Abstract
Neuromyelitis optica (NMO) is an autoimmune demyelinating disorder of the central nervous system (CNS) with predilection for the optic nerves and spinal cord. Since its emergence in the medical literature in the late 1800’s, the diagnostic criteria for NMO has slowly evolved from the simultaneous presentation of neurologic and ophthalmic signs to a relapsing or monophasic CNS disorder defined by clinical, neuroimaging, and laboratory criteria. Due to the identification of a specific autoantibody response against the astrocyte water channel aquaporin-4 (AQP4) in the vast majority of affected individuals, the clinical spectrum of NMO has greatly expanded necessitating the development of new international criteria for the diagnosis of NMO spectrum disorder (NMOSD). The routine application of new diagnostic criteria for NMOSD in clinical practice will be critical for future refinement and correlation with therapeutic outcomes.
NEUROMYELITIS OPTICA: A CLINICAL DIAGNOSIS
Neuromyelitis optica (NMO) is a rare inflammatory disorder of the central nervous system (CNS) that commonly presents with either monophasic or recurrent attacks of optic neuritis (ON) and transverse myelitis (TM) (1,2). The first clinical account of presumed NMO is often attributed to Sir Clifford Allbutt, a pioneering physician who promoted the adoption of the direct ophthalmoscope in clinical practice (3). However, even before Albutt’s seminal publication, “On the Ophthalmoscopic Signs of Spinal Disease,” clinicopathologic reports of individuals with concurrent vision loss and myelitis by Antoine Portal in 1804, Giovanni Pescetto in 1844, and Jacob Clarke in 1865 likely represent the earliest accounts of NMO in the literature (4). The term “neuro-myélite optique aiguë” was originally coined in 1894 by Eugene Devic and Fernand Gault when they presented a case of concurrent ON and TM and reviewed 16 additional cases from the literature (5). Although their initial article included patients with simultaneous and relapsing episodes of ON and TM, NMO was initially defined as a monophasic disorder. Interestingly, in the early 1900s, more than 100 cases had been reviewed in the literature, and an increasing number of relapsing cases were reported (6).
Wingerchuk et al (2) performed the first systematic evaluation of the demographics, clinical presentation, neuroimaging, and cerebrospinal fluid (CSF) in cases of monophasic and relapsing NMO. “Strict” NMO was defined as bilateral ON and TM occurring within a 2-year interval, whereas NMO “not meeting strict criteria” included cases of unilateral ON or recurrent demyelinating events occurring over greater than a 2-year period. Relapsing cases of NMO, which outnumbered monophasic cases by two-fold, were defined by the occurrence of additional clinical attacks outside the incident event. Although demographics distinguished monophasic and relapsing patients with NMO, common clinical, imaging, and CSF findings allowed the first modern diagnostic criteria to be proposed (Table 1). Several tenets of the 1999 NMO criteria persist in subsequent criteria including the clinical hallmarks of ON and TM, and also spinal cord magnetic resonance imaging (MRI) demonstrating a signal abnormality extending over 3 vertebral segments (longitudinally extensive TM, LETM). Other criteria such as a neutrophilic CSF pleocytosis have been moved to the realm of supportive paraclinical evidence. Minor criteria, such as bilateral ON, severe vision loss, or severe weakness, are no longer considered to have sufficient diagnostic sensitivity.
TABLE 1.
Historical classification of Neuromyelitis Optica and Neuromyelitis Optica Spectrum Disorder
| Wingerchuk 1999 NMO Criteria (2) | Wingerchuk 2006 NMO Criteria (7) | IPND 2015 NMOSD Criteria (8) |
|---|---|---|
| Diagnostic criteria | ||
| All absolute criteria and 1 major or 2 minor supportive criteria Absolute criteria
Major
|
All absolute criteria and 2 supportive criteria Absolute criteria
|
NMOSD with AQP4-IgG
Optic neuritis; acute myelitis; area postrema syndrome (hiccups; nausea and vomiting); acute brainstem syndrome; symptomatic narcolepsy or acute diencephalic clinical syndrome with NMOSD-typical diencephalic MRI lesions (Table 2, Fig. 1); symptomatic cerebral syndrome with NMOSD-typical brain lesions (Table 2, Fig. 1) *AQP4-IgG serology: Cell-based assay is strongly recommended |
| Methodology | ||
| Criteria were defined by chart analysis of the clinical, radiologic, and laboratory data from 71 patients with NMO at the Mayo clinic; there was no independent validation cohort | Criteria were defined by the evaluation of data from 129 patients ascertained through the Mayo Clinic MS Centers in Rochester, MN, and Scottsdale, AZ, and tested for NMO- IgG; there was no independent validation cohort | Criteria were developed by an 18-member panel of NMO physicians from 9 countries; working groups in clinical presentation, neuroimaging, laboratory studies/serology, pediatrics, systemic autoimmunity, and opticospinal MS conducted systematic literature reviews, and initial characteristics for NMOSD were rated and further refined by panel members using electronic surveys and clinical vignettes; those characteristics endorsed by a two-thirds majority were used to develop criteria for AQP4-IgG–seropositive and AQP4-IgG–seronegative NMOSD |
AQP4-IgG, anti–aquaporin-4 immunoglobulin G; CSF, cerebrospinal fluid; IPND, International Panel for NMO Diagnosis; LETM, longitudinally extensive transverse myelitis; MRC, Medical Research Council; MRI, magnetic resonance imaging; MS, multiple sclerosis; NMO, neuro-myelitis optica; NMOSD, neuromyelitis optica spectrum disorder; WBC, white blood cell.
