Abstract
Data are limited on the sex-specific prevalence of diseases and their risk factors in middle-aged and older workers in Japan. In this cross-sectional study, we investigated the age- and sex-specific prevalence of hypertension, diabetes, dyslipidemia, metabolic syndrome (defined using joint statement criteria), obesity, underweight, abdominal obesity, and smoking among approximately 70,000 to 90,000 Japanese workers (predominantly men) aged 20–69 years in 2014. We also investigated the prevalence of low cardiorespiratory fitness in 2012 and no leisure-time exercise in 2014. In both sexes, the prevalence of lifestyle-related risk factors, including hypertension, diabetes, dyslipidemia, metabolic syndrome, obesity, and abdominal obesity, was increased with aging. In contrast, the prevalence of underweight was decreased with aging. Smoking prevalence exceeded 30% in men regardless of age, whereas the prevalence was around 10% in women of all age groups. Prevalence of no leisure-time exercise exceeded 50% among middle-aged and older workers in both sexes. Among workers aged 50–64 years, less than half of men had low fitness, whereas more than half of women had low fitness. Given the high prevalence of lifestyle-related risk factors among middle-aged and older workers, effective strategies to prevent cardiovascular disease in this age group are needed in Japan.
Keywords: Descriptive study, Japan, Workers, Middle-aged, Elderly, Health
Introduction
Japan, a country that has successfully achieved good population health1), is now facing new challenges caused by a rapidly aging population2). Statistics in Japan suggest that the proportion of people aged 75 and over will exceed 25% until 20253), whereas the proportion of the working population will decrease3). Given that these situations may threaten the sustainability of economic growth and health insurance4), there is an urgent need to develop effective strategies to overcome these issues. One promising solution is prolonging working life and emphasizing health promotion among workers5). For effective health promotion, it is important to understand the current health status of middle-aged and older Japanese workers.
To date, few studies have shown the age- and sex-specific prevalence of cardiovascular risk factors in middle-aged and older workers in Japan. Suka et al.6) recently reported a higher prevalence of hypertension, hyperlipidemia, diabetes, and obesity in male workers than female workers (n=approximately 120,000), and a high prevalence of these factors among middle-aged and older workers in both sexes. Similar results were shown for hypertension, hyperlipidemia, and diabetes in a national survey of 11,140 Japanese male and female workers7). We also reported similar trends for diabetes and pre-diabetes in 55,000 male and female workers8). In addition, descriptive data among Japanese workers are limited for metabolic syndrome9), abdominal obesity10, 11), underweight11), physical activity12, 13), and fitness12), which would all be important factors for health management.
Providing updated and systematic data on diseases and their risk factors among Japanese workers—with a special emphasis on middle-aged and older workers—would lead to a better understanding of the current health situation and help develop effective strategies for health promotion in the occupational settings of Japan. Here, we show data on the age- and sex-specific prevalence of hypertension, diabetes, dyslipidemia, metabolic syndrome, obesity, underweight, abdominal obesity, and smoking among Japanese workers aged 20–69 years in 2014 using health checkup data from large-scale companies. Among subgroups, we also show data on leisure-time exercise in 2014 and cardiorespiratory fitness in 2012.
Participans and Methods
Study settings
The present descriptive analyses were performed using cross-sectional data on periodic health checkups from the Japan Epidemiology Collaboration on Occupational Health (J-ECOH) Study, an on-going, large-scale multi-company based study among Japanese workers from more than 10 companies. In Japan, workers are obliged to undergo health examination at least once a year under the Industrial Safety and Health Act. The details of the J-ECOH Study14) and sub-cohorts for analysis of fitness15) and physical activity16) have been described elsewhere. The J-ECOH Study was announced in each company using posters. Participants did not provide their verbal or written informed consent to take part in the study but were given an opportunity to refuse the use of their data for research, according to the Japanese Ethical Guidelines for Epidemiological Research. The study protocol was approved by the Ethics Committee of the National Center for Global Health and Medicine, Japan.
For analysis of data other than exercise and fitness, we extracted data on 91,150 workers (77,264 men and 13,886 women), aged 20–69, from 11 companies who received health checkups between April 2014 and March 2015 (in some companies, between January 2014 and December 2014). For analysis of leisure-time exercise, we used data on 50,864 workers (8,389 women) aged 20–69 who underwent their health checkups between April 2014 and March 2015 from one of the 11 participating companies16). For cardiorespiratory fitness, we extracted data on 4,346 workers (810 women) aged 20–64 collected between January 2012 and December 2012 from another one of the participating companies15).
Participants
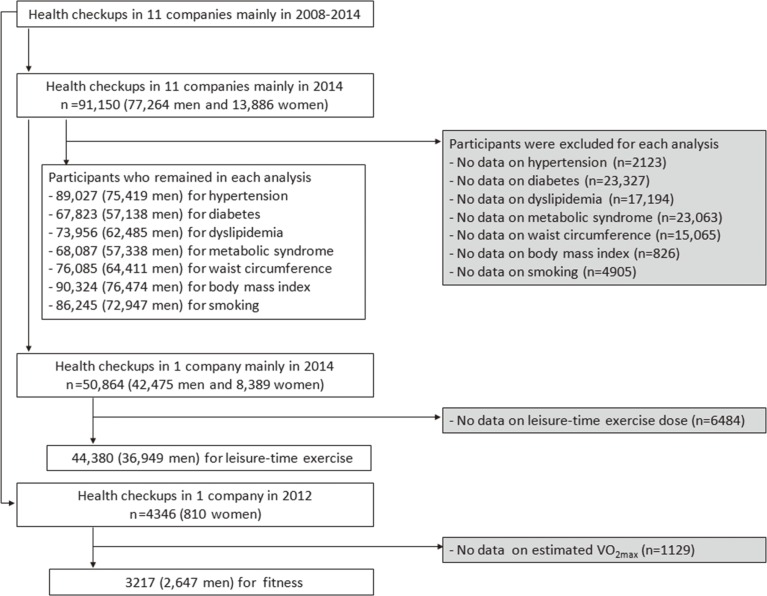
We excluded individuals who did not have data on target outcomes for respective analysis, which yielded different population sizes in each analysis, as shown in Fig. 1. Excluded participants were 1,845 men and 278 women for hypertension; 20,126 men and 3,201 women for diabetes; 14,779 men and 2,415 women for dyslipidemia; 19,926 men and 3,137 women for metabolic syndrome; 12,853 men and 2,212 women for waist circumference; and 790 men and 36 women for BMI. For leisure-time exercise analysis, we excluded 5,526 men and 958 women who did not have data on leisure-time exercise or who engaged only in unspecified activity in one of the participating companies. For cardiorespiratory fitness, 889 men and 240 women were excluded in another one of the participating companies.
