Abstract
Targeting cancer through the use of effector T cells bearing chimeric antigen receptors (CARs) leads to elimination of tumors in animals and patients, but recognition of normal cells or excessive activation can result in significant toxicity and even death. CAR T cells based on modified NKG2D receptors are effective against many types of tumors, and their efficacy is mediated through direct cytotoxicity and cytokine production. Under certain conditions, their ligands can be expressed on non-tumor cells, so a better understanding of the potential off tumor activity of these NKG2D CAR T cells is needed. Injection of very high numbers of activated T cells expressing CARs based on murine NKG2D or DNAM1 resulted in increased serum cytokines (IFNγ, IL-6, MCP-1) and acute toxicity similar to cytokine release syndrome. Acute toxicity required two key effector molecules in CAR T cells – perforin and GM-CSF. Host immune cells also contributed to this toxicity, and mice with severe immune cell defects remained healthy at the highest CAR T cell dose. These data demonstrate that specific CAR T cell effector mechanisms and the host immune system are required for this cytokine release-like syndrome in murine models.
Keywords: CAR T cell, DNAM-1, GM-CSF, cytokine release syndrome, perforin
Introduction
Chimeric antigen receptor (CAR) targeted T cells have recently shown remarkable clinical responses against B cell leukemias (1–6). CARs combine a recognition domain (e.g. scFv) with intracellular signaling domains to create an activating receptor in order to target a large number of T cells against a patient’s tumor. Both direct tumor cell killing and cytokine production are involved in CAR T cell efficacy in immune intact tumor models (7, 8). Several different CAR strategies to target tumors are in various stages of development (9–14). However, CAR T cells also have the potential to cause harm. Tumor lysis syndrome, recognition of ligands on non-tumor cells leading to tissue damage, cross-reactivity with normal proteins by modified CARs, and cytokine release syndrome (CRS) have been documented and can be severe (15–17). Activation of CAR T cells and the production of effector molecules are required for CAR T cell efficacy. A better understanding of mechanisms of toxicity, particularly the drivers of CRS, is vital to improve clinical outcomes and further develop these promising cell therapies.
NK cells recognize and kill a variety of tumor cells using evolutionarily optimized receptors, and several CARs have been developed based on these, including NKG2D and DNAM-1 CARs (18–21). This class of CARs recognizes the natural ligands of these NK cell receptors (NKR). CAR T cells not only kill ligand expressing tumor cells, but they activate innate and adaptive host immunity through CAR T cell production of cytokines. This activation of host myeloid and lymphoid cells is involved in NKG2D CAR T cell efficacy (22–24). Human NKG2D recognizes MICA, and MICB, ULBP1 - 6 on human cells, while murine NKG2D binds to Rae1 proteins, H60 proteins, and MULT1 in mice (25). These ligands are thought to be expressed on the cell surface in low amounts and on few tissues and not at all on most healthy tissues, although they can be induced by acute infection, irradiation, and chemotherapeutic agents through mechanisms involving the ATM/ATR DNA repair pathways (19, 26–30). DNAM1 is a receptor that recognizes PVR and Nectin-2, ligands that are expressed on several normal tissues, including lung epithelium (31, 32). These molecules are often highly upregulated on many tumor types and are involved in NK cell killing of tumors (33–35). Because NKG2D ligands are highly over-expressed on many types of human tumors, they are attractive targets for cancer therapy and a number of CAR and antibody-like approaches are under development to target them (18, 36–39).
Although attractive targets for immunotherapy, the potential of NKG2D ligands to be induced or expressed during immunotherapy resulting in off-tumor on-target toxicity remains unknown. One of the major challenges of immunotherapy is the potential to over-activate the immune system, such as occurs during cytokine release syndrome (CRS). In order to better understand how CAR T cells may activate immune-mediated toxicity, dose-escalation studies using NK receptor-targeting CAR T cells in immune intact animals was performed. This study demonstrates that high dose injection of NKG2D CAR or DNAM1 CAR T cells can result in CRS-like responses in mice that are similar to those seen in many patients given CAR T cells. Further, it elucidates key effector mechanisms from NKR-based CAR T cells that lead to this immune-mediated illness, and how host cells and molecules are involved. These murine models may provide a system to test potential therapies to prevent or limit CRS-like responses. These findings implicate both CAR T cells and host immune cells as required contributors to the development of acute immune-related toxicity.
Methods
Animals
C57BL/6 (B6) mice were purchased from the National Cancer Institute (Frederick, MD) or the Jackson Laboratory. Perforin-deficient mice C57BL/6Prf1tm1Sdz/J (Pfp−/−), interferon gamma deficient mice B6.129S7-Ifngtm1Ts/J (IFNγ −/−), interferon gamma receptor deficient mice B6.129S7-IfngR1tm1Agt/j (IFNγ R −/−), IL-1 receptor deficient mice B6129S7-Il1r1tm1Imx/J (IL-1R −/−), IL-6 deficient mice B6.129S2-Il6tm1Kopf/J (IL-6 −/−), IL-2Rγ chain deficient mice B6129S4-Il2rgtm1Wjl/J (IL-2Rγ −/−), Cd1d1 deficient mice B6(C)-Cd1d1tm1.2Aben/J (CD1 −/−), BALB/cJ, DBA/1J, DBA/2J, A/J, 129S1/SvImJ, and (B6x129)F1 and immune deficient mice B6.129P2(SJL)-MyD88tm1.1Defr/J (MyD88 −/−), B6129S7-Rag1tm1Mom/J (Rag −/−), NOD/ShiLtJ (NOD), NOD.CB17-Prkdcscid/J (NOD-SCID), were obtained from the Jackson Laboratory (Bar Harbor, ME). NOD.Cg-PrkdcscidIl2rgtm1Wji/SzJ (NSG) mice were maintained at the Geisel School of Medicine (Lebanon, NH), NKG2D deficient mice on a B6 background (NKG2D −/−) were provided by Dr. David Raulet (University of California, Berkeley, CA). DR5 deficient mice on a B6 background (DR5 −/−) were provided by Dr. Tak Mak (University of Toronto, Canada). GM-CSF-deficient mice were a C57BL/6/129/FVB mixed background (GM-CSF −/−) and were provided by Dr. Jeff Whitsett (University of Cincinnati, Cincinnati, OH). Mice used in experiments were between 7 to 12 weeks of age. All animal work was performed in the Geisel School of Medicine Animal Facility (Lebanon, NH) in accordance with institutional guidelines.
Cell lines
RMA and RMA-RG cells are B6-derived murine T cell lymphoma cells. RMA-RG cells express Rae-1 and GFP, while parental RMA cells do not. ID8 cells are B6-derived ovarian cancer cells and express Rae1. MC38 is a murine colon cancer cell line and expresses ligands for DNAM1. All cell lines tested negative for mycoplasma by PCR.
Generation of CAR expressing T cells
CAR T cells were generated by viral transduction of mouse splenocytes, as described previously (23, 40). Mouse splenocytes were stimulated with Con A for 18–20 h (0.75 μg/mL, lot 177K700 or 1 μg/mL lot SLBB841V, Sigma), retrovirally transduced with wtNKG2D (that expresses the full-length murine NKG2D protein; wilt-type NKG2D) or chNKG2D (that expresses a full-length NKG2D protein fused to the cytoplasmic portion of CD3zeta; chimeric NKG2D) virus as previously described, and injected into mice 8 d post-activation. Cells were grown in RPMI 1640 (Hyclone) supplemented with 10% heat-inactivated fetal bovine serum (Atlanta Biologicals, Atlanta GA), 100 units/mL of penicillin, 100 μg/mL of streptomycin (Hyclone), 1 mmol/L of pyruvate, 10 mmol/L of Hepes, 0.1 mmol/L of nonessential amino acids (Corning), and 50 μmol/L of 2-mercaptoethanol (Sigma).
