Abstract
Introduction
Deaf American Sign Language-users (ASL) have limited access to cancer genetics information they can readily understand, increasing risk for health disparities. We compared effectiveness of online cancer genetics information presented using a bilingual approach (ASL with English closed captioning) and a monolingual approach (English text).
Hypothesis
Bilingual modality would increase cancer genetics knowledge and confidence to create a family tree; education would interact with modality.
Methods
We used a block 2:1 randomized pre-post study design stratified on education. 150 Deaf ASL-users ≥18 years old with computer and internet access participated online; 100 (70 high, 30 low education) and 50 (35 high, 15 low education) were randomized to the bilingual and monolingual modalities. Modalities provide virtually identical content on creating a family tree, using the family tree to identify inherited cancer risk factors, understanding how cancer predisposition can be inherited, and the role of genetic counseling and testing for prevention or treatment. 25 True/False items assessed knowledge; a Likert scale item assessed confidence. Data were collected within 2 weeks before and after viewing the information.
Results
Significant interaction of language modality, education, and change in knowledge scores was observed (p=.01). High education group increased knowledge regardless of modality (Bilingual: p<.001; d=.56; Monolingual: p<.001; d=1.08). Low education group increased knowledge with bilingual (p<.001; d=.85), but not monolingual (p=.79; d=.08) modality. Bilingual modality yielded greater confidence creating a family tree (p=.03).
Conclusions
Bilingual approach provides a better opportunity for lower educated Deaf ASL-users to access cancer genetics information than a monolingual approach.
Keywords: health disparities, health education, genetic counseling, sign language, deaf
INTRODUCTION
Cancer disparities are widening among subpopulations differing by literacy level, race/ethnicity, language, and other characteristics (1), underscoring the need for culturally and linguistically appropriate cancer health communications. One subpopulation in need of appropriate cancer health communications is the US Deaf community (2), for whom American Sign Language (ASL) is the primary language. General information about some cancers exists for this community (2-8). However, up to 10% of cancers occur due to a genetic alteration in a high risk gene, which increases the chance of developing cancer and can affect medical management(9) in ways that could lead to cancer screening (10-12) and prevention (13, 14). Access to cancer genetics education is important because it increases genetics knowledge and understanding of factors involved in assessing risk for cancer and possible options (15, 16). However, no materials exist for Deaf ASL-users on this topic although, in the absence of research, there is no expectation that the prevalence of cancers with a strong genetic component differs between deaf and hearing populations. This study addresses the need for appropriate cancer genetics healthcare information for the Deaf community.
Health information in spoken or print English does not satisfactorily address Deaf ASL-users needs. Language acquisition background for deaf individuals is varied (17), and as a result, their English reading comprehension level tends to be lower on average (18, 19) than the average 7th-8th grade reading level in the general US population(20). Moreover, most health information is written at even higher grade levels (1) and without attention to cultural aspects of the Deaf community, a particularly important deficit when addressing the sensitive topic of genetics (21-24).
Increasing awareness of the need for effective access to health information has led to development of cancer prevention educational programs for the Deaf community. Though none have addressed genetic predispositions, efforts that address language-concordance by accounting for ASL as the first language for many deaf individuals have been found to increase their knowledge regarding a variety of cancers (3-8, 25, 26) and to promote cancer screening behaviors (6). Although conveying health information in ASL is key, these efforts also have included visual images and graphics and English language elements such as captioning or English text. These elements take into account the considerable linguistic variation in the Deaf community, ranging from use of ASL to more English-ordered signed form, and that many deaf people routinely communicate using a bilingual approach and visual modality (27). A bilingual approach allows for ASL information provision and inclusion of English medical terminology using text and fingerspelling, which can facilitate understanding and later information recall (28-30).
Though a bilingual approach is important, education level has not adequately been taken into account in the design of health information for the Deaf community. This is a significant oversight because education level, English reading literacy, and ASL proficiency are interrelated (19, 31, 32), suggesting that a more nuanced approach is needed. Since the 2013 American Community Survey1 found that ~50% of the US population with a hearing disability (defined as “person is deaf or has serious difficulty hearing”) aged 21-64 has high school or less education (33), the absence of education level in tailoring health information may result in a failure to identify and address the health education needs of a significant proportion of this population, likely the Deaf community members at greatest risk for lacking adequate health knowledge.
This randomized study compares the effectiveness of cancer genetics information presented in two modalities, a bilingual ASL with English closed captioning modality and a monolingual English text modality. We hypothesized that ASL-using Deaf adults randomly assigned to the bilingual modality would show greater knowledge gains compared with those randomized to the monolingual modality. We further hypothesized that education level would significantly interact with language modality.
METHODS
A parallel 2:1 randomized controlled study design was used, with education as a stratification factor. Before study enrollment began, the statistician prepared a block randomization scheme via excel macro where participant assignments were made within an education level by sampling from a randomly allocated block of size 3 to 15 without replacement. The routine masked block size and upcoming assignments from the study coordinator who implemented it. The statistician was blinded to subject assignment. Low education was defined as high school diploma or less education; high education as some college or more education.
Study Sample
Inclusion criteria were: ≥18 years, deaf or hard-of-hearing (by self-report), ASL-user, and computer and internet access. Individuals unable to complete an online ASL Grammar Judgment Task-Revised (TGJASL-R, a measure of ASL syntactic competency) (34, 35) within one week were excluded, serving as an additional mechanism to determine if a participant had access to a computer and the internet and was sufficiently computer literate to take part in the study.
Participants were recruited nationally, November 2013-May 2014, via deaf clubs, organizations, community events, and a previous genetic counseling and testing study (36). Recruitment materials described an online study focused on learning about family health history and were disseminated in ASL or English text via study website (deafgeneticsproject.org), Facebook, video blogs, and advertisements.
