Abstract
Aims and objectives:
It is widely recognized that Intensive Care Unit (ICU) patients have a greater likelihood of developing pressure ulcers in comparison to hospital or home care patients. Accordingly, this study aimed to evaluate whether specific clinical characteristics could be used as clinical indicators towards pressure ulcers prevention.
Method:
We monitored 210 hospitalized ICU patients during a 12-month period. Pressure ulcers were assessed following the current guidelines. Clinical characteristics such as gender, age, hospitalized days, hemodialysis treatment, hematocrit, and serum albumin levels were considered as the most common predictors for pressure ulcers development. The significance of associations was controlled using multiple logistic regression after adjusting for clinical characteristics and was presented as adjusted odds ratio (AOR).
Results:
The prevalence of pressure ulcers was 24.3%. Logistic regression revealed that patients with increased age AOR=1.04; (CI: 1.01-1.07) and last-long hospitalization AOR=1.17; (CI: 1.11-1.23) were significantly more likely to present pressure ulcers compared to the younger ones and patients with less length of stay, respectively. We also found that patients under hemodialysis treatment were more likely to present pressure ulcers AOR=4.09; (CI: 1.12-14.98) compared to patients that did not underwent hemodialysis and the risk of pressure ulcers development was decreased by 9% for every single unit of hematocrit value increase AOR=0.91; (CI: 0.82-0.99).
Conclusion:
Our data analysis confirms that the clinical characteristics that were studied are independently associated with pressure ulcers development, and therefore, it is a crucial incentive to consider that these specific clinical characteristics are important indicators in the evidence-based practice.
Keywords: pressure ulcers, predictors, risk factors, intensive care unit, prevention, evidence-based practice
1. INTRODUCTION
Pressure ulcers are common complications that affect least 10% of patients in acute care, 3% in long-term care and 4% in home care. Pressure ulcers affect largely the intensive care patients and its prevalence has been reported to exceed 28%, especially in ageing (1, 2). Clinically, pressure ulcer is defined by the occurrence of a confined destruction of a certain skin area and of the underlying tissues due to external pressure, leading to the necrosis of the ischaemic area (3, 4). It has been demonstrated that except long-lasting hospitalization, the inept elevation or turning of the patient, the folds of the sheets, and the foreign bodies such as food remains or fragments of plaster cast, were the most common risk factors contributing to the development of pressure ulcers (5, 6). Pressure ulcers pose important complications not only due to their high prevalence, but also because these are associated with conditions that account for leading causes of in-hospital mortality including anemia, and kidney diseases (7).
It has been suggested that patients attending intensive care units (ICU), often have higher prevalence rates of pressure ulcers and length stay compared to other hospitalized patients (8, 9). In the international literature, an association of both; pressure ulcers and length stay has also been reported (10), but a potential link between pressure ulcers and risk factors that are associated with their development has not been studied extensively in Greece (11). Therefore, evidence of an association between pressure ulcers and factors that increases the risk could serve as a crucial incentive for the systematic development of indicators in evidence-based practice.
Consequently the purpose of this study was to estimate the prevalence of pressure ulcers, and evaluate possible epidemiological association between the prevalence of pressure ulcers and specific clinical characteristics in order to develop clinical indicators towards pressure ulcers prevention. Our secondary aim was to examine the incidence of pressure ulcers with respect to length of stay in our study participants.
2. METHODS
Study design
In this prospective study we enrolled patients who were hospitalized in a public ICU in Greece, during a 12-month period (January to December 2013). We used a convenience sampling study involving subjects who were monitored during their entire hospitalization in the ICU, until their carriage to another hospital ward or clinic. We excluded 26 patients that had already produced pressure ulcers before their admittance to the ICU. Finally, of the total of 236 ICU patients that were hospitalized in the year of 2013, a total of 210 were fully met the inclusion criteria and involved in the statistical analysis–(response rate 89%).
