Abstract
Introduction:
Surgical and medical treatments of nasal obstruction are a common parts of otolaryngologist practice. The definitive treatment of deviated nasal septum is septoplasty.
Aim:
In this study was to evaluate the values of subjective parameters, and active anterior rhinomanometry parameters prior and three months after the septoplasty.
Patients and Methods:
We analyzed the subjective parameters (“NOSE” scale), the active anterior rhinomanometry parameters according to International Committee on Standardization of Rhinomanometry, on 40 patients. Thirty healthy adult volunteers participated belonged to the control group. None of the patients or healthy volunteers had previous history of nasal surgery or active rhinological disease.
Results:
The post-operative improvement in symptoms of nasal obstruction obtained in 92,5% patients and improvement parameters of the active anterior rhinomanometry in 42,5% patients.
Conclusion:
The correlation between the findings with rhinomanometry and subjective sensation of nasal patency remains uncertain. There still seems to be only a limited argument for the use of rhinomanometry for quantifying surgical results. Three months postoperative findings are very early results to interpret the permanent effects.
Keywords: nasal septum deviation, septoplasty, active anterior rhinomanometry, Nasal Obstruction Symptom Evaluation Scale
1. INTRODUCTION
Chronic nasal airway obstruction is one of the most frequent complaints visited to otolaryngologists by the patients. Deviation of nasal septum is a common anatomic variation and the most frequently causes of nasal obstruction (1, 2, 3). The Nasal Obstruction Symptom Evaluation Scale (NOSE) has valid, reliable, and responsive instrument that is brief and easy to complete and has potential use for outcomes studies in adults with nasal obstruction (4, 5). Rhinomanometry has been described as a gold standard for measurement of nasal obstruction (6). The definitive treatment of deviated nasal septum is septoplasty, and this surgical procedure is a very effective and satisfactory treatment and should improve the quality of life (7). Sometimes nasal obstruction can persist after septoplasty. In the current study, we evaluated the values of subjective parameters (NOSE score) and active anterior rhinomanometry parameters of deviated nasal septum before and three months after septoplasty.
2. PATIENTS AND METHODS
Forty patients with nasal septal deviation for study group and 30 healthy adult volunteers participated belonged to the control group were accepted to the study. All individuals studied had no previous history of nasal surgery or active rhinological disease and had not taken antihistamines, systemic or nasal steroids during the previous three months. Active anterior rhinomanomtry was the applied method using rhinomanometry to measure the transnasal airway resistance and nasal airflow. Before the test, subjects were confined to a quiet room for at least 30 min and consumed/inhaled no caffeine, alcohol or nicotine for the period of the analysis (8). The Nasal Obstruction Symptom Evaluation Scale (NOSE) Questionnaire was the applied before and 3 months after surgery. Septoplasty was performed by Cotll’s method.
Inclusion criteria: 18 years or older ages, septal deviation consistent with symptom of chronic nasal obstruction.
Exclusion criteria: were sinonasal malignancy, septoplasty performed as access to other sites, prior septoplasty, rhinoplasty, or turbinoplasty, history or clinical evidence of chronic sinusitis, septal perforation, craniofacial syndrome, acute nasal trauma or fracture in the past 3 months, nasal valve collapse, adenoid hypertrophy, sarcoidosis, Wegener’s granulomatosis, uncontrolled asthma, pregnancy, and illiteracy. Limited demographic data were collected on patients who refused enrollment or excluded.
Data analysis was carried out using the SPSS 10.0 (SPSS Inc., Chicago, IL). The Kolmogorov-Smirnov test assessed the compliance concerning the distribution of values in the normal curve. The ANOVA test for compare parameters active anterior rhinomanometry and non-parametric Wilcoxon T test was utilized in order to compare the NOSE questionnaire scores before and three months after surgery. We assessed the correlation between the preoperative score and the postoperative improvement, calculated by the difference between the postoperative and preoperative scores, using the Pearson correlation test. A p value lower than 5% was deemed significant.
