Abstract
Statement of the Problem:
In orthognathic surgeries, proper condylar position is one of the most important factors in postoperative stability. Knowing the condylar movement after orthognathic surgery can help preventing postoperative instabilities.
Purpose:
The aim of this study was to evaluate the condylar positional changes after Le Fort I maxillary superior repositioning along with mandibular advancement by using cone beam computed tomography (CBCT).
Materials and Method:
This cross-sectional study was conducted on 22 subjects who had class II skeletal malocclusion along with vertical maxillary excess. Subjects underwent maxillary superior repositioning (Le Fort I osteotomy) along with mandibular advancement. The CBCT images were taken a couple of days before the surgery (T0), and one month (T1) and 9 months (T2) after the surgery. The condyles positions were determined from the most superior point of the condyle to three distances including the deepest point of the glenoid fossa, the most anterior-inferior point of the articular eminence, and the most superior point of the external auditory meatus in the sagittal plane.
Results:
The mean mandibular advancement was 4.33±2.1 mm and the mean maxillary superior repositioning was 4.66±0.3 mm. The condyles displaced inferiorly, anteriorly, and laterally between T0 and T1. They were repositioned approximately in the initial position in T2. No correlation was observed between the mandibular and maxillary movement and the condylar positions.
Conclusion:
The condyles displaced in the inferior-anterior-lateral position one month after the bilateral sagittal split osteotomy for mandibular advancement in combination with the maxillary Le Fort I superior repositioning. It seems that the condyles adapted approximately in their initial position nine months after the surgeries.
Keywords: Mandible , Condyle , CBCT , Sagittal Osteotomy , Vertical Maxillary Excess
Introduction
Among the most determining factors of postoperative stability in orthognathic surgeries is the proper condylar position.[1] The location of mandibular condyle in the fossa can be changed by surgeons during fixation. Rigid fixation as an essential procedure for sagittal split osteotomy (SSO), is considered one of the major etiologies of temporomandibular disorder (TMD).[2] Knowing the condylar movement after orthognathic surgery is important to prevent postoperative instabilities.[3] However, condylar displacement within the physiologic capability of the adaptive mechanism does not lead to morphologic changes and dysfunction of temporomandibular joint (TMJ).[3] The postoperative condylar position is known to be affected by various factors such as rotational movement of the distal segment, tensional balance of the surrounding muscles, fixation method, and the surgeon’s experience.[1]
Cone beam computed tomography (CBCT) is a medical image acquisition technique based on a cone-shaped x-ray beam centered on a two-dimensional (2D) detector. The source-detector system rotates around the object and produces a series of 2D images. The images are reconstructed in a three-dimensional (3D) dataset by using a modification of the original cone-beam algorithm.[4] CBCT is the best modality for evaluation of bony and positional condylar changes in temporomandibular joints. It provides better information about glenoid fossa and its remodeling. Therefore, 3D CBCT can be a better modality in evaluation of the postoperative stability and changes of glenoid fossa.1 So far, few studies have used CT or CBCT to investigate the condylar changes after bimaxillary surgery. [1,3,5]
The purpose of this study was to evaluate the positional condylar changes compared to its original position in class II patients with vertical maxillary excess after Le Fort I maxillary superior repositioning in combination with mandibular advancement through bilateral SSO by using CBCT.
Materials and Method
This cross-sectional study was carried out between September 1st, 2010 and October 31st, 2012. The employed protocols were previously approved by the Medical Ethics Research Committee, Shiraz University of Medical Sciences. All the included subjects had class II skeletal deformity with vertical maxillary excess and underwent Le Fort I maxillary superior repositioning in combination with mandibular advancement through SSO. Patients with previous trauma or fracture in the mandible, osteotomy, or asymmetry were excluded from the study. Initially, the patients signed an informed written consent about using CBCT. The CBCT images were taken 1-2 days before surgery (T0), and then one month (T1), and nine months (T2) after surgery.
The CBCT scans were made by using New Tom VGI Flex (Image work Co.; USA) CBCT unit. We used a standardized protocol of the NewTom for the extended (15×15 cm) field of view (FOV) with 0.3-mm slice thickness and 26.9-s acquisition time.