Study analysis
Pressure ulcers were assessed by two experienced ICU nurses following the recent guidelines. Specifically, rely on skin temperature, we assessed change in tissue consistency and pain rather than identification of nonblanchable erythema – (stage I). Skin heat, tenderness, change in tissue consistency and pain was also assessed to assist in identifying the severity of pressure ulcers – (stage II) (12). Completing a comprehensive initial assessment of the individual with a pressure ulcer we employed the Cubbin and Jackson scale to control the sensitivity level of our data collection identifying patients at high-risk toward pressure ulcers development (13). Cubbin and Jackson scale has been widely used in intensive care showing high sensitivity 0.89 and specificity 0.61 for an intensive therapy patients (14). Briefly, the questionnaire evaluates specific variables such as general skin condition, mental condition, mobility, nutrition, respiration, incontinence, body hygiene, and hemodynamic status of patients. Summary score ranges between 10 and 40 (variables ranking 1-4), and a score less than 28 is indicative of high-risk for pressure ulcers development. The patients’ assessment concerning the hazard of turning up with pressure ulcers was conducted during the first 24 hours after their admittance to the ICU as well as after each significant change of their clinical condition.
To record specific clinical characteristics such as length of ICU stay, history of hemodialysis treatment, hematocrit (Ht) and albumin values we checked for laboratory tests in the medical records of individuals. Demographic characteristics such as gender and age were also recorded.
Statistical analysis
Descriptive frequency distributions of demographic and clinical characteristics of 210 ICU patients were calculated and tested as quantitative variables using simple logistic regression with binary outcomes. To adjust for potential confounding effects by gender, age and clinical characteristics, multiple logistic regression analysis was performed regarding the strength and direction of associations between pressure ulcers and clinical characteristics (backward method) and were presented using adjusted odds ratio (AOR), corresponding 95% confidence intervals (CI). All reported p-values were two-tailed, and a p-value<0.05 was considered statistically significant. Data were analyzed using the SPSS (version 19.0, Inc., Chicago, IL, USA).
Ethics
The study was conducted as a part of the clinical development of nursing interventions in intensive care, and therefore meets the written ethical approval by the Scientific Council of Nursing Department–Technological Institute of Thessaly.
3. RESULTS
Demographic characteristics
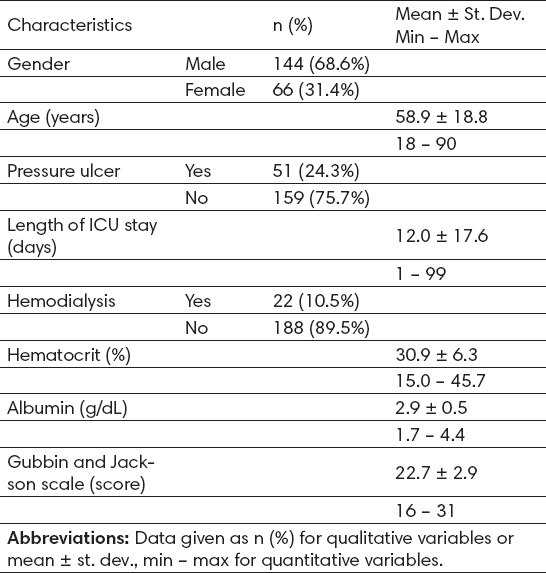
Demographic and clinical characteristics are presented in Table 1. The mean age and the length stay of the study subjects was 58.9 ± 18.8 and 12.0 ± 17.6, respectively. The prevalence of pressure ulcers was 24.3%, representing 2524 days of hospitalization were allocated (patient-days). The incidence rate (IR) of pressure ulcers was 2 cases per 100 patient-days IR=0.02; (95% CI: 0.015-0.026) [data not shown]. Also, the mean value of Ht and Albumin was 30.9 ± 6.3 and 2.9 ± 0.5, respectively. These findings were observed despite the fact that 10.5% of the subjects had already undergone hemodialysis treatment.
Table 1.