CHANGING FACE OF NEUROMYELITIS OPTICA: AQUAPORIN-4 AUTOANTIBODIES
In 2004, Lennon et al made the groundbreaking observation that most patients with NMO express serum autoantibodies (aquaporin-4 immunoglobulin G [AQP4-IgG]) against the aquaporin-4 (AQP4) water channel (9,10). Subsequently, multiple investigators devised a variety of assays to detect AQP4-IgG in serum and CSF. Although the sensitivity and specificity of individual assays vary, AQP4-IgG seropositivity is generally considered to have 75% sensitivity and 99% specificity for disease (9,11–15). Importantly, AQP4 autoantibodies are typically undetected in clinically definite multiple sclerosis (MS) (9,12,16).
The high specificity of AQP4-IgG for NMO prompted a revision in the diagnostic criteria in 2006 (Table 1). In the revised criteria, NMO was defined by the absolute requirement of simultaneous or sequential attacks of ON and TM, and the presence of 2 of 3 minor criteria: brain MRI inconsistent with MS, LETM, or positive serum AQP4-IgG (7). Using a cohort of 129 patients with NMO and MS, the revised 2006 criteria were found to be 94% sensitive and 96% specific for NMO; in comparison, the original 1999 criteria were only 85% sensitive and 48% specific for disease as assessed on 96 patients with NMO (7).
One of the immediate results of the adoption of AQP4-IgG serology in the revised 2006 criteria was the identification of seropositive patients with spatially limited or atypical clinical presentations. AQP4-IgG–seropositive patients with monophasic or recurrent events of ON or TM were termed NMO spectrum disorders (NMOSDs) (1), and affected individuals often demonstrated additional signs or symptoms of systemic autoimmunity or NMO-specific brain MRI abnormalities (Fig. 1; Table 2) (18). Atypical clinical presentations included protracted nausea and vomiting, narcolepsy, encephalopathy, and brainstem syndromes reflective of lesions in the dorsal medulla (area postrema), hypothalamus, limbic regions, brainstem, and cerebral white matter (1,19). Although not meeting the revised 2006 diagnostic criteria, these clinical presentations were considered formes frustes of disease as they occurred in definite patients with NMO, and affected individuals typically developed future attacks of TM or ON.
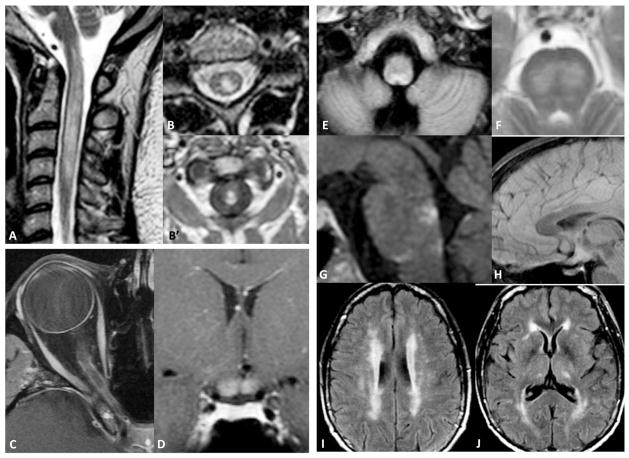
FIG. 1.
Magnetic resonance imaging in neuromyelitis optica spectrum disorders. A. Sagittal T2 scan shows longitudinally extensive cervical cord lesion extending into dorsal medulla. T2 (B) and postcontrast T1 (B′) central spinal cord lesions. C. Postcontrast T1 scan reveals extensive enhancing lesion of the optic nerve. D. Fluid-attenuated inversion recovery (FLAIR) imaging demonstrates bilateral prechiasmal and chiasmal optic nerve inflammation. E. Bilateral FLAIR lesions involve the dorsal medulla (area postrema). F. Bilateral confluent T2 lesions in the mid-pons. G. Sagittal FLAIR image demonstrates periependymal lesions around the fourth ventricle. H. Sagittal FLAIR image reveals diffuse hypothalamic inflammation. Axial FLAIR images show bilateral, confluent deep white matter (I, J) and thalamic (J) lesions.
TABLE 2.
