Abstract
Pain management after total knee arthroplasty (TKA) and total hip arthroplasty should permit early mobilization with minimal pain. Local infiltration analgesia (LIA) is a new popular method for decreasing postoperative pain. The goal of this meta-analysis is to evaluate the efficacy of LIA in comparison with epidural analgesia. A literature search was performed in PubMed, EMBASE, the OVID database, Web of Science, and the Cochrane Library databases. The risk of bias was assessed using the Cochrane collaboration tool. Outcomes of interest included visual analog scale score, range of flexion, length of stay, and complications. Nine trials involving 537 patients met the inclusion criteria. LIA provides better pain relief and larger range of motion in TKA patients compared to epidural analgesia at the late postoperative period. No significant difference was observed in regard to the length of stay and complications. The current evidence shows that the use of local infiltration is effective for postoperative pain management in TKA patients. More high-quality randomized controlled trials with long-term follow-up are required for examining the long-term efficacy and safety of local infiltration.
KEY WORDS: Total knee arthroplasty, total hip arthroplasty, local infiltration, epidural analgesia, meta-analysis
INTRODUCTION
Total joint arthroplasty such as total knee arthroplasty or total hip arthroplasty (TKA or THA) is one of the most successful surgical treatments for patients with end-stage osteoarthritis. It is estimated that over 700,000 joint replacements are performed in the United States each year [1]. Pain control and comfort level are linked to earlier mobilization and initiation of physiotherapy, better range of motion, decreased length of hospital stay and risk of postoperative complications, and improved patient satisfaction [2].
Epidural analgesia consisting of a local anesthetic agent and an opioid has been a regular regimen used for postoperative analgesia after total joint arthroplasty [3]. However, some studies have indicated that the benefit of epidural analgesia must be weighed against the frequency of its adverse effects such as urinary retention, hypotension, pruritus, and motor block that delays mobilization [4,5]. In recent years, there is a growing interest in the use of local infiltration analgesia (LIA) containing various constituents as a modality of postoperative pain control. The LIA technique was originally performed by Bianconi et al. [6] and Kerr and Kohan [7] with promising results. The advantage of LIA is the ability to provide pain control without interfering with lower extremity motor strength, thereby allowing early mobilization of patients [7]. Studies have shown that LIA is consistently more effective in the treatment of postoperative pain after TKA or THA when compared with placebo [8,9]. Comparison between LIA and epidural analgesia was conducted by several authors, which was more convincing to illustrate its superiority [10-18]. Tsukada et al. [16] have shown that local infiltration was associated with a lower visual analog scale (VAS) score and better flexion motion than epidural analgesia, while Jules-Elysee et al. [14] reported that epidural analgesia provided less opioid and a lower VAS score. Regarding different studies, analgesic advantage and functional benefits of LIA versus epidural analgesia remain a debate. Therefore, this meta-analysis was designed to quantitatively assess the clinical efficacy and safety of LIA compared with epidural analgesia in TKA or THA.
MATERIALS AND METHODS
PubMed, Cochrane Library, Web of Science, OVID, and EMBASE were searched up to October 2015. The search terms included “local infiltration”, “periarticular injection”, “intra-articular injection”, “knee arthroplasty”, “knee replacement”, “hip arthroplasty”, and “hip replacement”. No restrictions were imposed on language. Reference lists of all the eligible studies and relevant reviews were hand searched for any additional trials.
Inclusion criteria and study selection
We identified randomized controlled trials (RCTs) comparing LIA with epidural analgesia group following THA/TKA. Any type of local infiltration (both periarticular infiltration and intra-articular infiltration) and any type of medication (both single infiltration and continuous infiltration) were included. The primary outcomes included pain score at rest or on movement. Secondary outcomes included a range of flexion, length of hospital stay, and complications. Articles that reported at least one outcome were included. Letters, comments, editorials, practice guidelines, and trials published without the outcome measures of interest were excluded. Two authors independently assessed potentially relevant citations for inclusion; disagreements were resolved with a third author.
