Abstract
A patient with newly diagnosed right lung cancer had transient 18F-fluorodeoxyglucose (FDG)-avid left axillary lymph nodes and intense splenic FDG uptake on positron emission tomography (PET)/computed tomography (CT). History revealed that the patient received a left-sided influenza vaccine 2–3 days before the examination. Although inflammatory FDG uptake in ipsilateral axillary nodes is reported, to our knowledge, this is the first report of visualization of the systemic immune response in the spleen related to the influenza vaccination on FDG-PET/CT. The history, splenic uptake and time course on serial FDG-PET/CT helped to avoid a false-positive interpretation for progressing lung cancer and alteration of the radiation therapy plan.
Keywords: FDG, FDG-PET/CT, Vaccine, Spleen, Lung cancer, Immunization
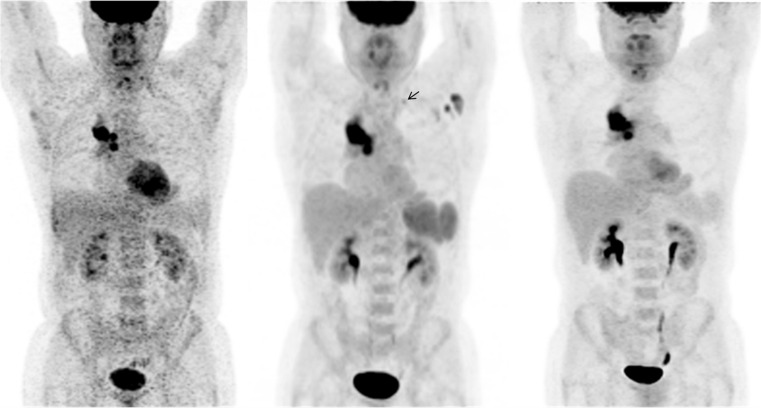
Fig. 1.
Initial staging 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET)/computed tomography (CT) was performed in a 55-year-old man with right lung cancer. Maximum intensity projection (MIP) images show the metabolically active right lung mass and ipsilateral hilar metastases, but also new enlarging FDG-avid left axillary lymph nodes, a left supraclavicular lymph node, and intense splenic FDG uptake (middle) compared to an FDG-PET/CT scan performed at an outside institution two months prior (left). The splenic uptake raised the question of a systemic inflammatory process and further questioning revealed that the patient received an influenza vaccine in the left upper extremity 2–3 days before the examination (middle). Since contralateral metastases would alter management, FDG-PET/CT was performed 12 days later without interval therapy (right). Left axillary and supraclavicular nodal and splenic FDG uptake resolved and was presumably due to local and systemic immune-mediated responses to the vaccine
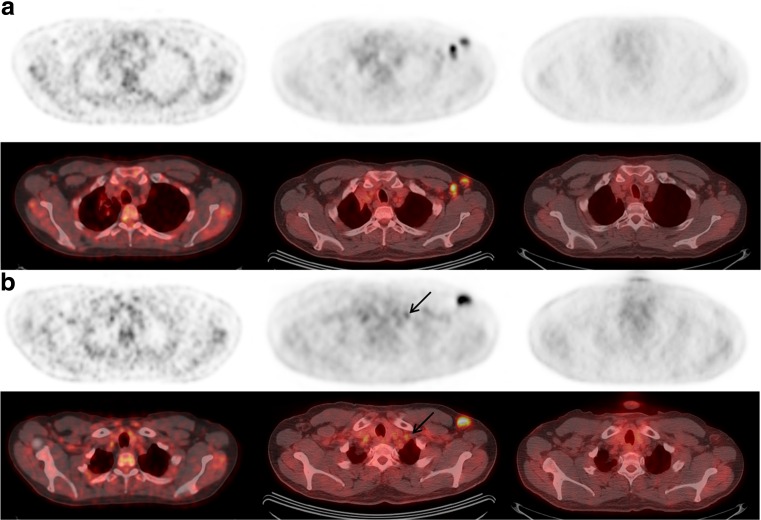
Fig. 2.