After initial eligibility determination, prospective participants received a link to the TGJASL-R assessment. Those who completed this assessment within one week were randomized, regardless of their TGJASL score, to receive either the intervention [bilingual modality] or the control [monolingual modality] materials. Blinded to study group assignment, participants had two weeks to complete an online pre-test survey assessing demographic, primary and secondary outcome variables. They then received a link to the intervention or control educational materials. After viewing the assigned materials, participants had two weeks to complete the online post-test survey. All demographic, pre-test, and post-test surveys items were translated into ASL using a translation-back translation procedure (37, 38) and provided by video along with English text. Individuals completed the study online at a location of their choosing and received a $40 gift card upon completion. If an individual did not have a computer, but lived in Los Angeles, arrangements were made to meet with the study coordinator in a public place where a study laptop was provided. Follow-up was completed in June 2014. This study was approved with waiver of written consent by the institutional review boards at the University of California, Los Angeles and Gallaudet University, in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Conditions
Intervention [Bilingual modality]: ASL with closed captioning
Content and format were developed with feedback from Deaf individuals and study consultants using focus groups, pilot testing, and individual comments. The material was designed to encourage a proactive approach to understanding, documenting, and analyzing one's family health history, and is organized into six modules (videos; available at aslcancergenetics.org). The “Introduction” explains that although the focus is on hereditary breast, ovarian, uterine, and colon cancers, the information provided is applicable to other hereditary diseases. The remainder is delivered as a storytelling narrative, where viewers are introduced to Anna, a fictional character concerned about her risk for inherited breast cancer. The viewer learns more about basic cancer genetic concepts, while following Anna as she ascertains her cancer risk. For example, Anna creates her family tree in the module titled “Creating a Family Tree,” which explains how to document family health history. The module “Risk Factors for Inherited Cancer” identifies what to look for in a family tree that would suggest risk for genetic predisposition to cancer; “How Cancer is Inherited” focuses on genes and autosomal dominant inheritance of predisposition to cancer; “Role of Genetic Counseling and Testing” explains genetic counseling and testing, including the purpose, benefits, and possible outcomes of genetic testing for cancer predisposition; the “Review” module briefly reviews the previous modules. Two to four quiz items are included in four of the modules.
An ASL-specific narrative discourse delivered by a Deaf, male, native signer is the main presentation strategy. In this style, a narrator visually presents information using space, head movements, eye gaze, facial expression, and body position (39). Visual aids, text, and closed captioning supported the ASL discourse. Graphics appear to the narrator's right or at full screen. Closed captioning is placed at the bottom of the screen and is turned on (default), with option to turn off. Quizzes, three different camera angles, and multi-sequence editing were used to keep the audience visually engaged (40). Total video running time is 37.3 minutes.
Control [Monolingual modality]: English text
The monolingual modality provides information in written English and features the same six modules, quizzes, and graphics used in the bilingual modality (available at aslcancergenetics.org). The English text was developed from the bilingual modality's closed captioning text. Because word-for-word translation from ASL to English is not possible, the text was modified to fit a stand-alone English text format. To facilitate computer screen reading, information was provided in small segments (41) of 1-7 short paragraphs and no more than one graphic per page. This resulted in 38 short, simple, web pages. Assuming 200 words per minute reading speed for an average reader at 6th-7th grade level (42), expected viewing time is 19.0 minutes. The text's Flesch-Kincaid (FK) grade level (43) is 6.8; and the FK reading ease score (44) is 64.8, considered standard English level and estimated at 7th-8th grade level (45).
Measures
Primary Outcome
Twenty-five true/false items assessed knowledge of cancer genetics (17 items) and genetic counseling (8 items) (Appendix Table A). Currently, no validated cancer genetics knowledge survey is available in ASL. Therefore, we used items from existing cancer genetics knowledge questionnaires (46, 47) and developed additional items to address the content. Pre- and post-test knowledge scores (number of correct responses; theoretical range 0-25) were computed for each participant. Higher scores indicate greater number of correct responses.
Secondary Outcomes
Secondary outcomes, assessed at pre- and post-test, evaluated the extent to which the material empowered participants to develop their family health history and utilize genetics healthcare (Appendix Table A). At post-test, general satisfaction, perceived usefulness, amount of new information provided, preference for language modality, and amount of attention paid to the signing and/or closed captioning (intervention only) also were assessed (Appendix Table A). Item responses are dichotomized for analyses (shown in Appendix Table A), with the exception of the item assessing amount of new information, which is treated as a quantitative variable.
Statistical Analyses
Participants were analyzed in the group to which they were assigned even if it could be ascertained that they did not view the educational materials. Individual missing knowledge items were treated as incorrect (7, 48); however, total knowledge scores were treated as missing if all items on the genetics or genetic counseling subscale were missing. Baseline characteristics were compared between the language modality groups. Between-group analyses were performed using t-tests for quantitative measures and Chi-square/Fisher's Exact tests for categorical measures. Repeated measures regression analysis using SAS PROC MIXED examined the effects of language modality (bilingual, monolingual), education level (high, low) and time (pre-test, post-test) on our primary outcome, knowledge scores. This statistical procedure allows for data collected at only one time point to be included in the analysis. The model included main effects, 2-way interactions and the 3-way interaction capturing the combined effects of language modality and education on knowledge score change. Within-group analyses used paired t-tests or McNemar's test for quantitative or dichotomous variables, respectively. Cohen's d statistic (49) was computed as a measure of effect size for between-group and within-group differences on quantitative variables. Absolute differences with 95% CI were computed for between-group and within-group comparisons on dichotomous variables. Analyses were performed using SAS v9.4 (50). Tests were 2-tailed and statistical significance was set at α=.05. No adjustments for multiple comparisons were made, hence examination of secondary outcomes is considered exploratory.