Data abstraction and quality assessment
Data were extracted independently by two reviewers. Full texts of any potentially useful studies were reviewed, disagreements regarding which studies to include were resolved by discussion. Data regarding the patient characteristics, intervention, and outcomes were extracted in duplicate by two authors using a standardized form. The postoperative pain intensity was measured by a 10 points VAS. When a numerical rating scale score was used, it was converted to a VAS score. Data in other forms (i.e., median, interquartile range, and mean ± 95% confidence interval [CI]) were converted to mean ± standard deviation (SD) according to Cochrane Handbook. If the data were not reported numerically, we extracted them by manual measurements from the published figures.
Two authors assessed the risk of bias of the included studies independently. Possible biases were recorded in a Cochrane risk of bias table. Random sequence generation, allocation concealment, blinding of participants and personnel, blind outcome assessment, incomplete outcome data, selective reporting, and other sources of bias were measured with care.
Statistical analysis
Review Manager Software (Revman 5.3, Cochrane Collaboration, Oxford, United Kingdom) was used for the meta-analysis. The heterogeneity of the studies was tested using the I2 statistic and Chi-squared tests. A fixed-effects model was used when the heterogeneity test did not reveal statistical significance (I2 < 50%). Otherwise, the random effects model was used. Mean difference (MD) with 95% CI was calculated for the continuous data and relative risk (RR) with 95% CI for the dichotomous data.
RESULTS
Search results
After comprehensive searches, 1354 citations were found. We excluded 549 duplicates and 789 citations after screening the titles and abstracts. After reading full texts, 7 citations which did not fulfill the inclusion criteria were excluded. Finally, 9 RCTs were identified in our study (Figure 1) [10-18].
FIGURE 1.
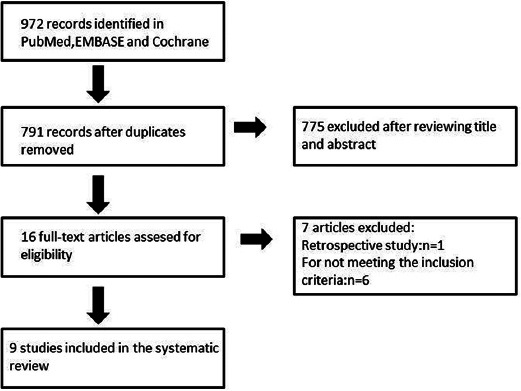
The flow chart of literature screening.
The characteristics of the included studies are presented in Table 1. Six hundred and seven TKAs (local infiltration/epidural analgesia: n = 302/305) in 537 patients (bilateral/unilateral: n = 70/467) were performed in 9 RCTs. The baseline characteristics between the two groups were well matched in each trial. One study investigated the effect of LIA by placement of a bilateral TKA.
TABLE 1.
Characteristics of included studies

Study quality
Of the nine included studies, eight were randomized by computer generated numbers or random table using sealed envelopes, while one study did not mention its design. Only two trials were double-blind to patients and outcome assessors while four were not able to be blinded for the trial designs and three did not mention it. The methodological quality of included studies is seen in Figure 2.
FIGURE 2.
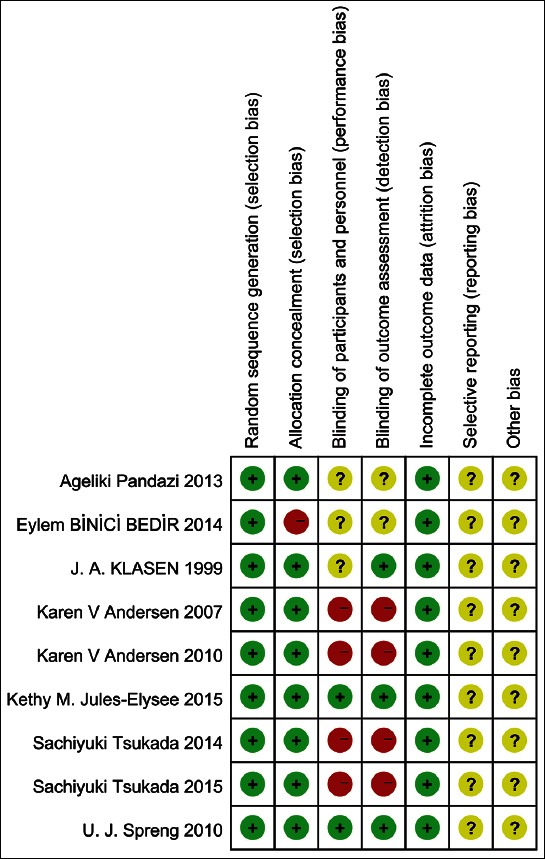
Risk bias of the included studies.
