Abstract
Objectives
FRAX incorporates rheumatoid arthritis (RA) as a dichotomous predictor for predicting the 10-year risk of hip and major osteoporotic fracture (MOF). However, fracture risk may deviate with disease severity, duration or treatment. Aims were to validate, and if needed to update, UK FRAX for patients with RA and to compare predictive performance with the general population (GP).
Methods
Cohort study within UK Clinical Practice Research Datalink (CPRD) (RA: n=11 582, GP: n=38 755), also linked to hospital admissions for hip fracture (CPRD-Hospital Episode Statistics, HES) (RA: n=7221, GP: n=24 227). Predictive performance of UK FRAX without bone mineral density was assessed by discrimination and calibration. Updating methods included recalibration and extension. Differences in predictive performance were assessed by the C-statistic and Net Reclassification Improvement (NRI) using the UK National Osteoporosis Guideline Group intervention thresholds.
Results
UK FRAX significantly overestimated fracture risk in patients with RA, both for MOF (mean predicted vs observed 10-year risk: 13.3% vs 8.4%) and hip fracture (CPRD: 5.5% vs 3.1%, CPRD-HES: 5.5% vs 4.1%). Calibration was good for hip fracture in the GP (CPRD-HES: 2.7% vs 2.4%). Discrimination was good for hip fracture (RA: 0.78, GP: 0.83) and moderate for MOF (RA: 0.69, GP: 0.71). Extension of the recalibrated UK FRAX using CPRD-HES with duration of RA disease, glucocorticoids (>7.5 mg/day) and secondary osteoporosis did not improve the NRI (0.01, 95% CI −0.04 to 0.05) or C-statistic (0.78).
Conclusions
UK FRAX overestimated fracture risk in RA, but performed well for hip fracture in the GP after linkage to hospitalisations. Extension of the recalibrated UK FRAX did not improve predictive performance.
Keywords: Epidemiology, Osteoporosis, Rheumatoid Arthritis
Introduction
Rheumatoid arthritis (RA) is a systemic inflammatory disease characterised by destruction of periarticular bone and joint structures and has been associated with osteoporosis.1 2 The risk of hip fracture,3–5 morphometric or clinical spine fracture2 6 and of other fractures is increased.3 5 The underlying reasons for the increased fracture risk in RA are complex. They may include chronic inflammation, inactivity and an increased risk of falling.1 7 RA has therefore been incorporated as a dichotomous predictor in the WHO FRAX algorithm for predicting the 10-year risk of hip or major osteoporotic fracture (MOF; hip, clinical spine, forearm, humerus).8
There is, however, uncertainty about the predictive performance of FRAX in RA.9 FRAX may underestimate fracture risk in patients with more severe RA, since it does not take the underlying disease activity and resulting joint damage into account. Conflicting results have been reported for correlation of the Health Assessment Questionnaire with clinical fracture risk, which is an often used measure for functional ability in RA,10–12 and limited evidence has shown higher fracture risk with longer duration of disease.3 13 On the other hand, FRAX may overestimate fracture risk due to higher mortality among patients with RA as compared with the general population,3 14 since FRAX adjusts fracture risk for competing mortality risk. Furthermore, the role of glucocorticoids on fracture risk in RA is uncertain where fracture risk was found to be independent of glucocorticoid use,3 but preservation of bone mineral density (BMD) has also been described with use of low-dose oral glucocorticoids (GCs).15–18
Therefore, this study aimed to validate UK FRAX for the 10-year risk of hip or MOF in patients with RA and to compare predictive performance with the general population. If needed, methods to recalibrate or extend UK FRAX were applied to improve its predictive performance.
Methods
Source population
A cohort study was conducted within the Clinical Practice Research Datalink (CPRD) (http://www.cprd.com). This database contains computerised medical records of 625 primary care practices in the UK, representing 8% of the total population. Data recorded in CPRD include demographic information, laboratory tests, primary care diagnoses, specialist referrals, hospital admissions, prescription details and lifestyle variables such as body mass index (BMI), smoking status and alcohol consumption. Previous studies have shown high validity of hip fracture registration (>90% was confirmed),19 and high degrees of accuracy and completeness of data have been shown for other diagnoses and mortality.20–23 Linkage of CPRD data to Hospital Episode Statistics (CPRD-HES) was eligible for 62% of the population captured within CPRD, all residing in England. Linkage to HES provides all hospital admissions including the date of discharge and the cause. Approval for this study was given by Independent Scientific Advisory Committee (ISAC) for Medicines and Healthcare product Regulatory Agency (MHRA) Database Research (protocol number 15_023A).
Study population
Data between 1 January 1987 and 31 December 2013 were extracted from CPRD. HES diagnoses were available between 1 April 1997 and 31 December 2013. We selected all patients with RA at 1 January 2004 (index date), who also had ≥1 year of data collection before the index date. We chose 1 January 2004 as the index date to allow for follow-up of 10 years. RA was defined by a previously validated algorithm24; ≥1 disease-modifying antirheumatic drug (DMARD) prescription after first RA diagnosis code. In line with FRAX, all patients had to be between 40 and 90 years at the index date and were excluded when they were exposed to any antiosteoporosis drug (AOD; bisphosphonates, raloxifene, strontium ranelate, denosumab, parathyroid hormone) ever before the index date.
