Abstract
Juxta-articular cysts are synovial cysts originating from the facet joints or the flava ligaments. If they grow intra-spinally they can compress nervous structures and cause a variety of symptoms. Micro-neurosurgery is usually the treatment of choice. Alternatively to surgical treatment the cyst can be approached and treated with a CT guided percutaneous injection inducing rupture. After fulfilling strict selection criteria twenty patients (25% of all treated lumbar synovial cyst patients), were treated minimally invasive by this method from 2010-2016. The facet joint was punctured under CT guidance and a mixture of a local anesthetic and contrast liquid was injected until the cyst was blasted. The mean follow-up period was 1.1 years (range 2 weeks - 5 years).
Fifteen of twenty procedures were successful and cyst rupture was confirmed by CT-scans. Twelve of these fifteen patients experienced a significant improvement of their symptoms and needed no further intervention or surgical procedure up until now, three patients showed no clinical improvement and were treated surgically within one week after cyst rupture. In five patients it was technically not possible to rupture the cyst. These patients were treated microsurgically by cyst resection and dynamic stabilization or fusion procedures. The percutaneus rupture of juxtaarticular cysts has fewer risks and is cost effective compared to microsurgical resection. It may be an alternative to surgical treatment for a selected group of patients. However there are some limitations to the procedure though, such as difficult patient selection, unpredictable outcome or technical problems due to highly degenerated facet joints.
Key words: Synovial cyst, microsurgical decompression, CT-guided cyst rupture
Introduction
Synovial juxta-articular cysts are dilatations of the synovia, extruding from the facet joints and causing possible instability as well as back- or radicular pain.1 There are various methods of treatment, starting from microsurgical decompression,1-4 decompressive laminectomy,2 hemilaminoplasty,5 concomitant or subsequent fusion,6,7 conservative treatment,2 and CT- or ultrasound guided intra-cystic steroid injections.8,9
As mentioned before, compression of the nervous structures can lead to radicular pain and development of neurological symptoms.4,10 However, there are reports of spontaneous regression of such cysts,7,11 as well as intradural invasion12 or spontaneous hemorrhage causing a cauda equina syndrome or bilateral foot drop.13,14 The clinical symptoms can differ and are difficult to predict.
There are also studies differentiating true synovial cysts with a thick wall of synovial cells from pseudocysts with a collagenous capsule containing myxoid material, which lack specialized epithelium and are considered as pseudocystic degeneration of the lumbar ligamentum flavum.4,7
The treatment of synovial cysts is discussed quite controversially in literature. There are reports of spontaneous cyst regression as well as regression after anti-inflammatory drug treatment with Cox-2 inhibitors.7,12 There are also reports showing that cysts can lead to cauda equina syndrome and have deleterious outcomes for patients.7 There is no need to treat asymptomatic cysts and a conservative treatment can be applied in symptomatic small cysts without neurological deficits in our opinion. Most of the reports deal with microsurgical treatment of synovial cysts.1-4 In one report surgical decompression with or without fusion is recommended as first line treatment since CT-guided cysts aspiration is associated with a 50-100% failure rate.1 The authors report a resolution of clinical symptoms after surgical decompression of 92%.1 Additionally they discuss the role of a stabilization, which remains controversial. Interestingly similar outcomes after surgical decompression were reported by another group even after a follow up time of 4 years.18 Other authors recommend surgical decompression after failure of conservative treatment.2 To the best of our knowledge there are no literature reports on use of dynamic stabilization additional to microsurgical decompression of facet joint cysts. And even though fusion procedures are reported in this entity it is still a matter of debate.1 Moreover overtreatment of these patients may be possible. Of course the treatment strategy (decompression with or without stabilization) depends on radiographic signs of instability15 and on the intraoperative situation. On the other hand there are a number of reports stating an excellent outcome after CT-guided intracystic and intraarticular steroid injections.8 One study of 120 patients showed that 54% of patients were satisfied after first intracystic injection, and 20% after a second injection.8 In sum 75% of patients were satisfied with intracystic injection treatment according to the study.8 There are a few other studies reporting similar good results with a CT-guided cyst injection. Even ultrasound-guided cyst-injection with a complete cyst resolution after 4 months has been reported.9 In the present study we demonstrate our results of CT-guided percutaneous injection of a mixture of local anesthetic and contrast liquid into lumbar cysts in respect to a follow up time of 1.1 years. Inclusion criteria were clear radicular pain due to the synovial cysts without additional hypertrophy of ligamentum flavum or massive degeneration of facet joint.
