Abstract
Recent theories posit that empathy, typically an adaptive characteristic, may be associated with internalizing problems when children are chronically exposed to mother’s depression. We tested this postulation in a sample of children (N=82, Mage=5 years). Children witnessed their mothers express sadness, anger, and happiness during a simulated phone conversation, and researchers rated children’s negative affective empathy, positive affective empathy, and information-seeking (cognitive empathy) in response to their mother’s emotions. The chronicity of mother's depression during the child’s lifetime moderated associations between children’s empathy and internalizing problems. As predicted, all three empathy measures were related to greater mother-rated internalizing problems in children of chronically (i.e., 2–3 years) depressed mothers. Greater positive empathy was related to lower internalizing problems in children of nondepressed mothers. Positive empathy may contribute to adaptive processes when mothers are not depressed, and positive, negative, and cognitive empathy may contribute to maladaptive processes when mothers are chronically depressed.
Keywords: empathy, internalizing problems, maternal depression, guilt, emotional development
A child’s tendency to respond empathically to others is typically associated with adaptive functioning and social competence, including compassionate and prosocial behavior (1, 2), likeability and good quality peer relationships (1, 3), and strong academic outcomes (4). We propose that being highly empathic may not always be adaptive but rather might be associated with certain risks, specifically elevated internalizing problems, when the child is exposed to chronic negative emotions in their parents, including mother’s depression. Long-term exposure to mother’s depression has negative consequences for children’s social and emotional functioning (5, 6); in particular, exposure to mother’s depressed emotions is one mechanism through which risk for internalizing problems is transmitted (7, 8). Researchers have recently suggested that being acutely aware of and emotionally responsive to a mother’s depression may lead to children’s hypervigilance and guilt resulting from inability to alleviate the mother’s distress; hypervigilance and guilt may consequently lead to internalizing symptoms (9, 10). The purpose of this study is to begin evaluating these suppositions by determining whether empathic tendencies are associated with high levels of internalizing problems in young children whose mothers are depressed and, conversely, low internalizing problems in children whose mothers are not depressed.
Defining Empathy
Empathy is a multifarious construct that has varied definitions in the literature. Developmental psychologists have generally defined empathy as a response elicited by observing or imagining another’s emotional state or condition that involves the apprehension of their emotional state (cognitive empathy) and experience of emotions that are similar to what the other person is feeling or is assumed to feel (affective empathy; 9, 11). A large literature supports these related but distinct cognitive and affective components of empathy (12–14). From a developmental perspective, behavioral signs of affective empathy emerge earlier in development, with the first signs evident in the neonatal period (15, 16), and cognitive empathy does not begin to emerge until early childhood, when the cognitive capacity for taking another’s perspective begins to develop (17). Behavioral research indicates that a child’s proclivity to understand and take the perspectives of others does not necessarily predict the child’s tendency to share in others’ emotional experiences, and vice versa (9, 18). Neurobiological research also supports largely distinct neural substrates for “top-down” cognitive awareness and understanding of others’ emotions and “bottom-up” affective sharing (19–21), and the neural circuits underlying cognitive and affective components of empathy appear to follow different developmental trajectories (20, 22).
One manifestation of cognitive empathy is information-seeking, or attempts to understand another’s mental state and viewpoint (21, 23, 24). It is often operationalized as a child asking questions about others’ observable affect during observational paradigms (14, 25). Affective empathy refers to a child’s arousal and emotion sharing when observing another’s emotions. It is typically measured by rating a child’s facial expressions of concern or sympathy for persons in distress (11, 14). The existing research on children’s affective empathy has focused almost exclusively on their negative empathy, meaning their empathic responses to others’ emotional distress and physical pain (22, 26), whereas children’s positive empathy, meaning their experience of happiness or joy after witnessing and comprehending another’s positive emotional state (27), has been investigated in only a few studies. In one of these studies, parents’ reports of positive empathy in their 4-year-old children had small to moderate size associations with measures of negative empathy, supporting these two facets of affective empathy as related but distinct constructs. Furthermore, although negative and positive empathy have both been associated with children’s social functioning (27), negative empathy has most often been associated with measures of prosocial behaviors (28), including comforting distressed mothers (16), and the limited research on positive empathy supports its association with warmth during parent-child interactions, an association that was not found for negative empathy (1). Together, this research suggests distinct correlates of cognitive and affective empathy and that affective empathy can be further subdivided into related but separate positive and negative empathy components. The present study includes measures of all three facets of empathy.
Development of Skills for Empathic Responding
Early childhood, generally defined as the developmental stage between ages 3 and 8 years of age, is a key period for the development of skills for recognizing and discerning others’ emotions, hypothesizing about the causes of their emotions, and self-regulating during emotional situations (29, 30). Parental socialization practices, including responsive caregiving, displaying well-regulated emotions, labeling and explaining others’ emotions, and eliciting children’s dialogue about emotions, are primary means through which children learn these skills during early childhood (31, 32). By the middle of early childhood, children have typically developed skills that allow them to take the perspectives of others and respond empathically to others’ positive and negative emotions (33, 34), but ineffective socialization of these skills during this period interferes with children’s development of these skills (35). Thus, early childhood is a potentially vulnerable stage for the emergence of empathy-related risks, perhaps particularly as they relate to parental socialization.
Depression in Mothers
Depression is one of the most common psychiatric disorders in adults, particularly women (36), and women’s most impairing episodes of depression tend to occur during the childbearing and child rearing years (37). Children of depressed mothers are at risk for depression and impaired functioning in varied social and emotional domains (7). The effect of mother’s depression on children’s negative outcomes, including their internalizing problems, is greatest when her depression is chronic (38–40), and a meta-analysis found the effect of mother’s depression on children’s internalizing problems was stronger in samples with younger children (41). The effect of mother’s chronic depression on young children’s outcomes may be explained in part by her depression interfering with children’s development of empathy skills during early childhood. Researchers have found that, compared to nondepressed mothers, depressed mothers are less aware of their emotional impact on their child, less able to take the perspective of their child, and less effective in scaffolding their young child’s emotion regulation skills (42, 43). Furthermore, depressed mothers’ parenting is most impaired when her depression is chronic (44).
While parenting practices of mothers and fathers have been linked to children’s emotional development (45), studies indicate that mothers typically take a more central role in scaffolding young children's emotion understanding (46, 47) and mothers’ depression is more strongly associated with children’s internalizing problems than is fathers’ depression (41). Thus, this study focuses on empathic responses to mother’s emotions.
Empathic Responding and Internalizing Problems in Children of Depressed Mothers
Although empathy is typically an adaptive characteristic (1, 2), children who respond to their depressed mother’s emotions with high levels of empathic sensitivity may be particularly vulnerable to developing internalizing problems through overinvolvement in their parent’s emotions. Zahn-Waxler and Van Hulle (2012) proposed distinct pathways through which empathy can be adaptive or maladaptive. Positive parental socialization experiences, good self-regulation, and minimal environmental adversity are thought to facilitate an adaptive pathway whereby empathy arouses other-oriented concern that leads to prosocial action and positive psychosocial outcomes. Chronic exposure to a mother’s depression is proposed to contribute to a maladaptive pathway in which children’s empathic responses arouse anxiety, sadness, guilt, and self-blame cognitions and prompt “costly” altruistic behaviors (e.g., role reversal in which the child cares for the parent) that lead to internalizing problems.