We matched up to four controls from the general population to every patient with RA by age, sex and practice in order to directly compare the predictive performance of FRAX between the RA cohort and the general population.
Outcomes
The occurrence of hip fracture and the composite of MOF (first of hip, forearm, clinical spine, humerus) were ascertained by medical codes in CPRD. Hip fractures were measured in CPRD-HES by International Classification of Diseases and Related Health problems (ICD)-10 codes S72.0, S72.1 and S72.2.
Definition of predictors
In records before the index date, FRAX predictors were determined: age at index date, sex, BMI (most recent), previous fracture at any site (ever before, yes/no), current smoking status (most recent; yes/no), alcohol use (most recent medical code for alcohol abuse or for alcohol use where the daily number of units was ≥3, yes/no), oral glucocorticoid use (prescription within 90 days before or ≥two prescriptions with a mean daily dose of prednisolone (equivalents) of ≥5 mg in the year before, yes/no), RA (ever before,24 yes/no) and secondary osteoporosis (ever before, medical code for type 1 diabetes mellitus, osteogenesis imperfecta, hypogonadism, premature menopause, malnutrition or malabsorption or chronic liver disease, yes/no). A parental history of hip fracture was not available. Therefore, we calculated a weighted average of the risks when assuming a parental hip fracture and by assuming absence of parental hip fracture based on a prevalence of parental hip fracture of 12%.8 An RA-specific predictor, duration of RA disease, was defined as years between the date of RA diagnosis and the index date.3 Rheumatoid factor-positive RA was not included because of unrealistically low prevalence (1.9%). Finally, oral glucocorticoid use was alternatively defined by mean daily dose in the year before (<2.5, 2.5–7.5 and >7.5 mg/day).
Missing values for BMI, smoking status and alcohol use were imputed by multiple imputation using all predictors and the outcome variable, resulting in five imputed datasets. Analysis by multiple imputation gives unbiased results under the less restrictive missing at random assumption instead of missing completely at random, and generally less bias than complete case analysis if data are missing not at random.
Statistical analyses
Predicted 10-year risks of hip fracture and MOF were calculated by UK FRAX (FRAX desktop V.3.9) without information on BMD for every patient. This was repeated for each imputed dataset to provide the mean predicted risks (95% CI). The observed 10-year risk of hip fracture and MOF was estimated by the cumulative incidence function (%) to comply with the outcome definition of FRAX, where fracture risk is adjusted for mortality risk (ie, sustaining a fracture within remaining lifetime up to 10 years), and to account for loss to follow-up.25 Fractures were measured between index date and death, end of the study period (truncated at 10 years following index date, 31 December 2013) or moving out of CPRD, whichever came first. Predictive performance was assessed by measures of discrimination (C-statistic) and calibration (on average and by percentiles of predicted risk). In a sensitivity analysis, observed risks among those using AODs after index date were increased inversely proportional to the estimated effect of AODs on hip fracture (assuming a relative risk of 0.526) to determine the influence of AOD use on the average observed risk.
Recalibration was performed for hip fracture in CPRD-HES by fitting the log-odds transformed FRAX probabilities (ie, the linear predictor) as a single continuous covariate in a logistic regression model with hospitalisation for hip fracture within 10 years as the outcome variable (CPRD-HES provided full coverage for hip fracture).27 28 Thereafter, individual FRAX predictors were added to the linear predictor to determine whether these had an additional predictive effect, and also glucocorticoid dose and duration of RA disease were included. Interactions between the linear predictor and FRAX predictors, glucocorticoid dose and duration of RA disease were also tested. The final (updated) model was derived by including all variables and interactions that were significantly related to hip fracture risk in a multivariable model and then performing backward elimination. In a sensitivity analysis, AOD treatment after the index date and its interaction terms were included into the model.
We determined whether hip fracture prediction was improved for the extended model compared with the recalibrated UK FRAX model in terms of discrimination (C-statistic) and category-based Net Reclassification Improvement (NRI).29 30 The NRI incorporates age-specific intervention thresholds set by the National Osteoporosis Guideline Group, which are linked to FRAX output in the UK. Positive NRI values indicate adequate reclassification of risk, whereas negative values indicate inadequate reclassification of risk. Bootstrapping (500 repetitions) was performed to correct the C-statistic for optimism.31 A shrinkage factor was applied to the β-coefficients of the final models. All statistical analyses were performed using SAS V.9.4 (SAS, Cary, North Carolina, USA). A p value <0.05 was considered statistically significant.