To predict the horizontal and vertical changes in maxillary and mandibular movement during the surgery, two expert examiners analyzed the reference planes and points by using the CBCT software (QR NNT; V 2.0.4, Quantitative Radiology). These references were porion (the most superior point of external auditory meatus), orbitale (the lowest point of the inferior orbital rim), basion (the most posterior inferior point of occipital bone at the anterior margin of foramen magnum), nasion (the most anterior point of frontonasal suture in midsagittal plane), menton (the most inferior point on symphyseal outline on the anterior view), Frankfort horizontal (FH) plane (the plane made by both sides of porion and right side of orbitale), and midsagittal reference plane. For this reason, the distance from the FH plane to point A was used to determine the amount of maxillary superior repositioning before and after the surgery. The horizontal distance from the menton to the nasion perpendicular plane to point A (the most anterior point of the maxillary apical base) was applied to assess the amount of the mandibular advancement.
To evaluate the changes in the condylar position, two oral and maxillofacial radiologists evaluated the radiographs on two separate occasions with at least one-week interval. DICOM files of the pre- and post-surgery images were read by using the CBCT software (QR NNT; Version 2.0.4, Quantitative Radiology) which had a linear measurement capability.
To prepare the optimal cross-sectional image of the condyle, the axial section of the condylar process that had the widest mediolateral diameter on the left and right side condyles was chosen as the reference view (Figure 1).
Figure1.
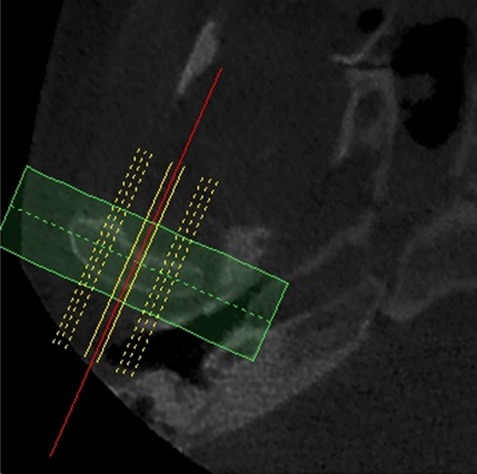
Measurement cuts in the axial view of the condyle.
In this reference view, a line parallel to the long axis of the condylar process was drawn and sagittal images were reconstructed as 0.5-mm slice interval and slice thickness. Three different linear distances on the central sagittal section of the condyle and another distance on the coronal section were obtained (Figure 2) including the most superior point of the condyle to the deepest point of the glenoid fossa in the sagittal plane, the most superior point of the condyle to the most anterior-inferior point of the articular eminence in the sagittal plane, and the most superior point of the condyle to the most superior point of the external auditory meatus in the sagittal plane. The most mid-superior point of the condyle to the deepest point of the glenoid fossa in the coronal plane was measured to control the accuracy of sagittal measurements.
Figure2.
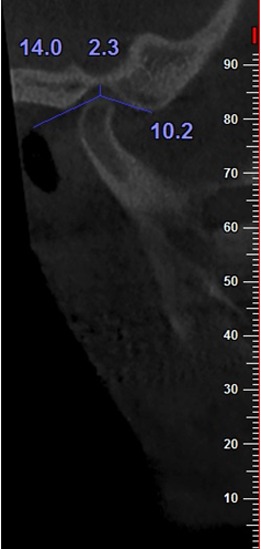
Condyle position in three measurements.
Surgical approach
The incision was made over the anterior portion of the vertical ramus, extending to the mesial aspect of the first molar. Subperiosteal dissection was carried out down to the inferior border of the mandible, where a lateral channel retractor was placed. A long bur was used to cut a horizontal bone through the medial cortex of the ramus, just above and approximately posterior to the lingula. The vertical cut was made through the buccal cortex, distal to the second molar or further anteriorly. The two osteotomies were then connected with a 701 fissure bur. The vestibular incision was made in the maxilla from the first molar to the contralateral first molar. The superior tissues were reflected subperiosteally, first at the piriform aperture margins. Then, the lateral, nasal, and infraorbital regions were exposed and extended posteriorly to the zygomatic maxillary buttress. Two internal reference points were marked intraorally to determine the anterior-posterior and vertical movements on each side of the maxilla. Osteotomy lines were made 5 mm superior to the apex of the teeth roots. After ending the osteotomies and down fracture, the maxilla was mobilized and positioned in the desirable position by using an intermediate splint. Bone interferences were removed and the maxilla was fixed with four miniplates. A spreader and a narrow osteotome were used to gently lift the lateral cortex of the sagittal osteotomy, and the osteotome was used to step along the connecting cut to ensure that the split stayed close to the lateral cortex. The mandible was positioned in the final position and the condyle was manually positioned by a superior and posterior pressure during fixation by using a miniplate and monocortical screws in each osteotomy site.