Depressed mothers’ sadness, withdrawal, irritability, and anger are threatening to young children given their implications for impaired parenting and caregiving (7, 48, 49), and highly empathic children may be especially sensitive to their mother’s harsh and withdrawn parenting practices. Negative affective empathy and cognitive empathy are perhaps most obviously relevant to the maladaptive empathy pathways in children of depressed mothers. Tendencies to “take on” a depressed mother’s sadness and irritability may interfere with children’s development of effective emotion regulation skills, and children with these negative affective empathy tendencies may be prone to experiencing unregulated arousal, hypervigilance and self-distress in response to their mother’s depression. Children with tendencies toward cognitive empathy may habitually attempt to understand their mother’s emotions and the reasons for fluctuations in her emotions and may thus be prone to developing guilt and self-blame responses to her emotions. In this way, negative affective empathy and cognitive empathy may trigger maladaptive empathy pathways leading to internalizing problems.
Children who are keenly aware of and invested in their depressed mother’s happiness, which likely signals safety and that the mother is emotionally available to connect with the child, may also be vulnerable to developing internalizing problems. These children may be prone to perceiving their mother’s happiness as evidence that their comforting or caring behaviors toward their mother were effective. As such, positive empathy, through children’s overinvestment in and misplaced perceptions of responsibility for their mother’s happiness, may also contribute to maladaptive empathy pathways. Moreover, research on children’s emotional development suggests that children may be particularly attuned to positive emotions during early childhood. Studies have found that 3- to 5-year-old children discriminate happy faces almost as well as adults (29), 4- to 8-year-old children are more accurate in recognizing happy facial expressions than negative facial expressions (29, 50), and happy faces evoke stronger activation in emotion-processing areas of 3.5-to 8.5-year-old children’s brains than do angry and sad faces, a difference that is not observed in adults (51).
Despite these proposed empathy pathways, studies have yet to investigate whether young children’s empathic responses to their mother’s emotions are associated with internalizing problems in children of depressed mothers. Instead, researchers have focused on investigating whether young children of depressed and nondepressed mothers differ in empathy-related constructs, such as interpersonal sensitivity and guilt. Some studies have shown that, during early childhood, children of depressed and nondepressed mothers differ in their sensitivity toward others’ distress (52, 53). For example, Zahn-Waxler, Kochanska, Krupnick, and McKnew (1990) coded 5- to 9-year-old children’s responses to questions about hypothetical interpersonal vignettes and found that the responses produced by children of depressed mothers contained more extreme and unresolved guilt themes than the responses of children of nondepressed mothers; furthermore, researchers have found that excessive shame and guilt are characteristic of some young children with high levels of depression and internalizing problems (54, 55).
Hypothesis
We tested the central hypothesis that responding to mother’s emotions with high levels of cognitive, negative affective, and positive affective empathy is associated with low levels of internalizing problems when mothers have not experienced an episode of depression during the child’s lifetime, and, conversely, with high levels of internalizing problems when children are chronically exposed to their mother’s depression. We tested this hypothesis separately for cognitive, negative affective, and positive affective empathy given research supporting related but distinct cognitive and affective components of empathy (13) and because separate analyses will provide the most information about this novel research question.
Method
Participants
A sample of 82 children (52.4% female) and their mothers were recruited from a pool of families interested in participating in research, families who responded to fliers soliciting individuals interested in participating in studies about mother’s and child’s emotions that were posted in the community (e.g., libraries and schools) and in pediatric health clinics and adult behavioral health clinics at a large HMO, and families who responded to letters sent to families who had a child in the desired age range of 4 to 5 years who were patients in the pediatric health clinics or adult behavioral health clinics. Families were contacted by telephone to describe the study and schedule a laboratory visit. Participating children were 48 to 74 months (M=59.5, SD=6.3). One family visited the lab 3 months after the child turned 6 years old; all other children were between the ages of 4 and 5. Most (90.2%) of the mothers were married or living with a partner and most (93.2%) had at least an undergraduate college degree. The mean yearly income for the families was relatively high, with 63% of the families earning at least $100,000 per year (average of $145,000/year). Mothers identified that their children were primarily Caucasian (80.5%), and small percentages of children were African American (7.3%), Hispanic (3.7%), Asian (3.7%), biracial (3.7%), and other races (1.2%).
Simulated Emotional Phone Call
Children’s empathic responses to their mother’s emotions were observed while the mother pretended to have an emotional phone conversation with a friend using a procedure adapted from the Simulated Phone Argument Task (56). The mother and child sat alone in a room, and the child was asked to draw a picture while the mother received a telephone call from the researcher. An audio recording of emotional phrases was played over the phone, and the mother repeated the emotional phrases in the appropriate emotional tones. The telephone call had eight segments: four 40-second segments during which the mother expressed emotions and four 30-second “on-hold” segments that followed each of the emotion segments to provide opportunities for the child to interact with the mother. Mothers did not make scripted verbal statements about their emotions during the on-hold phases but maintained nonverbal behavior consistent with the preceding target emotion. They were instructed not to initiate communication with their child to avoid providing additional information about the phone call. If the child asked about the phone call, mothers were instructed to say something like, “I’ll tell you about it later.”
The mother first greeted her “friend” using a happy tone while saying five happy phrases, such as “I am happy to hear that.” She then told the child she was “on hold.” Next, she used a sad tone while making five sad statements, such as “that makes me so sad.” She then pretended to be on hold again. This procedure was repeated for mother's happiness a second time and then her anger. She ended the phone conversation using a neutral tone. An additional one-minute of interaction was recorded to provide an additional opportunity for the child to seek information about the mother’s emotions and the phone call. Mothers were instructed not to initiate conversation or to provide details of the phone call, similar to the on-hold phase, during the extra minute.
The duration of the phone conversation was four minutes and forty seconds, with mothers spending equal time expressing positive and negative emotions. The statements indicated the valence of mother's emotions but not the causes of her emotions to avoid inclusion of details that may have been particularly salient to individual children and to provide need for information-seeking. Mothers were instructed to use a level of emotional expressiveness they might typically use in a similar situation.
Observational Ratings of Emotions
Children's empathy responses
Affective and cognitive aspects of children’s empathic responses to their mother’s emotions were rated from video recordings that used a split screen to display both the mother and the child simultaneously. Three raters, who were blind to all information about the children and mothers, were trained to rate children’s empathic responses using rating scales that other researchers have used and found to be related to psychophysiological changes during empathy-inducing scenarios and parent ratings of children’s empathic tendencies (25, 57). Children’s expressions of negative emotions, including concern, sadness, and anger, in response to their mother’s sadness and anger were scored during the sad and angry segments and their subsequent on-hold segments. Ratings were based on facial expressions (e.g., frowning, tightening of brow), verbalizations, and gestures/postures (e.g., body rigidity, quickly shifting eyes) that were discerned to be in response to mother’s distress. Duration and intensity of the empathic concern expressions were rated on a 4-point scale (1 = absent, 2 = slight, 3 = moderate, 4 = substantial). Scores were averaged across the four segments to create one negative affective empathy score. Similar 4-point ratings of children’s expressions of happiness (e.g., smiling, livening of actions, animated hand gestures, singing) in response to mother’s happiness were made during the two happy segments and their subsequent on-hold segments, and the scores were averaged to create one positive affective empathy score.
