In their latest work, Hillman et al. (1) observe optical path length changes of individual photoreceptor cells in response to light stimulation, noninvasively, in a living human subject. This is a remarkable technical feat, showing the reliable extraction of nanometer-scale changes across the photoreceptor mosaic, although involuntary motion of the target tissue is up to five orders of magnitude larger. The approach combines concepts from holography, optical coherence tomography (OCT), and computational adaptive optics, creating a powerful tool for studying vision, retinal disease, and response to treatment.
The vision process is initiated by phototransduction, which starts with the absorption of photons in the photoreceptor outer segments by photopigments. Impairments of phototransduction or photopigment regeneration lead to vision loss in numerous inherited retinal conditions, such as blue cone monochromacy and achromatopsia.
Importantly, the phototransduction process itself modifies the optical properties of the photoreceptors, by changing the amount of light that they transmit, scatter, or absorb; this allows one to study phototransduction noninvasively using light as a probe. Bleaching, the increase in probe light transmitted through the outer segment when high incident light levels drive a fraction of the photopigment to a nonabsorptive state, is one of the most studied of these phenomena (2). Although bleaching is the most direct result of a light stimulus, scattering (3, 4) and refractive index (5) may also change. These other optical changes, which are more prominent at near-infrared probe wavelengths, have never been fully explained, in part due to contradictory results in the literature derived from different techniques and species. These poorly understood, nonbleaching signals in the photoreceptors have been grouped under the somewhat ambiguous title of “intrinsic optical signals” (IOSs).
How can we pinpoint the origins of the IOSs? One fruitful path has been to use an interferometer, a very sensitive “clock” that measures the time difference, or optical path difference, between two light waves traveling along different paths, by adding them together (Fig. 1). If one or both paths change, the relative phase change of the waves translates into a measurable intensity change. Thus, path length changes can be measured with exquisite precision down to fractions of a wavelength. Jonnal et al. (6) elegantly used the photoreceptors themselves as a biological interferometer, building a flood illumination, adaptive optics ophthalmoscope where the two interfering paths were reflections from the proximal and distal ends of the photoreceptor outer segments (Fig. 1). The resulting oscillations in intensity after a light stimulus suggested that IOSs correlate with a change in the optical path length of the photoreceptors during phototransduction (6).
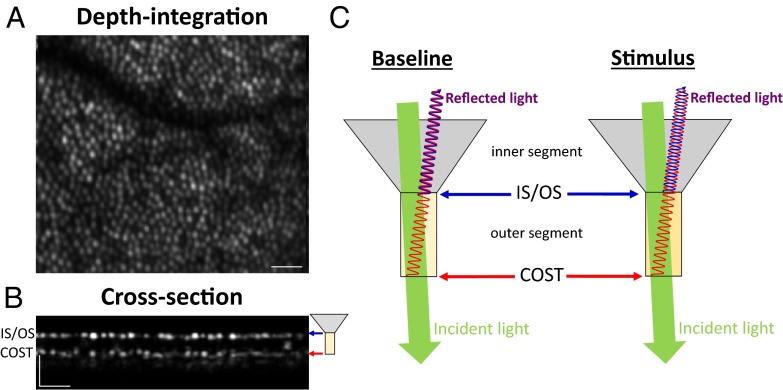
Fig. 1.
By comparing the phases of reflections from both ends of the cone outer segment, Hillman et al. (1) precisely measure nanometer-scale changes in the optical path length of the outer segments. (A) OCT depth-integrated image shows the cone photoreceptor mosaic, and (B) cross-sectional image shows the cone outer segments. OCT images are reproduced with permission (13) with horizontal scale bars of ∼0.1° and vertical scale bars of ∼50 microns. Two reflections, corresponding to the photoreceptor inner segment/outer segment junction (IS/OS, blue) and cone outer segment tips (COST, red), respectively, are evident. (C) During a light stimulus, the change in phase difference between the two reflected waves can quantify the change in optical path length of the outer segments. An innovative full-field, swept-source OCT approach for rapid, volumetric, and phase-stable imaging enables precise registration of datasets acquired over time, overcoming effects of involuntary eye motion. Finally, computational aberration correction achieves single-cell resolution over a wide field of view.
OCT is also an interferometer-based approach in which one of the two interfering light waves is outside of the eye, in a reference path. OCT is widely used in clinical ophthalmology for high-resolution imaging of retinal structure by measuring the echo time delay of back-scattered light. Indeed, using OCT to measure back-scattering changes (7), the elusive IOSs have been localized to the retinal outer segments (8, 9). However, so-called “flying spot” OCT systems, although capable of measuring phase changes corresponding to just a few nanometers of optical path length, are highly susceptible to involuntary motion that is inevitably present in the living retina. Although phase-sensitive OCT has been used to measure outer segment elongation over long time scales (10), reliable detection of changes associated with relatively fast IOSs during phototransduction has proven challenging due to eye motion and limited imaging speeds.