Statistical analyses
The statistical analyses were performed by using the IBM SPSS Statistics, version 19 (IBM; USA). A repeated-measures test was used to compare the four regions of interest before the surgery, one month, and nine months after the surgery. The Pearson correlation was applied to investigate the correlations between age, mandibular movement, and maxillary anterior and superior movement. An inter-examiner reliability analysis was performed through the kappa statistic to determine the consistency between the examiners.
Results
This study was conducted on 22 cases (15 females and 7 males) with the mean age of 22.18±5.6 years. The mean mandibular advancement was 4.33±2.1 mm and the mean maxillary superior repositioning was 4.66±0.3 mm. The mean maxillary anterior movement at point A was 1.04±0.87 mm. The distance between the condyle and the glenoid fossa in the sagittal plan was 3.62±1.43 mm before the operation, which increased to 4.13±1.43 mm one month after the surgery. The distance decreased to 3.80±1.50 mm at the third measurement which was 9 months after the surgery (Figure 3).
Figure3.
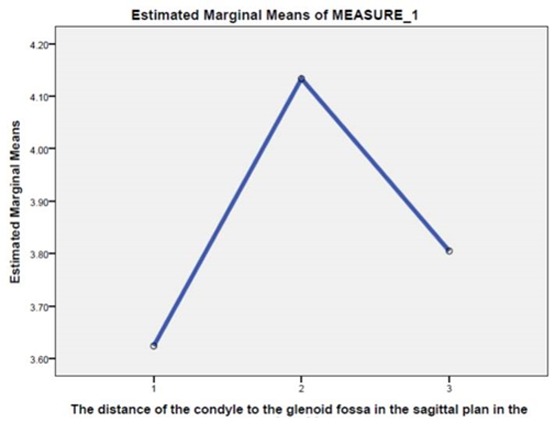
The distance between the condyle and glenoid fossa in the sagittal plane.
In the sagittal plane, a significant change in the distance of the condyle to the glenoid fossa in T0, T1, and T2 was observed. The mentioned distance changed between T0 and T1, but the condylar position was stable between T0 and T2 (Table 1).
Table 1.
Comparison of the distance between the condyle and glenoid fossa in the sagittal plane in various measurement times
| Time | Time | Pvalue | |
|---|---|---|---|
| The distance between the condyle and glenoid fossa in the sagittal plan (mm) | 3.62±1.43(T0) | 4.13±1.43(T1) | p< 0.05 |
| 3.62±1.43(T0) | 3.80±1.50(T2) | p> 0.05 | |
| 4.13±1.43(T1) | 3.80±1.50(T2) | p> 0.05 |
The distance of the condyle from the articular eminence in the sagittal plane was 10.81±1.99 mm in T0, 11.92±2.17 mm in T1, and 11.35±1.97 mm in T2. The changes of the mentioned distance were significant (Figure 4).
Figure4.
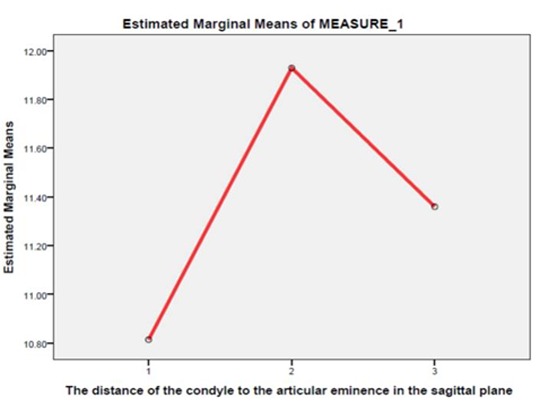
The distance between the condyle and articular eminence in the sagittal plane.