Information-seeking (cognitive empathy) was measured through ratings of children’s observed attempts to learn more about their mother’s emotions, such verifying the mother’s emotional state and asking questions about the cause of mother’s emotions. Frequency and sophistication of children’s information-seeking behavior were rated on a 5-point scale (1 = none; 2 = gestures/nonverbal—e.g., looking at mother while she was talking and communicating through a shrug that they wanted to know what was being discussed on the phone; 3 = simple verbal; 4 = sophisticated verbal; 5 = repeated, varied attempts). One rating was made during each of the four emotion phases and four on-hold phases of the phone call and during the one-minute segment after the phone call. These nine information-seeking ratings were averaged to create one information-seeking (cognitive empathy) score. Initial inter-rater reliabilities were established on 13 participants for each rater, and observer drift reliabilities were calculated for 18 (20%) of the sample. As recommended by Hallgren (58), one-way, absolute, single measures intra-class correlations (ICC) were used and ranged from .74 to .96 (M = .83) for initial reliability and .66 to.86 (M = .78) for drift reliability, which are all in the good to excellent range for this index.
Mother’s observed emotional expressiveness
Mother’s emotional expressiveness during the phone call was rated to serve as a statistical control in analyses. Mother’s happiness during the two happy phases, sadness during the sad phase, and anger during the angry phase were rated by three additional, blind researchers using a using a 5-point rating scale (1 = flat affect; 2 = mild affect; 3 = moderate affect; 4 = clear/strong affect; 5 = extreme affect) that is similar to rating scales used by other researchers (57). Raters considered duration and intensity of facial affect, nonverbal behavior, and tone of voice. Initial reliabilities (ICCs) on 10 participants ranged from .81 to .91 (M = .86) across emotions and raters, and average drift reliabilities on 23 participants (25% of the sample) ranged from .83 to .92 (M = .88), indicating reliability in the excellent range.
Mother’s Diagnostic Interview
Sections of the Structured Clinical Interview for DSM-IV Axis I Disorders-Non-Patient Edition (SCID; 59) were administered to the mothers by a master’s level clinical psychologist who had extensive training on diagnosis of depression with the SCID. The Mood Episodes Module and Optional Module J were used to assess dates of onset and offset of each mood episode. The dates of onset and offset of each episode of major depressive disorder (MDD) and dysthymic disorder (DD) that met full DSM-IV criteria (i.e., depression episodes, DEs) and the child’s birthdate were used to calculate whether or not the mother met criteria for a DE during the child’s lifetime, the number of DEs the mother experienced during the child’s lifetime, and the duration (number of months) that children were exposed to their mother’s depression. A second blind rater reviewed notes from the interviews and calculated the three scores for 35% of the participants. Inter-rater reliabilities were calculated and yielded a Kappa’s coefficient of .92 for whether or not diagnostic criteria was met, an ICC of .85 for the number of episodes, and an ICC of .82 for the number of months during the child’s lifetime the mother was depressed.
Questionnaires
Child Behavior Checklist/4-18 (CBCL)
Mothers completed the parent version of the CBCL (60). The CBCL is a 118-item measure for children aged four to eighteen years that assesses the presence of symptoms of emotional and behavioral problems during the previous six months. The responses are given on a three-point scale (0 = Not True, 1 = Somewhat True, 2 = Very True) and yield scores on several empirically-derived scales. Standardized T scores for the 32-item Internalizing Problems scale, which assesses symptoms of depression, anxiety and inhibition, were used in this study. The CBCL has well-established reliability and validity in young children (60). The internal consistency reliability for the Internalizing Problems scale in our sample was α = .91.
Procedure
All procedures were approved by the IRB at Emory University and were performed in accordance with the ethical standards of Emory University and Georgia State University. All parents first provided informed written consent for their participation and their child’s participation, and all children provided their verbal assent. The mother then completed the CBCL and other study questionnaires while a researcher played with the child to build rapport. The mother then moved to a separate room to be trained on the phone call procedure, which included reading a script of the dialogue, listening to the audio recording of the phone conversation, and practicing the script. The mother then rejoined her child. The two sat at a table in a room that had one video camera recording the mother and another camera recording the child. The child was asked to draw a picture and did not have access to other toys. The researcher left the room, called the mother on her cell phone, and played the recording of the conversation over the phone. After the phone call, the mother completed the SCID interview in another room.
Results
Descriptive Analyses
Characteristics of the sample and variables are described in this section using means, standard deviations, Pearson’s zero-order correlations, t tests, and ANOVAs (See Table 1). Slightly more than half (56.1%) of the mothers never met criteria for a depressive disorder during their own lifetime; 9.8% of the mothers met criteria before but not during their participating child's lifetime; and 34.1% (n=28) met criteria during their child's lifetime. Mothers in the full sample (N=82) were depressed for an average of 7.10 months during their child's lifetime. Mothers who met criteria for a depression diagnosis during their child's lifetime (n=28) were depressed for an average of 20.79 months during their child's lifetime and had an average of 1.36 depression episodes (MDD and DD) during their child’s lifetime. The majority of mothers who met criteria for a DE during their child’s lifetime reported only one episode – 79% reported 1 DE, 7% reported 2 DEs, and 14% reported 3 DEs. The number of months depressed ranged from 1 to 67 for mothers who reported 1 DE and ranged from 4 to 70 for mothers who reported 2 or more DEs, suggesting that the number of episodes was rather arbitrary in terms of duration of children’s exposure.
Table 1.
Means, Standard Deviations, and Zero-Order Correlations between all Variables
| M | SD | Range | Correlations
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
|
|
|
|||||||||
| Mother Variables | ||||||||||
| 1. Depression Duration | 7.10 | 16.25 | 0 – 70 | |||||||
| 2. Sad Expressiveness | 3.51 | .84 | 2 – 5 | −.01 | ||||||
| 3. Angry Expressiveness | 3.51 | .69 | 2 – 5 | .12 | .48** | |||||
| 4. Happy Expressiveness | 3.39 | .64 | 2 – 5 | −.01 | .63** | .48** | ||||
| Child Variables | ||||||||||
| 5. Information-Seeking (Cognitive Empathy) | 1.98 | 0.57 | 1 – 3.33 | −.04 | .02 | −.07 | .18 | |||
| 6. Negative Affective Empathy | 1.75 | 0.57 | 1 – 3.20 | −.17 | −.01 | −.18 | −.04 | .55** | ||
| 7. Positive Affective Empathy | 1.63 | 0.55 | 1 – 3.40 | −.11 | .03 | .23* | .05 | .11 | .11 | |
| 8. Internalizing Problems | 48.33 | 10.39 | 29 – 76 | .30** | −.12 | −.29** | −.11 | −.01 | −.01 | −.07 |
Notes.
< .05,
< .01.
Table 2 presents means of study variables for mothers who met criteria for a depression diagnosis during their child’s lifetime and mothers who did not meet criteria for a depression diagnosis during their child’s lifetime and results of t tests for group differences between the means. The children of depressed mothers had significantly higher levels of internalizing problems than children of nondepressed mothers. The two groups did not differ significantly in any other study variable.
Table 2.