Demographic and clinical characteristics of the 210 patients
Prevalence differences between patients with and without pressure ulcers
Prevalence of pressure ulcers did not differ between males and females (21.5% vs. 30.3%, p=0.170), while the mean age was also greater for patients with pressure ulcers (63.4 ± 17.5 vs. 57.5 ± 19.0, p=0.050) compared to patients without pressure ulcers (Table 2).
Table 2.
Differences between patients with and without pressure ulcers (PU) according to clinical characteristics
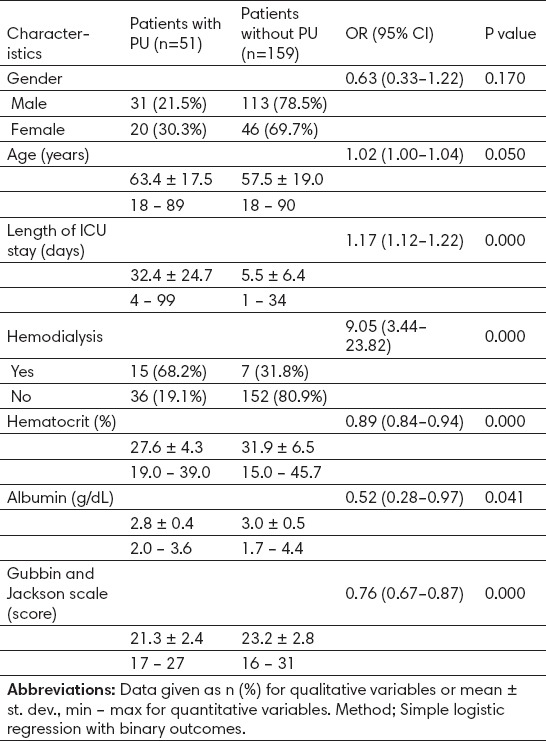
Bivariate logistic regression revealed that pressure ulcers were significantly presented more often in patients with greater length stay OR=1.17; (CI: 1.12-1.22) and, patients that underwent hemodialysis treatment OR=9.05; (CI: 3.44-23.82). However, patients with pressure ulcers were significantly presented with lower values of hematocrit OR=0.89; (CI: 0.84-0.94) and albumin OR=0.52; (CI: 0.28-0.97), compared to patients without pressure ulcers. Also, we found that patients with pressure ulcers were significantly more likely to present lower mean Gubbin and Jackson scale score (OR=0.76, p=0.000) compared to patients without pressure ulcers, suggesting that these patients were at high-risk for pressure ulcers development (Table 2).
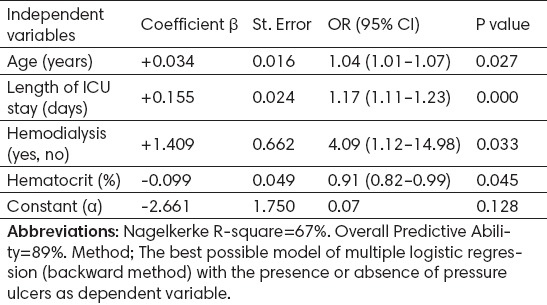
Risk assessment for pressure ulcers development
Multiple logistic regression was also revealed that these prevalence differences were significant even after adjusting (AOR) for patient’s clinical characteristics (Table 3). Practically, the risk of pressure ulcers development was increased by 4% for every single year of age growing AOR=1.04; (CI: 1.01-1.07). This risk was also increased for every single day of extended hospitalization by 17% AOR=1.17; (CI: 1.11-1.23). We also found that patients whose underwent hemodialysis treatment had a greater likelihood of developing pressure ulcers AOR=4.09; (CI: 1.12-14.98) compared to patients that did not underwent. These findings were observed while the risk of pressure ulcers development was decreased by 9% for every single unit of hematocrit value increase AOR=0.91; (CI: 0.82-0.99).
Table 3.