Sample size was determined using a fixed effects ANOVA model, 50:50 high:low education group ratio, published effect sizes(16), and pilot data suggesting a larger effect of genetic counseling on genetics knowledge of individuals with lower education. Under these conditions, our initially planned 1:1 bilingual:monolingual randomization scheme with n=25 individuals per language modality/education group (total n=100) had ≥80% power to detect Cohen's d effect size ≥.24 with two-sided p-value=.05.
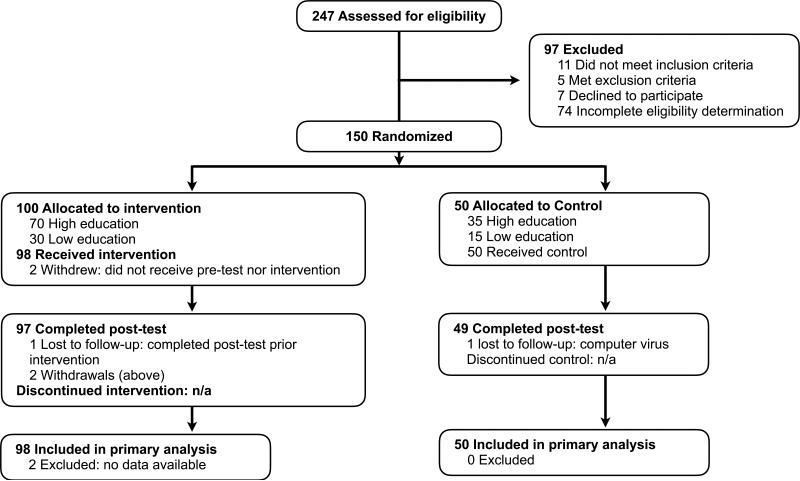
RESULTS
Figure 1 depicts study and sample flow. To accommodate additional bilingual modality investigation, we increased sample size from 100 to 150. Due to greater-than-anticipated recruitment challenges, the high:low education group ratio was changed from 50:50 to 70:30. We obtained no data on 2/150 (1.3%) participants at pre-test and 4/150 (2.67%) participants at post-test (Figure 1). The two individuals who dropped out after randomization were unaware of their group assignment. We obtained complete primary outcome data on 85.3% and 86.7% of the sample at pre- and post-test, respectively, and filled in missing data on 12.7% and 8.6% participants at pre- and post-test. Knowledge scores at only a single assessment timepoint were available on six participants due to missing all data on at least one knowledge subscale at the other time point. Primary outcome analysis is based on 148 participants with 290 out of 300 (96.7%) possible pre- and post-test observations. There was no evidence that participants with missing pre- or post-test observations were associated with group assignment or demographic variables. Language modality groups did not differ in sample characteristics (Table 1).
Figure 1.
Consort Flow Diagram for Deaf ASL-Users’ Knowledge of Cancer Genetics Health Information Study.
Table 1.
Sample Characteristics
| Characteristic | Intervention: Bilingual Modalitya | Control: Monolingual Modalitya | p |
|---|---|---|---|
| Sample size | 100 | 50 | |
| Deaf or hard-of-hearing, No. (%) | .11 | ||
| Deaf | 95 (95.0) | 44 (88.0) | |
| Hard-of-hearing | 4 (4.0) | 6 (12.0) | |
| Other§ | 1 (10) | 0 ( 0) | |
| Primary communication mode with deaf individuals, No. (%) | |||
| ASL | 95 (95.0) | 47 (94.0) | 1.0 |
| PSE, SEE, SIM-COM | 13 (13.0) | 9 (18.0) | 1.0 |
| Orally | 1 (10) | 0 (0) | .47 |
| In writing | 2 (2.0) | 0 (0) | .55 |
| Age, M (SD), years | 44.5 (14.7) | 44.6 (12.5) | .97 |
| Female, No. (%) | 60/100 (60) | 35/50 (70) | .28 |
| High school diploma or less, No. (%) | 30/100 (30) | 15/50 (30) | 1.0 |
| Ethnicity/Race, No. (%) | .58 | ||
| Non-Hispanic Caucasian | 64/96 (66.7) | 26/49 (53.1) | |
| Hispanic | 18/96 (18.8) | 13/49 (26.5) | |
| Asian | 6/96 (6.3) | 3/49 (6.1) | |
| Black | 4/96 (4.2) | 4/49 (8.2) | |
| Native American/American Indian | 1/96 (1.0) | 1/49 (2.0) | |
| Other | 3/96 (3.1) | 2/49 (4.1) | |
| Age became deaf, M (SD), years | 1.8 (1.6) | 1.5 (1.1) | .13 |
| Age began using ASL, M (SD), years | 7.7 (6.5) | 8.9 (8.8) | .39 |
| Cultural affiliation, No. (%) | .08 | ||
| Deaf community | 59/98 (60.2) | 25/48 (52.1) | |
| Deaf and Hearing communities | 30/98 (39.8) | 20/48 (41.7) | |
| Hearing community | 0 | 1/48 (2.1) | |
| Neither community | 0 | 2/48 (4.2) | |
| Type of High school attended†, No. (%) | .68 | ||
| Deaf-based | 55/98 (56.1) | 24/47 (52.2) | |
| Mainstream | 17/98 (17.4) | 12/47 (26.1) | |
| Mixed | 14/98 (14.3) | 5/47 (10.9) | |
| Hearing-based | 12/98 (12.2) | 5/47 (10.9) | |
| At least one deaf relative, No. (%) | 51/100 (51) | 20/50 (40) | .23 |
| Personal/family history of cancer‡, No. (%) | 57/98 (58.2) | 25/50 (50) | .60 |
| Current student, No. (%) | 15/98 (15.3) | 3/48 (6.3) | .18 |
| Prior genetic counseling or testing#, No. (%) | 40/98 (40.8) | 19/50 (38) | .86 |
| Pre-test knowledge score, M (SD) | 18.5 (3.3) | 18.1 (3.2) | .47 |
| TGJASL-R score§, M (SD) | 0.76 (0.15) | 0.73 (0.16) | .34 |
| Understand fingerspelling*, M (SD) | 8.2 (1.9) | 8.0 (2.1) | .59 |
| Read English well*, M (SD) | 8.0 (1.9) | 8.3 (2.0) | .39 |
| Time between pre-test survey and viewing materials, M (SD), days | 5.2 (6.4) | 4.7 (7.0) | .60 |
| Time between viewing materials and post-test survey, M (SD), days | 0.4 (1.0) | 0.5 (1.5) | .69 |