Means and Standard Deviations of Study Variables for Families of Mothers who were Depressed during her Child’s Lifetime and Families of Mothers who were not Depressed during her Child’s Lifetime
| Mother Depressed
|
Mother Not Depressed
|
t | p | |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Children’s CBCL Internalizing Problems | 53.25 (9.57) | 45.78 (9.94) | −3.27 | .002 |
| Mother’s Sad Expressiveness | 3.61 (0.69) | 3.46 (0.69) | −0.49 | .65 |
| Mother’s Angry Expressiveness | 3.57 (0.84) | 3.48 (0.84) | −0.90 | .37 |
| Mother’s Happy Expressiveness | 3.61 (0.69) | 3.38 (0.84) | −0.21 | .84 |
| Children’s Information-Seeking (Cognitive Empathy) | 1.94 (0.53) | 2.08 (0.60) | 0.55 | .59 |
| Children’s Negative Affective Empathy | 1.55 (0.50) | 1.78 (0.59) | 1.18 | .24 |
| Children’s Positive Affective Empathy | 1.72 (0.33) | 1.71 (0.64) | 0.51 | .61 |
Notes. “Mother Depressed” is coded as “1” and indicates the mother’s depression symptoms during her child’s lifetime met criteria for major depressive disorder or dysthymic disorder, and “Mother Not Depressed” is coded as “0” and indicates the mother’s symptoms did not meet criteria for a depression disorder during her child’s lifetime.
The paradigm and rating systems were effective in eliciting individual differences in children’s empathic responses. Ratings of children’s negative affective empathy spanned the full possible range of 1 to 4 in each of the relevant phases (i.e., the sad and angry phases and their subsequent on-hold phases) and within-person averages for negative affective empathy across the four phases ranged from 1.00 (absent) to 3.20 ( moderate). The sample mean for negative affective empathy was 1.75 ( slight; See Table 1). Ratings of children’s positive affective empathy also spanned the full range of 1 to 4 in each of the relevant phases (i.e., the two happy phases and their subsequent on-hold phases) and within-person averages for positive affective empathy across these four phases ranged from 1.00 (absent) to 3.40 ( moderate). The sample average for positive affective empathy was 1.63 ( slight). Ratings of children’s information-seeking (cognitive empathy) did not span the full range in all of the nine phases of the phone call; the ratings ranged from 1 (absent) to 3, 4, or 5 (M=4.44; sophisticated verbal) on the 5-point scale in the phases. Within-person averages across these nine phases ranged from 1 (none) to 3.33 (simple verbal), with a sample average of 1.98 ( gestures/nonverbal). The correlation between ratings of children’s information-seeking (cognitive empathy) and ratings of their negative affective empathy was significant, positive, and large in magnitude. Ratings of children’s positive affective empathy were not significantly correlated with negative affective empathy or information-seeking.
Ratings of mother’s observed sadness, anger, and happiness during the phone call ranged from 2 (mild affect) to 5 (extreme affect) with sample averages in the moderate affect to clear/strong affect range (See Table 1). Thus, all mothers expressed the targeted emotions, and, as expected given the instructions for the mothers to use a level of expressiveness that is typical for them, there was variability in the scores across the sample. Inter-correlations among ratings of mothers’ different emotions were moderate to strong, indicating that mothers who expressed one emotion strongly tended to express the other emotions strongly.
There were no significant gender differences in any study variables. Children's older age was significantly correlated with lower ratings of children’s negative empathy, r(82) = −.25, p=.03, and children’s positive empathy, r(82) = −.23, p=.04, but was not significantly related to any other study variable.
Tests of Hypotheses
Hierarchical multiple linear regression analyses were used to test the hypotheses using IBM® SPSS® Statistics, Version 21 software. Data were inspected for errors, outliers, and distributional assumptions; the assumptions of regression were met (61). The study hypothesis was tested with three separate regression equations – one each for cognitive empathy, negative affective empathy, and positive affective empathy. Internalizing problems was the outcome variable, and sample mean centered children’s empathy variables, mother’s depression duration, and the interaction between children’s empathy and mother’s depression duration were the predictor variables. Since skills for empathic responding develop and change across early childhood (29) and age was signifcantly associated with positive and negative empathy in our sample, children’s age was included as a covariate in the regression equations. Given the observed variability in ratings of mother’s expressiveness during the phone call, ratings of mother’s expressiveness during the phone call were also included as covariates. Specifically, ratings of mother’s happy expressiveness was used a covariate in the equation with children’s positive empathy as a predictor; ratings of mother’s sadness and anger were used in the equation with children’s negative empathy as a predictor; and ratings of mother’s sadness, anger, and happiness were used in the equation with children’s information-seeking (cognitive empathy) as a predictor.
Results for the regression models are presented in Table 3. As hypothesized, children’s internalizing problems were significantly predicted by interactions between the duration of mother's depression and (a) information-seeking cognitive empathy, (b) negative affective empathy, and (c) positive affective empathy, demonstrating that the strength and/or direction of the association between children's empathic responses to their mother’s emotions and their internalizing problems depends on their mother's depression duration. Tests of simple slopes were used to test associations between children’s empathic responding and internalizing problems when mothers were depressed for 0 months of her child’s lifetime (i.e., nondepressed mothers), 1 year (12 months) of the child’s lifetime, 2 years (24 months) of the child’s lifetime, and 3 years (36 months) of the child’s lifetime.
Table 3.
Parameters for Three Regression Equations Testing the Interactions between the Duration of Mother’s Depression during the Child’s Lifetime and Three Measures of Children’s Empathy Predicting Children’s Internalizing Problems
| Child’s Empathy Predictor
|
||||||
|---|---|---|---|---|---|---|
| Information Seeking (Cognitive Empathy)
|
Negative Affective Empathy
|
Positive Affective Empathy
|
||||
| ΔR2 | β | ΔR2 | β | ΔR2 | β | |
|
|
|
|
|
|||
| Step 1 | .05 | .05 | .02 | |||
| Age | −.08 | −.07 | −.05 | |||
| Mother’s Sad Expressiveness | −.04 | −.03 | − − | |||
| Mother’s Angry Expressiveness | −.20 | −.19 | -- | |||
| Mother’s Happy Expressiveness | .03 | -- | −.10 | |||
| Step 2 | .13** | .12** | .12** | |||
| Mother’s Depression Duration | .37** | .36** | .28* | |||
| Child’s Empathy | .01 | −.01 | −.17 | |||
| Step 3 | .05* | .05* | .09** | |||
| Mother’s Depression Duration x Child’s Empathy | .25* | .29* | .41** | |||
| Total R2 | .22** | .22** | .22** | |||
Notes. Gender (0=female, 1=male). Empathy variables, mother’s expressiveness variables, and age are sample mean centered.
< .05,
< .01.
Three separate regression equations were calculated, one for each of the three empathy predictors.