Assessment of the data indicated no positional change between T0 and T2; but significant change was detected between T0 and T1 in both condyles (Table 2).
Table 2.
Comparison of the distance between the condyle and articular eminence in the sagittal plane in various measurement times
| Time | Time | P.Value | |
|---|---|---|---|
| The distance between the condyle and articular eminence in the sagittal plane | 10.81±1.99(T0) | 11.92±2.17(T1) | p< 0.05 |
| 10.81±1.99(T0) | 11.35±1.97(T2) | p> 0.05 | |
| 11.92±2.17(T1) | 11.35±1.97(T2) | p> 0.05 |
The distance of the condyle from the superior point of the external auditory meatus was 12.81±1.97 mm in T0, 13.45±2.09 mm in T1, and 12.71±1.61 mm in T2. A repeated-measures test revealed a significant change of the condyle to the superior point of the external auditory meatus (Figure 5).
Figure5.
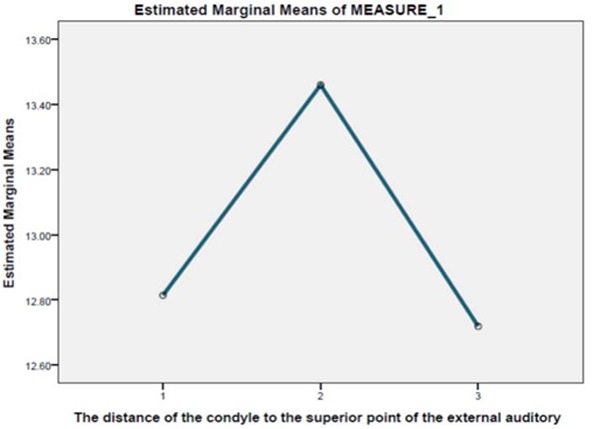
The distance between the condyle and superior point of the external auditory meatus.
Significant changes were observed between T0-T1, T1-T2, and T0-T2 (Table 3).
Table 3.
Comparison of the distance between the condyle and superior point of the external auditory meatus in various measurement times
| Time | Time | P.Value | |
|---|---|---|---|
| The distance between the condyle and the superior point of the external auditory meatus | 12.81±1.97(T0) | 13.45±2.09(T1) | p< 0.05 |
| 12.81±1.97(T0) | 12.71±1.61(T2) | p> 0.05 | |
| 13.45±2.09(T1) | 12.71±1.61(T2) | p< 0.05 |
The results revealed that the distance of the condyle to the superior in the external auditory meatus in the coronal plane was 3.75±1.6 mm in T0, 4.31±1.58 mm in T1, and 3.45±1.24 in T2. Changes of this distance were significant on both sides. Data analysis demonstrated significant changes between T0 and T1, with no change between T0 and T2.
Evaluation of the data by using Pearson correlation test revealed no association between the age and condylar changes in T0, T1, and T2 (p> 0.05). There was no correlation between the amount of the mandibular forward movement, maxillary superior reposition, and condylar changes in the measurement times (p> 0.05). The inter-examiner reliability was found to be Kappa 0.50 (p< 0.001), 95% confidence interval, indicating a moderate agreement between the examiners.
Discussion
Condylar displacement is one of the common complications of SSO. It can induce relapse and temporomandibular joint dysfunction symptoms. Several studies have shown that the condyle displaces after SSO in varying directions.[6-8] Skeletal changes such as mandibular setback surgery may affect other structures namely the TMJ or disc and their relationship.2 Displacement of the condyle from or in the fossa can be due to an abnormal mandibular movement, the methods used for fixation, segment rigidity, or masticatory muscle tension. Condylar displacement, especially after SSO, can result in postoperative complications. Furthermore, condylar displacement with altered inclination of the condylar long axis can substantially affect the postoperative function of TMJ. Simple sagittal displacement of the condyle can usually be corrected by postoperative adjustment of the occlusion. However, condylar displacement with axial rotation does not respond to occlusal adjustment and has an increased risk of TMD. Rotational changes also lead to idiopathic condylar resorption after SSO.[9] Yet, no investigation was conducted on the changes in condylar position after mandibular advancement with maxillary superior repositioning up to the time of the current study.