Materials and Methods
This outpatient procedure is performed under local anaesthesia and usually takes 10-15 minutes. A 20 G spinal needle is placed directly into the facet joint under CT-guidance and a 3 mL syringe with Luer® fitting to allow attachment of a syringe with 1:1 mixture of local anaesthetic (Maevarin® Actavis 1%) and contrast medium (Solutrast® 370) is connected and injected into the joint space in attempt to rupture the cyst. If the rupture of the cyst does not occur after the first 3 mL of solution is injected, additional 3 mL mixture of local anaesthetic and contrast solution is injected. The communication between the facet joint and synovial cyst is shown in simultaneously performed facet joint arthrogram. In case of successful rupture of the cyst, contrast medium emission into the epidural space is visible in CT scan, the patients usually feel slight radicular pain when the cyst is inflated and instant pain relief after rupture of the cyst. The success of this treatment is dependent on a communication between the facet joint and the synovial cyst, since we never perform direct cyst puncture.
From 2010-2016 we treated 20 patients with synovial cysts of the lumbar spine region with this technique. During the same time period we treated 59 patients with symptomatic lumbar synovial cysts by microsurgical decompression with or without additional instrumentation. The patients treated by this minimal invasive method make up a minority (25%) of our surgically treated lumbar synovial cyst population. All patients which were symptomatic from underlying lumbar stenosis, sponylarthrosis, degenerative spondylolisthesis and instability were primarily excluded from this method and considered for surgical treatment instead.
The mean follow-up period was 1.3 years (2 weeks - 5 years), the patients were examined clinically and the pain scores (Oswestry disability index score (ODI), visual analog scale score (VAS) for back and leg) were collected. Ten patients received an MRI at the point of last follow up. The patients charts were evaluated retrospectively and the patients were interviewed via phone call. In seven patients the Oswestry disability index was reported, and in 10 the visual analog scale score for the lumbar spine and the lower extremity was evaluated before treatment and in the last follow up. t-test statistical analysis was performed for the ODI and VAS scores in the pre- and post-treated patients.
Results
Fifteen patients were successfully treated with percutaneous cyst injection, in five patients rupturing of the cyst failed. The mean age was 63.5 years (19-86 years). Nine patients were males and eleven females. In fourteen patients (70%) the cyst was in L4/5, in one L5/S1 (5%) and in five in L3/4 (25%). In five out of twenty patients the rupture of the cyst after injection was not possible and in four of these cases the cyst was removed microsurgically. One patient after unsuccessful cyst rupture experienced temporary relief of symptoms of about 50% after conservative treatment with periradicular infiltrations and facet joint injections. This relief lasted for a few weeks, then symptoms returned and microsurgical decompression was performed in another hospital two months later. Five months after microsurgical decompression, fusion of the segment was performed due to the segmental instability with increased back pain. Immediately after injection treatment thirteen of twenty (65%) patients reported an improvement of their symptoms, mainly improvement of lumboischialgic pain. Three of twenty (15%) patients successfully treated showed a disappearance of their cysts in initial CT scans but no improvement of their clinical signs. These patients were treated by microsurgical decompression and dynamic stabilization within the first week after initial treatment.
There were no complications related to this treatment in any of the patients. In one case of unsuccessful cyst rupture the patient suffered an increase of radicular pain due to cyst enlargement without rupture. In this case microsurgical decompression was performed the next day, as there was no need of emergency surgery since the patient did not show any neurological deficits.
In ten of the twelve patients who improved after cyst rupture we evaluated the VAS for the lumbar spine and lower extremity. The ODI was evaluated in seven of twelve patients. Figure 1 A, B and C demonstrate the pre- and post-interventional changes of the ODI Score as well as VAS for lumbar pain and pain in lower extremity. Figure 2 illustrates the changes of mean values pre- and post-treatment ODI and VAS.
Figure 1.