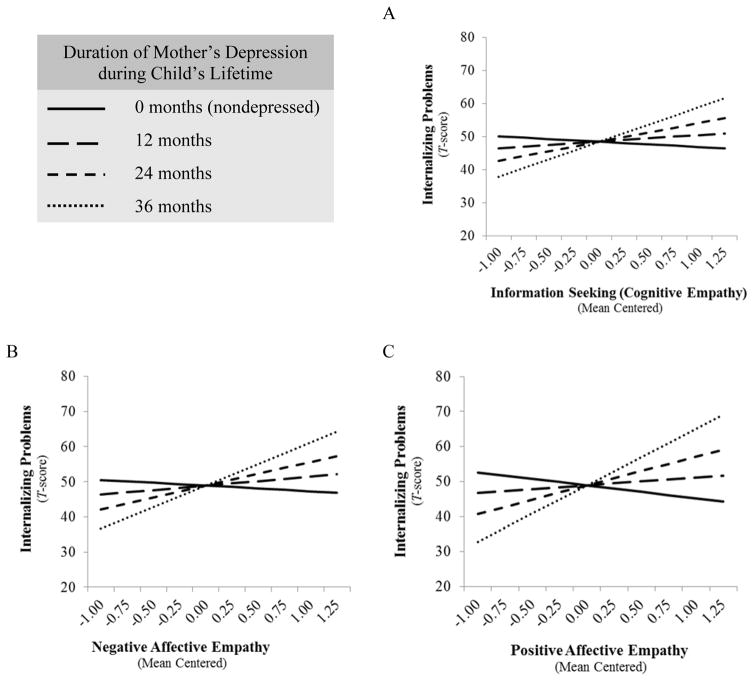
Information-seeking (cognitive empathy) was (1) positively but not significantly associated with internalizing problems in children whose mothers were depressed for 12 months during the child’s lifetime, β = .11, p = .36, (2) positively but not significantly associated with higher levels of internalizing problems in children whose mothers were depressed for 24 months during the child’s lifetime, β = .30, p = .09, (3) significantly associated with higher levels of internalizing problems in children whose mothers were depressed for 36 months during the child’s lifetime, β = .55, p = .047, and (4) negatively but not significantly associated with internalizing problems in children of nondepressed mothers, β = −.08, p = .47. See Figure 1, Panel A. Thus, as hypothesized, when mothers were chronically depressed, high levels of cognitive empathy in response to mother’s emotions were associated with higher levels of internalizing problems. Among children of mothers who were not clinically depressed during their mother’s lifetime, the association between children’s cognitive empathy and their internalizing problems was not significant but was in the expected direction in that higher cognitive empathy was associated with lower levels of internalizing problems.
Figure 1.
The effect of children's rated empathic behaviors during the simulated phone call – (A) information-seeking (cognitive empathy), (B) negative affective empathy, and (C) positive affective empathy – on children's CBCL internalizing problems score moderated by the duration of mother’s depression during children’s lifetime.
Children’s negative affective empathy was (1) again positively but not significantly associated with internalizing problems in children whose mothers were depressed for 12 months, β = .15, p = .25, (2) positively but not significantly associated with greater internalizing problems in children whose mothers were depressed for 24 months, β = .39, p = .06, (3) significantly associated with greater internalizing problems in children whose mothers were depressed for 36 months during their lifetime, β = .70, p = .04, and (4) negatively but not significantly associated with internalizing problems in children of nondepressed mothers, β = −.09, p = .42. See Figure 1, Panel B. Thus, similar to the findings for cognitive empathy, in children of chronically depressed mothers, higher levels of affective empathy in response to their mother’s negative emotions were associated with higher levels of internalizing problems. In children of mothers who were not clinically depressed during their mother’s lifetime, children’s negative affective empathy and their internalizing problems were not significantly associated but the association was again in the expected direction in that higher empathy was associated with lower internalizing problems.
Children’s positive affective empathy was (1) positively but not significantly associated with internalizing problems in children whose mothers were depressed for 12 months, β = .14, p = .36, (2) significantly associated with higher levels of internalizing problems in children whose mothers were depressed for 24 months, β = .51, p = .048, (3) significantly associated with higher levels of internalizing problems in children whose mothers were depressed for 36 months during their lifetime, β = .99, p = .02, and (4) significantly associated with lower levels of internalizing problems in children of nondepressed mothers, β = −.23, p = .04. See Figure 1, Panel C. Children’s affective empathy in response to mother’s happiness was thus significantly associated with internalizing problems in expected directions for both children of chronically depressed mothers and children of nondepressed mothers. That is, children who responded to mother’s displays of happiness with happy affect tended to have higher levels of internalizing problems if their mothers were chronically depressed and lower levels of internalizing problems if their mothers were not depressed.
Additional Analyses
Although we made no a priori predictions, we tested three-way interactions between the behavioral ratings of empathy (three z−score transformed ratings per participant), the number of months the mother was depressed, and the type of empathy (cognitive empathy, negative empathy, or positive empathy; positive empathy served as the reference group) to determine whether the interaction between children’s empathy and duration of exposure was significantly stronger for a particular type of empathy. The three-way interactions were not significant for cognitive empathy compared to positive affective empathy, β= −.15, p=.19, or negative affective empathy compared to positive affective empathy, β= −.10, p=.36, suggesting the hypothesized interaction effect did not differ significantly by type of empathy.
We also tested two additional indicators of children’s exposure to mother’s depression – whether or not mothers met criteria for a DE during the child’s lifetime and the number of mother’s DEs during the child’s lifetime – as moderators of the association between children’s empathy and their internalizing problems. Whether or not mothers met criteria for a DE did not interact significantly with any of the three types of empathy. The interaction between the number of mother’s DEs and children’s empathy was only significant for positive affective empathy, βInteraction=.34, p=.004. Children’s positive affective empathy was (a) significantly and positively associated with internalizing problems in children whose mothers experienced 2 or more DEs, β=.86, p=.02, (b) significantly and negatively associated with internalizing problems in children of mothers who experienced no DEs, β= −.29, p=.01, and (c) not significantly associated with internalizing problems in children whose mothers experienced 1 DE, β=.35, p=.09. Thus, the association between children’s empathic responses and their internalizing problems does not depend simply on whether or not the mothers were clinically depressed during the child’s lifetime and the number of DEs was only a significant moderator of mother’s positive affective empathy on children’s internalizing problems, suggesting that the duration of children’s exposure to mother’s depression is particularly important for understanding the conditions under which children’s empathy is a risk for internalizing problems.
Discussion
This study provided support for the novel hypothesis that empathic sensitivity is differentially associated with internalizing problems in children of chronically depressed mothers and children of nondepressed mothers. Displaying high levels of negative emotions in response to mother’s sadness and anger and seeking information about mother’s emotions were associated with higher levels of internalizing problems in children whose mothers were depressed for 3 years of the child’s lifetime, and responding to mother’s happiness with happiness was associated with higher levels of internalizing problems in children whose mothers were depressed for 2 or 3 years of the child’s lifetime. Conversely, high positive affective empathy in response to mother’s happiness was associated with lower levels of internalizing problems when mothers had not experienced an episode of depression during their child’s lifetime.
These findings support theoretical claims that empathic tendencies combined with family environments involving chronic parental suffering, such as mother’s depression, confer risk for internalizing problems in children, whereas children’s empathic tendencies facilitate adaptive processes that bring about social and emotional well-being in the context of positive, healthy family environments (9, 10). According to these theoretical models, high empathic sensitivity to mother’s negative emotions that interferes with children’s development of effective emotion regulation skills and activates maladaptive social cognitions, for example beliefs that the child is responsible for alleviating their mother’s distress, leads to a sense of personal failure, anxiety, and depression. These models also posit that children’s occasionally successful attempts to alleviate their mother’s negative emotions may reinforce children’s faulty and maladaptive beliefs that they have caused and are responsible for changing the parent’s depressed mood. Empathically sensitive children of depressed mothers may thus also be attuned and emotionally responsive to their mother’s happiness, particularly after their successful prosocial efforts, rendering them more vulnerable to such inaccurate beliefs of responsibility. Research on whether excessive prosocial efforts to alleviate mother’s depression, inappropriate guilt over failure to improve mother’s depressed mood, and disruptions in the development of emotion regulation strategies mediate associations between empathic sensitivity and internalizing problems in children of depressed mothers will be important aims for future research.