Results of the meta-analysis
VAS score at rest
Five studies with 272 patients showed a VAS score at 12 hours postoperatively [12,13,15,16,18]. No significant difference was found between local infiltration and epidural analgesia (Figure 3A) (MD = −0.42; 95% CI = −1.03-0.20).
FIGURE 3.
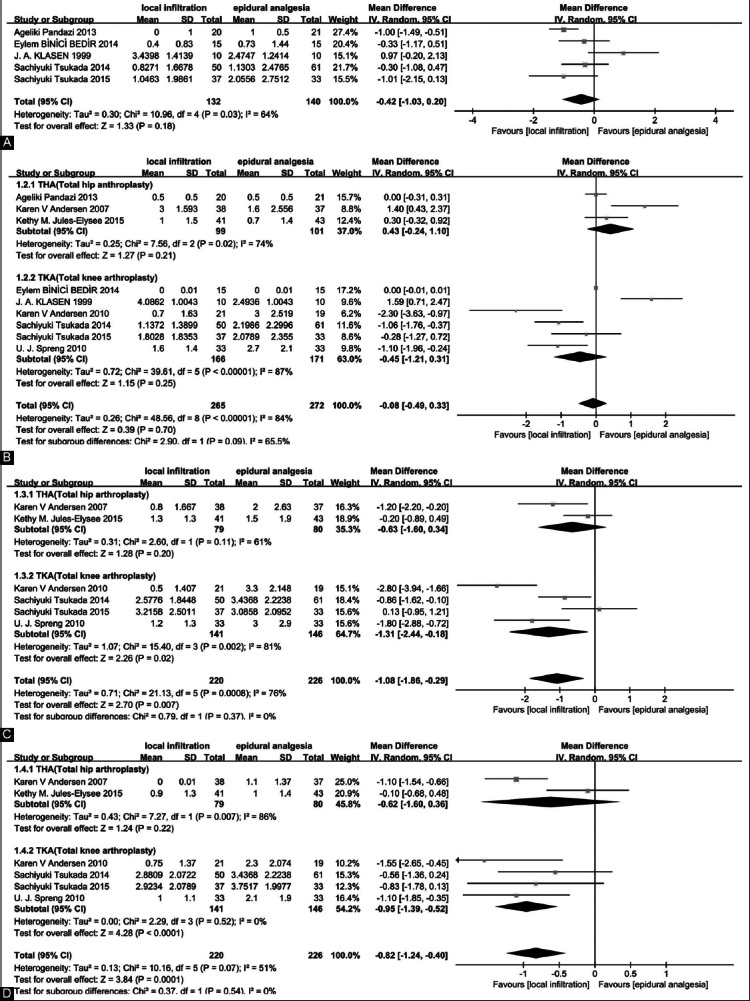
Analysis of the visual analog scale score at rest at 12 (A), 24 (B), 48 (C), and 72 hours (D) postoperatively.
Nine studies, which included RCTs with 537 patients, showed a VAS score at 24 hours postoperatively [10-18]. The meta-analysis showed no significant difference (Figure 3B) (MD = −0.08; 95% CI = −0.49-0.33). The subgroup analysis showed the same result.
Six studies with 446 patients showed a VAS score at 48 and 72 hours postoperatively [10,11,13,14,16,17]. The meta-analysis reported that local infiltration had a lower VAS score than epidural analgesia (Figure 3C and D) (MD = −1.08; 95% CI = −1.86 to −0.29 and MD = −0.82; 95% CI = −1.24 to −0.4). In the subgroup analysis of THA [14,17], the meta-analysis of two studies showed no significant difference between local infiltration and epidural analgesia at 48 and 72 hours postoperatively. However, the results combined from four studies [10,11,13,16] showed that in TKA local infiltration significantly reduced the VAS score at 48 and 72 hours.