Results
A total of 16 331 patients with RA were identified, of which 1031 were excluded because they were aged <40 or >90 years, and 3718 because they were previously exposed to an AOD. This left 11 582 patients with RA for analyses with 297 and 808 incident cases of hip fracture and MOF and 2733 deaths in CPRD, respectively. HES linkage reduced the number of patients with RA to 7221 (247 hip fractures, 1699 deaths). Table 1 details the characteristics of the RA population in CPRD and in CPRD-HES. The matched cohort from the general population comprised 38 755 individuals with 536 and 1925 incident cases of hip fracture and MOF, and 5636 deaths in CPRD, respectively. HES linkage reduced the number to 24 227 (476 hip fractures, 3550 deaths).
Table 1.
Characteristics of the RA study population in CPRD and in CPRD-HES
| Characteristic | CPRD (n=11 582) |
CPRD-HES (n=7221) |
|---|---|---|
| Median follow-up, years (IQR) | 9.0 (4.7–10) | 9.0 (5.3–10) |
| Sex, n (%) | ||
| Male | 3729 (32.2) | 2263 (31.3) |
| Female | 7853 (67.8) | 4958 (68.7) |
| Age, years, mean (±SD) | 62.9 (11.4) | 63.0 (11.5) |
| Body mass index, kg/m2, mean (±SD) | 26.8 (5.3) | 26.7 (5.3) |
| Missing | 1780 (15.4) | 1086 (15.0) |
| Current smoking, n (%) | 4147 (35.8) | 2573 (35.6) |
| Missing, n (%) | 890 (7.7) | 547 (7.6) |
| Alcohol use ≥3 units per day, n (%) | 580 (5.0) | 371 (5.1) |
| Missing, n (%) | 1759 (15.2) | 1081 (15.0) |
| Previous fracture, n (%) | 1908 (16.5) | 1184 (16.4) |
| Glucocorticoid use yes/no*, n (%) | 1806 (15.6) | 1176 (16.3) |
| Glucocorticoid use, daily dose†, mean (±SD) | 4.9 (3.2) | 4.9 (3.2) |
| 0<GC<2.5 mg/day, n (%) | 508 (4.4) | 295 (4.1) |
| 2.5≤GC≤7.5 mg/day, n (%) | 1160 (10.0) | 786 (10.9) |
| >7.5 mg/day, n (%) | 305 (2.6) | 200 (2.8) |
| Secondary osteoporosis, n (%) | 580 (5.0) | 372 (5.2) |
| Age of RA onset, years, mean (±SD) | 52.8 (13.5) | 52.8 (13.7) |
| RA disease duration, years, mean (±SD) | 10.1 (9.2) | 10.2 (9.3) |
| <2 years since diagnosis | 1336 (11.5) | 824 (11.4) |
| 2–10 years since diagnosis | 5900 (50.9) | 3671 (50.8) |
| >10 years since diagnosis | 4346 (37.5) | 2726 (37.8) |
*Glucocorticoid use was defined as in FRAX: prescription within 90 days before or ≥two prescriptions with a mean daily dose of prednisolone (or equivalents) of ≥5 mg in the year before.
†Glucocorticoid use was defined as ≥two prescriptions with a mean daily dose of prednisolone (or equivalents) of <2.5, 2.5–7.5 or >7.5 mg/day in the year before.CPRD, Clinical Practice Research Datalink; GC, oral glucocorticoids; HES, Hospital Episode Statistics; RA, rheumatoid arthritis.
UK FRAX overestimated fracture risk among the RA population in CPRD, both for MOF (mean predicted vs observed 10-year risk: 13.3% vs 8.4%, 95% CI 7.8 to 9.0) and for hip fracture (5.5% vs 3.1%, 95% CI 2.8 to 3.5) (figure 1). Linkage to hospitalisation data for hip fracture attenuated the overestimation, but it remained significant (5.5% vs 4.1%, 95% CI 3.6 to 4.6) (figure 2A). The AOD-adjusted mean observed risk was 4.6% (25% received an AOD). C-statistics were 0.78 and 0.69 for hip fracture and MOF, respectively.
Figure 1.

Calibration plot for prediction of (A) major osteoporotic fracture and (B) hip fracture by UK FRAX (Clinical Practice Research Datalink) among patients with rheumatoid arthritis, by percentiles of predicted risk.
Figure 2.

Calibration plot for prediction of hip fracture by UK FRAX (Clinical Practice Research Datalink-Hospital Episode Statistics) among (A) patients with rheumatoid arthritis and (B) the general population, by percentiles of predicted risk.
In the general population, UK FRAX also overestimated the risk of MOF (8.6% vs 6.2%, 95% CI 5.9 to 6.4) and hip fracture in CPRD (2.7% vs 1.8%, 95% CI 1.6 to 1.9). After linkage to hospitalisations, there was close agreement between predicted and observed risks of hip fracture (2.7% vs 2.4%, 95% CI 2.2 to 2.7) (figure 2B). The AOD-adjusted mean observed risk was 2.5% (6% received an AOD). C-statistics were 0.83 and 0.71 for hip fracture and MOF, respectively.