Another way to interpret our findings of associations in children of depressed mothers is that low empathic responding to mother’s emotions was associated with lower levels of internalizing problems in children of chronically depressed mothers, suggesting a potential benefit of disengaging from mother’s emotions when the mother is chronically depressed. Future research should examine whether, over time, low empathic responding to a depressed mother’s positive and negative emotions continues to be associated with low internalizing symptoms or progresses to detached mother-child relationships and subsequent deficits in interpersonal and emotional functioning.
Turning to children of nondepressed mothers, our finding that positive affective empathy in response to mother’s happiness was associated with low levels of internalizing problems supports an adaptive empathy pathway in these children and is consistent with research showing that empathic tendencies are related to a host of healthy psychosocial outcomes (1, 3, 4). These findings suggest that matching mother’s happy affect is a marker of emotional well-being in children of nondepressed mothers and may be a particularly adaptive way for these children to connect with their mothers. Indeed, children’s empathic engagement with others’ emotions facilitates their understanding of these emotions (62) and promotes prosocial behavior and strong interpersonal relationships (1, 63). Furthermore, positivity and warmth in the mother-child relationship has been found to buffer against the escalation of internalizing problems from early to late childhood (64). It is interesting to note that positive empathy is the one type of empathy that was related to internalizing problems in both children of depressed and nondepressed mothers, supporting the salience of mothers’ positive emotions to young children (50). Our findings about positive affective empathy make a novel contribution to a literature that has largely focused on relations between deficits in negative empathic responding and behavioral problems (65).
Findings from this study also provide a framework for novel investigations of empathy-related risk mechanisms more broadly. Future research on moderators of the association between high empathic sensitivity and internalizing problems in children will be important for clarifying the contexts in which empathic sensitivity functions as a risk factor. For example, studies might investigate the moderating role of other parenting practices, such as love withdrawal, guilt induction, and criticism (66), and children’s temperament, including poor effortful control (67), that may render children susceptible to develop empathy-related guilt and subsequent internalizing problems. Studies may also examine the moderating role of good self-regulation or the presence of an emotionally stable second parent, both of which may buffer risk for internalizing problems.
It is important to note that the children of depressed mothers and children of nondepressed mothers in our sample had, on average, similar levels of empathy across all empathy measures. Research on mean level differences in empathy between children of depressed mothers and children of never depressed mothers is mixed, with studies finding that children of depressed mothers demonstrate both lower (53) and higher levels of empathy (68) than children of nondepressed mothers. Even in the absence of mean level differences in empathy in our study, children’s empathy was differentially associated with internalizing problems depending on mother’s depression history, which lends support to models positing that high levels of empathy may function differently depending on aspects of the child’s emotional environment, such as chronic negative emotionality that characterizes depression (9). Mothers with and without depression also expressed equivalent levels of happy, sad and angry emotions during the paradigm, suggesting the findings were not driven by differences between the two groups in the salience of mother’s emotions and thus opportunities for empathic responding.
Limitations
Several limitations of the study should be discussed. First, levels of children’s internalizing problems were relatively low. However, lifetime rates of mother’s depression in this sample are relatively high compared to lifetime prevalence estimates in epidemiological samples (69), which may reflect that depression is particularly common in mothers of young children (70, 71) and our recruitment strategy (e.g., fliers in women’s behavioral health clinics and study description) likely appealed to families interested in the effect of mother’s emotions on children. Second, fathers were not included in the analyses and the sample was predominantly Caucasian and well educated. Future studies should include samples of children, mothers and fathers of diverse racial and socioeconomic backgrounds and with clinically significant symptoms to examine the generalizability of our findings in samples of differing characteristics. Third, some studies indicate that depressed parents provide negatively biased ratings of their children's behavioral and emotional problems (72, 73), though other studies do not support this (74, 75); studies using multi-informant measures of children’s internalizing problems may be an important extension of our findings. Fourth, recall bias may have affected mother’s report of her depression symptoms during her child’s lifetime. However, as expected, the number of months the mother was depressed had a significant, positive correlation with children’s internalizing problems, and it was a significant moderator of the association between empathy and internalizing problems. Lastly, the study used a cross-sectional design; future studies employing longitudinal designs with multiple time points might be used to answer questions about how relations among mother’s depression, children’s empathy, and children’s internalizing problems change over time, such as determining whether children’s high empathic sensitivity predisposes children to internalizing problems.
Summary
Empathic sensitivity, a characteristic typically associated with social and academic competence, was paradoxically associated with internalizing problems in children of chronically depressed mothers. Children’s attempts to seek information about their mother’s emotions (cognitive empathy), negative emotions in response to her sadness and anger (negative affective empathy), and positive emotions in response to her happiness (positive affective empathy) were associated with higher levels of internalizing problems in children whose mothers were depressed for at least several years during the child’s lifetime. Conversely, children’s positive empathy was associated with lower levels of internalizing problems in children whose mothers were not depressed.
Acknowledgments
We would like to thank the families who participated in the study and the many research assistants who assisted with data collection and coding.
Research reported in this publication was supported by the National Institute of Mental Health under award number F31 MH 072095. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors report no conflict of interest.
References
- 1.Zhou Q, Eisenberg N, Losoya SH, Fabes RA, Reiser M, Guthrie IK, et al. The relations of parental warmth and positive expressiveness to children's empathy-related responding and social functioning: A longitudinal study. Child Dev. 2002;3:893–915. doi: 10.1111/1467-8624.00446. [DOI] [PubMed] [Google Scholar]
- 2.Findlay LC, Girardi A, Coplan RJ. Links between empathy, social behavior, and social understanding in early childhood. Early Childhood Research Quarterly. 2006;3:347–359. [Google Scholar]
- 3.Denham SA, McKinley M, Couchoud EA, Holt R. Emotional and behavioral predictors of preschool peer ratings. Child Dev. 1990;4:1145–1152. [PubMed] [Google Scholar]
- 4.Spinrad TL, Eisenberg N. Empathy, prosocial behavior, and positive development in schools. In: Gilman R, Huebner ES, Furlong MJ, editors. Handbook of positive psychology in schools. New York, NY US: Routledge/Taylor & Francis Group; 2009. pp. 119–129. [Google Scholar]