VAS score on movement
The VAS score showed no significant differences between the two groups at 24 hours (MD = 0.38; 95% CI = −0.37-1.12) (Figure 4A) [10,11,14-17]. However, in THA [14,15,17], epidural analgesia showed a reduced VAS score, while in TKA [10,11,16], there was no statistical difference. In THA [14,17], no significant difference was observed between the two groups on movement at 48 and 72 hours postoperatively (Figure 4B and C) (at 48 hours: MD = −0.33; 95% CI = −2.48-1.82; at 72 hours: MD = −0.99; 95% CI = −3.74-1.75). On the contrary, in TKA [10,11,16], local infiltration had lowered VAS score on movement at 48 hours postoperatively (MD = −1.08; 95% CI = −1.86 to −0.29).
FIGURE 4.
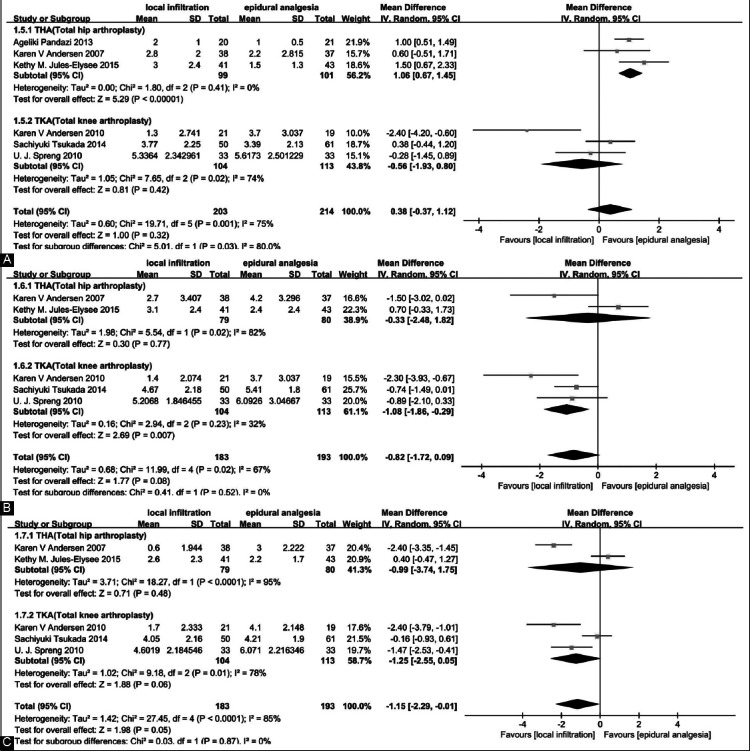
Analysis of the visual analog scale score on movement at 24 (A), 48 (B), and 72 hours (C) postoperatively.
Range of knee flexion
Three studies [11,13,16] reporting a range of knee flexion were included in the meta-analysis. Local infiltration had better flexion at 24, 48, and 72 hours (MD = 7.2; 95% CI = 3.16-11.23; MD = 6.69; 95% CI = 3.78-9.59 and MD = 5.19; 95% CI = 0.95-9.44) (Figure 5A-C).
FIGURE 5.
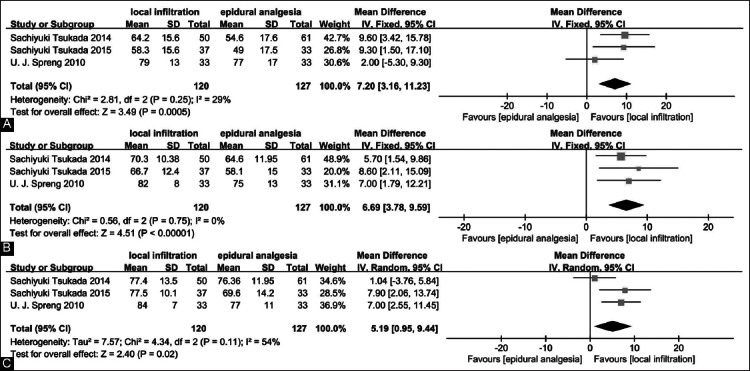
Analysis of the flexion angle at 24 (A), 48 (B), and 72 hours (C) postoperatively.