The present study showed that the condyle displaced inferiorly in the sagittal plane one month after mandibular advancement with maxillary superior repositioning. Then, it moved superiorly approximately in the initial position. In the second measurement, the condyle displaced laterally one month after the surgery in the sagittal plane and repositioned to its original position after nine months. In the third measurement, the condyle displaced anteriorly one month after the surgery; then it positioned more posteriorly than its initial position nine months after the surgery. Changes in the sagittal plane were controlled by evaluation of condylar changes to the superior point of the external auditory meatus in the coronal plane. A recent study demonstrated that the condyles moved inferoposteriorly immediately after the surgery; it was followed by anterosuperior movement three months after the SSO in combination with Le Fort I osteotomy. The condylar position in the glenoid fossa was evaluated by Pullinger and Hollender’s method. In their method, the anterior space (AS) and the posterior space (PS) were determined, and lnPS/AS was calculated. APS/AS> 0.25 indicated the anterior position of condyle in the glenoid fossa. If PS/ AS was< 0.25, it demonstrated the posterior position; and all the values in between indicated the concentric position. The authors also mentioned that the condyles tended to be positioned in a concentric position in relation to the glenoid fossa three months after the surgery and remained stable during the 1-year follow-up.[5]
Kang et al. employed CBCT to evaluate the postoperative condylar position by sagittal split ramus osteotomy. They used sagittal sections as well as 3D views to determine the condylar position.[6] Sagittal sections were also used by Pan et al. to compare the condylar position in the glenoid fossa in SSO and vertical ramus osteotomy.[10]
The postoperative position of condyle and the surgical techniques of intraoperative condylar fixation are still a field of discussion and an important aspect of TMD development after orthognathic surgeries. [11] Changes in the position of distal fragment (advancement and clockwise rotation during the surgical interval) and significant posterior relapse with clockwise rotation during the period of maxillomandibular fixation were reported. A small amount of counterclockwise rotation due to interocclusal splint removal was seen following the fixation release. It was observed that during the period of maxillomandibular fixation, both condyles exhibited a significant superior movement; the left condyle also moved posteriorly in SSO for mandibular advancement.[12] Another study demonstrated that the condylar displacement was not related with the mandible rotation. However, the condylar displacement in relation to the amount of backward movement of the mandible was significant, especially when it was greater than 10 mm of setback.[6] Harris et al. employed 3D computed tomography to study the changes in the condylar position after an SSO fixed with bicortical screws in order to assess the factors that may influence the ultimate position of the condyle after the surgery. They detected that 8 weeks after the SSO and mandibular advancement, most cases showed displacement of the condyle medially, posteriorly, superiorly, and angled medially. [13] Some studies demonstrated inward rotation of the condyle after SSO.[14-16]
The amount of mandibular advancement was not associated with medial-lateral change of the condyle. While, the amount of advancement was associated with the condyle angulation and superior-inferior changes in condyle position; there was no correlation between the amount of advancement and medial or anterior-posterior change in condyle position. Likewise, no associate was found between any of the condylar movements and the degree of proximal segment rotation or the shape of mandible.[13] Our study did not indicate any correlation between the mandibular advancement, maxillary superior repositioning and the condylar changes. Lee and Park demonstrated similar results in the mandibular setback by using SSO.[8]
Park et al. reported that bimaxillary orthognathic surgery decreased the condylar heights and condylar head remodeling. The CBCT volume superimposition method showed that the condylar head underwent remodeling after bimaxillary surgery.[3] Ueki et al. suggested that SSO, either with or without Le Fort I osteotomy, could not change the preoperative disc position or correct the anterior disc displacement, although these procedures did improve the symptoms associated with TMJ dysfunction.[17] After bimaxillary surgery, the neuromuscular function and bite force improve during the course of general recovery. The compressive force on the anterior and superior aspects of the condylar head in the articular fossa could be accounted for the decrease of condylar head size. The bony changes produced by the recovery of oral function might be a physiologic adaptive bone remodeling.[3]