Associations among clinical characteristics regarding pressure ulcers development
4. DISCUSSION
We assessed the prevalence of pressure ulcers and explored its association with the specific clinical characteristics among ICU patients. Our data analysis revealed that the prevalence of pressure ulcers was 24.3% and the incidence rate was 0.02 per patient-day. Importantly, 67% of the pressure ulcers frequency could be explained by age, length of ICU stay, hemodialysis, and hematocrit as predicting factors according to our analysis, suggesting that pressure ulcers are more prevalent in older people and independently associated with these specific clinical characteristics. Our results are similar to figures reported worldwide. In particular, the prevalence of pressure ulcers in the United States as previous reported ranging 10% to 18% in acute care, 2.3% to 28% in long-term care, and 0% to 29% in home care, while the incidence rate ranges from 0.4% to 38% in acute care, 2.2% to 23.9% in long-term care, and 0% to 17% in home care (1, 2). Similarly, an overall prevalence among European countries (Belgium, Italy, Portugal, Sweden, and the United Kingdom) was found 18.1%, although there were frequency variations among countries (15).
However, the main finding of the present study was that patients with long-lasting hospitalization were presented with a greater likelihood of developing pressure ulcers, suggesting that as length stay increases, as higher occurrence of pressure ulcers. In agreement with our finding, a recent study conducted in ICU in Saudi Arabia, showed that the length of stay and increased age were the most significant predictors of all stages of pressure ulcers development (16). Also important, data analyses of 535 hospitalized patients in Swedish showed significant associations between increased age and presence of pressure ulcers (17). Moreover, protracted bed rest of ICU patients declining patients’ mobility and therefore increases the risk for pressure ulcers (18).
We also found significant association between hemodialysis treatment and pressure ulcers prevalence, suggesting that patients that underwent hemodialysis were significantly more to present pressure ulcers. Possible explanations for this association could be that electrolyte balance disorder during hemodialysis as well as most ICU patients produce hemodynamic instability, which makes necessary the use of vasoconstriction drugs (inotropes) and thus, constitute a major risk factor for pressure ulcers development (19, 20). On the other hand, there are accumulating evidences suggesting that malnutrition has been associated with pressure ulcers development and their severity because of its negative impact on wound healing (21). Accordingly, decreased serum albumin levels have recently documented in seven out of eleven studies in accordance with the findings of systematic review (22). Also important, data of 34,238 hospital patients showed that patients with insufficient nutrition were 61% more likely to develop a pressure ulcer than those patients who did not have nutritional insufficiency. Evidently, correction of the serum albumin levels constitutes a key factor in pressure ulcers prevention and treatment (23, 24).
As expected we found strong association between hematocrit value and pressure ulcers development that has been previously reported in various studies (25, 26). Particularly, hematocrit values of less than 24% and hemoglobin values of less than 8.5 g/dL lead to insufficient tissue oxygenation, increasing the risk for pressure ulcers (27). Additionally, findings by study conducted in surgical ICU patients reported significant in hemoglobin value 48 hours prior to pressure ulcer development (OR=0.78) (28).
Despite the useful findings, our results have certain limitations that could be addressed. First, interpretation of the results may be limited because data were from a single institution. Secondly, we did not consider variability in severity of illness and thus, there may have been undiagnosed medical conditions such as neurosis and or anxiety disorders that might act as confounders in prevalence of the pressure ulcers. Third, use of a single study site also diminishes the generalizability of the study findings. However, the prospective design gives strength to this study and the statistical analysis is adequate.
5. CONCLUSIONS
In conclusion, specific clinical characteristics were studied are strongly and independently associated with increased likelihood of pressure ulcers developing, suggesting that this is a crucial incentive to consider these specific clinical characteristics as an important indicators in the evidence-based practice. The present study adds to an emerging pool of information regarding two newly developing areas of research, i.e. the epidemiology and clinical importance of pressure ulcers.
Acknowledgments
All authors would like to thanks all health professionals especially nursing and medical stuff employed in this specific ICU.
Footnotes
• Author Contributions: Conception and design: KT, MC and IVP; statistical analysis: KT; writing of the manuscript: KT, MC and CFK; interpretation of study findings and reviewing of the manuscript: ECF, LK and KT; final approval of the manuscript: KT, CFK, MC, ECF, LK and IVP.