Neuromyelitis Optica Spectrum Disorders—Magnetic Resonance Imaging features and systemic autoimmunity
| Associated MRI and Autoimmune Features of NMOSD |
|---|
| Optic nerve MRI |
| Increased T2 signal (standard T2 or STIR sequences) or T1 gadolinium enhancement of one or both optic nerves (Fig. 1C) |
| Additional characteristic features |
| Lesions are typically long (encompassing more than half of the optic nerve) or involve multiple regions of the nerve |
| Lesions typically involve the posterior, intracranial portion of the optic nerve and optic chiasm (Fig. 1D) |
| Spinal cord MRI |
| Longitudinally extensive lesion demonstrating increased T2 signal (standard T2, proton density, or STIR sequences) involving 3 or more contiguous vertebral segments (Fig. 1A) |
| Central cord predominance (>70% of the lesion residing within the central gray matter) (Fig. 1B) |
| Postcontrast enhancement of the lesion on T1 sequences (Fig. 1B′) |
| Additional characteristic features |
| Rostral extension into brainstem (Fig. 1A) |
| Cord edema |
| Cord atrophy may be observed in cases with long-standing injury |
| Cerebral MRI lesions |
| Large, confluent subcortical or deep white matter lesions (Fig. 1I, J) |
| Long diffuse or edematous corpus callosum lesions (typically involving half the length of the corpus callosum) |
| Diencephalic MRI Lesions |
| Thalamic (Fig. 1J) |
| Hypothalamic lesions (Fig. 1H) |
| Periependymal lesions around the third ventricle |
| Brainstem MRI lesions |
| Lesions of the dorsal medulla (area postrema) (Fig. 1E) |
| Additional characteristic features |
| Unilateral or bilateral lesions (Fig. 1F) |
| Often contiguous with an upper cervical spinal cord lesion (Fig. 1A) |
| Periependymal lesions around the fourth ventricle (Fig. 1G) |
| Extensive postcontrast enhancing periependymal brain lesions |
| Long corticospinal tract lesions involving internal capsule and cerebral peduncle |
| Associated systemic autoimmunity (1,17) |
| Antinuclear autoantibodies |
| Neural autoantibodies (anti-GAD, anti-CRMP5, anti-Ro, anti-VGC, anti-AchR) |
| Autoimmune disorders: thyroiditis, Sjogren disease, systemic lupus erythematosus, myasthenia gravis |
AchR, acetylcholine receptor; CRMP5, collapsin response-mediator protein 5; GAD, glutamic acid decarboxylase; MRI, magnetic resonance imaging; NMOSD, neuromyelitis optica spectrum disorder; STIR, short tau inversion recovery; VGC, voltage-gated channel.
NEUROMYELITIS OPTICA SPECTRUM DISORDERS: NEW INTERNATIONAL CONSENSUS CRITERIA
The rapidly expanding clinical spectrum of patients with seropositive AQP4-IgG required the development of new diagnostic criteria that would capture the clinical experience of physicians and provide a codification for future translational and clinical research. The International Panel for NMO Diagnosis (IPND) was convened in 2011 and tasked with developing new diagnostic criteria based on clinical, laboratory, and neuroimaging data (8). In recognition of accumulating data that the clinical behavior, treatment, and pathology of AQP4-IgG–seropositive patients with incomplete or atypical presentations of NMO are not different from patients fulfilling previous diagnostic criteria (20), the term NMOSD was chosen as a new diagnostic moniker. Because approximately 25% of patients meeting previous NMO criteria were seronegative for AQP4-IgG, separate diagnostic criteria for seronegative NMOSD were formulated using a mixture of clinical and radiologic criteria. The result was the generation of 2 new diagnoses: NMOSD with AQP4-IgG and NMOSD with negative or unknown AQP4-IgG.
The diagnosis of NMOSD with AQP4-IgG requires one of 6 core clinical characteristics and a positive test for AQP4-IgG. The core clinical presentations are distinguished by their neuro-anatomic locations: optic nerve, spinal cord, area postrema (dorsal medulla), diencephalon, brainstem, and cerebrum. Involvement of the optic nerves and spinal cord manifests as ON or TM. ON typically presents as acute vision or visual field loss in one or both eyes, whereas TM may present with a variety of motor, sensory, or sphincter problems. TM is commonly longitudinally extensive (3 or more vertebral segments) (Fig. 1A), involving the central cord (Fig. 1B) with contrast enhancement (Fig. 1B’). Optic nerve lesions are typically gadolinium enhancing and extensive (Fig. 1C) and often involve the prechiasmatic optic nerve and optic chiasm (Fig. 1D). An area postrema syndrome (incidence: 16%–43%) (19,21,22) is characterized by intractable hiccups or nausea/vomiting occurring for 7 consecutive days without, or 2 days with, an accompanying MRI lesion in the dorsal medulla (Fig. 1E). Acute brainstem symptoms include ocular motor, motor, sensory, or cerebellar dysfunction associated with parenchymal (Fig. 1F) or ependymal lesions (Fig. 1G) that may or may not be contiguous with spinal cord injury (Fig. 1A). Diencephalic syndromes include hypersomnolence, narcolepsy, anorexia, hypothermia, hypo-natremia, and behavioral changes associated with a MRI lesion in the thalamus, hypothalamus, or third ventricular region (Fig. 1H, J). Cerebral syndromes include hemiparesis, hemi-sensory loss, encephalopathy, postchiasmal visual field loss, and cortical vision loss that are often associated with large, confluent subcortical or deep white matter lesions (Fig. 1I, J).
Because of increased sensitivity (14,15,23), cell-based serum assays using microscopy-based or flow cytometry–based detection are recommended for AQP4-IgG serologic testing. Enzyme-linked immunosorbent assay (ELISA) and indirect immunofluorescence (IIF) of tissue sections are typically less sensitive and often yield lower-titer and false-positive tests (24,25). Therefore, caution is recommended in making a diagnosis of NMOSD with AQP4-IgG in cases where low-titer AQP4-IgG is detected by ELISA or IIF, and symptoms are outside the 3 most common core clinical presentations: ON, TM, or area postrema syndrome. Confirmatory testing using more than one assay is generally recommended.