| Time spent viewing materials, M (SD), minutes | 48.3 (18.3) | 25.1 (16) | n/a |
¥ Participant response was “oral deaf”
Hearing-based high schools predominantly provide oral instruction in the classroom, i.e., oral school for the deaf, or a public school without interpreter/support services; Deaf-based high schools predominantly provide signed instruction (ASL or coded communication) in the classroom; Mainstream highschools captures public schools that predominantly provide sign instruction (ASL or coded communication) with interpreter/support services; Mixed high schools is defined as attending two or more of the previously described high school programs
breast, ovarian, or colon cancer
includes participation in Deaf Genetics Project
TGJASL-R: ASL Grammar Judgement Task. >0.5-1 reflects increasing grammatical accuracy; 0.5 reflects random guessing; <0.5 reflects systematic bias
self-rated on scale of 0 (low) – 10 (high)
Education level was not associated with amount of time spent viewing the bilingual (t=−.25, p=.80, d=.06) or monolingual materials (t=.77, p=.44, d=.24). However, scores on TGJASL-R and self-rated ease with reading English were higher in the high education group (TGJASL-R M=.79, 95% CI .77-.82; English reading ease M=8.7, 95% CI 8.3-8.9) than the low education group (TGJASL-R M=.64, 95% CI .60-.68, p<.001, d=1.15; English reading ease M=6.8, 95% CI 6.2-7.4, p<.001, d=1.12).
Primary Outcome
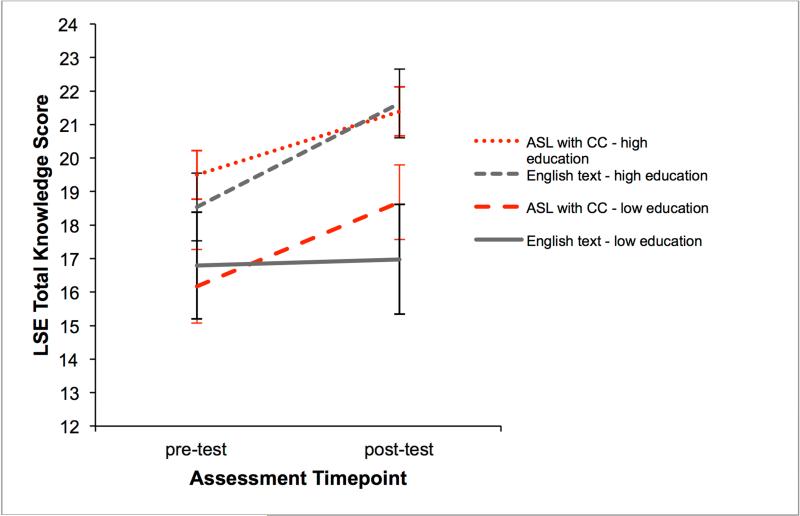
At pre-test, participants assigned to the bilingual and monolingual modalities correctly answered on average 73.9% (18.5/25) and 72.2% (18.1/25) of the knowledge items, and at post-test, 82.2% (20.6/25) and 81.6% (20.4/25), respectively. Repeated measures regression analysis found that scores were higher at post-test (F(1,138)=37.95, p<.001) and for the high education group (F(1,144)=38.07, p<.001) but did not differ by language modality (F(1,144)=.80, p=.37). However, the combination of language modality and education level affected knowledge score change (F(2,138)=4.33, p=.01; Figure 2). Knowledge score increased for the bilingual modality/low education group (M=2.55, 95% CI 1.41-3.7, t=4.57, p<.001, d=.85) but not for the monolingual modality/low education group (M=.25, 95% CI −1.76-2.26, t=.27, p=.79, d=.08). Knowledge scores increased for the bilingual modality/high education and monolingual modality/high education groups (M=1.9, 95% CI 1.07-2.72, t=4.58, p<.001, d=.56; M=3.0, 95% CI 2.03-4.0, t=6.31, p<.001, d=1.08, respectively).
Figure 2. Change in Least Square Estimates of the Total Knowledge Scores by Subgroups.
Least square estimates of the total knowledge scores (95% CI) from between-groups repeated measures regression are plotted for each language modality, education group, and assessment timepoint. 290 of 300 possible observations used in the analysis. CC = closed captions; LSE = least squares estimate
Secondary Outcomes
At pre-test, the intervention and control groups did not significantly differ in terms of intentions to develop a family health history or utilize genetics healthcare (Table 2). At post-test, these groups did not differ in terms of confidence to start a conversation with family about cancer history or intention to discuss their family history with a health care provider or genetic counselor (Table 2). However, those exposed to the bilingual modality were more likely than those exposed to the monolingual modality at post-test to feel ‘very confident’ developing their family tree (p=.03), and to report a ‘definite’ intention to see a genetic counselor upon a doctor's recommendation (p=.002), a ‘definite’ intention to have cancer genetic testing upon a doctor's recommendation (p=.02), and a ‘definite’ intention to encourage a friend or family member to seek genetic counseling for cancer risk (p=.001) (Table 2). Moreover, the percentage of participants exposed to the bilingual modality who reported feeling ‘very confident’ to develop their family tree and who ‘definitely’ intended to encourage friends or family members to seek genetic counseling for cancer risk significantly increased compared to pre-test (p=.005, p=.003, respectively), whereas this was not the case for participants exposed to the monolingual modality (Table 2).