Fig. 1.
Sampling design.
General health examination
Body height and weight were measured at each company in accordance with a standard protocol. Body mass index (BMI) was calculated as weight (kg) divided by squared height (m). Blood pressures were measured using an automated sphygmomanometer. Smoking habits and treatment for hypertension, dyslipidemia, and diabetes were self-reported using a questionnaire. Biochemical measurements included plasma glucose, hemoglobin A1c (HbA1c), low-density lipoprotein (LDL)-cholesterol, high-density lipoprotein (HDL)-cholesterol, and triglycerides. Plasma glucose level was determined by enzamatic method in ten companies and glucose oxidase peroxidative electrode method in one company. HbA1c level was determined by latex agglutination immunoassay in eight companies, high-performance liquid chromatography method in two companies, and enzymatic method in one company. LDL-cholesterol, HDL-cholesterol, and triglycerides levels were estimated by enzymatic method in all participating companies. All laboratories involved in the health examinations in the participating companies have received sufficiently high scores (score >95 out of 100 or rank A) from external quality control agencies, including National Federation of Industrial Health Organization, the Japan Medical Association, and Japanese Association of Laboratory Medical Technologists.
Diagnosis of disease
Hypertension was defined as systolic blood pressure of ≥140 mm Hg, diastolic blood pressure of ≥90 mm Hg, or under treatment for hypertension. Dyslipidemia was defined as LDL-cholesterol of ≥140 mg/dL, HDL-cholesterol of <40 mg/dL, fasting triglycerides of ≥150 mg/dL, or under treatment for dyslipidemia. Diabetes was defined as fasting plasma glucose of ≥126 mg/dL, HbA1c of ≥6.5%, or self-report (under treatment for diabetes and/or history of diabetes). Metabolic syndrome was defined according to the criteria of the joint interim statement17) as the presence of any three or more of the following criteria: (1) high waist circumference for Asians: ≥90 cm in men and ≥80 cm in women; (2) high triglycerides: ≥150 mg/dL; (3) low HDL cholesterol: <40 mg/dL in men, <50 mg/dL in women; (4) high blood pressure: systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg; and (5) high fasting glucose: ≥100 mg/dL. Participants reporting current treatment for dyslipidemia, hypertension, or diabetes were considered to meet the criteria for high triglycerides, high blood pressure, and high fasting glucose, respectively, irrespective of the data measured at the checkups.
Measurement of cardiorespiratory fitness and leisure-time exercise
As an indicator of cardiorespiratory fitness, we assessed estimated VO2max. Estimated VO2max was obtained by an incremental endurance exercise test using a bicycle ergometer (Aerobike 900 U, Combi, Tokyo, Japan) with three phases of three minutes duration each (a total of 9 minutes). Details of this fitness measurement has been described previously15). Participants were divided into two levels of cardiorespiratory fitness based on the criteria by Ministry of Health, Labour, and Welfare, Japan18): high cardiorespiratory fitness in men was defined as ≥39 mL/kg/min among individuals aged <40 years, ≥35 mL/kg/min among individuals aged 40-<60 years, and ≥32 mL/kg/min among individuals aged ≥60 years, whereas high cardiorespiratory fitness in women was defined as ≥33 mL/kg/min among individuals aged <40 years, ≥30 mL/kg/min among individuals aged 40-<60 years, and ≥26 mL/kg/min among individuals aged ≥60 years.
Weekly dose of leisure-time exercise expressed in metabolic equivalent (MET) hours was calculated using data on types, frequency, and duration of exercise or sports activities during leisure using a standard questionnaire as described elsewhere16). Participants were categorized into four groups according to the dose of leisure-time exercise per week: no exercise (0 MET hours), low (>0 to <7.5 MET hours), medium (7.5 to <15.0 MET hours), or high (≥15.0 MET-hours) in harmony with recommended dose of physical activity by World Health Organization19).
Statistical analysis
Data are shown as mean (standard deviation) for continuous variables and percentages for categorical variables.
Results
The crude prevalence of hypertension was 22.0% and 11.6% in men and women, respectively (Table 1). The prevalence of hypertension increased linearly with advancing age, reaching 48.4% and 37.4% among men and women aged 60–69 years, respectively. A large increase was observed in both men and women aged 30–69 years.