The higher observed risk of hip fracture in CPRD-HES as compared with CPRD indicates underascertainment of hip fractures in CPRD. Updating of UK FRAX was therefore not performed for MOF, but only for hip fracture in CPRD-HES for patients with RA. The recalibrated UK FRAX model for hip fracture in RA is shown in table 2. The extended model included the linear predictor, duration of RA disease and its interaction with the linear predictor, high-dose glucocorticoids (>7.5 mg/day) and secondary osteoporosis (table 2). In sensitivity analyses, AOD treatment and its interaction with the linear predictor were dropped from the recalibrated model (adjusted (adj.) OR for AOD treatment: 0.6, 95% CI 0.3 to 1.1, adj. OR for interaction: 0.8, 95% CI 0.7 to 1.1) and the extended model (adj. ORs of 0.6, 95% CI 0.3 to 1.1 and 0.8, 95% CI 0.7 to 1.1), respectively, during backward elimination.
Table 2.
Recalibrated and extended UK FRAX for 10-year risk of hip fracture (CPRD-HES) in RA
| β-coefficient | OR (95% CI) | Shrunken β-coefficient* | |
|---|---|---|---|
| Recalibrated UK FRAX | |||
| Intercept | −1.085 | – | −1.080 |
| UK FRAX† | 0.757 | 2.13 (1.92 to 2.37) | 0.749 |
| Extended UK FRAX | |||
| Intercept | −0.728 | – | −0.713 |
| UK FRAX† | 0.939 | 2.56 (2.17 to 3.02) | 0.921 |
| Secondary osteoporosis (yes/no) | 0.521 | 1.68 (1.04 to 2.74) | 0.511 |
| Glucocorticoid >7.5 mg/day (yes/no) | −1.303 | 0.27 (0.09 to 0.87) | −1.276 |
| Duration of RA disease (per year increase) | −0.029 | 0.97 (0.95 to 0.99) | −0.029 |
| Duration of RA disease† UK FRAX† | −0.015 | 0.99 (0.98 to 0.99) | −0.015 |
*The shrunken β-coefficients were derived by applying the shrinkage factor (0.98 for the extended model and 0.99 for the recalibrated model) to the original β-coefficients.
†Log odds transformed 10-year risks of hip fracture (ln(probhip/(1 − probhip)) as derived from the original UK FRAX algorithm.
CPRD, Clinical Practice Research Datalink; HES, Hospital Episode Statistics; RA, rheumatoid arthritis.
Calibration of the extended model was good (intercept: 0.00, β-linear predictor: 1.02) (figure 3). The C-statistic was 0.78. Extension did not improve correct classification of hip fracture cases and non-cases when compared with the recalibrated UK FRAX model with an NRI of 0.01 (95% CI −0.04 to 0.05) (table 3).
Figure 3.
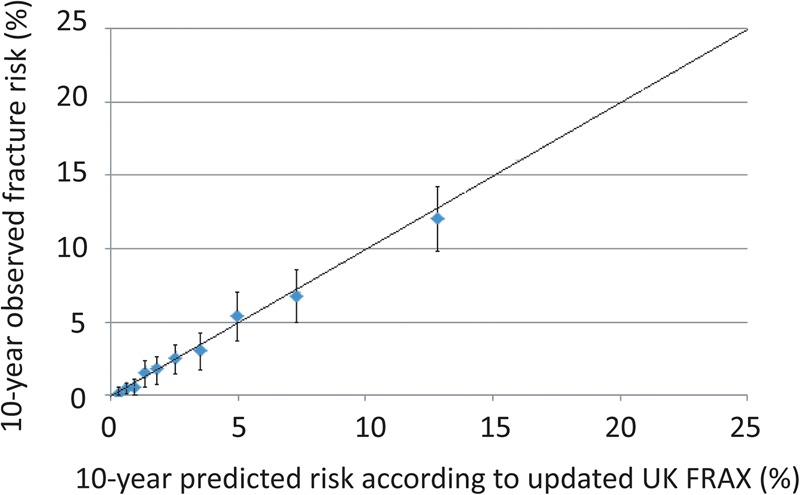
Calibration plot for prediction of hip fracture by the updated UK FRAX (Clinical Practice Research Datalink-Hospital Episode Statistics) among patients with rheumatoid arthritis, by percentiles of predicted risk.
Table 3.
Reclassification of hip fracture cases and non-cases with RA (CPRD-HES) with addition of duration of RA disease, high-dose glucocorticoids and secondary osteoporosis to the recalibrated UK FRAX model, using age-specific NOGG intervention thresholds*
| Extended UK FRAX | ||||
|---|---|---|---|---|
| Recalibrated UK FRAX | Above threshold | No change | Below threshold | Total |
| Total, n | 407 | 6508 | 306 | 7221 |
| Hip fracture cases, n | 18 | 216 | 13 | 247 |
| Hip fracture non-cases, n | 389 | 6292 | 293 | 6974 |
*The intervention threshold is set at the probability of hip fracture equal to that of a woman, with BMI 24 kg/m2, and prior fracture, for a specific year of age and is applied to both men and women.