Axial PET (a and b, top rows) and fused PET/CT (a and b, bottom rows) images from FDG-PET/CT examinations performed before (left), 2–3 days following (middle), and 12 days following the influenza vaccination (right) administered in the left upper extremity. Compared to the initial scan (left), new enlarged and FDG-avid left axillary lymph nodes (a) were seen on the examination 2–3 days following the influenza vaccination (middle), which resolved 12 days later (right). Several previous reports demonstrated the occurrence of false-positive ipsilateral FDG-avid axillary lymph nodes following vaccination [1–4]. The highest uptake typically occurred within the first 2 weeks after vaccination [1, 3], but persisted beyond 1 month in some cases [2]. Additionally, lymph node size was normal [1–4], in contrast to our case. These reports advocate caution when considering changes to the treatment plan prior to confirmation of the suspected false-positive uptake. FDG uptake can also be seen in lymph nodes ipsilateral to an FDG injection site, especially if tracer is extravasated. In this case, FDG was injected in the left antecubital fossa 2–3 days after vaccination, and in the right hand approximately 2 weeks later. This is a confounding factor in this case; however, the ipsilateral FDG injection alone does not explain the enlarging size of the left axillary lymph nodes, the left supraclavicular lymph node (arrows, b and Fig. 1) and the increased splenic uptake compared to the outside scan before vaccination (left, Fig. 3)
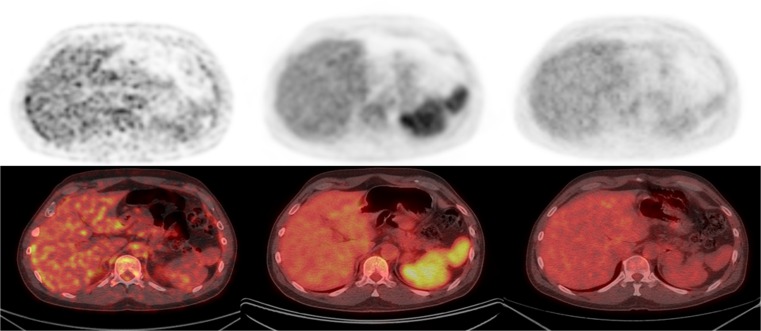
Fig. 3.
Axial FDG-PET (top row) and fused FDG-PET/CT (bottom row) images through the upper abdomen and corresponding to the time-points in Fig. 2 are shown (left before, middle 2–3 days following, and right 12 days following the left upper extremity influenza vaccination). There is diffuse splenic uptake of FDG on the examination 2–3 days following the influenza vaccination with a mean standardized uptake value corrected for lean body mass (SULmean) of 3.1, while that same finding is absent on the examinations prior to (SULmean, 1.3) and 12 days following the vaccination (SULmean, 1.5). Although involvement of metastatic disease is possible, the diffuse pattern and relatively lower level of FDG uptake in the spleen compared with the primary right lung cancer suggests a different etiology. The causes of diffuse FDG uptake in the spleen are varied, and include anemia [5], reactive marrow to tumor [6], recent administration of granulocyte-colony stimulating factors [7–10], and systemic inflammatory or infectious processes, for example human immunodeficiency virus (HIV) disease, sarcoidosis, malaria, hepatitis, and Epstein–Barr virus (EBV) [9, 11, 12]. A diffuse increase in bone marrow uptake of FDG typically accompanies splenic uptake due to recent administration of granulocyte colony stimulating factors [7, 9–11], to a greater extent than what was present in our study (bone marrow SULmean prior to immunization, 1.6; 2–3 days following immunization, 1.8; 12 days following immunization, 1.4). In addition, there are a few cases reports of rare cytokine-producing lung tumors causing increased FDG uptake in bone marrow [13, 14] and cytokine production could also conceivably result in increased uptake in the spleen. Our patient had a normal white blood cell count and grade 1 anemia and thrombocytopenia at the time of the FDG-PET/CT 2–3 days following the vaccine. A limitation of this case is lack of pathologic confirmation; however, this would have required a splenectomy. Subsequent FDG-PET/CT scan 6 months later (not shown) was negative for malignancy in the left axilla and spleen. We believe that the simultaneous increase in metabolism in lymph nodes ipsilateral to the site of vaccine administration and the spleen should be considered in the differential diagnosis in the evaluation of patients with cancer and that a careful history, overall pattern of uptake and time course helped to avoid a false-positive interpretation for progressing lung cancer and alteration of the radiation therapy plan
Compliance with Ethical Standards
Conflict of Interest
Mark Mingos, Stephanie Howard, Nicholas Giacalone, David Kozono and Heather Jacene declare that they have no conflicts of interest.
Ethical Statement
Oral informed consent was obtained from the individual included in this case report.