Table 1. Age- and sex-specific prevalence of smoking, diabetes, hypertension, dyslipidemia, metabolic syndrome, abdominal obesity, obesity, and underweight (n=67,823 to 90,324).
| Characteristics | Categories of age (year) | ||||||
|---|---|---|---|---|---|---|---|
| <30 | 30 to 39 | 40 to 49 | 50 to 59 | ≥60 | All (20 to 69) | ||
| Men, n | 11,778 | 14,989 | 24,362 | 19,617 | 6,518 | 77,264 | |
| Smoker | 36.9 | 38.3 | 37.6 | 34.2 | 30.1 | 36.1 | |
| Fasting glucose, mg/dL | 91±10 | 95±14 | 99±17 | 105±22 | 109±22 | 101±19 | |
| HbA1c, % | 5.3±0.4 | 5.4±0.5 | 5.6±0.6 | 5.8±0.8 | 5.9±0.7 | 5.6±0.7 | |
| Diabetes | 1.0 | 3.4 | 6.8 | 14.8 | 21.7 | 9.8 | |
| SBP, mmHg | 118±12 | 119±13 | 121±14 | 125±15 | 129±16 | 122±14 | |
| DBP, mmHg | 68±9 | 73±10 | 77±11 | 80±10 | 80±10 | 76±11 | |
| Hypertension | 3.6 | 8.2 | 19.6 | 37.0 | 48.4 | 22.0 | |
| Fasting triglyceride, mg/dL | 92±78 | 117±93 | 130±104 | 132±96 | 127±92 | 126±97 | |
| LDL-cholesterol, mg/dL | 105±29 | 119±30 | 125±30 | 124±30 | 122±30 | 121±31 | |
| HDL-cholesterol, mg/dL | 56±12 | 56±14 | 56±14 | 58±15 | 58±15 | 57±15 | |
| Dyslipidemia | 29.2 | 44.7 | 50.3 | 51.2 | 47.8 | 47.7 | |
| Metabolic syndrome | 3.6 | 11.1 | 20.3 | 31.1 | 36.8 | 23.2 | |
| Waist circumference, cm | 77.8±9.1 | 81.7±9.7 | 84.0±9.4 | 84.7±8.7 | 84.6±7.9 | 83.5±9.3 | |
| Waist circumference ≥90 cm | 9.7 | 17.6 | 23.5 | 24.6 | 23.8 | 21.9 | |
| BMI, kg/m2 | 22.7±3.7 | 23.6±3.8 | 24.1±3.6 | 23.9±3.2 | 23.7±2.9 | 23.7±3.5 | |
| Weight status | |||||||
| ≥30.0 kg/m2 | 4.8 | 5.9 | 6.3 | 4.3 | 2.8 | 5.2 | |
| 25.0 to <30.0 kg/m2 | 15.9 | 21.8 | 26.4 | 27.7 | 26.7 | 24.3 | |
| 23.0 to <25.0 kg/m2 | 17.9 | 21.6 | 25.0 | 26.4 | 27.3 | 23.8 | |
| 18.5 to <23.0 kg/m2 | 54.2 | 46.4 | 39.8 | 39.3 | 41.1 | 43.3 | |
| <18.5 kg/m2 | 7.2 | 4.3 | 2.6 | 2.3 | 2.2 | 3.5 | |
| Women, n | 2,051 | 2,859 | 5,219 | 2,939 | 818 | 13,886 | |
| Smoker | 8.6 | 13.3 | 11.5 | 10.4 | 9.7 | 11.1 | |
| Fasting glucose, mg/dL | 88±9 | 89±10 | 92±13 | 96±14 | 100±18 | 93±13 | |
| HbA1c, % | 5.3±0.4 | 5.4±0.4 | 5.5±0.5 | 5.7±0.5 | 5.9±0.6 | 5.5±0.5 | |
| Diabetes | 1.2 | 1.7 | 2.5 | 6.1 | 12.7 | 3.9 | |
| SBP, mmHg | 108±11 | 110±13 | 114±16 | 121±17 | 127±18 | 115±16 | |
| DBP, mmHg | 63±8 | 67±10 | 71±11 | 75±11 | 76±11 | 70±11 | |
| Hypertension | 0.7 | 3.4 | 9.3 | 23.1 | 37.4 | 11.6 | |
| Fasting triglyceride, mg/dL | 61±33 | 71±45 | 75±50 | 87±48 | 98±55 | 78±49 | |
| LDL-cholesterol, mg/dL | 98±26 | 105±28 | 115±29 | 130±31 | 129±30 | 116±31 | |
| HDL-cholesterol, mg/dL | 68±14 | 67±14 | 69±16 | 72±17 | 68±17 | 69±16 | |
| Dyslipidemia | 12.4 | 15.0 | 22.7 | 42.7 | 47.3 | 27.1 | |
| Metabolic syndrome | 1.4 | 5.2 | 8.4 | 21.1 | 36.7 | 12.7 | |
| Waist circumference, cm | 70.7±7.4 | 74.7±9.0 | 76.3±9.6 | 77.9±10.0 | 79.0±9.5 | 76.2±9.6 | |
| Waist circumference ≥80 cm | 10.3 | 24.9 | 30.4 | 39.0 | 45.5 | 31.4 | |
| BMI, kg/m2 | 20.9±3.2 | 21.5±3.7 | 22.0±3.8 | 22.3±3.8 | 22.7±3.5 | 21.8±3.7 | |
| Weight status | |||||||
| ≥30.0 kg/m2 | 2.4 | 3.6 | 4.4 | 4.8 | 4.2 | 4.0 | |
| 25.0 to <30.0 kg/m2 | 7.0 | 10.0 | 12.5 | 14.1 | 18.7 | 11.9 | |
| 23.0 to <25.0 kg/m2 | 8.1 | 11.2 | 13.2 | 15.6 | 19.6 | 12.9 | |
| 18.5 to <23.0 kg/m2 | 62.5 | 58.4 | 56.3 | 53.8 | 48.4 | 56.7 | |
| <18.5 kg/m2 | 20.1 | 16.8 | 13.6 | 11.7 | 9.2 | 14.6 | |
Data are shown as (%) for categorical variables and mean±standard deviation for continuous variables.