A diagnosis of NMOSD without AQP4-IgG requires additional clinical and radiologic criteria that are not mandated for seropositive patients. Patients with NMOSD who do not have detectable AQP4-IgG must have a minimum of 2 core clinical presentations, and 1 presentation must be ON, TM, or an area postrema syndrome. The clinical presentation may be simultaneous or sequential. Additional radiologic criteria are required based on the type of core presentation. For ON, the brain MRI should be normal if the optic nerve lesion is not extensive (half the length of the optic nerve) or involving the optic chiasm. For TM, spinal cord MRI should demonstrate a central medullary lesion or focal atrophy involving 3 contiguous segments. Area postrema syndromes require a dorsal medulla lesion, and acute brainstem syndromes should demonstrate periependymal lesions. These additional radiologic criteria were deemed necessary to provide additional specificity for NMOSD in the absence of AQP4-IgG. Because patients may convert to a positive AQP4-IgG serostatus over time, repeat serologic testing is recommended in relapsing seronegative patients before immunosuppressive or B-cell ablative therapies are initiated. Rarely, AQP4-IgG has been detected only in CSF (26,27). Therefore, routine CSF testing of AQP4-IgG–seronegative patients is generally not recommended. Additional CSF features such as extensive pleocytosis (>50 leukocytes/ μL), presence of neutrophils or eosinophils (>5/μL), absence of oligoclonal bands, or elevation of glial fibrillary acidic protein are considered supportive but not confirmatory evidence of NMOSD (2,28,29).
Because the diagnosis of NMOSD without AQP4-IgG may be difficult, the 2015 IPND criteria highlight multiple “red flags” that should caution clinicians against a NMOSD diagnosis. Clinical red flags include progressive disease course, hyperacute onset (<4 hours to symptom nadir), presence of CSF oligoclonal bands, partial TM, chronic infection, or clinical features suggestive of cancer or sarcoidosis (8). Radiologic red flags include brain MRI findings suggestive of MS, persistent contrast enhancement, (>3 months) short and predominantly peripheral spinal cord lesions, and diffuse, indistinct T2-weighted lesions (8).
NEUROMYELITIS SPECTRUM DISORDERS: MOVING FORWARD IN CLINICAL PRACTICE
The 2015 IPND criteria represent a substantial departure from previous diagnostic measures. In the near term, the institution of the new NMOSD criteria in clinical practice will facilitate the early identification of AQP4-IgG–seropositive patients. Previous diagnostic criteria had required the simultaneous or sequential presentation of ON and TM. In clinical practice, however, patients with atypical presentations related to cerebral, diencephalic, and brainstem pathology had been reported in association with AQP4-IgG, and their subsequent clinical course often included ON and LETM. The inclusion of these individuals, along with AQP4-IgG–seropositive patients with isolated or recurrent events of ON and TM, under the umbrella of NMOSD will allow rapid adoption of prophylactic therapy and aggressive treatment of acute attacks. As neurologists and ophthalmologists recognize the core clinical symptoms of NMOSD, by presentation or history, serologic testing for AQP4-IgG will expand leading to earlier diagnosis. In addition, the recognition of clinical presentations and neuroimaging typical of NMOSD will foster testing of AQP4-IgG in high-risk monosymptomatic cases of ON or TM. For instance, in monosymptomatic ON, bilateral ON, poor visual recovery (<20/200), severe visual field depression, altitudinal visual field loss, posterior nerve or optic chiasm involvement, extensive visual pathway lesions, or severe and diffuse peripapillary retinal nerve fiber layer loss should prompt AQP4-IgG testing (30–36).
In the long term, the 2015 IPND criteria also will be a guide for evaluating the natural history and treatment response of AQP4-IgG–seronegative patients. Patients with NMO diagnosed by the 2006 Wingerchuk criteria may transition between AQP4-IgG seropositive and seronegative states, indicating that all AQP4-IgG–seronegative cases are not merely phenotypic mimics. Therefore, monitoring the progress of patients meeting criteria for NMOSD without AQP4-IgG will be critical for developing future diagnostic criteria that delineate those patients with seronegative NMOSD at high risk for relapse and those that are responsive to therapy.
Nevertheless, multiple investigations on independent cohorts of patients with AQP4-IgG–seronegative NMO have demonstrated distinct demographics and clinical characteristics (37). AQP4-IgG–seronegative patients are more often Caucasian (38,39); show a lower female/male ratio (38–41); have a shorter disease duration (38); are more frequently monophasic (40,42); exhibit fewer features of concurrent autoimmunity (40,42); and more often present with simultaneous ON and TM (38–40). These distinctions suggest that a significant portion of seronegative patients represent disorders with overlapping phenotypic presentations of ON and TM. Similar demographic and clinical distinctions have been observed among a small fraction of AQP4-IgG–seronegative patients who are sero-positive for antibodies against myelin oligodendrocyte glycoprotein immunoglobulin G (MOG-IgG) (43,44). The 2015 IPND NMOSD criteria may differentiate some cohorts of patients previously labeled as seronegative NMO and may identify alternative cohorts at higher risk for relapse. Indeed, 2 studies with longer follow-up have revealed that a significant fraction of NMO-seronegative patients have disease recurrence (38,39).
Interestingly, the initial application of the new 2015 IPND NMOSD criteria in clinical practice has demonstrated enhanced diagnostic sensitivity. In adult cohorts, the 2015 IPND NMOSD criteria identified novel AQP4-IgG–seronegative patients (45,46), and, because of the need for only a single core presentation (8), detected AQP4-IgG–seropositive patients significantly faster following symptom onset (45). As a result, patients with NMOSD at risk for future relapse and disability progression are likely to be rapidly identified and treated. Similarly, in a study of pediatric patients with demyelinating disease, 97% of the panel-defined patients with NMOSD were correctly identified by the IPND 2015 NMOSD criteria; however, only 49% were diagnosed by 2006 Wingerchuk NMO criteria. This may be due in part to the distinct presentations of pediatric and adult NMO cases (47) and the new diagnostic criteria for monophasic AQP4-IgG–seropositive patients (8).