BMI, body mass index; CPRD, Clinical Practice Research Datalink; HES, Hospital Episode Statistics; NOGG, National Osteoporosis Guideline Group; RA, rheumatoid arthritis.
Discussion
UK FRAX overestimated the risk of hip fracture and MOF in CPRD for both the RA population and the general population. Linkage to hip fracture hospitalisations changed this finding, where calibration was good for the general population but overestimation of UK FRAX for hip fracture remained among patients with RA. Discrimination was good for hip fracture and moderate for MOF in both populations. Extension of the recalibrated UK FRAX model for RA with duration of RA disease, high-dose glucocorticoids, and secondary osteoporosis did not improve predictive performance.
Little is known about fracture risk assessment in RA32 33 and we are not aware of studies that have determined discrimination and calibration of FRAX, which has been developed and validated in the general population, in this subpopulation. Lee et al33 applied the Korean FRAX algorithm to 545 Korean patients with RA, and found no difference in fracture incidence between those who met the FRAX thresholds for treatment and those who had osteoporosis. However, the Korean FRAX model was not validated, which limits the interpretation of results.
In order to determine whether external influences other than RA itself influenced the performance of FRAX, we have also evaluated FRAX in a random sample from the general population. Worldwide, a limited number of independent external validation studies have been performed for FRAX and even fewer have assessed calibration.34 To date, one study has evaluated calibration of FRAX in the general population of the UK.35 This study was performed in the QResearch primary care database, where UK FRAX overestimated hip fracture risk in each percentile of predicted risk. This finding was likely the result of underascertainment of (hip) fractures in primary care data. Indeed, we found calibration to be improved upon linkage of CPRD to HES data. It remains, however, unclear how well UK FRAX calibrates for MOF risk. The higher discrimination of FRAX for hip fracture as compared with MOF is well in line with findings from other external validation studies.34 This may be the result of a different association of risk factors for different fracture types.35
A possible explanation for the overestimation of hip fracture risk by FRAX in RA is higher competing mortality as compared with the general population.14 36 Their lifespan is reduced by 3–10 years, for which no improvement has been found over the past decades.14 36 Also, all patients with RA were exposed to DMARDs. These drugs have been associated with a protective effect on loss of BMD and reduced fracture risk, but evidence has been conflicting.9 37 Biologics are now frequently used among patients with RA and may further reduce fracture risk, although the adjusted risk of non-vertebral fracture has been reported to be similar across patients with RA starting a tumour necrosis factor-α inhibitor, methotrexate or other non-biologic DMARDs.37 In addition, AOD treatment may have influenced observed fracture risks, but our results suggest that the overestimation of FRAX was (largely) independent of AOD treatment status. The adjusted observed risk for hip fracture remained lower than predicted when we assumed a 50% relative risk reduction among all patients treated with AOD. Similarly, a Canadian prospective cohort study found that AOD treatment status did not appear to interfere with the predictive performance of the Canadian FRAX algorithm in the general population.38 Treatment duration influenced this finding for hip fracture but not for MOF, where observed risks were significantly lower than predicted among patients adhering to AOD treatment for at least 5 years. The insufficient adherence to AOD treatment in clinical practice is well known, which has been shown to blunt the antifracture effectiveness, and may explain the independence of FRAX calibration from AOD treatment status.39
The finding that overestimation of UK FRAX for risk of hip fracture increased with longer duration of RA may relate to increased competing mortality with longer duration of RA disease,36 and greater loss of BMD during recent onset of disease. Second, patients with RA, who were exposed to high-dose glucocorticoids, had a lower risk of hip fracture, which was independent from the risk of hip fracture with use of glucocorticoids as defined in FRAX. The role of glucocorticoids on fracture risk in RA is not well understood. Inconsistent results were reported for the association between bone loss and exposure to low-dose to medium-dose glucocorticoids.15–18 40 Our finding may be related to increased mortality among those who are treated with high-dose GCs.41 42 The present study, however, was not designed to determine the causal association between glucocorticoid dose and hip fracture risk in RA. And third, secondary osteoporosis was selected as a predictor for the 10-year risk of hip fracture on top of FRAX. FRAX neglects the influence of secondary osteoporosis when RA is present, but our finding is not in line with this assumption. Most importantly, however, is that our results show that their addition to the recalibrated UK FRAX did not improve identification of RA individuals at high risk of hip fracture.