The crude prevalence of diabetes was 9.8% and 3.8% in men and women, respectively. The prevalence of diabetes increased with advancing age (Table 1), reaching 21.7% and 12.7% among men and women aged 60–69 years, respectively. A large increase was observed in both men and women aged 40–59 years. A similar trend was observed for fasting glucose and HbA1c in both men and women.
The crude prevalence of dyslipidemia was 47.7% and 27.1% in men and women, respectively (Table 1). In men, the prevalence of dyslipidemia increased with advancing age, reaching 51.2% in workers aged 50–59 years; the prevalence of dyslipidemia was slightly decreased in workers aged 60–69 years (47.8%). In women, the prevalence of dyslipidemia increased linearly with aging, reaching 47.3% in workers aged 60–69 years. Similar changes with aging were observed for triglycerides and LDL cholesterol. HDL cholesterol levels were not materially different by age group in both sexes.
The crude prevalence of metabolic syndrome, defined by the 2009 joint statement criteria, was 23.2% and 12.7% in men and women, respectively (Table 1). The prevalence of metabolic syndrome increased with advancing age, reaching 36.8% and 36.7% in men and women aged 60–69 years, respectively. A large increase was observed in men aged 30–69 years and in women aged 40–69 years.
Regarding abdominal obesity, defined as a waist circumference ≥90 cm in men and ≥80 cm in women, the crude prevalence was 21.9% in men and 31.4% in women. In men, the prevalence of abdominal obesity increased with aging for workers aged 50–59 years (reaching 24.6%), and then slightly decreased in workers aged 60–69 years (reaching 23.8%). In women, the prevalence of abdominal obesity gradually increased with aging, reaching 45.5% in workers aged 60–69 years.
The crude prevalence of obesity (BMI ≥25.0 kg/m2) was 29.5% and 15.9% in men and women, respectively (Table 1). In men, the prevalence of obesity increased with advancing age, reaching 32.7% in workers aged 40–49 years, then, the prevalence of obesity was slightly and gradually decreased in workers aged 50–69 years. In women, the prevalence of obesity increased linearly with aging; the highest prevalence of obesity was observed in workers aged 60–69 years (22.9%). Similar changes with aging were observed for mean BMI levels.
The crude prevalence of underweight (<18.5 kg/m2) was 3.5% and 14.6% in men and women, respectively (Table 1). The prevalence of underweight decreased with advancing age, reaching 2.2% and 9.2% in men and women aged 60–69 years, respectively.
The crude prevalence of smoking was 36.1% and 11.1% in women, respectively (Table 1). In both sexes, the prevalence of smoking increased in workers aged 20–39 years; in men and women aged 60–69 years, the prevalence of smoking slightly but steadily decreased with aging, reaching 30.1% and 9.7%, respectively.
The crude prevalence of no leisure-time exercise was 62.3% and 77.0% in men and women, respectively (Table 2). The prevalence of no leisure-time exercise increased in men aged 20–49 years, while in workers aged 60–69 years, the prevalence of no leisure-time exercise decreased with aging, reaching 54.8%. In women aged 20–39 years, the prevalence of no leisure-time exercise increased; however, the prevalence of no leisure-time exercise decreased with aging in workers aged 60–69 years, reaching 74.3%.
Table 2. Weekly dose of leisure-time exercise by age and sex (n=44,380).
| Characteristics | Categories of age (year) | ||||||
|---|---|---|---|---|---|---|---|
| <30 | 30 to 39 | 40 to 49 | 50 to 59 | ≥60 | All (20 to 69) | ||
| Men, n | 5,483 | 7,506 | 11,873 | 8,973 | 3,159 | 36,949 | |
| Weekly exercise dose | |||||||
| 0 MET-hour | 2,982 (54.8) | 4,869 (64.9) | 7,709 (64.9) | 5,736 (63.9) | 1,732 (54.8) | 23,028 (62.3) | |
| >0 to <7.5 MET-hours | 1,215 (22.3) | 1,191 (15.9) | 1,718 (14.5) | 1,135 (12.7) | 420 (13.3) | 5,679 (15.4) | |
| 7.5 to <15.0 MET-hours | 632 (11.6) | 766 (10.2) | 1,245 (10.5) | 989 (11.0) | 401 (12.7) | 4,033 (10.9) | |
| ≥15.0 MET-hours | 609 (11.2) | 680 (9.1) | 1,201 (10.1) | 1,113 (12.4) | 606 (19.2) | 4,209 (11.4) | |
| Women, n | 1,134 | 1,643 | 2,492 | 1,590 | 572 | 7,431 | |
| Weekly exercise dose | |||||||
| 0 MET-hour | 800 (70.6) | 1,328 (80.8) | 1,970 (79.1) | 1,195 (75.2) | 425 (74.3) | 5,718 (77.0) | |
| >0 to <7.5 MET-hours | 184 (16.2) | 181 (11.0) | 278 (11.2) | 205 (12.9) | 64 (11.2) | 912 (12.3) | |
| 7.5 to <15.0 MET-hours | 76 (6.7) | 68 (4.1) | 128 (5.1) | 91 (5.7) | 40 (7.0) | 403 (5.4) | |
| ≥15.0 MET-hours | 74 (6.5) | 66 (4.0) | 116 (4.7) | 99 (6.2) | 43 (7.5) | 398 (5.4) | |
Data are shown as number (%).
The crude prevalence of low cardiorespiratory fitness was 39.2% and 57.1% in men and women, respectively (Table 3). In men, the prevalence of low fitness was 33.7%, 51.2%, 33.8%, 38.1%, and 18.1% in workers aged <30, 30–39, 40–49, 50–59, and 60–64, respectively. In women, the corresponding values were 53.8%, 65.1%, 48.7%, 64.1%, and 33.3%, respectively.