Animal studies
RMA-RG tumor cells (105 cells) in 0.4 mL HBSS (Hyclone) were injected i.v. into C57BL/6 (B6) mice on day 0. On day 5, a dose of 0, 5, 10, or 20 × 106 full-length wild-type NKG2D (wtNKG2D) or NKG2D CAR (chNKG2D) T cells in HBSS was injected into tumor bearing or non-tumor bearing mice. In some experiments, one to three doses of 107 wtNKG2D, chNKG2D, DNAM1 CAR (D28z), or mock T cells in 0.4 mL of HBSS or HBSS alone were administered i.v. into tumor bearing or non-tumor bearing mice. For multi-dose experiments, a fresh cell dose was manufactured for each T cell injection. A single dose of 2 × 107, wtNKG2D or chNKG2D T cells derived from B6, 129, (B6x129)F1, or gene-deficient mice in 0.4 mL of HBSS was injected i.v. into mice with different genetic backgrounds or gene deficiencies. B6 mice were injected at the same time, as controls. Mice were euthanized after 18 h. A single dose of 107 DNAM1-based CAR T cells or mock T cells derived from B6, B6x129F1, IFNγ-, GM-CSF-, or perforin- deficient mice were injected into mice i.v. Further, mice were treated with antibodies to deplete specific cell populations, and the extent of cell depletion was confirmed by flow cytometry (data not shown). Mice were weighed prior to T cell injection, and then 2–3 times per week until time of euthanasia. Serum samples were taken and analyzed for cytokines and other analyts, as indicated in the Results.
Health status
The health status of mice was graded on a scale from 1 to 4 as follows: 1 - normal and healthy; 1.5 - some lethargy, walking a bit slowly; 2 - moving slowly, and (in tumor-bearing mice) a slight dragging of a limb; 2.5 – hunched posture, moving slowly, and (in tumor-bearing mice) dragging limbs; 3 - hunched posture with little movement; 3.5 - little movement upon touch; 4 - death.
Depletion of specific cell populations
For NK cell depletion studies, 50 μg of anti-NK1.1 (clone PK136, eBioscience) or control mouse γ-globulin (The Jackson Laboratory) was injected i.p. 2 d before T cell injection. Depletion of NK cells was confirmed by flow cytometry by analysis of splenocytes for CD49b+ CD3− cells. To deplete neutrophils, 500 μg of anti-mLy-6G (clone IA8, BioXCell, Lebanon, NH) or control mouse γ-globulin (Jackson labs) was injected i.p. one day prior to T cell injection. Depletion of PMNs was confirmed by flow cytometric analysis of splenocytes.
Serum analysis
Mouse serum was collected via tail bleeding or cardiac puncture, samples were allowed to coagulate 1 h then spun at 16,400 rcf for 15 min and the serum was frozen at −20 °C. Samples from days 3, 5, and the day of euthanasia were analyzed by multiplex cytokine analysis for G-CSF, IFNγ, IL-1β, IL-6, IL-10, MCP1, MIG, and MIP-1β by DartLab2, and for sAST or sCREA by ACE Alera (Alfa Wasserman, Wilmington, MA).
Histology
Dissected tissues were fixed in 10% formalin. Paraffin sections were generated and stained with hematoxylin and eosin by the Pathology Research Resource at Dartmouth-Hitchcock Medical Center. Histological analysis and scoring was performed in an independent and blinded manner by Charles River Animal Pathology services (Cambridge, MA). Eight tissues were taken for analysis from each mouse: heart, lungs, liver, kidney, large intestine, small intestine, pancreas, and spleen. Tissues were rated as normal or pathology was noted, which was graded 1 (mild), 2 (moderate), or 3 (severe). If insufficient tissue was available for scoring from a particular mouse, this tissue was absent from the analysis but other tissues from the mouse were scored. A summary table to the scoring is provided in supplemental data Tables 3 and 4.
Flow cytometry
Cell phenotyping of transduced primary T cells was determined by staining with specific antibodies: FITC-conjugated anti-CD3ε (clone 145-2C11; eBioscience), APC-conjugated anti-NKG2D (clone CX5; eBioscience), PE-conjugated anti-CD8b (clone CT-CD8b; Biolegend), APC-conjugated anti-CD4 (clone RM4-5; eBioscience), or APC- or PE- conjugated isotype control antibodies (eBioscience). All samples were preincubated with FcR block antibody (anti-mouse CD16/CD32, clone 93; eBioscience) to reduce nonspecific staining. Cells were analyzed using Accuri C6 flow cytometer (BD Biosciences, Ann Arbor, MI).
Cytokine production and cytotoxicity by CAR T cells
WtNKG2D or chNKG2D T cells (105) were cultured with RMA, RMA-RG and ID8 tumor cells at a 1:1 (RMA, RMA-RG) or 1:4 (ID8) ratio (105 T cells) or in media alone. Cell-free conditioned media were collected after 24 h and assayed for IFN-γ using mouse Duoset ELISA kits (R&D Systems). Cytotoxicity was determined by a 4 h 51Chromium (51Cr) release assay, as described (21). Co-culture was performed at effector to target ratios (E:T ratios) of 25:1, 5:1, and 1:1 in triplicate wells.
Statistical analysis
Each experiment was done at least twice with three to five animals per group in each experiment. Data are shown as combined data from the experiments and statistical analysis was done on the complete dataset. Hence, data from six to ten individual animals are shown from a given analysis. A Student’s t-test was used to compare differences between groups using a two-tailed test assuming unequal variance. To compare multiple groups, ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. For analysis of cell cytotoxicity in vitro, a one-way ANOVA with Dunnett’s method for multiple comparisons was used. Any individual mouse that did not receive a full injection of cells was removed from the experiment and further analysis at that time. Values of p<0.05 were considered significant (Prism Software, GraphPad, San Diego, CA).
Results
Determination of the Maximum Tolerated Dose
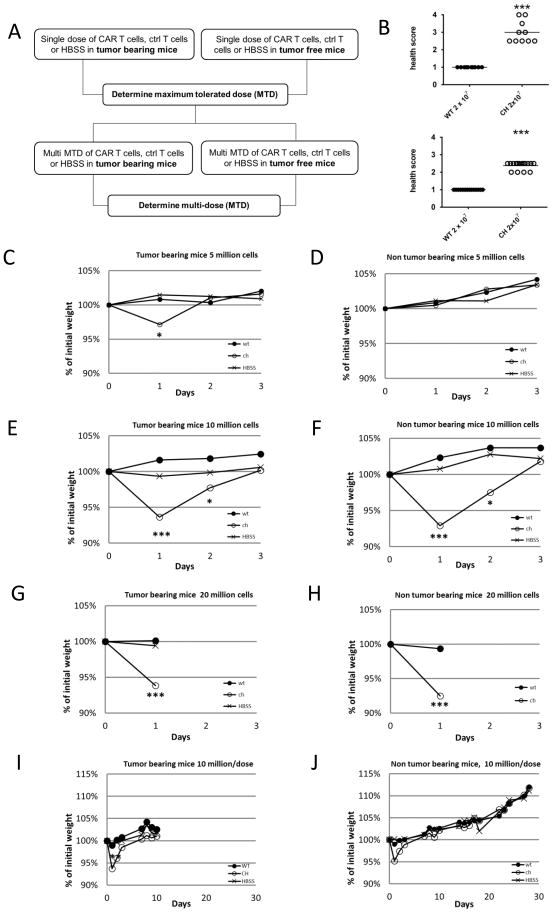
In order to evaluate tumor-dependent, receptor-specific, and non-specific toxicity after injection of NKG2D CAR T cells, dose escalation studies in tumor-bearing and non-tumor bearing mice were conducted (Figure 1A). Based on an effective dose of 5 x 106 CAR T cells from previous studies (7, 41), 5 x 106, 107, or 2 x 107 wtNKG2D T cells, NKG2D CAR T cells, or HBSS were injected into mice i.v. Only mice receiving NKG2D CAR T cells at the highest dose appeared ill. These mice were euthanized between 6 and 20 hours after T cell injection and had an average health status of 2.6 (1 to 4 scale) at the time of euthanasia (Figure 1B). This occurred in both tumor-bearing and non-tumor bearing mice. None of the mice receiving lower doses of NKG2D CAR T cells, any dose of wtNKG2D T cells, or HBSS showed outward signs of toxicity. Compared to control mice, there was a decrease in body weight one day after the injection of 2 x 107 or 107 NKG2D CAR T cells (Figure 1C–H). The average drop in body weight was 7.0% and 6.7% respectively. Although weight loss was typical, it was not observed in every experiment. However, only mice given the highest CAR T cell dose exhibited signs of overt illness. Mice given 107 NKG2D CAR T cells showed no outward signs of illness and began to gain weight on day 2 post-injection. In tumor-bearing mice given 5 x 106 NKG2D CAR T cells, there was a small decrease in body weight (2.6%) after one day which quickly recovered, but there was no change in weight for non-tumor bearing mice given 5 x 106 CAR T cells.
Figure 1. Determination of maximum tolerated dose (MTD) for NKG2D CAR T cells.