This study has several strengths. The included patients with RA were representative for the general RA population with a similar age at onset of RA disease and gender distribution as was previously reported.43 44 In addition, this is the first study that provides results for calibration of UK FRAX for RA and also for the general population, where hip fractures were completely captured and which enabled 10 years of follow-up. A limitation was that we had no data on BMD and RA disease severity parameters besides duration of RA disease.9 When access to dual-energy x-ray absorptiometry (DXA) is limited,45 46 however, FRAX without BMD may be used instead and a strong correlation between fracture risks by FRAX with and without BMD has been shown.47 Furthermore, information on parental hip fracture was not available. Therefore, we have calculated weighted average risks by assuming the prevalence of parental hip fracture as was observed in the FRAX developmental cohorts. This was done not to influence the average calibration and to evaluate methods to improve this, and this method resulted in good calibration of FRAX for hip fracture in the general population. We were also not able to determine whether duration of RA disease interacted with the individual predictors since β-coefficients of the original FRAX algorithm are not publicly available.
In conclusion, UK FRAX overestimated hip fracture and MOF risk in RA and in the general population when fractures were measured in primary care data. Linkage to hospitalisations for hip fracture showed good calibration for the general population, but overestimation remained in the RA population. Discrimination was good for hip fracture and moderate for MOF in both populations. Updating of UK FRAX for RA beyond recalibration did not improve predictive performance for hip fracture.
Acknowledgments
We wish to acknowledge Ms Thomas for providing the RA diagnostic medical code lists, which were used for validation of RA diagnosis in the former version of Clinical Practice Research Datalink (general practice research database; GPRD).
Footnotes
Contributors: Conceived and designed the experiments: CK FdV JWJB, HGML and PMJW. Analysed the data: CK and PMJW. Wrote the paper: CK. Reviewed the manuscript: CK, FdV, JWJB, HGML and PMJW.
Funding: This study was supported by a research grant from the Netherlands Organization for Health Research and Development (ZonMw; grant number 113101007).
Competing interests: The Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, employing authors CK and FdV, has received unrestricted funding from the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (ZIN), the Royal Dutch Pharmacists Association (KNMP), the private–public funded Top Institute Pharma (http://www.tipharma.nl), includes cofunding from universities, government and industry, the EU Innovative Medicines Initiative (IMI), the EU 7th Framework Program (FP7), the Dutch Ministry of Health and industry (including GlaxoSmithKline, Pfizer and others); HGML is a researcher at The WHO Collaborating Centre for Pharmaceutical Policy and Regulation, which receives no direct funding or donations from private parties, including pharma industry. Research funding from public–private partnerships, for example, IMI, TI Pharma (http://www.tipharma.nl) is accepted under the condition that no company-specific product or company-related study is conducted. The Centre has received unrestricted research funding from public sources, for example, the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), the EU 7th Framework Program (FP7), the Dutch Medicines Evaluation Board (MEB) and the Dutch Ministry of Health.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kaz H, Johnson D, Kerry S, et al. . Fall-related risk factors and osteoporosis in women with rheumatoid arthritis. Rheumatology (Oxford) 2004;43:1267–71. 10.1093/rheumatology/keh304 [DOI] [PubMed] [Google Scholar]
- 2.Ørstavik RE, Haugeberg G, Mowinckel P, et al. . Vertebral deformities in rheumatoid arthritis. A comparison with population-based controls. Arch Intern Med 2004;164:420–5. 10.1001/archinte.164.4.420 [DOI] [PubMed] [Google Scholar]
- 3.van Staa TP, Geusens P, Bijlsma JW, et al. . Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum 2006;54:3104–12. 10.1002/art.22117 [DOI] [PubMed] [Google Scholar]
- 4.Huusko TM, Korpela M, Karppi P, et al. . Threefold increased risk of hip fractures with rheumatoid arthritis in Central Finland. Ann Rheum Dis 2001;60:521–2. 10.1136/ard.60.5.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim SY, Schneeweiss S, Liu J, et al. . Risk of osteoporotic fracture in a large population-based cohort of patients with rheumatoid arthritis. Arthritis Res Ther 2010;12:R154 10.1186/ar3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spector TD, Hall GM, McCloskey EV, et al. . Risk of vertebral fracture in women with rheumatoid arthritis. BMJ 1993;306:558 10.1136/bmj.306.6877.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smulders E, Schreven C, Weerdesteyn V, et al. . Fall incidence and fall risk factors in people with rheumatoid arthritis. Ann Rheum Dis 2009;68:1795–6. 10.1136/ard.2009.109009 [DOI] [PubMed] [Google Scholar]
- 8.Kanis JA, Oden A, Johnell O, et al. . The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporosis Int 2007;18:1033–46. 10.1007/s00198-007-0343-y [DOI] [PubMed] [Google Scholar]