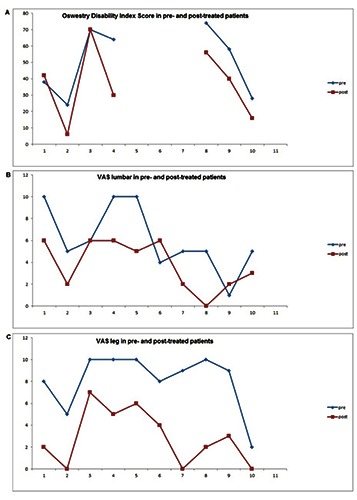
Outcome of 10 patients after intracystic local anaesthetic - contrast solution injection with cyst rupture after a mean follow up of 7 months. Oswestry disability score pre and post-injection in patients 1-4 and 8-10. The ODI decreases after treatment. However the difference is not significant. Visual analog scale (VAS) for lumbal pain shows a decrease in VAS score after treatment; VAS for leg pain shows a decrease in the VAS score after treatment (Blue: pre-treatment, red: posttreatment).
Figure 2.
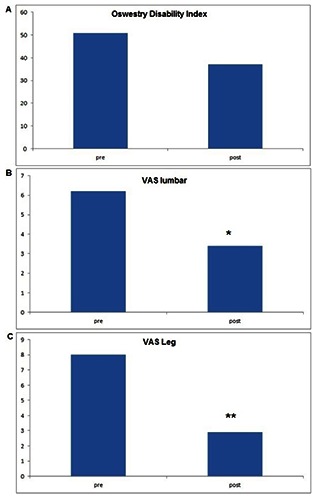
Mean scores of ODI and VAS 7 months after treatment. ODI mean score decreases after treatment. The change is not statistically significant; VAS for lumbar pain decreases after treatment significantly (P<0.05); VAS for leg pain decreases after treatment significantly (P<0.01).
The improvement of clinical symptoms and the decrease of the VAS value for the lower extremity from a mean of 6.2 in the pretreated patients to 2.9 after treatment was statistically significant (P<0.01).
The decrease of the VAS score for lumbar pain after treatment was statistically significant (P<0.05). The change in the ODI score was not significant since the patient number was too small. In the following we give the clinical and radiological description of two illustrative cases.
Illustrative Case 1
A 19 y.o. male with lumboischialgic pain for 10 months with failed conservative treatment asked for alternatives to the fusion procedure indicated elsewhere. The pain radiated from the lumbar area to the lateral part of the leg on the right side. The ODI score was 24 and the VAS back 5/10, VAS leg 2/10. The MRI of the lumbar spine revealed a juxta-articular cyst in L3/4 on the right side. The origin of the cyst was not the facet joint as initially assumed, but the lytic defect in L4. We placed the needle in the lytic defect and successfully ruptured the cyst. Figure 3 illustrates the pre- and post-treatment MRI. After treatment and in the follow up examination after 4 months the ODI score was 6 and the pain in the VAS back and leg was 2/10. The patient was satisfied and did not ask for further treatment.
Figure 3.
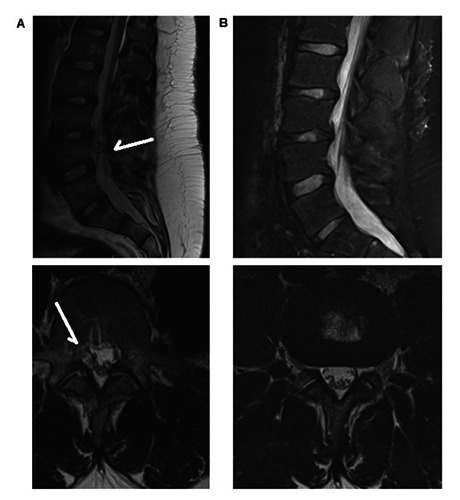
Illustrative case 1: MRIs of a 19 y.o. male with a synovial cyst. Sagittal and transversal sections (T2 weighted) showing the cyst behind lytic defect in L4; 4 months after treatment the cyst disappeared (arrow: cyst).
Illustrative Case 2
The second case is a 68 y.o. female with radicular pain, with an ODI score of 38 and VAS score of 10/10 lumbar and 10/10 for the right lower extremity. One year after percutaneous injection and rupture of the cyst the ODI remained at 32 but the VAS score was 0/10 for lumbar and lower extremity pain. Patient remained very satisfied also at the last follow up 2.8 years after treatment. Figure 4 illustrates the pre-, and the one-year post-traetment MRI.
Figure 4.