(a) overview of approach to determine MTD for single and multi-dose treatment with murine NKG2D CAR T cells. (b) The health score for mice injected with 2 x 107 wild type NKG2D T cells (WT) or NKG2D CAR T cells (CH) in non-tumor bearing (upper) and tumor-bearing (lower) mice is shown. Each symbol represents an individual mouse at the time of euthanasia. (c–j) The percent change in initial weight in the days following injection of NKG2D CAR T cells, wild type NKG2D T cells, or HBSS is plotted for 3 to 28 d after T cell injection. Average values for each group are shown (n=10/group). Mice were treated with a single dose of 5 x106 T cells (c, d), 107 T cells (e, f), or 2 x 107 T cells (g, h). Mice were RMA tumor bearing (c, e, g) or non-tumor bearing (d, f, h). (i) RMA tumor-bearing mice (RMA cells i.v. day -5) were injected with 107 T cells or HBSS on days 0 and 7. (j) Non-tumor bearing mice were injected with 107 T cells or HBSS on days 0, 7 and 14. Data are from two independent experiments (n=10/group). A Student’s t-test was used to compare differences between groups using a two-tailed test assuming unequal variance. An * indicates significant differences compared to WT; * p < 0.05, ** p <0.01, *** p <0.001.
Assessment of toxicity following multi-doses at the MTD
To determine whether multiple injections of CAR T cells would result in toxicity due to accumulation of T cells, tumor-bearing and non-tumor bearing mice were treated with up to three injections of 107 wtNKG2D T cells, 107 NKG2D CAR T cells, or HBSS. No signs of toxicity were observed due to T cell injection over 30 days. Because most of the control tumor-bearing mice had to be euthanized due to tumor growth before the third T cell injection, they only received two T cell doses. We observed a decrease in body weight (5.6%) one day after injection of 107 NKG2D CAR T cells but not in mice given wtNKG2D T cells or HBSS (Figure 1I–J). Notably, this occurred after the first cell injection only. We observed no differential body weight changes after the second or third NKG2D CAR T cell injection compared to controls. Thus, multiple doses of NKG2D CAR T cells were well tolerated.
Analysis of serum analytes
To understand the physiological effects of NKG2D CAR T cell injection, specific serum analytes were measured. RMA-RG tumor cells localize in the liver and kidney, and AST values increased in tumor-bearing mice at later stages of disease. In tumor-bearing mice, the AST values from mice given wtNKG2D T cells or NKG2D CAR T cells were different 3 days after T cell infusion (day 8), but the NKG2D CAR T cell treated and HBSS treated groups had similar AST values. In mice without tumors, the AST values were not affected by T cell treatment. Even when acute illness was observed after the high dose injection of NKG2D CAR T cells, there were no significant differences in AST values compared to control groups. Creatinine values did not change, regardless of T cell injections or tumor growth (Supplementary Table 1). Overall, treatment with NKG2D CAR T cells did not appear to affect kidney or liver function.
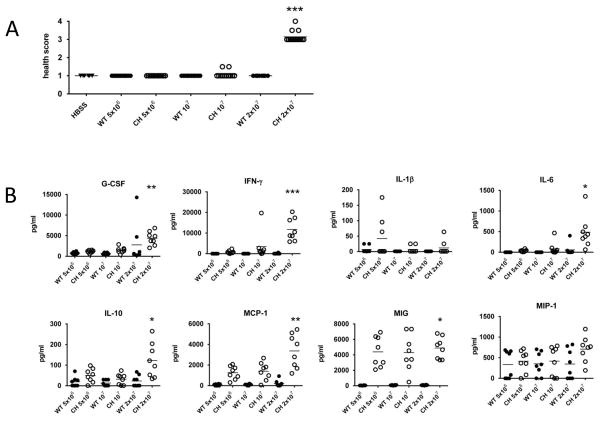
There were no significant differences in serum cytokine amounts (IL-6, IFN-γ, MCP-1, TNF-α) 3, 8, or 12 days post injection of NKG2D CAR T cells compared to controls (Supplementary Table 2). Only in mice injected with 2 x 107 NKG2D CAR T cells were clinical signs of illness observed (mean health score of 3.1, Figure 2A). An analysis of cytokines 20 hours after injection of CAR T cells showed an increase in G-CSF, IL-6, IFN-γ, MCP-1, IL-10, and MIG, with the highest cell dose having significant increases compared to controls (Figure 2B).
Figure 2. Serum cytokines of mice injected with NKG2D CAR T cells.
HBSS, NKG2D CAR T cells (CH) or wtNKG2D T cells (WT) were injected i.v. into mice at 5 x 106, 107, or 2 x 107 cells. (a) Overall health score on day 1 after transfer. (b) Serum samples were analyzed for G-CSF, IFNγ, IL-1β, IL-6, IL-10, MCP1, MIG, and MIP-1β by multiplex cytokine analysis. Each symbol represents an individual mouse (n=6–14/group). ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. An * indicates significant differences compared to WT; * p < 0.05, ** p <0.01, *** p <0.001.
Analysis of histopathology
Despite their health status, mice treated with 2 x 107 NKG2D CAR T cells exhibited little pathology. The liver, pancreas, small intestine, large intestine, heart, and kidney appeared similar to wtNKG2D T cell and HBSS treated mice (see Supplemental Tables 3 and 4). There was no infiltration of leukocytes in these tissues. In the spleen, mild single cell necrosis of lymphocytes in the white pulp of the spleen was evident in about 40% of the mice (11/26) treated with NKG2D CAR T cells from five independent experiments. In tumor-bearing mice, there was evidence of tumor infiltration in the liver and occasionally the kidney, as expected. Lung tissue from both wtNKG2D and NKG2D CAR T cell treated mice had an increased number of lymphocytes as may be anticipated after a large infusion of lymphocytes. There was no increase in cells or debris within the alveoli or airways. The epithelial cells and cells lining the alveoli were intact with no evidence of sloughing or death. In the multi-dose treatment experiments in tumor-bearing mice, mice from all groups showed undifferentiated round cells with atypical nuclear and cytotological features suggestive of neoplasia, and the most frequently affected tissues were liver, kidney, and lung. Splenic involvement or extramedullary hematopoietic activity was noted in a few mice treated with the CAR T cells in tumor-bearing mice. Noted observations in the exocrine pancreas of occasional mice in one multi-dose experiment were considered secondary to debility associated with the presence of neoplastic cells. Two of the CAR T cell injected mice showed neutrophilic infiltration of the alveolar walls in one experiment, and one single mouse from each treatment group over these nine experiments showed alveolar hemorrhage in the lungs, each in different experiments. There was no evidence of lysis of tissues or infiltration of lymphocytes into specific tissues after injection of NKG2D CAR T cells. These findings of high amounts of serum inflammatory cytokines and no obvious tissue damage are consistent with CRS.
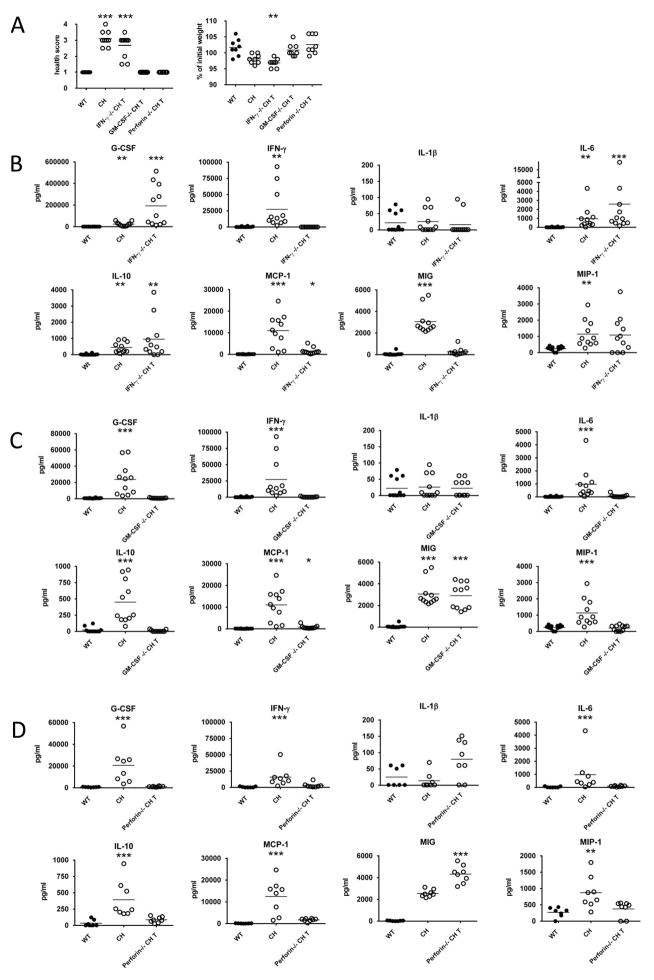
The role of CAR T cell effector mechanisms in acute toxicity
To determine which effector mechanisms of CAR T cells contributed to CRS, 2 x 107 NKG2D CAR T cells derived from mice that were deficient in perforin, IFN-γ, or GM-CSF were injected into mice. These molecules are needed for full efficacy of NKG2D CAR T cells (7, 8). We observed that mice injected with IFN-γ-deficient CAR T cells became acutely ill, similar to mice given B6 CAR T cells. However, when B6 mice were injected with NKG2D CAR T cells derived from GM-CSF- or perforin-deficient mice, there was no sign of illness nor change in body weight (Figure 3A). Analysis of serum cytokines 20 hours post T cell injection showed that inflammatory cytokines (G-CSF, IL-6, IL-10, and MCP-1) were increased in the serum of mice treated with IFN-γ-deficient NKG2D CAR T cells compared to wtNKG2D T cell treated mice. CAR T cells that lacked either perforin or GM-CSF resulted in much lower amounts of cytokines in the serum, which was consistent with their lack of CRS (Figure 3B–D). MIG, which is induced by IFN-γ, was a notable exception and remained elevated.