Table 3. Cardiorespiratory fitness level by age and sex (n=4,346).
| Characteristics | Categories of age (year) | ||||||
|---|---|---|---|---|---|---|---|
| <30 | 30 to 39 | 40 to 49 | 50 to 59 | 60 to 64 | All (20 to 64) | ||
| Men, n | 433 | 719 | 708 | 707 | 80 | 2,647 | |
| High cardiorespiratory fitnessa | 287 (66.3) | 351 (48.8) | 469 (66.2) | 438 (62.0) | 65 (81.3) | 1,610 (60.8) | |
| Low cardiorespiratory fitness | 146 (33.7) | 368 (51.2) | 239 (33.8) | 269 (38.1) | 15 (18.8) | 1,037 (39.2) | |
| Women, n | 158 | 109 | 150 | 153 | 3 | 573 | |
| High cardiorespiratory fitnessb | 71 (54.2) | 38 (34.9) | 77 (51.3) | 55 (36.0) | 2 (66.7) | 246 (42.9) | |
| Low cardiorespiratory fitness | 84 (53.8) | 71 (65.1) | 73 (48.7) | 98 (64.1) | 1 (33.3) | 327 (57.1) | |
Data are shown as number (%).
a High cardiorespiratory fitness was defined as ≥39 mL/kg/min in individuals aged <40 years, ≥35 mL/kg/min in individuals aged 40 to <60 years, and ≥32 mL/kg/min in individuals aged ≥60 years.
b High cardiorespiratory fitness was defined as ≥33 mL/kg/min in individuals aged <40 years, ≥30 mL/kg/min in individuals aged 40 to <60 years, and ≥26 mL/kg/min in individuals aged ≥60 years.
Discussion
The present study among Japanese workers aged 20–69 years from large-scale companies in Japan showed that the crude prevalence of cardiometabolic risk factors including hypertension, diabetes, dyslipidemia, metabolic syndrome, obesity, and abdominal obesity were 22.0%, 9.8%, 47.7%, 23.2%, 29.5%, and 21.9% in men, respectively, and 11.6%, 3.9%, 27.1%, 12.7%, 15.9%, and 31.4% in women, respectively. The prevalence of these factors increased overall with advancing age in both men and women. In contrast, the prevalence of underweight decreased linearly with increasing age in both men and women. The prevalence of smoking exceeded 30% in men regardless of age group, whereas smoking prevalence was around 10% in women. In both men and women, more than half of workers did not engage in leisure-time exercise regardless of age group.
In the present study, the prevalence of cardiometabolic risk factors including hypertension, dyslipidemia, diabetes, obesity defined by BMI, abdominal obesity defined by waist circumference, and metabolic syndrome increased with aging both in men and women. This finding is supported by previous studies among Japanese workers on hypertension6, 7), dyslipidemia, diabetes6, 7), obesity6), waist circumference10), and metabolic syndrome9). The present findings, together with existing data of Japanese workers, suggest the importance of effective strategies for protecting cardiovascular health among middle-aged and older workers in Japan. A high-risk approach using a risk predicting score for cardiovascular disease20) and/or a population-based approach to improve cardiovascular health21) would serve such a purpose. Given the nature of our cross-sectional design, we could not elucidate the incidence of untreated and uncontrolled hypertension or other diseases. Future longitudinal studies should investigate these issues to develop a better health management system in Japanese occupational settings.
Our study showed lower age- and sex-specific prevalence of hypertension and obesity compared with those in the nationally representative sample of Japanese, which included the self-employed, the unemployed, and the housewife22, 23). The national survey in 201322) showed that the prevalence of hypertension in individuals aged 20–29 years, 30–39 years, 40–49 years, 50–59 years, and 60–69 years were 11.6%, 17.9%, 32.9%, 56.4%, and 68.0% in men, and 1.8%, 5.7%, 16.4%, 34.7%, and 57.7% in women, respectively. The national survey in 201423) showed that the corresponding prevalence of obesity were 20.9%, 27.2%, 30.9%, 34.4%, 31.2%, respectively, in men, and 10.4%, 15.9%, 17.0%, 23.7%, and 24.0% in women, respectively. Further, a previous study using health checkup data in 2000 from five occupational health organizations24) reported that, among men, prevalence of hypertension and obesity were slightly lower among workers in large-scale companies than those in small-scale enterprises. Thus, our finding of lower prevalence of hypertension and obesity than those in the national representative sample may be ascribed to the fact that our sample did not include workers in small and medium-sized enterprises. Although prevalence of dyslipidemia and metabolic syndrome in our sample were higher than those in the nationally representative sample22, 25), this difference may be ascribed to the differences in the definition of the diseases (i.e., low HDL-cholesterol and self-report for dyslipidemia22); abdominal obesity plus any one or more of the three conditions including high blood glucose, high blood pressure, and dyslipidemia for metabolic syndrome25) in the national surveys). Previously, we reported similar age- and sex-specific prevalence of diabetes compared to those in nationally representative sample when using the same definition with HbA1c and self-report8).