References
- 1.Panagiotidis E, Exarhos D, Housianakou I, et al. FDG uptake in axillary lymph nodes after vaccination against pandemic (H1N1) Eur Radiol. 2010;20:1251–3. doi: 10.1007/s00330-010-1719-5. [DOI] [PubMed] [Google Scholar]
- 2.Shirone N, Shinkai T, Yamane T, et al. Axillary lymph node accumulation on FDG-PET/CT after influenza vaccination. Ann Nucl Med. 2012;26:248–52. doi: 10.1007/s12149-011-0568-x. [DOI] [PubMed] [Google Scholar]
- 3.Thomassen A, Lerberg Nielsen A, Gerke O, et al. Duration of 18 F-FDG avidity in lymph nodes after pandemic H1N1v and seasonal influenza vaccination. Eur J Nucl Med Mol Imaging. 2011;38:894–8. doi: 10.1007/s00259-011-1729-9. [DOI] [PubMed] [Google Scholar]
- 4.Williams G, Joyce RM, Parker JA. False-positive axillary lymph node on FDG-PET/CT scan resulting from immunization. Clin Nucl Med. 2006;31:731–2. doi: 10.1097/01.rlu.0000242693.69039.70. [DOI] [PubMed] [Google Scholar]
- 5.Nam HY, Kim SJ, Kim IJ, et al. The clinical implication and prediction of diffuse splenic FDG uptake during cancer surveillance. Clin Nucl Med. 2010;35:759–63. doi: 10.1097/RLU.0b013e3181ef0905. [DOI] [PubMed] [Google Scholar]
- 6.Salaun PY, Gastinne T, Bodet-Milin C, et al. Analysis of 18 F-FDG PET diffuse bone marrow uptake and splenic uptake in staging of Hodgkin’s lymphoma: a reflection of disease infiltration or just inflammation? Eur J Nucl Med Mol Imaging. 2009;36:1813–21. doi: 10.1007/s00259-009-1183-0. [DOI] [PubMed] [Google Scholar]
- 7.Basu S, Baghel NS. Intense FDG uptake in the spleen due to recent granulocyte-macrophage colony-stimulating factor administration: follow-up scan clarifying the situation. J Cancer Res Ther. 2011;7:228–9. doi: 10.4103/0973-1482.82933. [DOI] [PubMed] [Google Scholar]
- 8.Jacene HA, Ishimori T, Engles JM, et al. Effects of pegfilgrastim on normal biodistribution of 18 F-FDG: preclinical and clinical studies. J Nucl Med. 2006;47:950–6. [PubMed] [Google Scholar]
- 9.Liu Y. Clinical significance of diffusely increased splenic uptake on FDG-PET. Nucl Med Commun. 2009;30:763–9. doi: 10.1097/MNM.0b013e32832fa254. [DOI] [PubMed] [Google Scholar]
- 10.Sugawara Y, Zasadny KR, Kison PV, et al. Splenic fluorodeoxyglucose uptake increased by granulocyte colony-stimulating factor therapy: PET imaging results. J Nucl Med. 1999;40:1456–62. [PubMed] [Google Scholar]
- 11.Jacene HA, Stearns V, Wahl RL. Lymphadenopathy resulting from acute hepatitis C infection mimicking metastatic breast carcinoma on FDG PET/CT. Clin Nucl Med. 2006;31:379–81. doi: 10.1097/01.rlu.0000222675.10765.14. [DOI] [PubMed] [Google Scholar]
- 12.Thomas DL, Syrbu S, Graham MM. Epstein-Barr virus mimicking lymphoma on FDG-PET/CT. Clin Nucl Med. 2009;34:891–3. doi: 10.1097/RLU.0b013e3181bed135. [DOI] [PubMed] [Google Scholar]
- 13.Balink H, Nabers H, Kibbelaar RE. High F-18 FDG uptake in bone marrow by cytokines secreting ectopic mucoepidermoid carcinoma. Clin Nucl Med. 2009;34:823–4. doi: 10.1097/RLU.0b013e3181b81cbd. [DOI] [PubMed] [Google Scholar]
- 14.Morooka M, Kubota K, Murata Y, et al. (18)F-FDG-PET/CT findings of granulocyte colony stimulating factor (G-CSF)-producing lung tumors. Ann Nucl Med. 2008;22:635–9. doi: 10.1007/s12149-008-0146-z. [DOI] [PubMed] [Google Scholar]