Figure 3. GM-CSF and perforin are essential for NKG2D CAR T cell induced toxicity.
A single dose of 2 x 107 NKG2D CAR T cells or wild type NKG2D T cells were injected into mice. Changes in health status, body weight (a), and serum cytokines (b–d) were measured after 20 h. The amounts (pg/mL) of G-CSF, IFNγ, IL-1β, IL-6, IL-10, MCP1, MIG, and MIP-1β were measured by multiplex analysis. Serum samples from mice given B6-derived T cells that expressed wild type NKG2D (WT) or the NKG2D CAR (CH) were compared to samples from B6 mice given NKG2D CAR T cells derived from (b) IFNγ-(c) GM-CSF-, or (d) perforin-deficient mice. Each symbol represents an individual mouse. ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. An * indicates significant differences compared to WT; * p < 0.05, ** p <0.01, *** p <0.001.
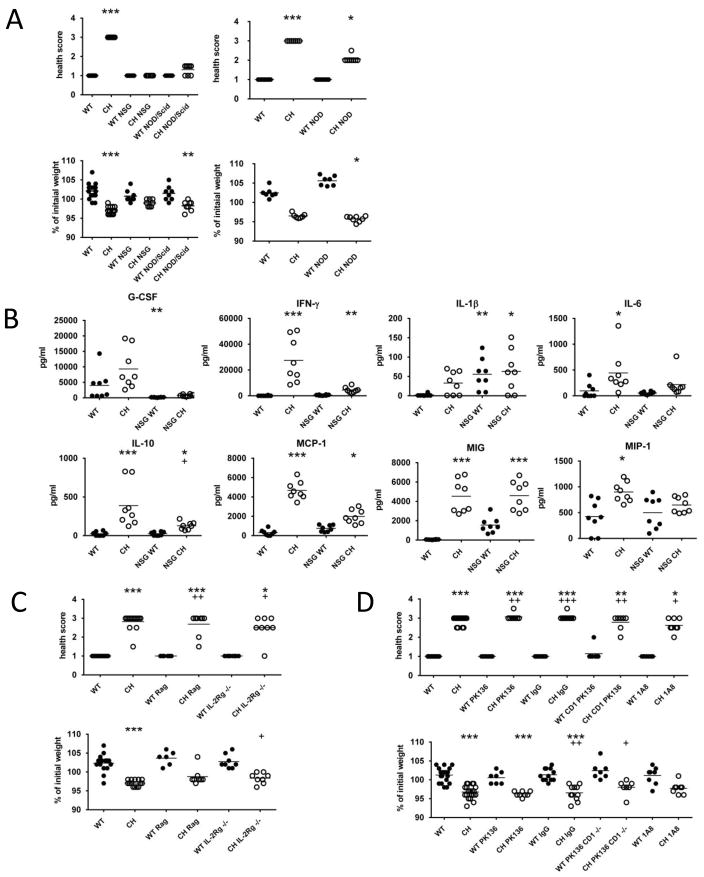
The role of host immune cells
To investigate the role of host immune cells in this process, NOD/SCID/IL-2Rγ-deficient (NSG) mice, NOD/SCID mice, IL-2Rγ-deficient, and Rag-1-deficient mice were injected with a high dose (2 x 107 cells) of either NKG2D CAR T cells or wtNKG2D T cells. The NSG and NOD/SCID mice remained healthy throughout the experiment, while the NOD, Rag-1-deficient, and IL-2Rγ-deficient mice became acutely ill and lost body weight after receiving the high dose of NKG2D CAR T cells similar to B6 mice (Figure 4A–C). In addition to their lack of T cells and B cells, the NSG and NOD/SCID mice also have significant alterations in inflammatory and myeloid cell responses. NK cells and neutrophils can be involved in rapid immune responses in vivo. Treatment of B6 mice with antibodies to deplete NK cells (anti-NK1.1 mAbs) or neutrophils (anti-Ly6G mAbs), prior to injection of a high dose of NKG2D CAR T cells, did not affect the development of CRS (Figure 4D). Taken together, these data indicate that mice that had defective myeloid cells, T cells, and B cells did not develop CRS, but mice with more restricted deficiencies in immune cell populations did develop CRS.
Figure 4. Role of host immunity in NKG2D CAR T cell toxicity.
A single dose of 2 x 107 B6-derived NKG2D CAR T cells (CH) or wild type NKG2D T cells (WT) was injected i.v. into mice and health status and body weight were evaluated after 20 h. (a) Recipients were B6, NSG, NOD/SCID, and NOD mice (n=8/group). (b) At the time of euthanasia, serum samples were isolated and analyzed for G-CSF, IFNγ, IL-1β, IL-6, IL-10, MCP1, MIG, and MIP-1β by multiplex analysis. In other experiments, recipients were (c) Rag1-deficient or IL-2Rγ-deficient mice, (d) B6 mice pretreated with anti-NK1.1 mAbs (PK136), IgG controls, CD1-deficient mice pretreated with anti-NK1.1 mAbs, or anti-Ly6G (1A8). Each symbol represents an individual mouse. ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. An * indicates significant differences compared to B6 WT; * p < 0.05, ** p <0.01, *** p <0.001. A + indicates significant differences compared to the similar deficient or depleted WT; + p < 0.05, ++ p <0.01, +++ p <0.001.
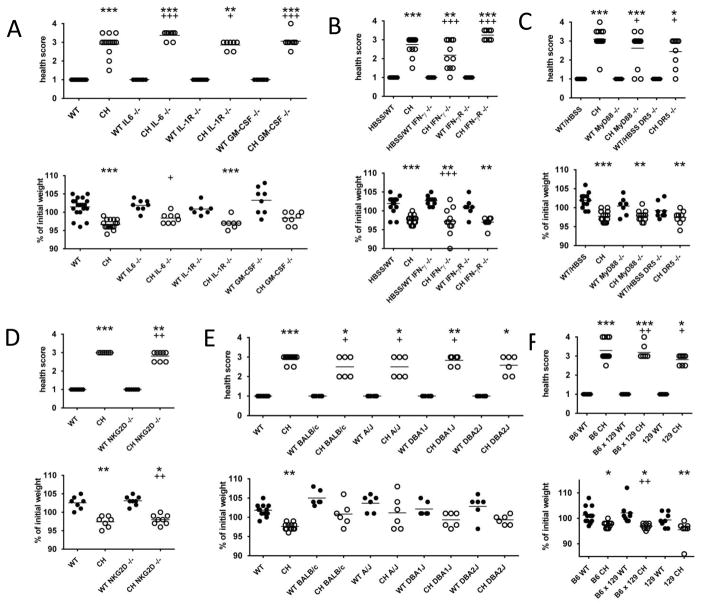
The role of host cytokines
To determine whether specific cytokines shown to be elevated in the serum of NKG2D CAR T cell treated mice were essential for development of CRS, 2 x 107 NKG2D CAR T cells or wtNKG2D T cells were injected into mice deficient in IL-1R, IL-6, GM-CSF, IFN-γ, or IFN-γR. All mice treated with the high dose of NKG2D CAR T cells lost weight and became acutely ill similar to B6 mice (Figure 5A–B). While IL-1 and IL-6 are involved in the acute inflammatory response, the data indicate that the host’s ability to respond to IL-1 or produce IL-6 was irrelevant to the outcome. GM-CSF from the CAR T cells was essential for induction of the CRS-like response, but the host did not need to produce GM-CSF for illness to occur. This suggests that GM-CSF is essential early in the induction of acute inflammation but host production was not required. CAR T cells produce a significant IFN-γ response and this is key for anti-tumor immunity, yet neither the production of IFN-γ nor the response to the IFN-γ present by the host were necessary for CRS-like illness. Similarly, hosts deficient in NKG2D, DR5 (TRAIL receptor), or MyD88 also developed CRS after injection of a high dose of NKG2D CAR T cells (Figure 5C–D). While the host’s endogenous NKG2D+ cells might contribute to the acute inflammatory response, the absence of host NKG2D did not alter the extent of the illness. MyD88 is a key signaling molecule in responses of Toll-like receptors that leads to production of proinflammatory cytokines, such as TNF-α and IL-12 (42). However, the absence of MyD88 did not affect the development of the CRS-like illness, indicating that this signaling pathway was not essential in the acute illness observed.