3. RESULTS
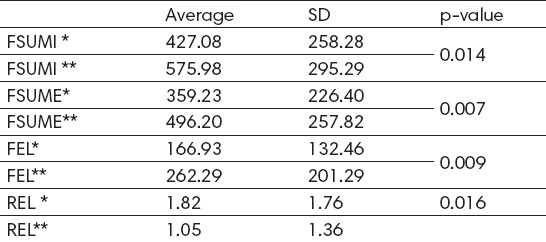
We analyzed 40 examinees on the experimental group: male patients (62.5%), (age 27.6 years ± 10.80; range 16-55 years: median 25). Control group: male patients 70% (age 33.4 ± 7. 95: range 18-58; median 34). The post-operative improvement in symptoms of nasal obstruction obtained in 92.5% patients and improvement parameters of the active anterior rhinomanometry in 42.5% patients. Table 1 shown statistically significant differences in the measurement of active anterior rhinomanometry before and after the septoplasty. Statistically significant improvement shown by the parameters: Sum of inspiratory flow; Sum of expiratory flow; Expiratory resistance of left; Expiratory resistance of left (p≤0.05).
Table 1.
Testing the parameters of rhinomanometry before* and after surgery**. FSUMI- Sum of inspiratory flow; FSUME- Sum of expiratory flow; REL expiratory resistance of left; FEL expiratory resistance of left; p≤0.05.
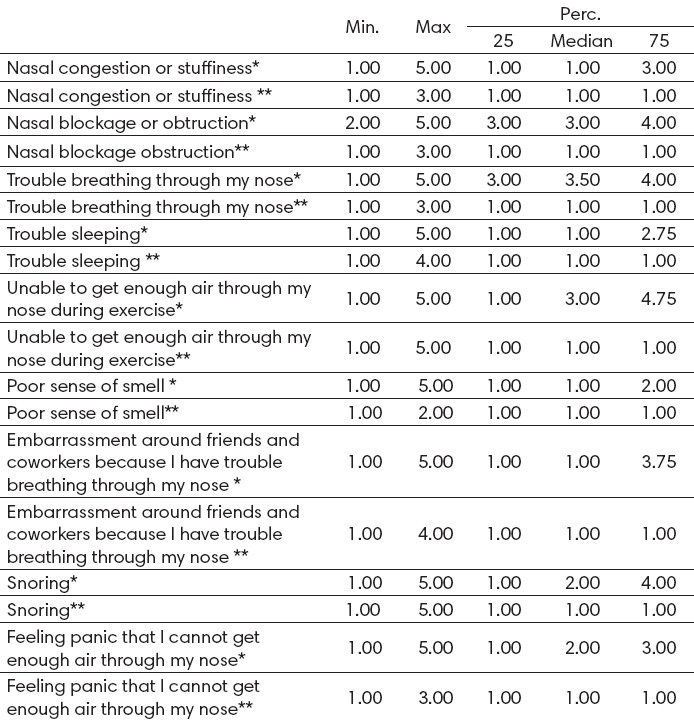
There was a statistically significant improvement shown by the Wilcoxon T test (Z=-5.34; p<0.001) -between the preoperative NOSE questionnaire score and three months later (Table 2). After the surgery correlated values of the parameters of active anterior rhinomanometry and NOSE scale. There was no statistically significant correlation between the values of active anterior rhinomanometry and NOSE scale.
Table 2.
Statistically significant differences in the parameters NOSE scale before* and after** surgery
4. DISCUSSION
This is a prospective analysis of 40 patients with nasal septal deviations, before and three months after septoplasty. Their mean age was 27.6 years. Other studies have patients with similar age means (20-31 years) (3, 9, 10).