Length of hospital stay
Pooling four trials [10,11,14,17] with 265 patients, the results showed that local infiltration failed to reduce the length of hospital stay (MD = −1.12; 95% CI = −2.33-0.09) (Figure 6).
FIGURE 6.
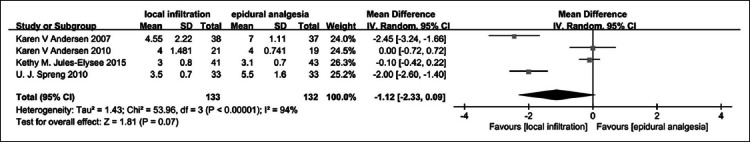
Analysis of the length of hospital stay.
Complications
The meta-analysis of five studies [11-13,16,17] revealed no significant difference in the incidence of nausea between the two groups (RR = 0.46; 95% CI = 0.19-1.11) (Figure 7A). The meta-analysis of four studies [11,13,16,17] showed there was no statistical difference between local infiltration and epidural analgesia (RR = 2.02; 95% CI = 0.51-7.99) (Figure 7B).
FIGURE 7.
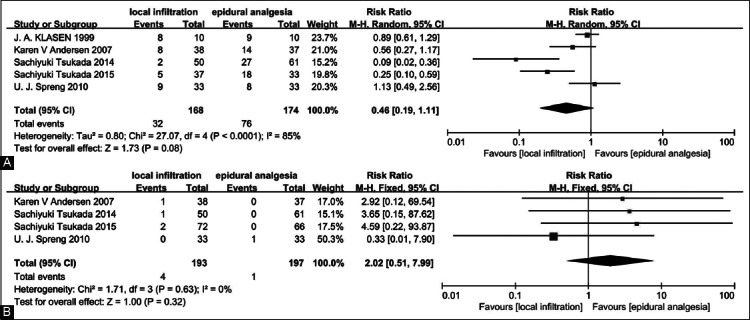
Analysis of the complications such as nausea (A) and wound infection (B).
DISCUSSION
To our knowledge, this is the first meta-analysis of RCTs comparing the efficacy and safety of local infiltration with epidural analgesia in the management of postoperative pain in THA and TKA. The most important finding of this study was that in TKA local infiltration may have better pain relief in the late postoperative period compared with epidural analgesia, and in the early postoperative period, local infiltration provided postoperative analgesia comparable to that of epidural analgesia. Moreover, there was no significant difference in pain relief between local infiltration and epidural analgesia both in the early postoperative period and in the late postoperative period in THA.
Pain intensity was measured as VAS score at 12, 24, 48, and 72 hours after THA and TKA. In THA, local infiltration showed no superiority in analgesic effects over epidural analgesia both at rest and on movement, while in TKA local infiltration showed better pain relief in the late postoperative period both at rest and on movement compared to epidural analgesia. The different outcome between THA and TKA may be due to the different pain intensities between THA and TKA. The different outcome between early and late postoperative periods may be due to short time pain relief of epidural analgesia. Choi et al. [4] discussed epidural analgesia or systemic analgesia in patients undergoing hip or knee replacement in a Cochrane review and concluded that the beneficial effect of epidural analgesia on pain relief was limited to the early postoperative period.
With respect to functional recovery, local infiltration had a wider range of flexion at 24, 48, and 72 hours postoperatively. This may be explained by the fact that the pain scores were consistently lower in the local infiltration group when compared with the epidural analgesia. Mullaji et al. [19] suspected that the duration of the effect of methylprednisolone acetate led to extended pain control, thereby aiding flexion. Additionally, because local infiltration affects only the surgical area with moderate analgesia, there is limited interference to muscle strength of the lower limb. The application of continuous epidural analgesia has been reported to lengthen motor block compared to LIA [20]. Thus, improved mobilization was observed in the local infiltration group [7].
Regarding the length of hospital stay, our study failed to demonstrate any significant difference in the length of hospital stay between the two groups. The length of hospital stay following TKA and THA depends on many factors including factors unrelated to the patient’s medical or rehabilitation status.