- 9.Broy SB, Tanner SB, on behalf of the FRAX® Position Development Conference Members . Official positions for FRAX® clinical regarding rheumatoid arthritis. From Joint Official Positions development conference of the international society for clinical densitometry and international osteoporosis foundation on FRAX. J Clin Densitom 2011;14:184–9. 10.1016/j.jocd.2011.05.012 [DOI] [PubMed] [Google Scholar]
- 10.Coulson KA, Reed G, Gilliam BE, et al. . Factors influencing fracture risk, T score, and management of osteoporosis in patients with rheumatoid arthritis in the consortium of rheumatology researchers of North America (CORRONA) registry. J Clin Rheum 2009;15:155–60. 10.1097/RHU.0b013e3181a5679d [DOI] [PubMed] [Google Scholar]
- 11.Furuya T, Kotake S, Inoue E, et al. . Risk factors associated with incident clinical vertebral and nonvertebral fractures in Japanese women with rheumatoid arthritis: a prospective 54-month observational study. J Rheumatol 2007;34:303–10. [PubMed] [Google Scholar]
- 12.Michel BA, Bloch DA, Wolfe F, et al. . Fractures in rheumatoid arthritis: an evaluation of associated risk factors. J Rheumatol 1993;20:1666–9. [PubMed] [Google Scholar]
- 13.El Maghraoui A, Rezqi A, Mounach A, et al. . Prevalence and risk factors of vertebral fractures in women with rheumatoid arthritis using vertebral fracture assessment. Rheumatology (Oxford) 2010;49:1303–10. 10.1093/rheumatology/keq084 [DOI] [PubMed] [Google Scholar]
- 14.Myasoedova E, Davis JM III, Crowson CS, et al. . Epidemiology of rheumatoid arthritis: rheumatoid arthritis and mortality. Curr Rheumatol Rep 2010; 12:379–85. 10.1007/s11926-010-0117-y [DOI] [PubMed] [Google Scholar]
- 15.Capell HA, Madhok R, Hunter JA, et al. . Lack of radiological and clinical benefit over two years of low dose prednisolone for rheumatoid arthritis: results of a randomised controlled trial. Ann Rheum Dis 2004;63:797–803. 10.1136/ard.2003.014050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boers M, Verhoeven AC, Markusse HM, et al. . Randomised comparison of combined step-down prednisolone, methotrexate and sulphasalazine with sulphasalazine alone in early rheumatoid arthritis. Lancet 1997;350:309–18. 10.1016/S0140-6736(97)01300-7 [DOI] [PubMed] [Google Scholar]
- 17.Laan RF, van Riel PL, van de Putte LB, et al. . Low-dose prednisone induces rapid reversible axial bone loss in patients with rheumatoid arthritis. A randomized, controlled study. Ann Intern Med 1993;119:963–8. 10.7326/0003-4819-119-10-199311150-00001 [DOI] [PubMed] [Google Scholar]
- 18.Svensson B, Boonen A, Albertsson K, et al. . Low-dose prednisolone in addition to the initial disease-modifying antirheumatic drug in patients with early active rheumatoid arthritis reduces joint destruction and increases the remission rate: a two-year randomized trial. Arthritis Rheum 2005;52:3360–70. 10.1002/art.21298 [DOI] [PubMed] [Google Scholar]
- 19.Van Staa TP, Abenhaim L, Cooper C, et al. . The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf 2000;9:359–66. [DOI] [PubMed] [Google Scholar]
- 20.Herrett E, Thomas SL, Schoonen WM, et al. . Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 2010;69:4–14. 10.1111/j.1365-2125.2009.03537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract 2010;60:e128–36. 10.3399/bjgp10X483562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewis JD, Brensinger C. Agreement between GPRD smoking data: a survey of general practitioners and a population-based survey. Pharmacoepidemiol Drug Saf 2004;13:437–41. 10.1002/pds.902 [DOI] [PubMed] [Google Scholar]
- 23.Dregan A, Moller H, Murray-Thomas T, et al. . Validity of cancer diagnosis in a primary care database compared with linked cancer registrations in England. Population-based cohort study. Cancer Epidemiol 2012;36:425–9. 10.1016/j.canep.2012.05.013 [DOI] [PubMed] [Google Scholar]
- 24.Thomas SL, Edwards CJ, Smeeth L, et al. . How accurate are diagnoses for rheumatoid arthritis and juvenile idiopathic arthritis in the general practice research database? Arthritis Rheum 2008;59:1314–21. 10.1002/art.24015 [DOI] [PubMed] [Google Scholar]
- 25.Leslie WD, Lix LM, Wu X, et al. . Competing mortality and fracture risk assessment. Osteoporos Int 2013;24:681–8. 10.1007/s00198-012-2051-5 [DOI] [PubMed] [Google Scholar]
- 26.Murad MH, Drake MT, Mullan RJ, et al. . Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J Clin Endocrinol Metab 2012;97:1871–80. 10.1210/jc.2011-3060 [DOI] [PubMed] [Google Scholar]
- 27.Janssen KJM, Moons KGM, Kalkman CJ, et al. . Updating methods improved the performance of a clinical prediction model in new patients. J Clin Epidemiol 2008;61:76–86. 10.1016/j.jclinepi.2007.04.018 [DOI] [PubMed] [Google Scholar]
- 28.Steyerberg EW. Clinical prediction models: A practical approach to development, validation, and updating. Springer, 2009. [Google Scholar]
- 29.Leening MJ, Vedder MM, Witteman JC, et al. . Net Reclassification Improvement: computation, interpretation, and controversies: a literature review and clinician's guide. Ann Intern Med 2014;160:122–31. 10.7326/M13-1522 [DOI] [PubMed] [Google Scholar]
- 30.Cook NR, Ridker PM. Advances in measuring the effect of individual predictors of cardiovascular risk: the role of reclassification measures. Ann Intern Med 2009;150:795–802. 10.7326/0003-4819-150-11-200906020-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brigham & Women's Hospital. Division of Preventative Medicine. Risk prediction modeling. SAS Macro's. http://ncook.bwh.harvard.edu/sas-macros.html (assessed 26 Sept 2015).