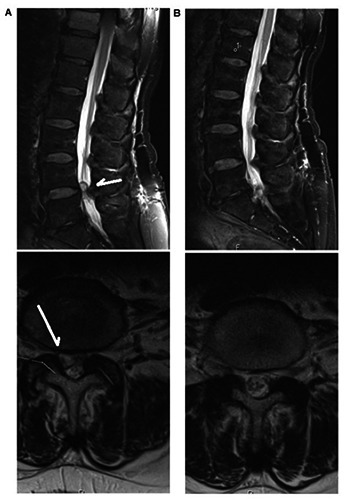
Illustrative case 2: 68 y.o. female patient. Pre-treatment MRIs showing the cyst in L4/5. 1 year after treatment the cyst disappeared (arrow: cyst).
Discussion
Synovial cysts may have serious implications for patients and have to be treated in case of onset clinical symptoms after unsuccessful conservative treatment. Since there are different kinds of such cysts the treatment response to different therapies varies. The invasive treatment of lumbar synovial cysts still remains controversial. An individualized treatment strategy for every patient considering age, anatomy, risk factors, neurological presentation, calcification and cyst size has to be planned. Concomitant pathologic findings such as hypertrophy and ossification of ligamentum flavum or segmental instability, as well as general health condition also have to be considered. According to literature it seems that the best surgical treatment option for these patients is surgical decompression with cyst removal. It is still not clear if additional fusion brings clinical improvement. With surgical decompression the results are excellent with a success rate of about 90% and a need for a second surgery because of recurrence of just 6%.1 One of the main complications with surgery is that of dural tears and CSF leaks. To avoid this risk Scholz et al, left a part of the cyst and did not proceed to complete removal. In none of these patients did a recurrence occur in a minimum follow up time of one year.16 Since aspiration of cyst has a failure rate of 50-100% this method is clearly not the method of choice.
Many excellent outcomes after CT-guided intra-cystic and intra-articular injections were reported after minimaly invasive percutaneus treatment of the symptomatic lumbar synovial cysts. Like the study of Amoretti et al.8 with a failure rate of 25%, we also experienced a failure rate of 25% in our patients. In all five cases with unsuccessful treatment, the patients were treated surgically.
In our study the outcome was not satisfying in three cases although the cysts were ruptured, these patients were treated surgically within the first week after rupture. The reason why the therapy was primarily not satisfying in these cases remains unclear. Overall success rate in our study was twelve out of twenty (60%) of all treated patients or twelve out of fifteen (80%) in cases of successful cyst rupture. These patients experienced significant benefit and avoided surgery or hospitalization. Considering the average operative time of 106 minutes and a hospitalization length of stay of approximately 5 days, which had been reported in the study of Kaminsky and Banse,17 this should acclaim a good reason to add this less invasive procedure for suitable patients as an additive to our armamentarium. We consider this treatment primarily in patients with non-calcified cysts and without general spinal canal stenosis or ligamentum flavum thickening and without preoperative instability. This method is also a good option for patients, which are at the high risk for surgeries under general anesthesia. On the other hand, if younger patients in good general health also fulfill these criteria we would consider this minimally invasive treatment as a choice in order to avoid surgical treatment. It is essential to inform the patient about the expected success rate of approximately 50-75% as reported in literature18,19 in order to avoid disappointment if treatment fails. If the patients do not profit though we do not proceed to a second trial, patients are then treated microsurgicaly. The main reason to apply cyst injection is the avoidance of surgical complications like dural tear with injury of nerve roots and CSF leakage. One of the main problems of the method is to puncture the cyst in case of degeneration. New methods with the use of navigational software are offering some help here.20 As stated in the review of Epstein and Baisden there is another problem in the use of cyst injections. The ease of use lead to an immense increase of using and abusing the method of 231% with an increase of total reimbursement from 24 million $ to 175 million $ showing that the method is used too deliberately.
Conclusions
Microsurgical decompression with or without stabilization remains the treatment of choice in symptomatic synovial cysts. In patients with non-calcified synovial cysts without hypertrophy of ligamenta flava and instability in the lumbar spine a treatment with a CT-guided percutaneous injection of local anesthetic - contrast medium mixture should be considered since a 50-75% rate of a satisfying outcome has been reported and was also confirmed in our study. Should such a therapeutic trial fail, microsurgical decompression is still the therapy of choice.
A limitation of the study is its retrospective character. Not every patient got an ODI score and some received only a VAS score, which makes the data heterogenous and limits our conclusion.