Figure 5. Role of host cytokines and background in NKG2D CAR T cell toxicity.
A single dose of 2 x 107 B6-derived NKG2D CAR T cells (CH) or wild type NKG2D T cells (WT) was injected i.v. into mice and health status and body weight were evaluated after 20 h. Recipients were (a) IL-6-deficient, IL-1R-deficient or GM-CSF-deficient mice, (b) IFNγ-deficient or IFNγR-deficient mice, (c) MyD88-deficient or DR5-deficient mice, (d) NKG2D-deficient mice, (e) BALB/c, A/J, DBA/1, or DBA/2 mice, (f) B6 mice injected with CAR or control T cells derived from B6, 129 or (B6x129) F1 mice. Each symbol represents an individual mouse. ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. An * indicates significant differences compared to B6 WT; * p < 0.05, ** p <0.01, *** p <0.001. A + indicates significant differences compared to the similar deficient or depleted WT; + p < 0.05, ++ p <0.01, +++ p <0.001.
The role of genetic background
Because NOD/SCID and NSG mice have a different genetic background than B6 mice, we tested whether NKG2D CAR T cells would result in CRS in other mouse strains. Injection of 2 x 107 NKG2D CAR T cells derived from B6 mice resulted in a CRS response in BALB/c, A/J, DBA1, and DBA2 recipients (Figure 5E). DBA/1 and A/J mice have a defect in C5 component of the complement cascade, which when activated produces a powerful anaphylatoxin and is necessary for the generation of the membrane attack complex. However, there was no difference in the observed response in DBA/1 or A/J mice compared to the other mouse strains tested. When the NKG2D CAR was expressed in 129/Sv or (B6 x 129)F1 T cells and injected at a high dose into B6 recipient mice, the mice all exhibited a CRS similar to when B6 T cells were used as a source of NKG2D CAR T cells (Figure 5F). Thus, there were no differences in the CRS response when an allogeneic or F1 combination was used.
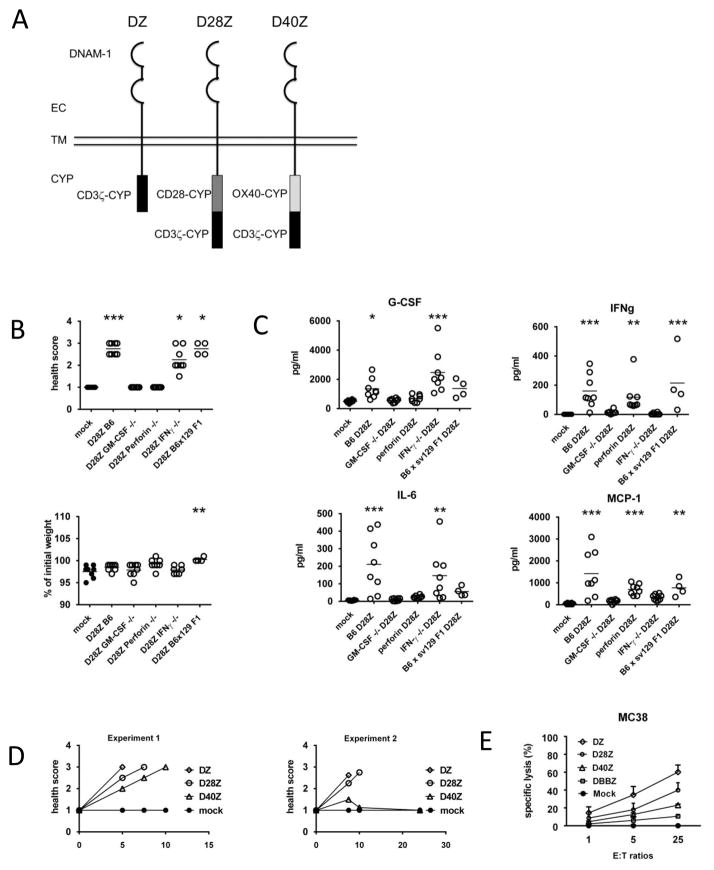
DNAM1 based CARs show similar acute CRS toxicity
To test whether these observations were limited to NKG2D CARs, we also tested CARs based on the NK cell receptor DNAM1 (Figure 6A) (21). DNAM1 CAR T cells lyse PVR and Nectin-2 expressing tumor cells in vitro and reduce the growth of B16F10 melanoma cells in vivo (21). To test whether similar effector mechanisms were essential for the induction of CRS after injection of DNAM1 CAR T cells, perforin-, GM-CSF-, or IFN-γ-deficient DNAM1-CD28-CD3z (D28Z) T cells or intact DNAM1 CAR T cells were injected into mice. Similar to NKG2D CAR T cells, D28Z T cells derived from mice deficient in either perforin or GM-CSF did not cause CRS (Figure 6B). However mice injected with 107 D28Z T cells from B6, B6x129F1, or IFN-γ-deficient T cells showed signs of CRS with an average health score of 2.5 to 2.8. Furthermore, the mice that showed signs of CRS had elevated serum inflammatory cytokines (Figure 6C). Thus, perforin and GM-CSF were essential effector molecules of both NKG2D and DNAM1 CAR T cells for the induction of CRS. DNAM1 CARs that included CD3z, CD28, or OX40 cytoplasmic domains induced CRS in B6 mice when injected at 107 T cells i.v. The time to development of CRS showed a trend with the CAR T cells that had greater cytotoxicity in vitro against MC38 tumor cells inducing a more rapid CRS-like illness in vivo (Figure 6D–E).
Figure 6. Mechanisms of DNAM1 CAR mediated toxicity.
A single dose of 107 DNAM1 based CAR T cells were injected into B6 mice and health status and body weight were evaluated. (a) The CARs used were constructed using the entire murine DNAM1 protein combined with cytoplasmic portions of CD3z (DZ), CD28 and CD3z (D28Z), or OX40 and CD3z (D40Z). (b) Health status and body weight of B6 mice after a single injection of HBSS or 107 D28Z CAR T cells derived from B6, (B6x129)F1, or GM-CSF-, perforin-, or IFNγ-deficient mice. All groups had 8 mice, except the (B6x129)F1 that had 4 mice. All mice in groups treated with HBSS, or GM-CSF- or perforin-deficient T cells had a health score of 1. (c) At the time of euthanasia, serum samples were isolated and analyzed for G-CSF, IFNγ, IL-6, and MCP1 by multiplex analysis. (d) Health status at different times after CAR T cells derived from B6 mice or HBSS injections from two independent experiments (experiment 1, experiment 2). (e) Specific lysis of MC38 tumor cells at various effector:target (E:T) ratios by T cells expressing a DNAM1 CAR – DZ, D28Z, D40Z, DBBZ (DNAM1 protein with cytoplasmic domains from 4-1BB and CD3z), or mock T cells. Error bars are SD. ANOVA was performed using a nonparametric Kruskal-Wallis test with Dunn’s test for multiple comparisons. For analysis of cell cytotoxicity in vitro (6e), a one way ANOVA with Dunnett’s method for multiple comparisons was used. An * indicates significant differences compared to WT; * p < 0.05, ** p <0.01, *** p <0.001.