FUTURE CLASSIFICATION OF NEUROMYELITIS SPECTRUM DISORDERS
Each iteration of diagnostic criteria for NMO has attempted to aid clinicians in the recognition of this relatively rare but devastating CNS inflammatory disorder. Although the gold standard of diagnostic accuracy, lesion histopathology (48,49), remains unobtainable in most cases, the progressive incorporation of new clinical, radiologic, and serologic criteria seems to be improving both diagnostic sensitivity and specificity. Nonetheless, because of the limited sensitivity of the AQP4-IgG serologic assay and the limited specificity of clinical and radiologic presentations, a clear categorization of NMOSD among other demyelinating disorders remains murky.
The ultimate classification of NMOSD may be molecular (50), using multiple discrete biomarkers to combine seemingly diverse demyelinating disorders into a common nosologic category based on shared immunopathology and histopathology. For NMOSD, progress has been made in the identification of potential cellular, serum, and CSF bio-markers (51). The most notable has been AQP4-IgG, a serum biomarker of humoral immunopathology that is highly specific for NMOSD and has important prognostic and therapeutic implications. Unfortunately, additional bi-omarkers of NMOSD immunopathology and CNS injury (51) lack the sensitivity and specificity to provide successful categorization of all cases of seronegative NMOSD (46). In addition, it remains unclear which cases of clinically defined AQP4-IgG–seronegative NMOSD show NMO-specific lesional histopathology.
As noted previously, approximately 20% of AQP4-IgG–seronegative patients are seropositive for MOG-IgG. Multiple immunologic and histopathologic features of MOG-IgG–seropositive NMOSD indicate that this condition is nosologically distinct from AQP4-IgG–seropositive NMOSD despite its overlapping clinical presentation. Patients with MOG-IgG–seropositive NMOSD are typically male and more often have simultaneous ON and TM, monophasic disease, inflammation of the conus, cauda equina, and deep brain nuclei, and improved functional recovery (43,44). The intracerebral microinjection of MOG-IgG–seropositive patient serum into murine brain produces no inflammation or significant CNS injury (52), and brain lesions from a patient with MOG-IgG–seropositive NMOSD revealed MS-type II pathology (53). The combined clinical and experimental data indicate that MOG-IgG–seropositive patients with TM and ON should be classified outside NMOSD and may represent a subgroup of patients with MS or acute disseminated encephalomyelitis.
A molecular classification of demyelinating disorders may ultimately require substantial advances in technology to reach fruition. Improvement in serologic, radiologic, and immunologic assays is likely to be required to reach levels of sensitivity and specificity necessary to delineate closely aligned demyelinating disorders with overlapping clinical presentations and immunopathologies. High throughput analysis of large biologic data sets from affected individuals may hold the key to discovering groups of biomarkers that can define molecular boundaries between NMOSD and phenotypic mimics. Ultimately, a molecular nosology of CNS demyelinating disorders will result in targeted immunotherapy and improved clinical outcomes in patients with NMOSD.
Footnotes
The author reports no conflicts of interest.
References
- 1.Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG. The spectrum of neuromyelitis optica. Lancet Neurol. 2007;6:805–815. doi: 10.1016/S1474-4422(07)70216-8. [DOI] [PubMed] [Google Scholar]
- 2.Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic’s syndrome) Neurology. 1999;53:1107–1114. doi: 10.1212/wnl.53.5.1107. [DOI] [PubMed] [Google Scholar]
- 3.Allbutt T. On the ophthalmoscopic signs of spinal disease. Lancet. 1870;95:76–78. [Google Scholar]
- 4.Jarius S, Wildemann B. The case of the Marquis de Causan (1804): an early account of visual loss associated with spinal cord inflammation. J Neurol. 2012;259:1354–1357. doi: 10.1007/s00415-011-6355-8. [DOI] [PubMed] [Google Scholar]
- 5.Devic E. Myelite Aigue compliquee de nevrite optique. Bull Med (paris) 1894;8:1033–1034. [Google Scholar]
- 6.Balser BH. Neuromyelitis optica. Brain. 1936;59:353–365. [Google Scholar]