CT scans, particularly the 3D types, have errors in evaluation of condylar changes after orthognathic surgery. These errors are related to slice thickness, window level and width, matrix size, and rendering technique.[18] A 3D analysis gives additional information compared with the traditional cephalometric methods. Moreover, quantification of the 3D morphologic changes poses methodological challenges. In this study, to measure the distances between the bone surfaces at the two times, the closest surface point method was used.[19] The postoperative condyles may be displaced three dimensionally; that is, the condyles may change not only in position, but also in inclination. It is difficult to differentiate a true condylar displacement from a radiographic error.[15]
Sanroman et al. compared MRI and CT scans of patients undergoing orthognathic surgery pre- and postoperatively with regard to TMJ disorders. The results showed that the condylar position was different after the surgery; however, no alteration was noted in the final clinical outcome.[20]
One of the possible explanations for the condylar adaptation after 9 months is bone remodeling that follows SSOs. Enami et al. suggested that bone remodeling happen after SSO and is a main reason for morphological changes.[21] Fixation method is another important issue in condylar displacement after SSO. In the current study, we used only miniplates for fixation method. Furthermore, a recent study reported that more rigid fixation by bicortical screws were associated with less flexibility in postoperative condyle adaptation.[22] It was suggested that CT value of condylar bone changes and anterior disc displacement may happen 1 year after SSO.[23]
Conclusion
According to the results of this study it can be concluded that the condyles displace in the inferior-anterior-lateral position one month after the SSO for mandibular advancement in combination with the maxillary Le Fort I superior repositioning. It seems that the condyles adapted approximately in their initial position nine months after the surgeries. Additionally, the amount of mandibular advancement and maxillary superior repositioning may not correlate with condylar changes.
Footnotes
Conflict of interests: The authors of this manuscript certify no financial or other competing interest regarding this article.
References
- 1.Kim YJ, Oh KM, Hong JS, Lee JH, Kim HM, Reyes M, et al. Do patients treated with bimaxillary surgery have more stable condylar positions than those who have undergone single-jaw surgery? . J Oral Maxillofac Surg . 2012;70: 2143–2152. doi: 10.1016/j.joms.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 2.Kim YK, Yun PY, Ahn JY, Kim JW, Kim SG. Changes in the temporomandibular joint disc position after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108: 15–21. doi: 10.1016/j.tripleo.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Park SB, Yang YM, Kim YI, Cho BH, Jung YH, Hwang DS. Effect of bimaxillary surgery on adaptive condylar head remodeling: metric analysis and image interpretation using cone-beam computed tomography volume superim-position. J Oral Maxillofac Surg. 2012; 70: 1951–1959. doi: 10.1016/j.joms.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 4.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg. 2009; 38: 609–625. doi: 10.1016/j.ijom.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 5.Chen S, Lei J, Wang X, Fu KY, Farzad P, Yi B. Short- and long-term changes of condylar position after bilateral sagittal split ramus osteotomy for mandibular advancement in combination with Le Fort I osteotomy evaluated by cone-beam computed tomography. J Oral Maxillofac Surg. 2013; 71: 1956–1966. doi: 10.1016/j.joms.2013.06.213. [DOI] [PubMed] [Google Scholar]
- 6.Kang MG, Yun KI, Kim CH, Park JU. Postoperative condylar position by sagittal split ramus osteotomy with and without bone graft. J Oral Maxillofac Surg. 2010; 68: 2058–2064. doi: 10.1016/j.joms.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Hackney FL, Van Sickels JE, Nummikoski PV. Condylar displacement and temporomandibular joint dysfunction following bilateral sagittal split osteotomy and rigid fixation. J Oral Maxillofac Surg. 1989; 47: 223–227. doi: 10.1016/0278-2391(89)90221-8. [DOI] [PubMed] [Google Scholar]