• Funding: There was no specific funding for the current work.
• Conflict of interest: All authors declare that there is no financial or personal conflict of interest related to this paper.
REFERENCES
- 1.Lyder CH. Pressure ulcer prevention and management. JAMA: the Journal of the American Medical Association. 2003;289(2):223–6. doi: 10.1001/jama.289.2.223. [DOI] [PubMed] [Google Scholar]
- 2.Clark M, Bours G, Defloor T. Summary report on the prevalence of pressure ulcers. EPUAP Review. 2002;4:49–57. [Google Scholar]
- 3.Bouten CV, Oomens CW, Baaijens FP, Bader DL. The etiology of pressure ulcers: skin deep or muscle bound? Archives of physical medicine and rehabilitation. 2003;84(4):616–9. doi: 10.1053/apmr.2003.50038. [DOI] [PubMed] [Google Scholar]
- 4.Berlowitz DR, Brienza DM. Are all pressure ulcers the result of deep tissue injury? A review of the literature. Ostomy/wound managemen. 2007;53(10):34–8. [PubMed] [Google Scholar]
- 5.Jaul E, Menczel J. A comparative, descriptive study of systemic factors and survival in elderly patients with sacral pressure ulcers. Ostomy/wound management. 2015;61(3):20–6. [PubMed] [Google Scholar]
- 6.Cooper KL. Evidence-based prevention of pressure ulcers in the intensive care unit. Critical care nurse. 2013;33(6):57–66. doi: 10.4037/ccn2013985. [DOI] [PubMed] [Google Scholar]
- 7.Lyder CH, Wang Y, Metersky M, Curry M, Kliman R, Verzier NR, Hunt DR. Hospital-Acquired pressure ulcers: Results from the national medicare patient safety monitoring system study. Journal of the American Geriatrics Society. 2012;60(9):1603–8. doi: 10.1111/j.1532-5415.2012.04106.x. [DOI] [PubMed] [Google Scholar]
- 8.Lahmann NA, Kottner J, Dassen T, Tannen A. Higher pressure ulcer risk on intensive care? Comparison between general wards and intensive care units. Journal of clinical nursing. 2012;21(3-4):354–61. doi: 10.1111/j.1365-2702.2010.03550.x. [DOI] [PubMed] [Google Scholar]
- 9.Molon JND, Estrella EP. Pressure ulcer incidence and risk factors among hospitalized orthopedic patients: Results of a prospective cohort study. Ostomy Wound Management. 2011;57(10):64–9. [Google Scholar]
- 10.Shahin ES, Dassen T, Halfens RJ. Pressure ulcer prevalence and incidence in intensive care patients: a literature review. Nursing in critical care. 2008;13(2):71–9. doi: 10.1111/j.1478-5153.2007.00249.x. [DOI] [PubMed] [Google Scholar]
- 11.Apostolopoulou E, Tselebis A, Terzis K, Kamarinou E, Lambropoulos I, Kalliakmanis A. Pressure ulcer incidence and risk factors in ventilated intensive care patients. Health Science Journal. 2014;8(3):333–42. [Google Scholar]
- 12.Haesler E. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: quick reference guide. 1st ed. Perth, Australia: Cambridge Media; 2014. [Google Scholar]
- 13.Cubbin B, Jackson C. Trial of a pressure area risk calculator for intensive therapy patients. Intensive Care Nursing. 1991;7(1):40–4. doi: 10.1016/0266-612x(91)90032-m. [DOI] [PubMed] [Google Scholar]
- 14.Seongsook RJ, Ihnsook RJ, Younghee RL. Validity of pressure ulcer risk assessment scales;Cubbin and Jackson, Braden, and Douglas scale. International journal of nursing studies. 2004;41(2):199–204. doi: 10.1016/s0020-7489(03)00135-4. [DOI] [PubMed] [Google Scholar]
- 15.Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. Journal of evaluation in clinical practice. 2007;13(2):227–35. doi: 10.1111/j.1365-2753.2006.00684.x. [DOI] [PubMed] [Google Scholar]