Table 2.
Within-Group and Between-Group Analyses of Secondary Outcomes
| Within-Group Comparisons | Between-Group Comparisons | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention: Bilingual Modality | Control: Monolingual Modality | Pre | Post | |||||||||
| Item | Pre | Post | AD‡ (95% CI) | p | Pre | Post | AD (95% CI) | p | AD (95% CI) | p | AD (95% CI) | p |
| Very confident developing family tree | 28.9 (28/97) | 43.7 (42/96) | 13.6 (4.6, 22.7) | .005 | 22.9 (11/48) | 24.5 (12/49) | 0 (−14.4, 14.4) | 1.0 | 5.95 (−8.9, 2.1) | .55 | 19.3 (3.7, 34.9) | .03 |
| Very confident starting a conversation with family about health history | 41.7 (40/96) | 46.9 (45/96) | 5.3 (−5.4, 15.9) | .34 | 43.8 (21/48) | 55.1 (27/49) | 10.6 (−1.4, 22.8) | .09 | −2.1 (−19.2, 15.1) | .86 | −8.2 (−25.4, 8.9) | .38 |
| Intend to discuss family history with health care provider or genetic counselor | 54.6 (53/97) | 51.6 (49/95) | −2.1 (−13.4, 9.3) | .72 | 57.1 (28/49) | 51.1 (24/47) | −6.4 (−22.3, 9.7) | .44 | −2.5 (−19.5, 14.5) | .86 | .52 (−17.0, 18.0) | 1.0 |
| Intend to see a genetic counselor upon a doctor's recommendation | 51.1 (48/94) | 54.7 (52/95) | 1.1 (−9.1, 11.3) | .83 | 38.8 (19/49) | 26.5 (13/49) | −10.4 (−23.6, 2.8) | .13 | 12.3 (−4.7, 29.4) | .22 | 28.2 (12.3, 44.1) | .002 |
| Intend to have cancer genetic testing upon a doctor's recommendation | 53.1 (51/96) | 57.3 (55/96) | 3.2 (−7.5, 13.9) | .56 | 42.9 (21/49) | 36.7 (18/49) | −4.2 (−15.6, 7.3) | .48 | 10.3 (−6.8, 27.4) | .29 | 20.6 (3.8, 37.3) | .02 |
| Intend to encourage friend or family member to seek genetic counseling for cancer risk | 32.6 (31/95) | 51.0 (49/96) | 17.0 (6.6, 27.5) | .003 | 24.5 (12/49) | 22.5 (11/49) | −2.1 (−12.8, 8.7) | .71 | 8.1 (−7.2, 23.4) | .34 | 28.6 (13.2, 43.9) | .001 |
AD = absolute difference
At post-test, there was no significant difference between language modalities in mean rating of amount of new information provided in the educational material (bilingual: M=68.5, 95% CI 62.2-74.8; monolingual: M=61.8, 95% CI 52.1-71.6; p=.24, d=.21). Moreover, both groups endorsed that the modules explained things in understandable terms; that the information was ‘very useful’; that answering module quiz questions was not annoying; and that the modules were not too long (Table 3). However, compared to the monolingual modality, those exposed to the bilingual modality were more likely to report that they ‘liked’ the format (p<.0001), were ‘very satisfied’ with the modules (p=.04), and that they would ‘definitely’ recommend the educational modules to their family and friends (p=.03) (Table 3). Of those exposed to the bilingual modality, 95.7% indicated that the ASL speed was good, and 73.1% indicated that they focused their attention on both the signer and the closed captioning, while 19.4% focused most of their attention on the signer only, and 7.5% on the closed captioning only.
Table 3.
Between-Group Analyses of Opinions about Language Modality
| Item | Intervention: Bilingual Modality % (No.) | Control: Monolingual Modality % (No.) | AD‡ (95% CI) | p |
|---|---|---|---|---|
| Liked the format of the educational modules | 84.9 (79/93) | 47.7 (21/44) | 37.2 (20.8, 53.7) | <.0001 |
| Very satisfied with the educational modules | 78.6 (70/89) | 61.4 (27/44) | 17.3 (.57, 34.0) | .04 |
| Very useful information in the educational modules | 77.7 (73/94) | 61.7 (29/47) | 15.9 (−.29, 32.2) | .07 |
| Definitely recommend educational modules to family or friends | 55.3 (52/94) | 34.1 (15/44) | 21.2 (4.0, 38.5) | .03 |
| Educational module explained things in understandable terms | 91.6 (87/95) | 85.4 (41/48) | 6.2 (−5.3, 17.6) | .26 |
| Not annoying to answer the quiz questions in the educational module | 86.3 (82/95) | 81.3 (39/48) | 5.1 (−7.9, 18.1) | .47 |
| Educational modules not too long | 68.4 (65/95) | 70.8 (34/48) | −2.4 (−18.3, 13.5) | .85 |
AD = absolute difference
DISCUSSION
This randomized study addresses, for the first time, approaches to effectively bring non face-to-face cancer genetic information to a wide range of Deaf adult ASL-users. When comparing the effectiveness of the bilingual and monolingual approaches without regard for educational level, there was no evidence that they differed in their ability to enhance ASL-users’ cancer genetics knowledge. However, when taking education into account, significant differences in knowledge gains were found. Deaf individuals with some college or more education experienced knowledge gains regardless of language modality. Deaf individuals with high school or less education exposed to the bilingual modality also experienced knowledge gains. However, despite spending as much time reviewing the monolingual educational materials as the higher education group, those with high school or less education received no benefit in terms of increased understanding. Because ~50% of the US deaf/hard-of-hearing population has a high school or less education (33) this highlights the importance of providing health information using a bilingual approach, especially when the materials are targeted to all members of the Deaf community. As this intervention was evaluated with Deaf adult male and female ASL-users of different ethnic/racial groups, education levels, and ASL proficiency, the results indicate that a wide range of Deaf adult ASL-users would benefit from viewing the bilingual cancer genetics education modules for increasing their cancer genetics knowledge, with the goal of preventing cancer.