- 8.Lee W, Park JU. Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94: 305–309. doi: 10.1067/moe.2002.126452. [DOI] [PubMed] [Google Scholar]
- 9.Ueki K, Degerliyurt K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. Horizontal changes in the condylar head after sagittal split ramus osteotomy with bent plate fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106: 656–661. doi: 10.1016/j.tripleo.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Pan JH, Lee JJ, Lin HY, Chen YJ, Jane Yao, CC Kok, SH Transverse and sagittal angulations of proximal segment after sagittal split and vertical ramus osteotomies and their influence on the stability of distal segment. J Formos Med Assoc. 2013; 112: 244–252. doi: 10.1016/j.jfma.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Draenert FG, Erbe C, Zenglein V, Kämmerer PW, Wriedt S, Al Nawas, B 3D analysis of condylar position after sagittal split osteotomy of the mandible in mono- and bimaxillary orthognathic surgery- a methodology study in 18 patients. J Orofac Orthop. 2010; 71: 421–429. doi: 10.1007/s00056-010-1021-9. [DOI] [PubMed] [Google Scholar]
- 12.Will LA, Joondeph DR, Hohl TH, West RA. Condylar position following mandibular advancement: its relationship to relapse. J Oral Maxillofac Surg. 1984; 42: 578–588. doi: 10.1016/0278-2391(84)90088-0. [DOI] [PubMed] [Google Scholar]
- 13.Harris MD, Van Sickels, JE Alder, M Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg. 1999; 57: 650–654. doi: 10.1016/s0278-2391(99)90422-6. [DOI] [PubMed] [Google Scholar]
- 14.Ghang MH, Kim HM, You JY, Kim BH, Choi JP, Kim SH, et al. Three-dimensional mandibular change after sagittal split ramus osteotomy with a semirigid sliding plate system for fixation of a mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115: 157–166. doi: 10.1016/j.oooo.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E. Change in condylar long axis and skeletal stability following sagittal split ramus osteotomy and in-traoral vertical ramus osteotomy for mandibular progna-thia. J Oral Maxillofac Surg. 2005; 63: 1494–1499. doi: 10.1016/j.joms.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Nishimura A, Sakurada S, Iwase M, Nagumo M. Positional changes in the mandibular con-dyle and amount of mouth opening after sagittal split ramus osteotomy with rigid or non rigid osteosynthesis. J Oral Maxillofac Surg. 1997; 55: 672–676. doi: 10.1016/s0278-2391(97)90572-3. [DOI] [PubMed] [Google Scholar]
- 17.Ueki K, Marukawa K, Shimada M, Hashiba Y, Nakgawa K, Yamamoto E. Condylar and disc positions after sagittal split ramus osteotomy with and without Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103: 342–348. doi: 10.1016/j.tripleo.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa K, Langlais RP. Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 85: 371–376. doi: 10.1016/s1079-2104(98)90059-2. [DOI] [PubMed] [Google Scholar]
- 19.Carvalho Fde, A Cevidanes, LH da, Motta AT, Almeida MA, Phillips C. Three-dimensional assessment of mandibular advancement 1 year after surgery. Am J Orthod Dentofacial Orthop. 2010; 137(4 Suppl): S53.e1–12. doi: 10.1016/j.ajodo.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernández Sanromán, J Gomez, Gonzalez JM, Alonso Del, Hoyo J, Monje Gil, F Morphometric and morphological changes in the temporomandibular joint after orthognathic surgery: a magnetic resonance imaging and computed tomography prospective study. J Craniomaxillofac Surg. 1997; 25: 139–148. doi: 10.1016/s1010-5182(97)80005-4. [DOI] [PubMed] [Google Scholar]
- 21.Enami K, Yamada K, Kageyama T, Taguchi A. Morpho-logical changes in the temporomandibular joint before and after sagittal splitting ramus osteotomy of the mandible for skeletal mandibular protrusion. Cranio. 2013; 31: 123–132. doi: 10.1179/crn.2013.020. [DOI] [PubMed] [Google Scholar]
- 22.Han JJ, Hwang SJ. Three-dimensional analysis of post operative returning movement of perioperative condylar displacement after bilateral sagittal split ramus osteotomy for mandibular setback with different fixation methods. J Craniomaxillofac Surg. 2015; 43: 1918–1925. doi: 10.1016/j.jcms.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Ueki K, Yoshizawa K, Moroi A, Iguchi R, Kosaka A, Ikawa H, et al. Changes in computed tomography values of mandibular condyle and temporomandibular joint disc position after sagittal split ramus osteotomy. J Cranio-maxillofac Surg. 2015; 43: 1208–1217. doi: 10.1016/j.jcms.2015.05.007. [DOI] [PubMed] [Google Scholar]