References
- 1.Epstein NE, Baisden J. The diagnosis and management of synovial cysts: efficacy of surgery versus cyst aspiration. Surg Neurol Int 2012;3:S157-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.el Bashir F, Ajani O. Management of lumbar spine juxtafacet cysts. World Neurosurg 2012;77:141-6. [DOI] [PubMed] [Google Scholar]
- 3.El Shazly AA, Khattab MF. Surgical excision of a juxtafacet cyst in the lumbar spine: a report of thirteen cases with long-term follow up. Asian J Neurosurg 2011;6:78-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jankowski R, Szymas J, Nowak S, et al. Synovial cysts of the lumbar spine. Neurol Nneurochir Polska 2012;46:456-61. [DOI] [PubMed] [Google Scholar]
- 5.Zhenbo Z, Huanting L, Jin W, et al. Hemilaminoplasty for the treatment of lumbar intraspinal synovial cysts (LISCs) and literature review. Eur Spine J 2016;25:3393-402. [DOI] [PubMed] [Google Scholar]
- 6.Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg 2000;93:53-57. [DOI] [PubMed] [Google Scholar]
- 7.Mattei TA, Goulart CR, McCall TD. Pathophysiology of regression of synovial cysts of the lumbar spine: the ‘anti-inflammatory hypothesis’. Med Hypoth 2012;79:813-8. [DOI] [PubMed] [Google Scholar]
- 8.Amoretti N, Huwart L, Foti P, et al. Symptomatic lumbar facet joint cysts treated by CT-guided intracystic and intra-articular steroid injections. Eur Radiol 2012;22:2836-40. [DOI] [PubMed] [Google Scholar]
- 9.Lin TL, Chung CT, Lan HH, Sheen HM. Ultrasound-guided facet joint injection to treat a spinal cyst. J Chinese Med Assoc 2014;77:213-6. [DOI] [PubMed] [Google Scholar]
- 10.Kalevski SK, Haritonov DG, Peev NA. Lumbar intraforaminal synovial cyst in young adulthood: case report and review of the literature. Global Spine J 2014;4:191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ngo T, Decina P, Hsu W. Spontaneous resolution of symptoms associated with a facet synovial cyst in an adult female - a case report. J Canadian Chiropractic Assoc 2013;57:87-92. [PMC free article] [PubMed] [Google Scholar]
- 12.Bae JS, Lee SH, Kim JS, et al. Intradural invasion of lumbar synovial cyst. Case report. Neurol Medico-Chir 2012;52:234-7. [DOI] [PubMed] [Google Scholar]
- 13.George K, Roy D, Shad A. Haemorrhage into juxta-facet cysts causing bilateral foot drop. J Surg Case Rep 2012;2012:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Machino M, Yukawa Y, Ito K, et al. Spontaneous hemorrhage in an upper lumbar synovial cyst causing subacute cauda equina syndrome. Orthopedics 2012;35:e1457-60. [DOI] [PubMed] [Google Scholar]
- 15.Wildi LM, Kurrer MO, Benini A, et al. Pseudocystic degeneration of the lumbar ligamentum flavum: a little known entity. J Spinal Disord Techn 2004;17:395-400. [DOI] [PubMed] [Google Scholar]
- 16.Scholz C, Hubbe U, Kogias E, Klingler J-H. Incomplete resection of lumbar synovial cysts - evaluating the risk of recurrence. Clin Neurol Neurosurg 2015;136:29-32. [DOI] [PubMed] [Google Scholar]
- 17.Kaminski L, Banse X. Time spent per patient in lumbar spinal stenosis surgery. Eur Spine J 2013;22:1868-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau NJ, Kaplan PA, Dussault RG. Lumbar facet joint synovial cyst: percutaneous treatment with steroid injections and distention - clinical and imaging follow-up in 12 patients. Radiology 2001;221: 179-85. [DOI] [PubMed] [Google Scholar]
- 19.Sabers SR, Ross SR, Grogg BE, Lauder TD. Procedure-based nonsurgical management of lumbar zygapophyseal joint cyst-induced radicular pain. Archiv Phys Med Rehab 2005;86:1767-71. [DOI] [PubMed] [Google Scholar]
- 20.Wang DJ, Lownie SP, Pelz D, Pandey SA. novel approach to symptomatic lumbar facet joint synovial cyst injection and rupture using iGuide navigational software: a case report and review. Interv Neuroradiol 2016;22:596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