We found that the prevalence of no leisure-time exercise was high, especially in women. Although both male and female workers aged 60–69 years tended to engage in leisure-time exercise compared with younger workers, the prevalence of no exercise among workers aged 60–69 years exceeded 50% in men and 70% in women. This finding is supported by a recent national survey in Japan13) showing similar age and sex difference in weekly sports time among workers. Additionally, another national survey of general population conducted in Japan in 2013 showed that the proportion of adults who did not engage in exercise (≥2 days per week of ≥30 min of exercise in a day for at least 1 year) was 66.2% in men and 72.8% in women22). In addition, our results on the lower prevalence of no leisure-time exercise among workers aged 60–69 years compared with younger groups agree with this survey’s findings22). Given that women after menopause are at high risk of osteoporosis26), physical activity promotion among middle-aged to older women would help to prevent this disease27) and contribute to healthy life span. Given the decreasing trend of energy expenditure at work28) and the high prevalence of no leisure-time exercise, workplace interventions for physical activity, including workstation interventions and promoting the use of stairs29), may be a solution for maintaining or increasing regular physical activity level for Japanese workers.
In the present study, the prevalence of low fitness was 30–50% in men aged 20–59 years and approximately 20% in men aged 60–64 years. In women, the prevalence of low fitness was approximately 50–70% among workers aged 20–59 years, and approximately 30% in workers aged 60–64 years. However, only three women aged 60 to 64 years provided cardiorespiratory fitness data. Thus, any conclusion can be drawn for women aged 60 and over. The low prevalence of low fitness in men aged 60–64 years may be due to the selective inclusion of healthy workers, rather than a true prevalence; indeed, the proportion of those who did not provide cardiorespiratory fitness data increased with aging (data not shown). A previous study of Japanese workers showed that, compared with workers aged 50–59 years, workers aged 60–64 years and those aged 65 years and over tended to have lower fitness, although the proportion of women in each age group in that study is unclear12). To minimize non-participation bias, measurement of grip strength, which is another indicator of fitness and can be assessed more simply, quickly, and inexpensively, and has been considered to be a promising biomarker of aging30), may help stratify target individuals for intervention in occupational settings.
The strengths of this study include a large sample size and measurement of cardiorespiratory fitness, although fitness data were available only in a subgroup. However, there are limitations of our study. First, this study used existing data from more than 10 companies. Thus, questionnaires for lifestyles, history of disease, and medication, and the procedures for measuring anthropometric and biochemical data, were different by companies. All laboratories that conducted biochemical measurements for the participating companies, however, have participated in one or more external quality control programs and received the highest rank of certification. Second, although cancer31) and mental health32) in a working population are growing concerns in Japan, we did not systematically collect data on either of these factors. Future studies should elucidate the current situations of these issues among Japanese workers. In addition, we have no data on social class and occupation, and thus are not able to examine whether socioeconomic status is related to health among Japanese workers33). Lastly, study participants were workers mainly from large-scale companies (electric machinery and apparatus manufacturing, steel, chemical, gas, non-ferrous metal manufacturing, automobile and instrument manufacturing, plastic product manufacturing). Therefore, the present findings may not be applicable to workers in small- to mid-sized companies, companies with different background, or general population in Japan.
We found that the prevalence of lifestyle-related risk factors including hypertension, diabetes, dyslipidemia, metabolic syndrome, and obesity was higher in men than women, and that the prevalence of these factors was high overall in workers aged 60–69 years. These findings reinforce the importance of developing effective strategies for the prevention of cardiovascular disease among middle-aged and older Japanese workers, especially in men. Regardless of age group, the prevalence of smoking exceeded 30% in men, whereas the prevalence of smoking was about 10% in women; smoking cessation and prevention of smoking initiation should be recommended, especially for men regardless of age. The prevalence of underweight was lowest among workers aged 60–69 years regardless of sex. Given the low proportion of workers who engaged in leisure-time exercise regardless of age or sex, physical activity promotion may yield large health benefits.
Funding
This study was funded by the Industrial Health Foundation.
Conflict of Interest
The authors declare there is no conflict of interest. T. Nakagawa, S. Yamamoto, and T. Honda belong to Hitachi, Ltd.; H. Okazaki and S. Dohi, Mitsui Chemicals, Inc.; A. Uehara and M. Yamamoto, YAMAHA CORPORATION; T. Miyamoto, Nippon Steel & Sumitomo Metal Corporation Kimitsu Works; T. Kochi, M. Eguchi, and I. Kabe, Furukawa Electric Co., Ltd.; T. Murakami and M. Shimizu, Mizue Medical Clinic, Keihin Occupational Health Center; K. Tomita, Mitsubishi Plastics, Inc.; S. Nagahama, All Japan Labour Welfare Foundation; T. Imai and A. Nishihara, Azbil Corporation; N. Sasaki and T. Ogasawara, Mitsubishi Fuso Truck and Bus Corporation; A. Hori and C. Nishiura, Tokyo Gas Co., Ltd. T. Nakagawa, S. Yamamoto, T. Honda, H. Okazaki, S. Dohi, A. Uehara, M. Yamamoto, T. Miyamoto, T. Kochi, M. Eguchi, I. Kabe, T. Murakami, M. Shimizu, K. Tomita, S. Nagahama, T. Imai, A. Nishihara, N. Sasaki, T. Ogasawara, A. Hori, C. Nishiura are the health professionals in each participating company.
Acknowledgments
We thank Toshiteru Okubo (Chairperson of Industrial Health Foundation, Former Director of Radiation Effects Research Foundation) for scientific advice on the conduct of J-ECOH Study; Maki Konishi (National Center for Global Health and Medicine) for data management; and Rika Osawa (National Center for Global Health and Medicine) for administrative support.