Although we observed some differences when comparing the incidence of nausea between the two groups, there were no significant differences showing the method of local infiltration being better or worse. Also, there was no difference in wound infection between the two groups. In a meta-analysis of studies involving the continuous infusion of local anesthetic into the surgical wound after various surgical procedures, Liu et al. [21] found that there was no statistically significant difference in wound infection rates between patients who received active treatment (0.7%) and those who received placebo treatment (1.2%).
Considerable heterogeneity across the trials exists in our meta-analysis which might have a bias impact on our results. This could be the result of non-standardized local infiltration and different administration methods and study designs. First, the cocktail content differed from each other. Six studies [10,11,13,15-17] used ropivacaine, two studies [14,18] used bupivacaine, six studies [11-16] used morphine, five studies [10,11,13,16,17] used ketorolac, and four studies [13-16] used corticosteroid. Ropivacaine has the similar efficiency to bupivacaine but is associated with a longer acting and fewer complications in the nervous and cardiovascular systems [22,23]. Second, different administration methods were used in nine trials. Five studies [12-16] had a single-shot infiltration, and two studies [11,17] had a combination of intraoperative and postoperative infiltration, whereas another two studies [10,18] used continuous infiltration. Zhang et al. [24] found that continuous local infiltration provided prolonged superior analgesia and were associated with more favorable functional recovery and patient satisfaction compared with single local infiltration. Moreover, most trials were not sufficiently blinded due to the design, which may also arise a bias. Therefore, the standardization of the multimodal drugs and administration methods should be dealt with carefully.
In addition, the optimal site of administration of local infiltration should be of concern. Five studies [13-16,18] used periarticular infiltration and four studies [10-12,17] used intra-articular infiltration. There were several trials comparing intra-articular infiltration with periarticular infiltration. Andersen et al. [25] and Perret et al. [26] concluded no clear statistically significant benefit with either technique. On the contrary, Tsuyoshi Nakai et al. [27] showed the level of pain control was higher in periarticular infiltration than in intra-articular infiltration. Therefore, further studies are needed comparing the pain-relief efficacy between intra-articular infiltration and periarticular infiltration to confirm the optimal site of administration.
Furthermore, in this meta-analysis, we focused on the pain score, range of flexion, length of hospital stay, and complications shortly after THA and TKA. However, longer follow-up would be preferable to evaluate the results, especially in terms of long-term knee motion and complications. A study about the long-term outcome of local infiltration is needed to solidate the advantage of local infiltration.
Another limitation of the meta-analysis are the small sample sizes in each study. The overestimation of the treatment effect is more likely in smaller trials compared with larger samples. Furthermore, variable reporting of outcomes and inconsistent definitions mean that some data were provided insufficiently. Ultimately, some outcomes could not be included in the meta-analysis, which might lower the level of evidence.
CONCLUSION
Local infiltration appeared to be an efficient and safe alternative for postoperative pain management in TKA. There is a high level of heterogeneity between the studies, and more homogenous research is necessary to validate our conclusion.
ACKNOWLEDGMENTS
This work was supported by grants from the National Natural Scientific Foundation of China (81301615 to H.W.) and the Natural Scientific Foundation of Shanghai (14ZR1406900 to Z.X.).