- 7.Wingerchuk D, Lennon V, Pittock S, Lucchinetti C, Weinshenker B. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485–1489. doi: 10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 8.Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, de Seze J, Fujihara K, Greenberg B, Jacob A, Jarius S, Lana-Peixoto M, Levy M, Simon JH, Tenembaum S, Traboulsee AL, Waters P, Wellik KE, Weinshenker BG International Panel for NMOD. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–189. doi: 10.1212/WNL.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lennon V, Wingerchuk D, Kryzer T, Pittock S, Lucchinetti C, Fujihara K, Nakashima I, Weinshenker B. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–2112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 10.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–477. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mader S, Lutterotti A, Di Pauli F, Kuenz B, Schanda K, Aboul-Enein F, Khalil M, Storch MK, Jarius S, Kristoferitsch W, Berger T, Reindl M. Patterns of antibody binding to aquaporin-4 isoforms in neuromyelitis optica. PLoS One. 2010;5:e10455. doi: 10.1371/journal.pone.0010455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalluri SR, Illes Z, Srivastava R, Cree B, Menge T, Bennett JL, Berthele A, Hemmer B. Quantification and functional characterization of antibodies to native aquaporin 4 in neuromyelitis optica. Arch Neurol. 2010;67:1201–1208. doi: 10.1001/archneurol.2010.269. [DOI] [PubMed] [Google Scholar]
- 13.Matsuoka T, Matsushita T, Kawano Y, Osoegawa M, Ochi H, Ishizu T, Minohara M, Kikuchi H, Mihara F, Ohyagi Y, Kira J. Heterogeneity of aquaporin-4 autoimmunity and spinal cord lesions in multiple sclerosis in Japanese. Brain. 2007;130:1206–1223. doi: 10.1093/brain/awm027. [DOI] [PubMed] [Google Scholar]
- 14.Waters PJ, McKeon A, Leite MI, Rajasekharan S, Lennon VA, Villalobos A, Palace J, Mandrekar JN, Vincent A, Bar-Or A, Pittock SJ. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology. 2012;78:665–671. doi: 10.1212/WNL.0b013e318248dec1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waters PJ, Pittock SJ, Bennett JL, Jarius S, Weinshenker BG, Wingerchuk DM. Evaluation of aquaporin-4 antibody assays. Clin Exp Neuroimmunol. 2014;5:290–303. doi: 10.1111/cen3.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paul F, Jarius S, Aktas O, Bluthner M, Bauer O, Appelhans H, Franciotta D, Bergamaschi R, Littleton E, Palace J, Seelig HP, Hohlfeld R, Vincent A, Zipp F. Antibody to aquaporin 4 in the diagnosis of neuromyelitis optica. PLoS Med. 2007;4:e133. doi: 10.1371/journal.pmed.0040133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKeon A, Lennon VA, Jacob A, Matiello M, Lucchinetti CF, Kale N, Chan KH, Weinshenker BG, Apiwattinakul M, Wingerchuk DM, Pittock SJ. Coexistence of myasthenia gravis and serological markers of neurological autoimmunity in neuromyelitis optica. Muscle Nerve. 2009;39:87–90. doi: 10.1002/mus.21197. [DOI] [PubMed] [Google Scholar]
- 18.Pittock S, Lennon V, Krecke K, Wingerchuk D, Lucchinetti C, Weinshenker B. Brain abnormalities in neuromyelitis optica. Arch Neurol. 2006;63:390–396. doi: 10.1001/archneur.63.3.390. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi T, Miyazawa I, Misu T, Takano R, Nakashima I, Fujihara K, Tobita M, Itoyama Y. Intractable hiccup and nausea in neuromyelitis optica with anti-aquaporin-4 antibody: a herald of acute exacerbations. J Neurol Neurosurg Psychiatr. 2008;79:1075–1078. doi: 10.1136/jnnp.2008.145391. [DOI] [PubMed] [Google Scholar]
- 20.Sato DK, Nakashima I, Takahashi T, Misu T, Waters P, Kuroda H, Nishiyama S, Suzuki C, Takai Y, Fujihara K, Itoyama Y, Aoki M. Aquaporin-4 antibody-positive cases beyond current diagnostic criteria for NMO spectrum disorders. Neurology. 2013;80:2210–2216. doi: 10.1212/WNL.0b013e318296ea08. [DOI] [PubMed] [Google Scholar]
- 21.Apiwattanakul M, Popescu BF, Matiello M, Weinshenker BG, Lucchinetti CF, Lennon VA, McKeon A, Carpenter AF, Miller GM, Pittock SJ. Intractable vomiting as the initial presentation of neuromyelitis optica. Ann Neurol. 2010;68:757–761. doi: 10.1002/ana.22121. [DOI] [PubMed] [Google Scholar]
- 22.Misu T, Fujihara K, Nakashima I, Sato S, Itoyama Y. Intractable hiccup and nausea with periaqueductal lesions in neuromyelitis optica. Neurology. 2005;65:1479–1482. doi: 10.1212/01.wnl.0000183151.19351.82. [DOI] [PubMed] [Google Scholar]
- 23.Jarius S, Wildemann B. Aquaporin-4 antibodies (NMO-IgG) as a serological marker of neuromyelitis optica: a critical review of the literature. Brain Pathol. 2013;23:661–683. doi: 10.1111/bpa.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jarius S, Franciotta D, Paul F, Bergamaschi R, Rommer PS, Ruprecht K, Ringelstein M, Aktas O, Kristoferitsch W, Wildemann B. Testing for antibodies to human aquaporin-4 by ELISA: sensitivity, specificity, and direct comparison with immunohistochemistry. J Neurol Sci. 2012;320:32–37. doi: 10.1016/j.jns.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Pittock SJ, Lennon VA, Bakshi N, Shen L, McKeon A, Quach H, Briggs FB, Bernstein AL, Schaefer CA, Barcellos LF. Seroprevalence of aquaporin-4-IgG in a northern California population representative cohort of multiple sclerosis. JAMA Neurol. 2014;71:1433–1436. doi: 10.1001/jamaneurol.2014.1581. [DOI] [PubMed] [Google Scholar]