Although health knowledge may be necessary to reduce health disparities, individuals must ultimately take action to promote good health outcomes. Given the association between uptake of preventive health services among Deaf ASL-users and language-concordance with face-to-face peer-educators (6) and in the clinical setting (51), we were eager to identify the type of non-face-to-face communication that most likely would promote action. We found that language-concordant health information provided in ASL within the framework of a bilingual approach resulted in benefits such as greater confidence in developing a family tree, intention to see a genetic counselor or have cancer genetic testing upon a doctor's recommendation, intention to encourage others to seek genetic counseling for cancer risk, and recommending the health information to family and friends. The last finding is particularly important because of the importance of peer-to-peer information exchange in the Deaf community (52). Based on these findings we hypothesize that the bilingual approach will be more likely to lead to actions that would promote good health outcomes than a monolingual approach that offers non-language-concordant health information. Given the evidence that this bilingual modality had a positive impact on cancer genetics knowledge, confidence, and intentions, the next step would be to evaluate whether those changes in knowledge result in health behaviors that result in good health outcomes.
The majority of those exposed to the bilingual modality reported that they focused their attention on both the signer and the closed captioning, validating the importance of a bilingual approach. Although no standards exist for implementing a bilingual approach, there also is no evidence that adapting existing video material developed for a hearing audience by embedding a window with a video of an interpreter signing the information with closed captioning (picture in picture) is an effective way to implement a bilingual approach (2). Rather, this study adds to the growing evidence that ASL-users’ knowledge and satisfaction increases when materials are developed with Deaf community input, ASL discourse is the main point of reference, first-language users sign the material, and supplemental captioning and graphics are included (3-8).
Our findings also suggest that attention be paid to the audience's language proficiency and the material's complexity. The control condition's ~7th grade reading grade level conforms to the average US adult reading level (20) and to NIH guidelines for health information (53). Although this health information was of value to Deaf ASL-users with at least some college education, it was insufficient to increase cancer genetics knowledge for ASL-users with less education. Providing information in ASL with captioning and appropriate presentation format and discourse addressed this gap. The bilingual modality produced knowledge gains for the low education group despite their lower ASL grammar competency scores, suggesting that the material's ASL level was accessible to a range of ASL-users. Because there is no formal system yet for evaluating ASL grade level for educational materials, participant ASL grammar proficiency can be used as one means for examining the utility of ASL-based educational material.
Limitations
First, we developed some knowledge items to provide content coverage, however, item reliability and validity were not tested. Both language modalities yielded knowledge gains for the high education group, suggesting that they provided comparable information and contained the requisite information on the concepts assessed. Second, English is the standard US language for disseminating health information. Therefore we compared the intervention with virtually identical content provided in written English at the general US reading grade level to simulate the real world experience of deaf individuals. Although factors other than reading level may have been present in the monolingual modality to bias results, both language modality groups endorsed that the modules provided new information, explained concepts in understandable terms, and were reasonable in length. These findings suggest that the conditions were comparable on factors beyond reading level and reduce the possibility of potential bias. Third, we assessed reading literacy via a self-reported confidence with reading English instead of an objective English reading comprehension test. We found that the mean self-reported English reading ease score for the higher education group was significantly higher than the mean score for the lower education group. This result is consistent with the finding that education is positively associated with reading comprehension in a sample of deaf adults (19) using an objective measure of reading comprehension, thereby providing some support for the validity of our self-report measure. Fourth, because no adjustments for multiple comparisons were made, examination of secondary outcomes is considered exploratory. Finally, we developed web-based educational materials to reach as many individuals as possible. A limitation of our approach is that our results do not necessarily generalize to Deaf ASL-users who do not have a computer or internet access.
Conclusions
Effective access to language-concordant preventive health information is an important step towards reducing health disparities. This study fills a gap in knowledge regarding the effectiveness of a bilingual approach for providing non face-to-face genetic information for Deaf individuals whose primary language is ASL. An online approach allows deaf people in any geographical area to access important genetic information. A bilingual format using ASL video clips with closed captioning options provides this population with full access in their preferred language with access to specific medical terminology in written English. More broadly, taking education and language into account can inform the design and evaluation of other health educational initiatives for the Deaf community.
Supplementary Material
Acknowledgments
This study was funded by the National Cancer Institute R25CA154290 which had no input on the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no conflicts of interest to report.
www.disabilitystatistics.org. Click on American Community Survey >Educational Attainment > Disability Type {Hearing Disability} > Education {less than a High School education}. The percentage of this group is 17.6%. Repeat for Education {a high school diploma or equivalent}. The percentage of this group is 32.3%.
This work was presented at the Sixth Annual Meeting of the Coalition for Global Hearing Health, Oct 9-10, 2015, Gallaudet University, Washington DC, and the 2016 Midwinter Meeting of the Association for Research in Otolaryngology, Feb 21, 2016, and accepted for presentation at the 2016 Annual Education Conference of the National Society of Genetic Counselors, Sept 28-Oct 1, 2016.