Discussion
These studies in an immune intact murine model using murine CAR T cells provide the opportunity to dissect critical components of CRS and particularly components of the host immune system which cannot be interrogated in xenograft models of human CAR T cells. These data show that a high dose of CAR T cells can induce CRS in immune intact mice. CRS was dependent upon cell dose, specific CAR T cell effector mechanisms, and host immune cells (Table 1). Mice showed an acute inflammatory distress syndrome associated with production of pro-inflammatory cytokines. There was little significant histological damage in any of the eight organs examined, although some NKG2D CAR T cell treated mice had single cell necrosis in the splenic white pulp. There was no accumulation of T cells in any organ other than lung, and this occurred in mice given either wtNKG2D or NKG2D CAR T cells indicating that this was not associated with toxicity and likely reflected a first pass effect of i.v. injection of a large number of T cells. At lower doses of NKG2D CAR T cells, there was a drop in body weight, but only at the first dose, and without any clinical phenotype; mice quickly recovered. Thus, toxicity was associated with a single high-dose injection of CAR cells rather than the cumulative dose of cells, and likely involves CAR recognition of ligands. Whether these ligands are present due to endogenous expression, are induced upon an injection of a large dose of activated T cells, or due to interaction of the CAR T cells with each other is unknown. These data indicate that NKR based CAR T cells may lead to acute toxicities associated with proinflammatory cytokine production consistent with CRS, and also in conjunction with prior studies, they confirm that lower T cell doses and/or the use of repeated doses leads to favorable anti-tumor effects without toxicity.
Table 1.
Summary of CAR T cell injection experiments
| Source of CAR T cells | Host strain/treatment* | Immune status/deficiency | Outcome |
|---|---|---|---|
| B6 | B6 | none | illness |
| IFN-γ−/− | B6 | IFN-γ from CAR T cells | illness |
| GM-CSF−/− | B6 | GM-CSF from CAR T cells | healthy |
| Perforin−/− | B6 | Perforin killing via CAR T cells | healthy |
| B6 | MyD88−/− | host TLR signaling pathways | illness |
| B6 | IL-6−/− | host IL-6 production | illness |
| B6 | IL-1R−/− | host responses to IL-1 | illness |
| B6 | IFN-γ−/− | host IFN-γ production | illness |
| B6 | IFN-γ−/− | host responses to IFN-γ | illness |
| B6 | GM-CSF−/− | host GM-CSF production | illness |
| B6 | DR5 | host TRAIL receptor | illness |
| B6 | anti-NK† | Depletion of host NK cells | illness |
| B6 | anti-PMN‡ | Depletion of host PMNs | illness |
| B6 | RAG-1−/− | host T and B cells | illness |
| B6 | anti-NK in CD1−/− | Depletion of host NK & NKT cells | illness |
| B6 | NSG§ | host T, B, NK cells and myeloid cell defects | healthy |
| B6 | NOD/SCID | host T, B, and myeloid cell defects | mild illness |
| B6 | NOD | allogeneic, C5 deficiency | illness |
| B6 | DBA/1 | allogeneic, C5 deficiency | illness |
| B6 | DBA/2 | allogeneic | illness |
| B6 | BALB/c | allogeneic | illness |
| B6 | A/J | allogeneic, C5 deficiency | illness |
| 129 | B6 | minor allogeneic | illness |
| (129xB6) F1 | B6 | minor allogeneic | illness |
All mice were given 2 x 107 T cells i.v.
anti-NK1.1 mAbs
anti-1A8 mAbs
NOD/SCID/γ-chain deficient mice
Our previous studies have shown that NKG2D CAR T cells require IFN-γ, GM-CSF, and cytotoxicity for complete efficacy in lymphoma and ovarian cancer tumor models, although partial efficacy was observed in the absence of GM-CSF or perforin (7, 8). Even if one of these molecules is absent, the other cytokines and/or cytotoxicity pathways remain intact and active. IFN-γ from NKG2D CAR T cells has been shown to activate local macrophages, induce antigen presentation and NO production from macrophages, and there was a reduction in a large number of cytokines in the ovarian cancer tumor microenvironment when the CAR T cells were IFN-γ deficient (43). CAR T cells that lack either perforin or GM-CSF did not result in acute toxicity when injected at high cell doses, although CAR T cells derived from these mice have anti-tumor activity in vivo in lymphoma and ovarian cancer tumor models. Mice treated with DNAM1 based CAR T cells i.v. exhibited similar acute symptoms that was again dependent upon perforin and GM-CSF. The manner in which these molecules drive CRS-like illness remains to be elucidated in future studies. GM-CSF from NKG2D CAR T cells drives monocyte recruitment via induction of CCR2, antigen processing, and IL-12 production (24). GM-CSF is known to activate a variety of myeloid cell activities, including the production of cytokines (44). The absence of perforin in CAR T cells does not reduce the cytokines produced or present in the TME to a large degree (43). The observation that the absence of the perforin cytotoxic pathway in CAR T cells prevented the CRS-like illness suggests that CAR T cell-mediated death of ligand-expressing cells and the inflammation and macrophage activation induced by the cell debris may be a key component that drives this acute clinical illness. Cell debris may drive non-infectious inflammation and wound healing responses, but the illness observed in this study was not dependent on the MyD-88/TLR dependent signaling pathway. Moreover, these data indicate that the efficacy of CAR T cells can be detached from their ability to cause CRS-like illness. For example, IFN-γ is dispensable for the acute toxicity observed, but it is required for anti-tumor efficacy. Whereas partial efficacy was observed after only one dose of CAR T cells in the absence of GM-CSF or perforin, yet no acute toxicity was seen when either of these effector molecules was absent (7, 8). Our findings are consistent with a recent study showing that NKG2D CAR T cells did not cause significant toxicity when injected at 107 CAR T cells i.v. into B6 or BALB/c mice. The addition of further costimulation domains to an NKG2D CAR from CD28 resulted in increased toxicity, especially if the CAR T cells were injected following cyclophosphamide preconditioning (45). These findings suggest that methods to “improve” NKG2D CAR design with stronger signaling or the use of immune preconditioning should be considered carefully.
Data from patients treated with CAR T cells have shown similar patterns of elevated serum cytokines that is believed to be triggered by recognition of target antigens (2, 15, 46, 47). In these clinical studies, a set of cytokines has been elevated 75-fold or more above baseline. This set included IFN-γ, IL-6, CXCL9, CXCL10, MCP-1, IL-10, G-CSF, and GM-CSF. The development of CRS and elevation in serum cytokines was associated with the extent of expansion of anti-CD19 CAR T cells in vivo and the extent of tumor burden. However, development of severe CRS is not required for therapeutic success. Both high dose steroids and anti-IL-6R antibodies have successfully mitigated CRS in the clinic (48, 49). However, the mechanisms of CRS and required elements of immune activation have not been clearly dissected. Advances in the understanding of CRS will be critical to optimize the use of CAR T cells in patients.
The use of genetic mouse models (which lack one or several key molecule or cell types) and the use of cell-depleting antibodies, allowed the evaluation of the host immune cells and effector molecules essential for CRS-like illness observed after injection of NKG2D CAR T cells. The data demonstrated that many cells and molecules known to contribute to inflammation under different conditions, including B cells, T cells, NK cells, IL-6, and IFN-γ, were not required for toxicity. That a particular gene knockout or cell depletion did not lead to an altered phenotype does not indicate that the gene or cell plays no role in the acute CRS-like illness, only that the gene or cell is not a critical component. In contrast, mice of the NOD/SCID background, including NSG mice, developed none or at most a mild illness due to the severe immune deficiency associated with NOD/SCID mice. Not only do NOD/SCID and NSG mice lack T cells and B cells, they also have a number of other immune deficiencies, such as decreased NK cells, altered PMNs, more immature macrophages, reduced macrophage activation, and altered lymphoid tissue architecture. This severe immune deficiency is in contrast to Rag1-deficient mice that only lack T and B cells, or IL-2Rγ-deficient mice that have no NK cells and defects in T and B cell numbers and responses. Thus, a defect in multiple immune cell populations in the host, including the monocyte/macrophage compartment, protected against the development of the CRS-like illness, and this is consistent with a clinical phenotype that resembles Macrophage Activation Syndrome. This is an important observation because severely immunodeficient NSG mice are often used to evaluate and optimize CAR T cells in vivo. However, toxicity associated with CAR T cell treatment may not be observed in these mice. There are notable human cytokines that do not function in mice. One of these cytokines is GM-CSF, so GM-CSF from human CAR T cells will not affect mouse immune responses. The data from this study showed that acute illness was independent of genetic background in the strains tested. The sum of data suggest that host myeloid cells and innate cells are key players in this CRS-like illness that we observe at high doses of CAR T cells. Overall, the data show that murine NKG2D CAR T cells can result in an acute CRS-like phenotype, the bolus dose is more important than cumulative cell dose for CRS development, and that specific effector mechanisms from the CAR T cells and host are involved.