- 26.McKeon A, Pittock SJ, Lennon VA. CSF complements serum for evaluating paraneoplastic antibodies and NMO-IgG. Neurology. 2011;76:1108–1110. doi: 10.1212/WNL.0b013e318211c379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarius S, Franciotta D, Paul F, Ruprecht K, Bergamaschi R, Rommer PS, Reuss R, Probst C, Kristoferitsch W, Wandinger KP, Wildemann B. Cerebrospinal fluid antibodies to aquaporin-4 in neuromyelitis optica and related disorders: frequency, origin, and diagnostic relevance. J Neuroinflammation. 2010;7:52. doi: 10.1186/1742-2094-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarius S, Paul F, Franciotta D, Ruprecht K, Ringelstein M, Bergamaschi R, Rommer P, Kleiter I, Stich O, Reuss R, Rauer S, Zettl UK, Wandinger KP, Melms A, Aktas O, Kristoferitsch W, Wildemann B. Cerebrospinal fluid findings in aquaporin-4 antibody positive neuromyelitis optica: results from 211 lumbar punctures. J Neurol Sci. 2011;306:82–90. doi: 10.1016/j.jns.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 29.Misu T, Takano R, Fujihara K, Takahashi T, Sato S, Itoyama Y. Marked increase in cerebrospinal fluid glial fibrillar acidic protein in neuromyelitis optica: an astrocytic damage marker. J Neurol Neurosurg Psychiatry. 2009;80:575–577. doi: 10.1136/jnnp.2008.150698. [DOI] [PubMed] [Google Scholar]
- 30.Fernandes DB, de Ramos RI, Falcochio C, Apostolos-Pereira S, Callegaro D, Monteiro ML. Comparison of visual acuity and automated perimetry findings in patients with neuromyelitis optica or multiple sclerosis after single or multiple attacks of optic neuritis. J Neuroophthalmol. 2012;32:102–106. doi: 10.1097/WNO.0b013e31823a9ebc. [DOI] [PubMed] [Google Scholar]
- 31.Khanna S, Sharma A, Huecker J, Gordon M, Naismith RT, Van Stavern GP. Magnetic resonance imaging of optic neuritis in patients with neuromyelitis optica versus multiple sclerosis. J Neuroophthalmol. 2012;32:216–220. doi: 10.1097/WNO.0b013e318254c62d. [DOI] [PubMed] [Google Scholar]
- 32.Costa C, Arrambide G, Tintore M, Castillo J, Sastre-Garriga J, Tur C, Rio J, Saiz A, Vidal-Jordana A, Auger C, Nos C, Rovira A, Comabella M, Horga A, Montalban X. Value of NMO-IgG determination at the time of presentation as CIS. Neurology. 2012;78:1608–1611. doi: 10.1212/WNL.0b013e3182563b32. [DOI] [PubMed] [Google Scholar]
- 33.Storoni M, Davagnanam I, Radon M, Siddiqui A, Plant GT. Distinguishing optic neuritis in neuromyelitis optica spectrum disease from multiple sclerosis: a novel magnetic resonance imaging Scoring system. J Neuroophthalmol. 2013;33:123–127. doi: 10.1097/WNO.0b013e318283c3ed. [DOI] [PubMed] [Google Scholar]
- 34.Green AJ, Cree BAC. Distinctive retinal nerve fibre layer and vascular changes in neuromyelitis optica following optic neuritis. J Neurol Neurosurg Psychiatr. 2009;80:1002–1005. doi: 10.1136/jnnp.2008.166207. [DOI] [PubMed] [Google Scholar]
- 35.Naismith RT, Tutlam NT, Xu J, Klawiter EC, Shepherd J, Trinkaus K, Song S-K, Cross AH. Optical coherence tomography differs in neuromyelitis optica compared with multiple sclerosis. Neurology. 2009;72:1077–1082. doi: 10.1212/01.wnl.0000345042.53843.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ratchford JN, Quigg ME, Conger A, Frohman T, Frohman E, Balcer LJ, Calabresi PA, Kerr DA. Optical coherence tomography helps differentiate neuromyelitis optica and MS optic neuropathies. Neurology. 2009;73:302–308. doi: 10.1212/WNL.0b013e3181af78b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernard-Valnet R, Liblau RS, Vukusic S, Marignier R. Neuromyelitis optica: a positive appraisal of seronegative cases. Eur J Neurol. 2015;22:1511–1518. e1582–1513. doi: 10.1111/ene.12679. [DOI] [PubMed] [Google Scholar]
- 38.Jiao Y, Fryer JP, Lennon VA, Jenkins SM, Quek AM, Smith CY, McKeon A, Costanzi C, Iorio R, Weinshenker BG, Wingerchuk DM, Shuster EA, Lucchinetti CF, Pittock SJ. Updated estimate of AQP4-IgG serostatus and disability outcome in neuromyelitis optica. Neurology. 2013;81:1197–1204. doi: 10.1212/WNL.0b013e3182a6cb5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marignier R, Bernard-Valnet R, Giraudon P, Collongues N, Papeix C, Zephir H, Cavillon G, Rogemond V, Casey R, Frangoulis B, De Seze J, Vukusic S, Honnorat J, Confavreux C, Group NS. Aquaporin-4 antibody-negative neuromyelitis optica: distinct assay sensitivity-dependent entity. Neurology. 2013;80:2194–2200. doi: 10.1212/WNL.0b013e318296e917. [DOI] [PubMed] [Google Scholar]