- 16.Tayyib N, Coyer F, Lewis P. Saudi Arabian adult intensive care unit pressure ulcer incidence and risk factors: a prospective cohort study. International wound journal. 2015 doi: 10.1111/iwj.12406. doi:10.1111/iwj.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wann-Hansson C, Hagell P, Willman A. Risk factors and prevention among patients with hospital-acquired and pre-existing pressure ulcers in an acute care hospital. Journal of clinical nursing. 2008;17(13):1718–27. doi: 10.1111/j.1365-2702.2008.02286.x. [DOI] [PubMed] [Google Scholar]
- 18.Schoonhoven L, Grobbee DE, Donders AR, Algra A, Grypdonck MH, Bousema MT, Schrijvers AJ, Buskens E. Prediction of pressure ulcer development in hospitalized patients: a tool for risk assessment. Quality and safety in health care. 2006;15(1):65–70. doi: 10.1136/qshc.2005.015362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keller PB, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: a review of risks and prevention. Intensive care medicine. 2002;28(10):1379–88. doi: 10.1007/s00134-002-1487-z. [DOI] [PubMed] [Google Scholar]
- 20.Mathus-Vliegen EM. Old age, malnutrition, and pressure sores: an ill-fated alliance. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59(4):M355–M360. doi: 10.1093/gerona/59.4.m355. [DOI] [PubMed] [Google Scholar]
- 21.Iizaka S, Okuwa M, Sugama J, Sanada H. The impact of malnutrition and nutrition-related factors on the development and severity of pressure ulcers in older patients receiving home care. Clinical Nutrition. 2010;29(1):47–53. doi: 10.1016/j.clnu.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 22.Coleman S, Gorecki C, Nelson EA, Closs SJ, Defloor T, Halfens R, Farrin A, Brown J, Schoonhoven L, Nixon J. Patient risk factors for pressure ulcer development: systematic review. International journal of nursing studies. 2013;50(7):974–1003. doi: 10.1016/j.ijnurstu.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 23.Nonnemacher M, Stausberg J, Bartoszek G, Lottko B, Neuhaeuser M, Maier I. Predicting pressure ulcer risk: a multifactorial approach to assess risk factors in a large university hospital population. Journal of clinical nursing. 2009;18(1):99–107. doi: 10.1111/j.1365-2702.2008.02425.x. [DOI] [PubMed] [Google Scholar]
- 24.Sugino H, Hashimoto I, Tanaka Y, Ishida S, Abe Y, Nakanishi H. Relation between the serum albumin level and nutrition supply in patients with pressure ulcers: retrospective study in an acute care setting. The Journal of Medical Investigation. 2014;61(1.2):15–21. doi: 10.2152/jmi.61.15. [DOI] [PubMed] [Google Scholar]
- 25.Anthony D, Reynolds T, Russell L. The role of hospital acquired pressure ulcer in length of stay. Clinical Effectiveness in Nursing. 2004;8(1):4–10. [Google Scholar]
- 26.Compton F, Hoffmann F, Hortig T, Strauss M, Frey J, Zidek W, Schäfer JH. Pressure ulcer predictors in ICU patients: nursing skin assessment versus objective parameters. Journal of wound care. 2008;17(10):417–24. doi: 10.12968/jowc.2008.17.10.31304. [DOI] [PubMed] [Google Scholar]
- 27.Morison MJ, Van Rijswijk L. The epidemiology, the pathophysiology and etiology of pressure ulcers. In The prevention and treatment of pressure ulcers (ed MJ. Morison) New York: Mosby; 2001. pp. 7–35. [Google Scholar]
- 28.Nijs N, Toppets A, Defloor T, Bernaerts K, Milisen K, Van Den Berghe G. Incidence and risk factors for pressure ulcers in the intensive care unit. Journal of clinical nursing. 2009;18(9):1258–66. doi: 10.1111/j.1365-2702.2008.02554.x. [DOI] [PubMed] [Google Scholar]