References
- 1.Neuhauser L, Kreps GL. Online cancer communication: Meeting the literacy, cultural and linguistic needs of diverse audiences. Patient Educ Couns. 2008;71(3):365–77. doi: 10.1016/j.pec.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 2.Zazove P, Meador HE, Reed BD, Sen A, Gorenflo D. Cancer prevention knowledge of people with profound hearing loss. J Gen Intern Med. 2009;24(3):320–6. doi: 10.1007/s11606-008-0895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen LG, Nakaji M, Harry KM, Gallegos N, Malcarne VL, Sadler GR. Ovarian cancer: Deaf and hearing women's knowledge before and after an educational video. J Cancer Educ. 2013;28(4):647–55. doi: 10.1007/s13187-013-0529-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yao CS, Merz EL, Nakaji M, Harry KM, Malcarne VL, Sadler GR. Cervical cancer control: deaf and hearing women's response to an educational video. J Cancer Educ. 2012;27(1):62–6. doi: 10.1007/s13187-011-0264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Folkins A, Sadler GR, Ko C, Branz P, Marsh S, Bovee M. Improving the Deaf community's access to prostate and testicular cancer information: a survey study. BMC Public Health. 2005 Jun 6;5:63. doi: 10.1186/1471-2458-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaskowitz SR, Nakaji MC, Clark KL, Gunsauls DC, Sadler GR. Bringing prostate cancer education to deaf men. Cancer Detect Prev. 2006;30(5):439–48. doi: 10.1016/j.cdp.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Hickey S, Merz EL, Malcarne VL, Gunsauls DC, Huang J, Sadler GR. Breast cancer education for the Deaf community in American Sign Language. Oncol Nurs Forum. 2013;40(3):E86–91. doi: 10.1188/13.ONF.E86-E91. [DOI] [PubMed] [Google Scholar]
- 8.Sacks L, Nakaji M, Harry KM, Oen M, Malcarne VL, Sadler GR. Testicular cancer knowledge among deaf and hearing men. J Cancer Educ. 2013;28(3):503–8. doi: 10.1007/s13187-013-0493-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Q. Cancer predisposition genes: molecular mechanisms and clinical impact on personalized cancer care: examples of Lynch and HBOC syndromes. Acta Pharmacol Sin. 2015 Nov 30;2015:1–7. doi: 10.1038/aps.2015.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plevritis SK, Kurian AW, Sigal BM, et al. Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA. 2006;295(20):2374–84. doi: 10.1001/jama.295.20.2374. [DOI] [PubMed] [Google Scholar]
- 11.Kinney AY, Hicken B, Simonsen SE, et al. Colorectal cancer surveillance behaviors among members of typical and attenuated FAP families. Am J Gastroenterol. 2007;102(1):153–62. doi: 10.1111/j.1572-0241.2006.00860.x. [DOI] [PubMed] [Google Scholar]
- 12.Hadley DW, Jenkins JF, Dimond E, de Carvalho M, Kirsch I, Palmer CGS. Colon cancer screening practices following genetic counseling and testing for hereditary non-polyposis colorectal cancer. J Clin Oncol. 2004;22(1):39–44. doi: 10.1200/JCO.2004.06.128. [DOI] [PubMed] [Google Scholar]
- 13.Kauff ND, Domchek SM, Friebel TM. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26(8):1331–7. doi: 10.1200/JCO.2007.13.9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rebbeck TR, Freibel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2004;22(6):1055–62. doi: 10.1200/JCO.2004.04.188. [DOI] [PubMed] [Google Scholar]
- 15.Green MJ, Peterson SK, Baker MW, Harper GR, Friedman LC, Rubinstein WS, et al. Effect of a computer-based decision aid on knowledge, perceptions, and intentions about genetic testing for breast cancer susceptibility: A randomized controlled trial. JAMA. 2004;292(4):442–52. doi: 10.1001/jama.292.4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venne VL, Hamann HA. Successful use of peer educators for sharing genetic information. J Genet Counsel. 2007;16(4):515–25. doi: 10.1007/s10897-007-9087-2. [DOI] [PubMed] [Google Scholar]
- 17.Humphries T, Kushalnagar P, Mathur G, Napoli DJ, Padden C, Rathmann C, et al. Language acquisition for deaf children: Reducing the harms of zero tolerance to the use of alternative approaches. Harm Reduct J. 2012 Apr 2;9:16. doi: 10.1186/1477-7517-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Traxler CB. The Stanford Achievement Test, 9th Edition: National norming and performance standards for deaf and hard-of-hearing students. J Deaf Stud Deaf Educ. 2000;5(4):337–48. doi: 10.1093/deafed/5.4.337. [DOI] [PubMed] [Google Scholar]
- 19.Zazove P, Meader HE, Reed BD, Gorenflo DW. Deaf persons' English reading levels and associations with epidemiological, educational, and cultural factors. J Health Commun. 2013;18(7):760–72. doi: 10.1080/10810730.2012.743633. [DOI] [PubMed] [Google Scholar]
- 20.Neuhauser L, Ivey SL, Huang D, Engelman A, Tseng W, Dahrouge D, et al. Availability and readability of emergency preparedness materials for deaf and hard-of-hearing and older adult populations: Issues and assessments. PLoS One. 2013;8(2):e55614. doi: 10.1371/journal.pone.0055614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schuchman JS. Deafness and eugenics in the Nazi Era. In: van Eleve JE, editor. Genetics, Disability, and Deafness. Gallaudet University; Washington, DC: 2004. pp. 72–8. [Google Scholar]
- 22.Middleton A, Hewison J, Mueller RF. Attitudes of Deaf adults toward genetic testing for hereditary deafness. Am J Hum Genet. 1998;63(4):1175–80. doi: 10.1086/302060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Middleton A, Emery SD, Turner GH. Views, knowledge, and beliefs about genetics and genetic counseling among deaf people. Sign Lang Stud. 2010;10(2):170–96. [Google Scholar]
- 24.Lane H. Mask of Benevolence: Disabling the Deaf Community. DawnSignPress; San Diego: 1999. [Google Scholar]