Members of the Japan Epidemiology Collaboration on Occupational Health Study Group are: T. Mizoue, A. Nanri, K. Kurotani, K. Kuwahara, I. Kashino, S. Akter, and H. Hu, National Center for Global Health and Medicine, Tokyo, Japan; T. Nakagawa, S. Yamamoto, and T. Honda, Hitachi, Ltd., Ibaraki, Japan; S. Dohi and H. Okazaki, Mitsui Chemicals, Inc., Tokyo, Japan; T. Imai and A. Nishihara, Azbil Corporation, Tokyo, Japan; N. Sasaki and T. Ogasawara, Mitsubishi Fuso Truck and Bus Corporation, Kanagawa, Japan; A. Uehara and M. Yamamoto, YAMAHA CORPORATION, Shizuoka, Japan; T. Miyamoto, Nippon Steel & Sumitomo Metal Corporation Kimitsu Works, Chiba, Japan; I. Kabe, T. Kochi, and M. Eguchi, Furukawa Electric Co., Ltd., Tokyo, Japan; T. Murakami, and M. Shimizu, Mizue Medical Clinic, Keihin Occupational Health Center, Kanagawa, Japan; N. Kato and A. Tomizawa, Fuji Electric Co., Ltd., Kanagawa, Japan; K. Tomita, Mitsubishi Plastics, Inc., Tokyo, Japan; S. Nagahama, All Japan Labour Welfare Foundation, Tokyo, Japan; N. Kunugita and T. Sone, National Institute of Public Health, Saitama, Japan; K. Fukasawa, ADVANTAGE Risk Management Co., Ltd., Tokyo, Japan; A. Hori, C. Nishiura, and C. Kinugawa, Tokyo Gas Co., Ltd., Tokyo, Japan; R. Kuroda and K. Yamamoto, The University of Tokyo, Tokyo, Japan; M. Ohtsu, Himawari Industrial Physician & Occupational Health Consultant Office, Saitama, Japan; D. Omoto, Mitsubishi Heavy Industries, Ltd., Aichi, Japan; N. Sakamoto and Y. Osaki, Health Design Inc., Tokyo, Japan; T. Totsuzaki, Mizuho Health Insurance Society, Tokyo, Japan; M. Endo, Tokyo Women’s Medical University, Tokyo, Japan; T. Itoh, New Japan Radio Co., Ltd., Tokyo, Japan; M. Kawashima, Central Japan Railway Company, Aichi, Japan; M. Masuda, AEON Co., Ltd., Chiba, Japan; C. Nagano, KUBOTA Corporation, Ibaraki, Japan.
References
- 1.Shibuya K, Hashimoto H, Ikegami N, Nishi A, Tanimoto T, Miyata H, Takemi K, Reich MR (2011) Future of Japan’s system of good health at low cost with equity: beyond universal coverage. Lancet 378, 1265–73. [DOI] [PubMed] [Google Scholar]
- 2.Miyata H, Ezoe S, Hori M, Inoue M, Oguro K, Okamoto T, Onishi K, Onozaki K, Sakakibara T, Takeuchi K, Tokuda Y, Yamamoto Y, Yamazaki M, Shibuya K; Health Care 2035 Advisory Panel (2015) Japan’s vision for health care in 2035. Lancet 385, 2549–50. [DOI] [PubMed] [Google Scholar]
- 3.Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, Shibuya K, Kawachi I, Campbell JC (2011) Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. Lancet 378, 1183–92. [DOI] [PubMed] [Google Scholar]
- 4.Arai H, Ouchi Y, Toba K, Endo T, Shimokado K, Tsubota K, Matsuo S, Mori H, Yumura W, Yokode M, Rakugi H, Ohshima S (2015) Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr Gerontol Int 15, 673–87. [DOI] [PubMed] [Google Scholar]
- 5.Hudson RB. (2015) The Need for and the Needs of Older Workers: An International Perspective. Public Policy Aging Rep 25, 117–9. [Google Scholar]
- 6.Suka M, Miwa Y, Ono Y, Yanagisawa H (2013) [Changes in the prevalence of cardiovascular risk factors in Japanese workers during decade 2001–2011] Sangyo Eiseigaku Zasshi 55, 1–10. [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Health, Labour and Welfare (2007) Survey on State of Employees’ Health 2007. http://www.mhlw.go.jp/toukei/itiran/roudou/saigai/anzen/kenkou07/. Accessed May 3, 2016.
- 8.Uehara A, Kurotani K, Kochi T, Kuwahara K, Eguchi M, Imai T, Nishihara A, Tomita K, Yamamoto M, Kuroda R, Nagata T, Omoto D, Murakami T, Shimizu C, Shimizu M, Miyamoto T, Nagahama S, Nakagawa T, Honda T, Yamamoto S, Okazaki H, Sasaki N, Nanri A, Pham NM, Kabe I, Mizoue T, Kunugita N, Dohi S; Japan Epidemiology Collaboration of Occupational Health Study Group (2014) Prevalence of diabetes and pre-diabetes among workers: Japan Epidemiology Collaboration on Occupational Health Study. Diabetes Res Clin Pract 106, 118–27. [DOI] [PubMed] [Google Scholar]
- 9.Kawada T, Okada K (2006) The metabolic syndrome: prevalence and associated lifestyles in Japanese workingmen. J Cardiometab Syndr 1, 313–7. [DOI] [PubMed] [Google Scholar]
- 10.Kawada T, Otsuka T, Inagaki H, Wakayama Y, Li Q, Li YJ, Katsumata M (2011) Optimal cut-off levels of body mass index and waist circumference in relation to each component of metabolic syndrome (MetS) and the number of MetS component. Diabetes Metab Syndr 5, 25–8. [DOI] [PubMed] [Google Scholar]
- 11.Anuurad E, Shiwaku K, Nogi A, Kitajima K, Enkhmaa B, Shimono K, Yamane Y (2003) The new BMI criteria for asians by the regional office for the western pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health 45, 335–43. [DOI] [PubMed] [Google Scholar]
- 12.Japan Organization for Employment of the Elderly, Persons with Disabilities and Job Seekers. 70歳雇用に向けた高年齢者の体力等に関する調査研究結果 http://www.jeed.or.jp/elderly/research/report/elderly/tairyoku.html. Accessed May 3, 2016.