- 5.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clin Child Fam Psychol Rev. 2011;1:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 6.Katz SJ, Hammen CL, Brennan PA. Maternal depression and the intergenerational transmission of relational impairment. J Fam Psychol. 2013;1:86–95. doi: 10.1037/a0031411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodman SH, Tully E. Children of depressed mothers: Implications for the etiology, treatment, and prevention of depression in children and adolescents. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York, NY US: Guilford Press; 2008. pp. 415–440. [Google Scholar]
- 8.Tully EC, Iacono WG, McGue M. An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. The American Journal of Psychiatry. 2008;9:1148–1154. doi: 10.1176/appi.ajp.2008.07091438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tone EB, Tully EC. Empathy as a 'risky strength': A multilevel examination of empathy and risk for internalizing disorders. Dev Psychopathol. 2014;4(Pt 2):1547–1565. doi: 10.1017/S0954579414001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zahn-Waxler C, Van Hulle C. Empathy, guilt, and depression: When caring for others becomes costly to children. In: Oakley B, Knafo A, Madhavan G, et al., editors. Pathological altruism. New York, NY US: Oxford University Press; 2012. pp. 321–344. [Google Scholar]
- 11.Eisenberg N, Fabes RA. Prosocial development. In: Eisenberg N, editor. Handbook of child psychology, 5th ed.: Vol 3. Social, emotional, and personality development. Hoboken, NJ, US: John Wiley & Sons Inc; 1998. pp. 701–778. [Google Scholar]
- 12.Decety J. A social cognitive neuroscience model of human empathy. In: Harmon-Jones E, Winkielman P, editors. Social neuroscience: Integrating biological and psychological explanations of social behavior. New York, NY US: Guilford Press; 2007. pp. 246–270. [Google Scholar]
- 13.Dadds MR, Hunter K, Hawes DJ, Frost ADJ, Vassallo S, Bunn P, et al. A measure of cognitive and affective empathy in children using parent ratings. Child Psychiatry Hum Dev. 2008;2:111–122. doi: 10.1007/s10578-007-0075-4. [DOI] [PubMed] [Google Scholar]
- 14.Knafo A, Zahn-Waxler C, Davidov M, Hulle CV, Robinson JL, Rhee SH. Empathy in early childhood: Genetic, environmental, and affective contributions. In: Vilarroya O, Altran S, Navarro A, et al., editors. Values, empathy, and fairness across social barriers. New York, NY US: New York Academy of Sciences; 2009. pp. 103–114. [DOI] [PubMed] [Google Scholar]
- 15.Diego MA, Jones NA. Neonatal antecedents for empathy. In: Farrow T, Woodruff P, editors. Empathy in mental illness. New York, NY US: Cambridge University Press; 2007. pp. 145–167. [Google Scholar]
- 16.Roth-Hanania R, Davidov M, Zahn-Waxler C. Empathy development from 8 to 16 months: Early signs of concern for others. Infant Behavior & Development. 2011;3:447–458. doi: 10.1016/j.infbeh.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 17.Schwenck C, Göhle B, Hauf J, Warnke A, Freitag CM, Schneider W. Cognitive and emotional empathy in typically developing children: The influence of age, gender, and intelligence. European Journal of Developmental Psychology. 2014;1:63–76. [Google Scholar]
- 18.Belacchi C, Farina E. Feeling and thinking of others: Affective and cognitive empathy and emotion comprehension in prosocial/hostile preschoolers. Aggressive Behavior. 2012;2:150–165. doi: 10.1002/ab.21415. [DOI] [PubMed] [Google Scholar]
- 19.Decety J. Dissecting the neural mechanisms mediating empathy. Emotion Review. 2011;1:92–108. [Google Scholar]
- 20.Decety J. The neurodevelopment of empathy in humans. Dev Neurosci. 2010;4:257–267. doi: 10.1159/000317771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shamay-Tsoory SG, Aharon-Peretz J, Perry D. Two systems for empathy: A double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain: A Journal of Neurology. 2009;3:617–627. doi: 10.1093/brain/awn279. [DOI] [PubMed] [Google Scholar]
- 22.Decety J, Michalska KJ. Neurodevelopmental changes in the circuits underlying empathy and sympathy from childhood to adulthood. Developmental Science. 2010;6:886–899. doi: 10.1111/j.1467-7687.2009.00940.x. [DOI] [PubMed] [Google Scholar]
- 23.Davis MH. The effects of dispositional empathy on emotional reactions and helping: A multidimensional approach. J Pers. 1983;2:167–184. [Google Scholar]
- 24.Ickes W, Stinson L, Bissonnette V, Garcia S. Naturalistic social cognition: Empathic accuracy in mixed-sex dyads. J Pers Soc Psychol. 1990;4:730–742. [Google Scholar]
- 25.Zahn-Waxler C, Cole PM, Welsh JD, Fox NA. Psychophysiological correlates of empathy and prosocial behaviors in preschool children with behavior problems. Dev Psychopathol. 1995;1:27–48. [Google Scholar]
- 26.Liew J, Eisenberg N, Spinrad TL, Eggum ND, Haugen RG, Kupfer A, et al. Physiological regulation and fearfulness as predictors of young children's empathy-related reactions. Social Development. 2011;1:111–134. doi: 10.1111/j.1467-9507.2010.00575.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sallquist J, Eisenberg N, Spinrad TL, Eggum ND, Gaertner BM. Assessment of preschoolers' positive empathy: Concurrent and longitudinal relations with positive emotion, social competence, and sympathy. The Journal of Positive Psychology. 2009;3:223–233. doi: 10.1080/17439760902819444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eisenberg N. Prosocial behavior. In: Bear GG, Minke KM, editors. Children's needs iii: Development, prevention, and intervention. Washington, DC US: National Association of School Psychologists; 2006. pp. 313–324. [Google Scholar]
- 29.Durand K, Gallay M, Seigneuric A, Robichon F, Baudouin J-Y. The development of facial emotion recognition: The role of configural information. J Exp Child Psychol. 2007;1:14–27. doi: 10.1016/j.jecp.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Calkins SD, Marcovitch S. Emotion regulation and executive functioning in early development: Integrated mechanisms of control supporting adaptive functioning. In: Calkins SD, Bell MA, editors. Child development at the intersection of emotion and cognition. Washington, DC US: American Psychological Association; 2010. pp. 37–57. [Google Scholar]
- 31.Brophy-Herb HE, Schiffman RF, Bocknek EL, Dupuis SB, Fitzgerald HE, Horodynski M, et al. Toddlers' social-emotional competence in the contexts of maternal emotion socialization and contingent responsiveness in a low-income sample. Social Development. 2011;1:73–92. [Google Scholar]
- 32.Cole PM, Dennis TA, Smith-Simon KE, Cohen LH. Preschoolers' emotion regulation strategy understanding: Relations with emotion socialization and child self-regulation. Social Development. 2009;2:324–352. [Google Scholar]
- 33.Bengtsson H, Arvidsson Å. The impact of developing social perspective-taking skills on emotionality in middle and late childhood. Social Development. 2011;2:353–375. [Google Scholar]
- 34.Eisenberg N. Empathy-related responding: Links with self-regulation, moral judgment, and moral behavior. In: Mikulincer M, Shaver PR, editors. Prosocial motives, emotions, and behavior: The better angels of our nature. Washington, DC, US: American Psychological Association; 2010. pp. 129–148. [Google Scholar]
- 35.Thompson RA, Meyer S. Socialization of emotion regulation in the family. In: Gross JJ, editor. Handbook of emotion regulation. New York, NY US: Guilford Press; 2007. pp. 249–268. [Google Scholar]
- 36.Kessler RC. The epidemiology of depression among women. In: Keyes CLM, Goodman SH, Keyes CLM, et al., editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York, NY, US: Cambridge University Press; 2006. pp. 22–37. [Google Scholar]
- 37.Wilhelm K. Depression: From nosology to global burden. In: Keyes CLM, Goodman SH, Keyes CLM, et al., editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York, NY, US: Cambridge University Press; 2006. pp. 3–21. [Google Scholar]