Supplementary Material
Acknowledgments
The authors thank the DHMC Pathology department for assistance with analyte measurement and organ histology, the National Cancer Institute Biological Resource Branch for providing recombinant human IL-2, and the staff of the Center for Comparative Medicine and Research in Dartmouth College for providing animal care. The authors also wish to thank DartLab: Immunoassay and Flow Cytometry Shared Resource at the Geisel School of Medicine at Dartmouth.
Footnotes
Research support: R44 HL099217 and funds from Dartmouth’s Center for Synthetic Immunity.
DartLab is a shared resource and is supported by 5 P30 CA023108-36 from the National Cancer Institute and 8 P30 GM103415-14 from the National Institute of General Medical Sciences.
References
- 1.Brentjens RJ, Davila ML, Riviere I, Park J, Wang X, Cowell LG, Bartido S, Stefanski J, Taylor C, Olszewska M, Borquez-Ojeda O, Qu J, Wasielewska T, He Q, Bernal Y, Rijo IV, Hedvat C, Kobos R, Curran K, Steinherz P, Jurcic J, Rosenblat T, Maslak P, Frattini M, Sadelain M. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci Transl Med. 2013;5:177ra138. doi: 10.1126/scitranslmed.3005930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalos M, Levine BL, Porter DL, Katz S, Grupp SA, Bagg A, June CH. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med. 2011;3:95ra73. doi: 10.1126/scitranslmed.3002842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grupp SA, Kalos M, Barrett D, Aplenc R, Porter DL, Rheingold SR, Teachey DT, Chew A, Hauck B, Wright JF, Milone MC, Levine BL, June CH. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–1518. doi: 10.1056/NEJMoa1215134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, Chew A, Gonzalez VE, Zheng Z, Lacey SF, Mahnke YD, Melenhorst JJ, Rheingold SR, Shen A, Teachey DT, Levine BL, June CH, Porter DL, Grupp SA. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371:1507–1517. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee DW, Kochenderfer JN, Stetler-Stevenson M, Cui YK, Delbrook C, Feldman SA, Fry TJ, Orentas R, Sabatino M, Shah NN, Steinberg SM, Stroncek D, Tschernia N, Yuan C, Zhang H, Zhang L, Rosenberg SA, Wayne AS, Mackall CL. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385:517–528. doi: 10.1016/S0140-6736(14)61403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kochenderfer JN, Dudley ME, Kassim SH, Somerville RP, Carpenter RO, Stetler-Stevenson M, Yang JC, Phan GQ, Hughes MS, Sherry RM, Raffeld M, Feldman S, Lu L, Li YF, Ngo LT, Goy A, Feldman T, Spaner DE, Wang ML, Chen CC, Kranick SM, Nath A, Nathan DA, Morton KE, Toomey MA, Rosenberg SA. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33:540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang T, Barber A, Sentman CL. Chimeric NKG2D modified T cells inhibit systemic T-cell lymphoma growth in a manner involving multiple cytokines and cytotoxic pathways. Cancer Res. 2007;67:11029–11036. doi: 10.1158/0008-5472.CAN-07-2251. [DOI] [PubMed] [Google Scholar]
- 8.Barber A, Zhang T, Sentman CL. Immunotherapy with chimeric NKG2D receptors leads to long-term tumor-free survival and development of host antitumor immunity in murine ovarian cancer. J Immunol. 2008;180:72–78. doi: 10.4049/jimmunol.180.1.72. [DOI] [PubMed] [Google Scholar]
- 9.Sadelain M, Brentjens R, Riviere I. The basic principles of chimeric antigen receptor design. Cancer Discov. 2013;3:388–398. doi: 10.1158/2159-8290.CD-12-0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maus MV, Grupp SA, Porter DL, June CH. Antibody-modified T cells: CARs take the front seat for hematologic malignancies. Blood. 2014;123:2625–2635. doi: 10.1182/blood-2013-11-492231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klebanoff CA, Rosenberg SA, Restifo NP. Prospects for gene-engineered T cell immunotherapy for solid cancers. Nat Med. 2016;22:26–36. doi: 10.1038/nm.4015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu X, Ranganathan R, Jiang S, Fang C, Sun J, Kim S, Newick K, Lo A, June CH, Zhao Y, Moon EK. A Chimeric Switch-Receptor Targeting PD1 Augments the Efficacy of Second-Generation CAR T Cells in Advanced Solid Tumors. Cancer Res. 2016;76:1578–1590. doi: 10.1158/0008-5472.CAN-15-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown CE, Badie B, Barish ME, Weng L, Ostberg JR, Chang WC, Naranjo A, Starr R, Wagner J, Wright C, Zhai Y, Bading JR, Ressler JA, Portnow J, D’Apuzzo M, Forman SJ, Jensen MC. Bioactivity and Safety of IL13Ralpha2-Redirected Chimeric Antigen Receptor CD8+ T Cells in Patients with Recurrent Glioblastoma. Clin Cancer Res. 2015;21:4062–4072. doi: 10.1158/1078-0432.CCR-15-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geldres C, Savoldo B, Dotti G. Chimeric antigen receptor-redirected T cells return to the bench. Semin Immunol. 2016 doi: 10.1016/j.smim.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linette GP, Stadtmauer EA, Maus MV, Rapoport AP, Levine BL, Emery L, Litzky L, Bagg A, Carreno BM, Cimino PJ, Binder-Scholl GK, Smethurst DP, Gerry AB, Pumphrey NJ, Bennett AD, Brewer JE, Dukes J, Harper J, Tayton-Martin HK, Jakobsen BK, Hassan NJ, Kalos M, June CH. Cardiovascular toxicity and titin cross-reactivity of affinity-enhanced T cells in myeloma and melanoma. Blood. 2013;122:863–871. doi: 10.1182/blood-2013-03-490565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgan RA, Yang JC, Kitano M, Dudley ME, Laurencot CM, Rosenberg SA. Case Report of a Serious Adverse Event Following the Administration of T Cells Transduced With a Chimeric Antigen Receptor Recognizing ERBB2. Molecular Therapy. 2010;18:843–851. doi: 10.1038/mt.2010.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan RA, Chinnasamy N, Abate-Daga D, Gros A, Robbins PF, Zheng Z, Dudley ME, Feldman SA, Yang JC, Sherry RM, Phan GQ, Hughes MS, Kammula US, Miller AD, Hessman CJ, Stewart AA, Restifo NP, Quezado MM, Alimchandani M, Rosenberg AZ, Nath A, Wang T, Bielekova B, Wuest SC, Akula N, McMahon FJ, Wilde S, Mosetter B, Schendel DJ, Laurencot CM, Rosenberg SA. Cancer regression and neurological toxicity following anti-MAGE-A3 TCR gene therapy. J Immunother. 2013;36:133–151. doi: 10.1097/CJI.0b013e3182829903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sentman CL, Meehan KR. NKG2D CARs as cell therapy for cancer. Cancer J. 2014;20:156–159. doi: 10.1097/PPO.0000000000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spear P, Wu MR, Sentman ML, Sentman CL. NKG2D ligands as therapeutic targets. Cancer Immun. 2013;13:8. [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang T, Wu MR, Sentman CL. An NKp30-Based Chimeric Antigen Receptor Promotes T Cell Effector Functions and Antitumor Efficacy In Vivo. J Immunol. 2012;189:2290–2299. doi: 10.4049/jimmunol.1103495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu MR, Zhang T, Alcon A, Sentman CL. DNAM-1-based chimeric antigen receptors enhance T cell effector function and exhibit in vivo efficacy against melanoma. Cancer Immunol Immunother. 2015;64:409–418. doi: 10.1007/s00262-014-1648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barber A, Sentman CL. Chimeric NKG2D T cells require both T cell- and host-derived cytokine secretion and perforin expression to increase tumor antigen presentation and systemic immunity. J Immunol. 2009;183:2365–2372. doi: 10.4049/jimmunol.0900721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spear P, Barber A, SCL Collaboration of chimeric antigen receptor (CAR) and host T cells for optimal elimination of established ovarian tumors. Oncoimmunology. 2013:2. doi: 10.4161/onci.23564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spear P, Barber A, Rynda-Apple A, Sentman CL. Chimeric Antigen Receptor T Cells Shape Myeloid Cell Function within the Tumor Microenvironment through IFN-gamma and GM-CSF. J Immunol. 2012;188:6389–6398. doi: 10.4049/jimmunol.1103019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carapito R, Bahram S. Genetics, genomics, and evolutionary biology of NKG2D ligands. Immunol Rev. 2015;267:88–116. doi: 10.1111/imr.12328. [DOI] [PubMed] [Google Scholar]