- 32.Furuya T, Hosoi T, Saito S, et al. . Fracture risk assessment and osteoporosis treatment disparities in 3,970 Japanese patients with rheumatoid arthritis. Clin Rheumatol 2011;30:1105–11. 10.1007/s10067-011-1748-8 [DOI] [PubMed] [Google Scholar]
- 33.Lee JH, Suh YS, Koh JH, et al. . The risk of osteoporotic fractures according to the FRAX model in Korean patients with rheumatoid arthritis. J Korean Med Sci 2014;29:1082–9. 10.3346/jkms.2014.29.8.1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marques A, Ferreira RJ, Santos E, et al. . The accuracy of osteoporotic fracture risk prediction tools: a systematic review and meta-analysis. Ann Rheum Dis 2015;74:1958–67. 10.1136/annrheumdis-2015-207907. [DOI] [PubMed] [Google Scholar]
- 35.Hippisley-Cox J, Coupland C. Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ 2009;339:b4229 10.1136/bmj.b4229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radovits BJ, Fransen J, Al Shamma S, et al. . Excess mortality emerges after 10 years in an inception cohort of early rheumatoid arthritis. Arthritis Care Res (Hoboken) 2010;62:362–70. 10.1002/acr.20105 [DOI] [PubMed] [Google Scholar]
- 37.Kim SY, Schneeweiss S, Liu J, et al. . Effects of disease-modifying antirheumatic drugs on nonvertebral fracture risk in rheumatoid arthritis: a population-based cohort study. J Bone Miner Res 2012;27:789–96. 10.1002/jbmr.1489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leslie WD, Lix LM, Johansson H, et al. , Manitoba Bone Density Program. Does osteoporosis therapy invalidate FRAX for fracture prediction? J Bone Miner Res 2012;27:1243–51. 10.1002/jbmr.1582 [DOI] [PubMed] [Google Scholar]
- 39.Ross S, Samuels E, Gairy K, et al. . A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 2011;14:571–81. 10.1016/j.jval.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 40.van Everdingen AA, Jacobs JW, Siewertsz Van Reesema DR, et al. . Low-dose prednisone therapy for patients with early active rheumatoid arthritis: clinical efficacy, disease-modifying properties, and side effects: a double-blind placebo-controlled clinical trial. Ann Intern Med 2002;136:1–12. 10.7326/0003-4819-136-1-200201010-00006 [DOI] [PubMed] [Google Scholar]
- 41.Del Rincón I, Battafarano DF, Restrepo JF, et al. . Glucocorticoid dose thresholds associated with all-cause and cardiovascular mortality in rheumatoid arthritis. Arthritis Rheumatol 2014;66:264–72. 10.1002/art.38210 [DOI] [PubMed] [Google Scholar]
- 42.Schols AM, Wesseling G, Kester AD, et al. . Dose dependent increased mortality risk in COPD patients treated with oral glucocorticoids. Eur Respir J 2001;17:337–42. 10.1183/09031936.01.17303370 [DOI] [PubMed] [Google Scholar]
- 43.Solomon DH, Massarotti E, Garg R, et al. . Association between disease-modifying antirheumatic drugs and diabetes risk in patients with rheumatoid arthritis and psoriasis. JAMA 2011;305:2525–31. 10.1001/jama.2011.878 [DOI] [PubMed] [Google Scholar]
- 44.Crane MM, Juneja M, Allen J, et al. . Epidemiology and treatment of New-Onset and Established Rheumatoid Arthritis in an Insured US Population. Arthritis Care Res (Hoboken) 2015;67:1646–55. 10.1002/acr.22646 [DOI] [PubMed] [Google Scholar]
- 45.Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 2005;16:229–38. 10.1007/s00198-004-1811-2 [DOI] [PubMed] [Google Scholar]
- 46.Curtis JR, Laster A, Becker DJ, et al. . The geographic availability and associated utilization of dual-energy X-ray absorptiometry (DXA) testing among older persons in the United States. Osteoporos Int 2009;20:1553–61. 10.1007/s00198-008-0821-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leslie WD, Morin S, Lix LM, et al. . Fracture risk assessment without bone density measurement in routine clinical practice. Osteoporos Int 2012;23:75–85. 10.1007/s00198-011-1747-2 [DOI] [PubMed] [Google Scholar]