In the current study the post-operative improvement in symptoms of nasal obstruction obtained in 92.5% patients and improvement parameters of the active anterior rhinomanometry in 42.5% patients. This is similar to that in the most of the published. Zahedi et al. (11) and Stewart et al. (4) have noted a weak correlation between subjective symptoms and rhinoscopic findings. Dinis and Haider (12) reported that patients with significant nasal obstruction have milder degrees of septal deviation, while other patients with severe septal deformities have mild symptoms. The post-operative improvement in symptoms of nasal obstruction was reported to range between 26 and 94.4% depending on the length of follow-up and the method of assessment of results (7, 13-16). Sipila and Sounpaa (17) showed that postoperatively were satisfied with 85% of patients who had high preoperative intranasal resistance, compared with 69% of satisfied patients who have had a proper preoperative intranasal resistance. Dommerby et al. (18) analyzed postoperative results of 161 patients after septoplasty (25-64 months). They reported that 35% of patients were not satisfied with the operation of which is 9% of cases the cause of dissatisfaction was not in compliance with postoperative rhinoscopic findings in 11% of patients the reason for dissatisfaction was associated with the results of operations.
There is a lack of medical literature demonstrating a positive correlation between subjective and objective results in functional nasal surgery. One of the works confirming that claim is by Murrell (19). The author presents his experience measuring nasal function subjectively and objectively before and after functional nasal surgery. Statistically significant subjective and objective functional improvements were reported in 98.9% and 95.6% of patients, while 94.4% of patients had both subjective and objective statistically significant functional improvement. Dürr et al. (20) in 41 patients before and after septoplasty, nasal resistance examined, olfactory function and subjective symptoms. The authors noted that after the surgery was not significantly changed olfactory functions. In addition, an increase of nasal ventilation, functional and cosmetic nasal surgery can lead to improved olfactory function.
Gupta et al. (21) investigated the olfactive function changes after septoplastics in 41 patients. The authors recorded the improvement in olfactory function in 29 patients (70.6%); there was no change in 5 patients (20.1%); and reduced olfactory function was noticed in 3 (7.3%) patients. The authors concluded that, even though the septal surgery is performed in an area remote from the olfactory epithelial area, changes in nasal airflow and intranasal volume can change the olfactory function of an individual.
Shammas et al. (9) noted that there is a significant correlation between the subjective sensation of nasal obstruction, clinical rhinoscopic findings and the objective rhinomanometric measurements of nasal airway resistance and nasal airflow. Authors recommended to use rhinomanometry in patient selection who need septal surgical correction, knowing that the severity of nasal septal deformity does not always correlate with the severity of the clinical features. However, in our study was no statistically significant correlation between the values of active anterior rhinomanometry and NOSE scale. We found out the discrepancy between subjective (NOSE) and objective findings (rhinomanometry) after septoplasty.
5. CONCLUSION
The correlation between the findings with rhinomanometry and subjective sensation of nasal patency remains uncertain. There still seems to be only a limited argument for the use of rhinomanometry for quantifying surgical results. Three months postoperative findings are very early results to interpret the permanent effects.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Haroon Y, Saleh HA, Abou-Issa AH. Nasal soft tissue obstruction improvement after septoplasty without turbinectomy. Eur Arch Otorhinolaryngol. 2013;270:2649–55. doi: 10.1007/s00405-012-2304-0. [DOI] [PubMed] [Google Scholar]