- 13.Ministry of Internal Affairs and Communications (2013) The 2011 Survey on Time Use and Leisure Activities. http://www.stat.go.jp/english/data/shakai/. Accessed June 20, 2016.
- 14.Nanri A, Nakagawa T, Kuwahara K, Yamamoto S, Honda T, Okazaki H, Uehara A, Yamamoto M, Miyamoto T, Kochi T, Eguchi M, Murakami T, Shimizu C, Shimizu M, Tomita K, Nagahama S, Imai T, Nishihara A, Sasaki N, Hori A, Sakamoto N, Nishiura C, Totsuzaki T, Kato N, Fukasawa K, Huanhuan H, Akter S, Kurotani K, Kabe I, Mizoue T, Sone T, Dohi S; Japan Epidemiology Collaboration on Occupational Health Study Group (2015) Development of Risk Score for Predicting 3-Year Incidence of Type 2 Diabetes: Japan Epidemiology Collaboration on Occupational Health Study. PLoS One 10, e0142779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuwahara K, Uehara A, Kurotani K, Pham NM, Nanri A, Yamamoto M, Mizoue T (2014) Association of cardiorespiratory fitness and overweight with risk of type 2 diabetes in Japanese men. PLoS One 9, e98508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuwahara K, Honda T, Nakagawa T, Yamamoto S, Akter S, Hayashi T, Mizoue T (2016) Leisure-time exercise, physical activity during work and commuting, and risk of metabolic syndrome. Endocrine 53, 710–21. [DOI] [PubMed] [Google Scholar]
- 17.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr; . International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–5. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health, Labour and Welfare (2013) Physical activity reference for health promotion 2013. http://www.mhlw.go.jp/stf/houdou/2r9852000002xple-att/2r9852000002xpqt.pdf. Accessed May 3, 2016.
- 19.World Health Organization (2010) Global recommendations on physical activity for health. http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/. Accessed May 3, 2016. [PubMed]
- 20.Nishimura K, Okamura T, Watanabe M, Nakai M, Takegami M, Higashiyama A, Kokubo Y, Okayama A, Miyamoto Y (2014) Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the framingham risk score: the suita study. J Atheroscler Thromb 21, 784–98. [DOI] [PubMed] [Google Scholar]
- 21.Pearson TA, Bazzarre TL, Daniels SR, Fair JM, Fortmann SP, Franklin BA, Goldstein LB, Hong Y, Mensah GA, Sallis JF Jr, Smith S Jr, Stone NJ, Taubert KA; American Heart Association Expert Panel on Population and Prevention Science (2003) American Heart Association guide for improving cardiovascular health at the community level: a statement for public health practitioners, healthcare providers, and health policy makers from the American Heart Association Expert Panel on Population and Prevention Science. Circulation 107, 645–51. [DOI] [PubMed] [Google Scholar]
- 22.Ministry of Health, Labour and Welfare (2015) The National Health and Nutrition Survey in Japan, 2013. http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h25-houkoku.pdf. Accessed June 20, 2016.
- 23.Ministry of Health, Labour and Welfare (2016) The National Health and Nutrition Survey in Japan, 2014. http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h26-houkoku.pdf. Accessed June 20, 2016.
- 24.Hoshuyama T, Hino Y, Kayashima K, Morita T, Goto H, Minami M, Sakuragi S, Tanaka C, Takahashi K (2007) Inequality in the health status of workers in small-scale enterprises. Occup Med (Lond) 57, 126–30. [DOI] [PubMed] [Google Scholar]
- 25.Ministry of Health, Labour and Welfare (2013) The National Health and Nutrition Survey in Japan, 2011. http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h23-houkoku.pdf. Accessed June 20, 2016.
- 26.Lane NE. (2006) Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol 194 Suppl, S3–11. [DOI] [PubMed] [Google Scholar]
- 27.Schmitt NM, Schmitt J, Dören M (2009) The role of physical activity in the prevention of osteoporosis in postmenopausal women-An update. Maturitas 63, 34–8. [DOI] [PubMed] [Google Scholar]
- 28.Ng SW, Popkin BM (2012) Time use and physical activity: a shift away from movement across the globe. Obes Rev 13, 659–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Commissaris DA, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes LL, Hendriksen IJ (2016) Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scand J Work Environ Health 42, 181–91. [DOI] [PubMed] [Google Scholar]
- 30.Sayer AA, Kirkwood TB (2015) Grip strength and mortality: a biomarker of ageing? Lancet 386, 226–7. [DOI] [PubMed] [Google Scholar]
- 31.Endo M, Haruyama Y, Takahashi M, Nishiura C, Kojimahara N, Yamaguchi N (2016) Returning to work after sick leave due to cancer: a 365-day cohort study of Japanese cancer survivors. J Cancer Surviv 10, 320–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsuchiya M, Kawakami N, Ono Y, Nakane Y, Nakamura Y, Fukao A, Tachimori H, Iwata N, Uda H, Nakane H, Watanabe M, Oorui M, Naganuma Y, Furukawa TA, Kobayashi M, Ahiko T, Takeshima T, Kikkawa T (2012) Impact of mental disorders on work performance in a community sample of workers in Japan: the World Mental Health Japan Survey 2002–2005. Psychiatry Res 198, 140–5. [DOI] [PubMed] [Google Scholar]
- 33.Wada K, Higuchi Y, Smith DR (2015) Socioeconomic status and self-reported health among middle-aged Japanese men: results from a nationwide longitudinal study. BMJ Open 5, e008178. [DOI] [PMC free article] [PubMed] [Google Scholar]