Here Hillman et al. (1) surmount the major technical challenge of eye motion. They accomplished this by using a novel high-speed, complementary metal–oxide–semiconductor (CMOS) camera to build a full-field, swept-source OCT system for retinal imaging. This enabled the rapid acquisition of a series of phase-stabilized volumes at rates of hundreds of volumes per second. With this impressive imaging speed, building on the hypothesis by Jonnal et al. (6), the authors were able to measure elongation of the outer segments by referencing the phase of the proximal outer segment reflection to the phase of the distal one (Fig. 1). Because swept-source OCT can make a direct measurement of optical phase, rather than inferring the phase from the intensity as in Jonnal et al. (6), the results presented here are unambiguous: In response to a light stimulus, the outer segment optical path length increases; that is, the photoreceptor outer segment apparently elongates. If this apparent elongation is due to an increase in refractive index, as it seems to be, this work also helps to explain scattering IOSs. Finally, the authors leveraged a computational adaptive optics approach (11), achieved by postprocessing, to “sharpen” images and perform single photoreceptor measurements. This approach is better suited for the full-field implementation of OCT demonstrated here, because, unlike flying spot systems, it collects all of the light returning from the eye. Ultimately, the results show compelling maps of optical path length changes with single-cell transverse resolution, clearly demonstrating signal specificity to the photoreceptor outer segments.
The results represent the thoughtful application of state-of-the-art technologies to a biological problem that they are almost ideally suited to address. In the future, it will be critical to further apply these technologies to determine precisely which aspects of the phototransduction cascade (12) cause the observed signal, and whether rods and cones can be independently assessed. These basic studies will enable the eventual exploration of numerous questions around scotopic (low light) and photopic (bright light) vision. On the clinical side, the approach is very timely indeed, as gene therapies for inherited conditions affecting photopigments are under development, and some are even starting clinical trials. These technologies might enable new ways of quantitatively monitoring efficacy of these promising therapies.
Acknowledgments
The authors’ research is supported by the Glaucoma Research Foundation Catalyst for a Cure.
Footnotes
Author contributions: V.J.S. and A.D. wrote the paper.
The authors declare no conflict of interest.
See companion article on page 13138.
References
- 1.Hillmann D, et al. In vivo optical imaging of physiological responses to photostimulation in human photoreceptors. Proc Natl Acad Sci USA. 2016;113:13138–13143. doi: 10.1073/pnas.1606428113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masella BD, Hunter JJ, Williams DR. New wrinkles in retinal densitometry. Invest Ophthalmol Vis Sci. 2014;55(11):7525–7534. doi: 10.1167/iovs.13-13795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grieve K, Roorda A. Intrinsic signals from human cone photoreceptors. Invest Ophthalmol Vis Sci. 2008;49(2):713–719. doi: 10.1167/iovs.07-0837. [DOI] [PubMed] [Google Scholar]
- 4.Li YG, Zhang QX, Liu L, Amthor FR, Yao XC. High spatiotemporal resolution imaging of fast intrinsic optical signals activated by retinal flicker stimulation. Opt Express. 2010;18(7):7210–7218. doi: 10.1364/OE.18.007210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeLint PJ, Berendschot TT, van de Kraats J, van Norren D. Slow optical changes in human photoreceptors induced by light. Invest Ophthalmol Vis Sci. 2000;41(1):282–289. [PubMed] [Google Scholar]
- 6.Jonnal RS, et al. In vivo functional imaging of human cone photoreceptors. Opt Express. 2007;15(24):16141–16160. [PMC free article] [PubMed] [Google Scholar]
- 7.Bizheva K, et al. Optophysiology: Depth-resolved probing of retinal physiology with functional ultrahigh-resolution optical coherence tomography. Proc Natl Acad Sci USA. 2006;103(13):5066–5071. doi: 10.1073/pnas.0506997103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Srinivasan VJ, Wojtkowski M, Fujimoto JG, Duker JS. In vivo measurement of retinal physiology with high-speed ultrahigh-resolution optical coherence tomography. Opt Lett. 2006;31(15):2308–2310. doi: 10.1364/ol.31.002308. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki W, Tsunoda K, Hanazono G, Tanifuji M. Stimulus-induced changes of reflectivity detected by optical coherence tomography in macaque retina. Invest Ophthalmol Vis Sci. 2013;54(9):6345–6354. doi: 10.1167/iovs.13-12381. [DOI] [PubMed] [Google Scholar]
- 10.Jonnal RS, Kocaoglu OP, Wang Q, Lee S, Miller DT. Phase-sensitive imaging of the outer retina using optical coherence tomography and adaptive optics. Biomed Opt Express. 2012;3(1):104–124. doi: 10.1364/BOE.3.000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adie SG, Graf BW, Ahmad A, Carney PS, Boppart SA. Computational adaptive optics for broadband optical interferometric tomography of biological tissue. Proc Natl Acad Sci USA. 2012;109(19):7175–7180. doi: 10.1073/pnas.1121193109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pugh EN, Jr, Lamb TD. 2000. Phototransduction in vertebrate rods and cones: Molecular mechanisms of amplification, recovery and light adaptation. Handbook of Biological Physics, eds Stavenga DG, DeGrip WJ, Pugh EN (Elsevier/North-Holland, New York), Vol 3, pp 183−255.
- 13.Pircher M, et al. Temporal changes of human cone photoreceptors observed in vivo with SLO/OCT. Biomed Opt Express. 2010;2(1):100–112. doi: 10.1364/BOE.2.000100. [DOI] [PMC free article] [PubMed] [Google Scholar]