- 2.Kuduban O, Bingol F, Budak A, Kucu C. The Reason of Dissatisfaction of Patient after Septoplasty. Eurasian J Med. 2015;47(3):190–3. doi: 10.5152/eurasianjmed.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reitzen SD, Chung W, Shah AR. Nasal septum deviation in the pediatric and adult populations. Ear Nose Throat J. 2011;90:112–5. doi: 10.1177/014556131109000308. [DOI] [PubMed] [Google Scholar]
- 4.Stewart M, Witsell D, Timothy L, Smith T, Edward M, Yueh B, Maueen T, Hannley M. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) Scale. Otolaryngol Head Neck Surg. 2004;130:157–63. doi: 10.1016/j.otohns.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Yilmaz MS, Guven M, Akidil O, Kayabasoglu G, Demir D, Mermer H. Does septoplasty improve the quality of life in children? Int J Pediatr Otorhinolaryngol. 2014;78(8):1274–6. doi: 10.1016/j.ijporl.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Schumacher MJ. Nasal dyspnoea: the place of rhinomanometry in its objective assessment. Am J Rhinol. 2004;18:41–6. [PubMed] [Google Scholar]
- 7.Bezerra TFP, Steward MG, Fornazierei MA, et al. Quality of life assessment septoplasty in patient with nasal obstruction. Braz J Otorhinolaryngol. 2012;78:57–62. doi: 10.1590/S1808-86942012000300011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clement PAR. Commitete report on standardization of rhinomanometry. Rhinology. 1984;22:151–5. [PubMed] [Google Scholar]
- 9.Shammas S. Khammas A.H. Albayati A.I. Rhinomanometry evaluation in Septoplasty. Iraqi J Comm Med. 2007;20(2):363–8. [Google Scholar]
- 10.Sahan M, Deveer M, Erdogan S, Tetiker H, Koseoglu S. The Causes of Persistent and Recurrent Nasal Obstruction After Primary Septoplasty. J Craniofac Surg. 2016;27(4):828–30. doi: 10.1097/SCS.0000000000002505. [DOI] [PubMed] [Google Scholar]
- 11.Zahedi FD, Husain S, Gendeh BS. Functional Outcome Evaluation of Septorhinoplasty for Nasal Obstruction. Indian J Otolaryngol Head Neck Surg. 2016;68(2):218–23. doi: 10.1007/s12070-015-0899-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dinis PB, Haider H. Septoplasty: long term evaluation of results. Am J Otolaryngol. 2002;23:85–90. doi: 10.1053/ajot.2002.30987. [DOI] [PubMed] [Google Scholar]
- 13.Siegel N, Gliklich R, Taghizadeh F, Chang Y. Outcomes of septoplasty. Otolaryngol Head Neck Surg. 2000;122(2):229–32. doi: 10.1016/S0194-5998(00)70244-0. [DOI] [PubMed] [Google Scholar]
- 14.Chambers KJ, Horstkotte KA, Shanley K, Lindsay RW. Evaluation of in Nasal Obstruction Following Nasal Valve Correction in Patients With a History of Failed Septoplasty. JAMA Facial Plast Surg. 2015;17(5):347–50. doi: 10.1001/jamafacial.2015.0978. [DOI] [PubMed] [Google Scholar]
- 15.Uppal S, Mistry H, Nadig S, Back G, Andrew C. Evaluation of patient benefit from nasal septal surgery for nasal obstruction. Auris Nasus Larynx. 2005;32:129–37. doi: 10.1016/j.anl.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Velasco LC, Arima LM, Tiago RS. Assessment of symptom improvement following nasal septoplasty with or without turbinectomy. Braz J Otorhinolaryngol. 2011;77(5):577–83. doi: 10.1590/S1808-86942011000500007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sipila J, Sounpaa J. A prospective study using rhinomanometry and patient clinical satisfaction to determine if objective measurements of nasal airway resistance can improve the quality of septoplasty. Eur Arch Otorhinolaryngol. 1997;254:387–90. doi: 10.1007/BF01642556. [DOI] [PubMed] [Google Scholar]
- 18.Dommerby H, Rasmussen OR, Rosborg J. Long-term results of septal operations. J Otorhinolaryngol Relat Spec. 1985;47:151–7. doi: 10.1159/000275761. [DOI] [PubMed] [Google Scholar]
- 19.Murrell GL. Correlation between subjective and objective results in nasal surgery. Aesthet Surg J. 2014;34(2):249–57. doi: 10.1177/1090820X13520001. [DOI] [PubMed] [Google Scholar]
- 20.Dürr J, Lindemann J, Keck T. Sense of smell before and after functional esthetic rhinoplasty. HNO. 2002;50(7):626–9. doi: 10.1007/s00106-001-0586-4. [DOI] [PubMed] [Google Scholar]
- 21.Gupta N, Singh PP, Bagla RK. Will Septal Correction Surgery for Deviated Nasal Septum Improve the Sense of Smell? A Prospective Study. Surg Res Pract. 2015;32:496–505. doi: 10.1155/2015/496542. [DOI] [PMC free article] [PubMed] [Google Scholar]