- 26.Gasser S, Orsulic S, Brown EJ, Raulet DH. The DNA damage pathway regulates innate immune system ligands of the NKG2D receptor. Nature. 2005;436:1186–1190. doi: 10.1038/nature03884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borchers MT, Harris NL, Wesselkamper SC, Zhang S, Chen Y, Young L, Lau GW. The NKG2D-activating receptor mediates pulmonary clearance of Pseudomonas aeruginosa. Infect Immun. 2006;74:2578–2586. doi: 10.1128/IAI.74.5.2578-2586.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruocco MG, Pilones KA, Kawashima N, Cammer M, Huang J, Babb JS, Liu M, Formenti SC, Dustin ML, Demaria S. Suppressing T cell motility induced by anti-CTLA-4 monotherapy improves antitumor effects. J Clin Invest. 2012;122:3718–3730. doi: 10.1172/JCI61931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vales-Gomez M, Chisholm SE, Cassady-Cain RL, Roda-Navarro P, Reyburn HT. Selective induction of expression of a ligand for the NKG2D receptor by proteasome inhibitors. Cancer Res. 2008;68:1546–1554. doi: 10.1158/0008-5472.CAN-07-2973. [DOI] [PubMed] [Google Scholar]
- 30.Skov S, Pedersen MT, Andresen L, Straten PT, Woetmann A, Odum N. Cancer cells become susceptible to natural killer cell killing after exposure to histone deacetylase inhibitors due to glycogen synthase kinase-3-dependent expression of MHC class I-related chain A and B. Cancer Res. 2005;65:11136–11145. doi: 10.1158/0008-5472.CAN-05-0599. [DOI] [PubMed] [Google Scholar]
- 31.Bottino C, Castriconi R, Pende D, Rivera P, Nanni M, Carnemolla B, Cantoni C, Grassi J, Marcenaro S, Reymond N, Vitale M, Moretta L, Lopez M, Moretta A. Identification of PVR (CD155) and Nectin-2 (CD112) as cell surface ligands for the human DNAM-1 (CD226) activating molecule. J Exp Med. 2003;198:557–567. doi: 10.1084/jem.20030788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tahara-Hanaoka S, Shibuya K, Onoda Y, Zhang H, Yamazaki S, Miyamoto A, Honda S, Lanier LL, Shibuya A. Functional characterization of DNAM-1 (CD226) interaction with its ligands PVR (CD155) and nectin-2 (PRR-2/CD112) Int Immunol. 2004;16:533–538. doi: 10.1093/intimm/dxh059. [DOI] [PubMed] [Google Scholar]
- 33.Verhoeven DHJ, de Hooge ASK, Mooiman ECK, Santos SJ, ten Dam MM, Gelderblom H, Melief CJM, Hogendoorn PCW, Egeler RM, van Tol MJD, Schilham MW, Lankester AC. NK cells recognize and lyse Ewing sarcoma cells through NKG2D and DNAM-1 receptor dependent pathways. Molecular Immunology. 2008;45:3917–3925. doi: 10.1016/j.molimm.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 34.Castriconi R, Dondero A, Corrias MV, Lanino E, Pende D, Moretta L, Bottino C, Moretta A. Natural killer cell-mediated killing of freshly isolated neuroblastoma cells: critical role of DNAX accessory molecule-1-poliovirus receptor interaction. Cancer Res. 2004;64:9180–9184. doi: 10.1158/0008-5472.CAN-04-2682. [DOI] [PubMed] [Google Scholar]
- 35.Cho D, Shook DR, Shimasaki N, Chang YH, Fujisaki H, Campana D. Cytotoxicity of activated natural killer cells against pediatric solid tumors. Clin Cancer Res. 2010;16:3901–3909. doi: 10.1158/1078-0432.CCR-10-0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang T, Sentman CL. Cancer immunotherapy using a bi-specific NK receptor- fusion protein that engages both T cells and tumor cells. Cancer Research. 2011;71:2066–2076. doi: 10.1158/0008-5472.CAN-10-3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pogge von Strandmann E, Hansen HP, Reiners KS, Schnell R, Borchmann P, Merkert S, Simhadri VR, Draube A, Reiser M, Purr I, Hallek M, Engert A. A novel bispecific protein (ULBP2-BB4) targeting the NKG2D receptor on natural killer (NK) cells and CD138 activates NK cells and has potent antitumor activity against human multiple myeloma in vitro and in vivo. Blood. 2005 doi: 10.1182/blood-2005-05-2177. [DOI] [PubMed] [Google Scholar]
- 38.Steinbacher J, Baltz-Ghahremanpour K, Schmiedel BJ, Steinle A, Jung G, Kubler A, Andre MC, Grosse-Hovest L, Salih HR. An Fc-optimized NKG2D-immunoglobulin G fusion protein for induction of natural killer cell reactivity against leukemia. Int J Cancer. 2015;136:1073–1084. doi: 10.1002/ijc.29083. [DOI] [PubMed] [Google Scholar]
- 39.Rothe A, Jachimowicz RD, Borchmann S, Madlener M, Kessler J, Reiners KS, Sauer M, Hansen HP, Ullrich RT, Chatterjee S, Borchmann P, Yazaki P, Koslowsky TC, Engert A, Heukamp LC, Hallek M, von Strandmann EP. The bispecific immunoligand ULBP2-aCEA redirects natural killer cells to tumor cells and reveals potent anti-tumor activity against colon carcinoma. Int J Cancer. 2014;134:2829–2840. doi: 10.1002/ijc.28609. [DOI] [PubMed] [Google Scholar]
- 40.Zhang T, Lemoi BA, Sentman CL. Chimeric NK-receptor-bearing T cells mediate antitumor immunotherapy. Blood. 2005;106:1544–1551. doi: 10.1182/blood-2004-11-4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barber A, Meehan KR, Sentman CL. Treatment of multiple myeloma with adoptively transferred chimeric NKG2D receptor-expressing T cells. Gene Ther. 2011;18:509–516. doi: 10.1038/gt.2010.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004;4:499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 43.Barber A, Rynda A, Sentman CL. Chimeric NKG2D expressing T cells eliminate immunosuppression and activate immunity within the ovarian tumor microenvironment. J Immunol. 2009;183:6939–6947. doi: 10.4049/jimmunol.0902000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van Nieuwenhuijze A, Koenders M, Roeleveld D, Sleeman MA, van den Berg W, Wicks IP. GM-CSF as a therapeutic target in inflammatory diseases. Mol Immunol. 2013;56:675–682. doi: 10.1016/j.molimm.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 45.VanSeggelen H, Hammill JA, Dvorkin-Gheva A, Tantalo DG, Kwiecien JM, Denisova GF, Rabinovich B, Wan Y, Bramson JL. T Cells Engineered With Chimeric Antigen Receptors Targeting NKG2D Ligands Display Lethal Toxicity in Mice. Mol Ther. 2015;23:1600–1610. doi: 10.1038/mt.2015.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davila ML, Riviere I, Wang X, Bartido S, Park J, Curran K, Chung SS, Stefanski J, Borquez-Ojeda O, Olszewska M, Qu J, Wasielewska T, He Q, Fink M, Shinglot H, Youssif M, Satter M, Wang Y, Hosey J, Quintanilla H, Halton E, Bernal Y, Bouhassira DC, Arcila ME, Gonen M, Roboz GJ, Maslak P, Douer D, Frattini MG, Giralt S, Sadelain M, Brentjens R. Efficacy and toxicity management of 19–28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6:224ra225. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725–733. doi: 10.1056/NEJMoa1103849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maude SL, Barrett D, Teachey DT, Grupp SA. Managing cytokine release syndrome associated with novel T cell-engaging therapies. Cancer J. 2014;20:119–122. doi: 10.1097/PPO.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, Grupp SA, Mackall CL. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.