten J I. Radiation exposure to medical staff in interventional and cardiac radiology. Br J Radiol. 1998 Sep;71 (849):954–60. doi: 10.1259/bjr.71.849.10195011. [DOI] [PubMed] [Google Scholar]
- 11.Andreassi Maria Grazia, Cioppa Angelo, Manfredi Samantha, Neri Maria Giovanna, Foffa Ilenia, Picano Eugenio. N-acetyl cysteine reduces chromosomal DNA damage in circulating lymphocytes during cardiac catheterization procedures: a pilot study. Int. J. Cardiol. 2012 Nov 15;161 (2):93–6. doi: 10.1016/j.ijcard.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Kovoor P, Ricciardello M, Collins L, Uther J B, Ross D L. Risk to patients from radiation associated with radiofrequency ablation for supraventricular tachycardia. Circulation. 1998 Oct 13;98 (15):1534–40. doi: 10.1161/01.cir.98.15.1534. [DOI] [PubMed] [Google Scholar]