DECLARATION OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
- [1].Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5. doi: 10.2106/JBJS.F.00222. http://dx.doi.org/10.2106/JBJS.F.00222 . [DOI] [PubMed] [Google Scholar]
- [2].Nussenzveig TC. Pain management after total joint replacement and its impact on patient outcomes. AORN J. 1999;70(6):1060–2. doi: 10.1016/s0001-2092(06)62213-8. http://dx.doi.org/10.1016/s0001-2092(06)62213-8 . [DOI] [PubMed] [Google Scholar]
- [3].Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91(1):8–15. doi: 10.1097/00000542-199907000-00006. http://dx.doi.org/10.1097/00000542-199907000-00006 . [DOI] [PubMed] [Google Scholar]
- [4].Choi PT, Bhandari M, Scott J, Douketis J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev. 2003;3:CD003071. doi: 10.1002/14651858.CD003071. http://dx.doi.org/10.1002/14651858.cd003071 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Tang R, Evans H, Chaput A, Kim C. Multimodal analgesia for hip arthroplasty. Orthop Clin North Am. 2009;40(3):377–87. doi: 10.1016/j.ocl.2009.04.001. http://dx.doi.org/10.1016/j.ocl.2009.04.001 . [DOI] [PubMed] [Google Scholar]
- [6].Bianconi M, Ferraro L, Traina GC, Zanoli G, Antonelli T, Guberti A, et al. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth. 2003;91(6):830–5. doi: 10.1093/bja/aeg277. http://dx.doi.org/10.1093/bja/aeg277 . [DOI] [PubMed] [Google Scholar]
- [7].Kerr DR, Kohan L. Local infiltration analgesia: A technique for the control of acute postoperative pain following knee and hip surgery: A case study of 325 patients. Acta Orthop. 2008;79(2):174–83. doi: 10.1080/17453670710014950. http://dx.doi.org/10.1080/17453670710014950 . [DOI] [PubMed] [Google Scholar]
- [8].Teng Y, Jiang J, Chen S, Zhao L, Cui Z, Khan MS, et al. Periarticular multimodal drug injection in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1949–57. doi: 10.1007/s00167-013-2566-0. http://dx.doi.org/10.1007/s00167-013-2566-0 . [DOI] [PubMed] [Google Scholar]
- [9].Jiang J, Teng Y, Fan Z, Khan MS, Cui Z, Xia Y. The efficacy of periarticular multimodal drug injection for postoperative pain management in total knee or hip arthroplasty. J Arthroplasty. 2013;28(10):1882–7. doi: 10.1016/j.arth.2013.06.031. http://dx.doi.org/10.1016/j.arth.2013.06.031 . [DOI] [PubMed] [Google Scholar]
- [10].Andersen KV, Bak M, Christensen BV, Harazuk J, Pedersen NA, Søballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop. 2010;81(5):606–10. doi: 10.3109/17453674.2010.519165. http://dx.doi.org/10.3109/17453674.2010.519165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Spreng UJ, Dahl V, Hjall A, Fagerland MW, Ræder J. High-volume local infiltration analgesia combined with intravenous or local ketorolac morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth. 2010;105(5):675–82. doi: 10.1093/bja/aeq232. http://dx.doi.org/10.1093/bja/aeq232 . [DOI] [PubMed] [Google Scholar]
- [12].Klasen JA, Opitz SA, Melzer C, Thiel A, Hempelmann G. Intraarticular, epidural, and intravenous analgesia after total knee arthroplasty. Acta Anaesthesiol Scand. 1999;43(10):1021–6. doi: 10.1034/j.1399-6576.1999.431009.x. http://dx.doi.org/10.1034/j.1399-6576.1999.431009.x . [DOI] [PubMed] [Google Scholar]
- [13].Tsukada S, Wakui M, Hoshino A. Pain control after simultaneous bilateral total knee arthroplasty: A randomized controlled trial comparing periarticular injection and epidural analgesia. J Bone Joint Surg Am. 2015;97(5):367–73. doi: 10.2106/JBJS.N.00373. http://dx.doi.org/10.2106/JBJS.N.00373 . [DOI] [PubMed] [Google Scholar]
- [14].Jules-Elysee KM, Goon AK, Westrich GH, Padgett DE, Mayman DJ, Ranawat AS, et al. Patient-controlled epidural analgesia or multimodal pain regimen with periarticular injection after total hip arthroplasty: A randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am. 2015;97(10):789–98. doi: 10.2106/JBJS.N.00698. http://dx.doi.org/10.2106/JBJS.N.00698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Pandazi A, Kanellopoulos I, Kalimeris K, Batistaki C, Nikolakopoulos N, Matsota P, et al. Periarticular infiltration for pain relief after total hip arthroplasty: A comparison with epidural and PCA analgesia. Arch Orthop Trauma Surg. 2013;133(11):1607–12. doi: 10.1007/s00402-013-1849-8. http://dx.doi.org/10.1007/s00402-013-1849-8 . [DOI] [PubMed] [Google Scholar]