- 40.Jarius S, Ruprecht K, Wildemann B, Kuempfel T, Ringelstein M, Geis C, Kleiter I, Kleinschnitz C, Berthele A, Brettschneider J, Hellwig K, Hemmer B, Linker RA, Lauda F, Mayer CA, Tumani H, Melms A, Trebst C, Stangel M, Marziniak M, Hoffmann F, Schippling S, Faiss JH, Neuhaus O, Ettrich B, Zentner C, Guthke K, Hofstadtvan Oy U, Reuss R, Pellkofer H, Ziemann U, Kern P, Wandinger KP, Bergh FT, Boettcher T, Langel S, Liebetrau M, Rommer PS, Niehaus S, Munch C, Winkelmann A, Zettl UU, Metz I, Veauthier C, Sieb JP, Wilke C, Hartung HP, Aktas O, Paul F. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a multicentre study of 175 patients. J Neuroinflammation. 2012;9:14. doi: 10.1186/1742-2094-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang Y, Huang DH, Wu WP, Wu L, Chen LF, Wu Q. The role of aquaporin-4 antibodies in Chinese patients with neuromyelitis optica. J Clin Neurosci. 2013;20:94–98. doi: 10.1016/j.jocn.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 42.Akman-Demir G, Tuzun E, Waters P, Icoz S, Kurtuncu M, Jarius S, Yapici Z, Mutlu M, Yesilot N, Vincent A, Eraksoy M. Prognostic implications of aquaporin-4 antibody status in neuromyelitis optica patients. J Neurol. 2011;258:464–470. doi: 10.1007/s00415-010-5780-4. [DOI] [PubMed] [Google Scholar]
- 43.Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, Kuker W, Chandratre S, Vincent A, Palace J. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA Neurol. 2014;71:276–283. doi: 10.1001/jamaneurol.2013.5857. [DOI] [PubMed] [Google Scholar]
- 44.Sato DK, Callegaro D, Lana-Peixoto MA, Waters PJ, de Haidar Jorge FM, Takahashi T, Nakashima I, Apostolos-Pereira SL, Talim N, Simm RF, Lino AM, Misu T, Leite MI, Aoki M, Fujihara K. Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology. 2014;82:474–481. doi: 10.1212/WNL.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hyun JW, Jeong IH, Joung A, Kim SH, Kim HJ. Evaluation of the 2015 diagnostic criteria for neuromyelitis optica spectrum disorder. Neurology. 2016;86:1–8. doi: 10.1212/WNL.0000000000002655. [DOI] [PubMed] [Google Scholar]
- 46.Uzawa A, Mori M, Uchida T, Masuda H, Ohtani R, Kuwabara S. Seronegative neuromyelitis optica spectrum disorder patients diagnosed using new diagnostic criteria. Mult Scler. doi: 10.1177/1352458515615954. published ahead of print November 9, 2015. doi:10.1177/ 1352458515615954. [DOI] [PubMed] [Google Scholar]
- 47.McKeon A, Lennon VA, Lotze T, Tenenbaum S, Ness JM, Rensel M, Kuntz NL, Fryer JP, Homburger H, Hunter J, Weinshenker BG, Krecke K, Lucchinetti CF, Pittock SJ. CNS aquaporin-4 autoimmunity in children. Neurology. 2008;71:93–100. doi: 10.1212/01.wnl.0000314832.24682.c6. [DOI] [PubMed] [Google Scholar]
- 48.Lucchinetti CF, Mandler RN, McGavern D, Bruck W, Gleich G, Ransohoff RM, Trebst C, Weinshenker B, Wingerchuk D, Parisi JE, Lassmann H. A role for humoral mechanisms in the pathogenesis of Devic’s neuromyelitis optica. Brain. 2002;125:1450–1461. doi: 10.1093/brain/awf151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Misu T, Höftberger R, Fujihara K, Wimmer I, Takai Y, Nishiyama S, Nakashima I, Konno H, Bradl M, Garzuly F, Itoyama Y, Aoki M, Lassmann H. Presence of six different lesion types suggests diverse mechanisms of tissue injury in neuromyelitis optica. Acta Neuropathol. 2013;125:815–827. doi: 10.1007/s00401-013-1116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pittock SJ. Demyelinating disease: NMO spectrum disorders: clinical or molecular classification? Nat Rev Neurol. 2016;12:129–130. doi: 10.1038/nrneurol.2016.9. [DOI] [PubMed] [Google Scholar]
- 51.Melamed E, Levy M, Waters PJ, Sato DK, Bennett JL, John GR, Hooper DC, Saiz A, Bar-Or A, Kim HJ, Pandit L, Leite MI, Asgari N, Kissani N, Hintzen R, Marignier R, Jarius S, Marcelletti J, Smith TJ, Yeaman MR, Han MH, Aktas O, Apiwattanakul M, Banwell B, Bichuetti D, Broadley S, Cabre P, Chitnis T, De Seze J, Fujihara K, Greenberg B, Hellwig K, Iorio R, Jarius S, Klawiter E, Kleiter I, Lana-Peixoto M, Nakashima I, O’Connor K, Palace J, Paul F, Prayoonwiwat N, Ruprecht K, Stuve O, Tedder T, Tenembaum S, Garrahan JP, Aires B, van Herle K, van Pelt D, Villoslada P, Waubant E, Weinshenker B, Wingerchuk D, Wurfel J, Zamvil S. Update on biomarkers in neuromyelitis optica. Neurol Neuroimmunol Neuroinflamm. 2015;2:e134. doi: 10.1212/NXI.0000000000000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saadoun S, Waters P, Owens GP, Bennett JL, Vincent A, Papadopoulos MC. Neuromyelitis optica MOG-IgG causes reversible lesions in mouse brain. Acta Neuropathol Commun. 2014;2:35. doi: 10.1186/2051-5960-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spadaro M, Gerdes LA, Mayer MC, Ertl-Wagner B, Laurent S, Krumbholz M, Breithaupt C, Hogen T, Straube A, Giese A, Hohlfeld R, Lassmann H, Meinl E, Kumpfel T. Histopathology and clinical course of MOG-antibody-associated encephalomyelitis. Ann Clin Transl Neurol. 2015;2:295–301. doi: 10.1002/acn3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]