- 25.Berman BA, Guthmann DS, Crespi CM, Liu W. Development and testing of an anti-tobacco school-based curriculum for deaf and hard of hearing youth. Am Ann Deaf. 2011;155(5):592–604. doi: 10.1353/aad.2011.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choe S, Lim RS-H, Clark K, Wang R, Branz P, Sadler GR. The impact of cervical cancer education for deaf women using a video educational tool employing American Sign Language, open captioning, and graphics. J Cancer Educ. 2009;24(1):10–5. doi: 10.1080/08858190802665245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baker C. Foundations of Bilingual Education and Bilingualism. 3rd edition. Multilingual Matters; Cleveland: 2001. [Google Scholar]
- 28.Padden C, Ramsey C. Reading ability in signing deaf children. Topics in Language Disorders. 1998;18(August):30–46. [Google Scholar]
- 29.Padden C. Early bilingual lives of deaf children. In: Parasnis I, editor. Cultural and Language Diversity: Reflections on the Deaf Experience. Cambridge University Press; Cambridge, MA: 1996. pp. 99–116. [Google Scholar]
- 30.Haptonstall-Nykaza TS, Schick B. The transition from fingerspelling to English print: Facilitating English decoding. J Deaf Stud Deaf Educ. 2007;12(2):172–83. doi: 10.1093/deafed/enm003. [DOI] [PubMed] [Google Scholar]
- 31.Safeer RS, Keenan J. Health literacy: The gap between physicians and patients. Am Fam Physician. 2005;72(3):463–8. [PubMed] [Google Scholar]
- 32.Chamberlain C, Mayberry RI. American sign language syntactic and narrative comprehension in skilled and less skilled readers: Bilingual and bimodal evidence for the linguistic basis of reading. Applied Psycholinguistics. 2008;29(3):367–88. [Google Scholar]
- 33.Disability Statistics from the 2013 American Community Survey (ACS) [Internet] Cornell University Employment and Disability Institute (EDI); 2015. [Sep 16, 2015]. [from http://www.disabilitystatistics.org/reports/acs.cfm?statistic=9] [Google Scholar]
- 34.Boudreault P, Mayberry RI. Grammatical processing in American Sign Language: Age of first-language acquisition effects in relation to syntactic structure. Language and Cognitive Processes. 2006;21(5):608–35. [Google Scholar]
- 35.Boudrealt P. Language and identity: A quantitative study of American Sign Language grammatical competency and deaf identity through online technology. University of Manitoba; Winnipeg, Canada: 2006. [Google Scholar]
- 36.Boudreault P, Baldwin EE, Fox M, Dutton L, Tullis L, Linden J, et al. Deaf adults' reasons for genetic testing depend on cultural affiliation: Results from a prospective, longitudinal genetic counseling and testing study. J Deaf Stud Deaf Educ. 2010;15:209–27. doi: 10.1093/deafed/enq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brislin R. Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology. 1970;1:185–216. [Google Scholar]
- 38.Samady W, Sadler GR, Nakaji M, Malcarne V. Translation of the Multidimensional Health Locus of Control Scales for users of American Sign Language. Public Health Nursing. 2008;25:480–9. doi: 10.1111/j.1525-1446.2008.00732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thurmann M. Identifying depiction constructed action and constructed dialogue in ASL presentations. In: Roy CH, editor. Discourse in Signed Languages. Gallaudet University Press; Washington, DC: 2011. pp. 46–66. [Google Scholar]
- 40.Chen Y-T, Chen L-F. Integrating thematic strategy and modularity concept into interactive video-based learning system. Information Tech J. 2012;11(8):1103–8. [Google Scholar]
- 41.Lynch PJ, Horton S. Web Style Guide: Basic Design Principles for Creating Web Sites. 3rd Edition. Yale University; Kendallville, Indiana: 2009. [Google Scholar]
- 42.Carver R. Silent reading rates in grade equivalents. J Literacy Res. 1989;21(2):155–66. [Google Scholar]
- 43.Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. Research Branch Report 8-75. US Naval Air Station; Memphis, TN: 1975. Derivation of New Readability Formulas (Automated Readability Index, Fog Count and Flesch Reading Ease Formula) for Navy Enlisted Personnel. [Google Scholar]
- 44.Flesch R. A new readability yardstick. J App Psychol. 1948;32(3):221–33. doi: 10.1037/h0057532. [DOI] [PubMed] [Google Scholar]
- 45.Elliott JO, Charyton C, Long L. A health literacy assessment of the National Epilepsy Foundation Web site. Epilepsy Behav. 2007;11(4):525–32. doi: 10.1016/j.yebeh.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 46.Lerman C, Narod S, Schulman K, Hughes C, Gomez-Caminero A, Bonney G, et al. BRCA1 testing in families with hereditary breast-ovarian cancer. A prospective study of patient decision making and outcomes [see comments]. JAMA. 1996;275(24):1885–92. [PubMed] [Google Scholar]
- 47.Pieterse AH, Ausems M, Van Dulmen AM, Beemer FA, Bensing JM. Initial cancer genetic counseling consultation: Change in counselees' cognitions and anxiety, and association with addressing their needs and preferences. Am J Med Genet. 2005;137A(1):27–35. doi: 10.1002/ajmg.a.30839. [DOI] [PubMed] [Google Scholar]
- 48.Baldwin EE, Boudrealt P, Fox M, Sinsheimer JS, Palmer CG. Effect of pre-test genetic counseling for deaf adults on knowledge of genetic testing. J Genet Couns. 2012;21(2):256–72. doi: 10.1007/s10897-011-9398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates, Inc.; Hillsdale, NH, England: 1977. [Google Scholar]
- 50.SAS. SAS (Version 9.4) SAS Institute Inc.; Cary, North Carolina: 2002. [Google Scholar]
- 51.McKee MM, Barnett SL, R.C. B, Pearson TA. Impact of communication on preventive services among deaf American Sign Language users. Am J Prev Med. 2011;41(1):75–9. doi: 10.1016/j.amepre.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Holcomb TK. Introduction to American Deaf Culture. Oxford University Press; New York: 2013. [Google Scholar]
- 53.National Cancer Institute Office of Communications . Making Health Communication Programs Work: A Planner's Guide. U.S. Dept. of Health and Human Services; Bethesda, Md.: 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.