- 38.Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry. 2003;3:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- 39.Brennan PA, Hammen C, Andersen MJ, Bor W, Najman JM, Williams GM. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Dev Psychol. 2000;6:759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- 40.Sohr-Preston SL, Scaramella LV. Implications of timing of maternal depressive symptoms for early cognitive and language development. Clin Child Fam Psychol Rev. 2006;1:65–83. doi: 10.1007/s10567-006-0004-2. [DOI] [PubMed] [Google Scholar]
- 41.Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children's internalizing and externalizing behavior problems: A meta-analysis. Psychol Bull. 2002;5:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- 42.Coyne LW, Low CM, Miller AL, Seifer R, Dickstein S. Mothers' empathic understanding of their toddlers: Associations with maternal depression and sensitivity. Journal of Child and Family Studies. 2007;4:483–497. [Google Scholar]
- 43.Hoffman C, Crnic KA, Baker JK. Maternal depression and parenting: Implications for children's emergent emotion regulation and behavioral functioning. Parenting: Science and Practice. 2006;4:271–295. [Google Scholar]
- 44.NICHD Early Child Care Research Network in the reference list. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Dev Psychol. 1999;5:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 45.Denham SA, Workman E, Cole PM, Weissbrod C, Kendziora KT, Zahn-Waxler C. Prediction of externalizing behavior problems from early to middle childhood: The role of parental socialization and emotion expression. Dev Psychopathol. 2000;1:23–45. doi: 10.1017/s0954579400001024. [DOI] [PubMed] [Google Scholar]
- 46.Hastings PD, Rubin KH, DeRose L. Links among gender, inhibition, and parental socialization in the development of prosocial behavior. Merrill-Palmer Quarterly: Journal of Developmental Psychology. 2005;4:467–493. [Google Scholar]
- 47.Denham SA, Kochanoff AT. Parental contributions to preschoolers' understanding of emotion. Marriage & Family Review. 2002;3–4:311–343. [Google Scholar]
- 48.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;3:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 49.Lovejoy M, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clin Psychol Rev. 2000;5:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 50.Herba CM, Phillips M. Annotation: Development of facial expression recognition from childhood to adolescence: Behavioural and neurological perspectives. Journal of Child Psychology and Psychiatry. 2004;7:1185–1198. doi: 10.1111/j.1469-7610.2004.00316.x. [DOI] [PubMed] [Google Scholar]
- 51.Todd RM, Evans JW, Morris D, Lewis MD, Taylor MJ. The changing face of emotion: Age-related patterns of amygdala activation to salient faces. Soc Cogn Affect Neurosci. 2011;1:12–23. doi: 10.1093/scan/nsq007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zahn-Waxler C, Cummings EM, McKnew DH, Radke-Yarrow M. Altruism, aggression, and social interactions in young children with a manic-depressive parent. Child Dev. 1984;1:112–122. [PubMed] [Google Scholar]
- 53.Apter-Levy Y, Feldman M, Vakart A, Ebstein RP, Feldman R. Impact of maternal depression across the first 6 years of life on the child’s mental health, social engagement, and empathy: The moderating role of oxytocin. The American Journal of Psychiatry. 2013;10:1161–1168. doi: 10.1176/appi.ajp.2013.12121597. [DOI] [PubMed] [Google Scholar]
- 54.Luby J, Belden A, Sullivan J, Hayen R, McCadney A, Spitznagel E. Shame and guilt in preschool depression: Evidence for elevations in self-conscious emotions in depression as early as age 3. Journal of Child Psychology and Psychiatry. 2009;9:1156–1166. doi: 10.1111/j.1469-7610.2009.02077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cornell AH, Frick PJ. The moderating effects of parenting styles in the association between behavioral inhibition and parent-reported guilt and empathy in preschool children. J Clin Child Adolesc Psychol. 2007;3:305–318. doi: 10.1080/15374410701444181. [DOI] [PubMed] [Google Scholar]
- 56.Davies PT, Cummings EM, Winter MA. Pathways between profiles of family functioning, child security in the interparental subsystem, and child psychological problems. Dev Psychopathol. 2004;3:525–550. doi: 10.1017/s0954579404004651. [DOI] [PubMed] [Google Scholar]
- 57.Eisenberg N, Fabes RA, Bustamante D, Mathy RM, Miller PA, Lindholm E. Differentiation of vicariously induced emotional reactions in children. Dev Psychol. 1988;2:237–246. [Google Scholar]
- 58.Hallgren KA. Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantitative Methods for Psychology. 2012;1:23–34. doi: 10.20982/tqmp.08.1.p023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for dsm-iv-tr axis i disorders, research version, non-patient edition (scid-i/np) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 60.Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: Author; 1991. [Google Scholar]
- 61.Tabachnick BG, Fidell LS. Using multivariate statistics. 6. Boston: Pearson; 2013. [Google Scholar]
- 62.Tully EC, Donohue MR, Garcia SE. Children's empathy responses and their understanding of mother's emotions. Cognition and Emotion. 2015;1:118–129. doi: 10.1080/02699931.2014.898614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eisenberg N, Eggum ND. Empathy-related and prosocial responding: Conceptions and correlates during development. In: Sullivan BA, Snyder M, Sullivan JL, editors. Cooperation: The political psychology of effective human interaction. Malden: Blackwell Publishing; 2008. pp. 53–74. [Google Scholar]
- 64.Brock RL, Kochanska G. Decline in the quality of family relationships predicts escalation in children’s internalizing symptoms from middle to late childhood. J Abnorm Child Psychol. 2015 doi: 10.1007/s10802-015-0008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hughes C, White A, Sharpen J, Dunn J. Antisocial, angry, and unsympathetic: 'Hard-to-manage' preschoolers' peer problems and possible cognitive influences. Journal of Child Psychology and Psychiatry. 2000;2:169–179. [PubMed] [Google Scholar]
- 66.Donatelli J-AL, Bybee JA, Buka SL. What do mothers make adolescents feel guilty about? Incidents, reactions, and relation to depression. Journal of Child and Family Studies. 2007;6:859–875. [Google Scholar]
- 67.Liang Z-b, Zhang G-z, Chen H-c. Relation of children's temperament and parenting style with children's conscience. Chinese Journal of Clinical Psychology. 2009;1:90–92. [Google Scholar]
- 68.Zahn-Waxler C, Kochanska G. The origins of guilt. In: Thompson RA, Lincoln NE, editors. Nebraska symposium on motivation, 1988: Socioemotional development. US: University of Nebraska Press; 1990. pp. 183–258. [PubMed] [Google Scholar]
- 69.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (ncs-r) JAMA: Journal of the American Medical Association. 2003;23:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 70.Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, Carter AS, Horwitz SM, Briggs-Gowan MJ, et al. Prevalence, correlates, and persistence of maternal depression. J Womens Health. 2007;5:678–691. doi: 10.1089/jwh.2006.0185. [DOI] [PubMed] [Google Scholar]
- 71.McLennan JD, Kotelchuck M, Cho H. Prevalence, persistence, and correlates of depressive symptoms in a national sample of mothers of toddlers. J Am Acad Child Adolesc Psychiatry. 2001;11:1316–1323. doi: 10.1097/00004583-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 72.Najman JM, Williams GM, Nikles J, Spence S, Bor W, O'Callaghan M, et al. Mothers' mental illness and child behavior problems: Cause–effect association or observation bias? J Am Acad Child Adolesc Psychiatry. 2000;5:592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- 73.Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychol Bull. 1992;3:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- 74.Weissman MM, Wickramaratne P, Warner V, John K. Assessing psychiatric disorders in children: Discrepancies between mothers' and children's reports. Arch Gen Psychiatry. 1987;8:747–753. doi: 10.1001/archpsyc.1987.01800200075011. [DOI] [PubMed] [Google Scholar]
- 75.Conrad M, Hammen C. Role of maternal depression in perceptions of child maladjustment. J Consult Clin Psychol. 1989;5:663–667. doi: 10.1037//0022-006x.57.5.663. [DOI] [PubMed] [Google Scholar]