- [16].Tsukada S, Wakui M, Hoshino A. Postoperative epidural analgesia compared with intraoperative periarticular injection for pain control following total knee arthroplasty under spinal anesthesia: A randomized controlled trial. J Bone Joint Surg Am. 2014;96(17):1433–8. doi: 10.2106/JBJS.M.01098. http://dx.doi.org/10.2106/JBJS.M.01098 . [DOI] [PubMed] [Google Scholar]
- [17].Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Søballe K. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: A randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop. 2007;78(2):180–6. doi: 10.1080/17453670710013654. http://dx.doi.org/10.1080/17453670710013654 . [DOI] [PubMed] [Google Scholar]
- [18].Binici Bedir E, Kurtulmus T, Basyigit S, Bakir U, Saglam N, Saka G. A comparison of epidural analgesia and local infiltration analgesia methods in pain control following total knee arthroplasty. Acta Orthop Traumatol Turc. 2014;48(1):73–9. doi: 10.3944/AOTT.2014.3256. http://dx.doi.org/10.3944/AOTT.2014.3256 . [DOI] [PubMed] [Google Scholar]
- [19].Mullaji A, Kanna R, Shetty GM, Chavda V, Singh DP. Efficacy of periarticular injection of bupivacaine, fentanyl, and methylprednisolone in total knee arthroplasty: A prospective, randomized trial. J Arthroplasty. 2010;25(6):851–7. doi: 10.1016/j.arth.2009.09.007. http://dx.doi.org/10.1016/j.arth.2009.09.007 . [DOI] [PubMed] [Google Scholar]
- [20].Starks I, Frost A, Wall P, Lim J. Is a fracture of the transverse process of L5 a predictor of pelvic fracture instability? J Bone Joint Surg Br. 2011;93(7):967–9. doi: 10.1302/0301-620X.93B7.26772. http://dx.doi.org/10.1302/0301-620X.93B7.26772 . [DOI] [PubMed] [Google Scholar]
- [21].Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: A quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203(6):914–32. doi: 10.1016/j.jamcollsurg.2006.08.007. http://dx.doi.org/10.1016/j.jamcollsurg.2006.08.007 . [DOI] [PubMed] [Google Scholar]
- [22].Vendittoli PA, Makinen P, Drolet P, Lavigne M, Fallaha M, Guertin MC, et al. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am. 2006;88(2):282–9. doi: 10.2106/JBJS.E.00173. http://dx.doi.org/10.2106/JBJS.E.00173 . [DOI] [PubMed] [Google Scholar]
- [23].Mather LE. The acute toxicity of local anesthetics. Expert Opin Drug Metab Toxicol. 2010;6(11):1313–32. doi: 10.1517/17425255.2010.514265. http://dx.doi.org/10.1517/17425255.2010.514265 . [DOI] [PubMed] [Google Scholar]
- [24].Zhang S, Wang F, Lu ZD, Li YP, Zhang L, Jin QH. Effect of single-injection versus continuous local infiltration analgesia after total knee arthroplasty: A randomized, double-blind, placebo-controlled study. J Int Med Res. 2011;39(4):1369–80. doi: 10.1177/147323001103900423. http://dx.doi.org/10.1177/147323001103900423 . [DOI] [PubMed] [Google Scholar]
- [25].Andersen LØ, Kristensen BB, Husted H, Otte KS, Kehlet H. Local anesthetics after total knee arthroplasty: Intraarticular or extraarticular administration? A randomized, double-blind, placebo-controlled study. Acta Orthop. 2008;79(6):800–5. doi: 10.1080/17453670810016885. http://dx.doi.org/10.1080/17453670810016885 . [DOI] [PubMed] [Google Scholar]
- [26].Perret M, Fletcher P, Firth L, Yates P. Comparison of patient outcomes in periarticular and intraarticular local anaesthetic infiltration techniques in total knee arthroplasty. J Orthop Surg Res. 2015;10:119. doi: 10.1186/s13018-015-0249-x. http://dx.doi.org/10.1186/s13018-015-0249-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Nakai T, Tamaki M, Nakamura T, Nakai T, Onishi A, Hashimoto K. Controlling pain after total knee arthroplasty using a multimodal protocol with local periarticular injections. J Orthop. 2013;10(2):92–4. doi: 10.1016/j.jor.2013.02.001. http://dx.doi.org/10.1016/j.jor.2013.02.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]


