Abstract
Context
Parent-based adolescent sexual health interventions aim to reduce sexual risk behaviors by bolstering parental protective behaviors. Few studies of theory use, methods, applications, delivery and outcomes of parent-based interventions have been conducted.
Methods
A systematic search of databases for the period 1998–2013 identified 28 published trials of U.S. parent-based interventions to examine theory use, setting, reach, delivery mode, dose and effects on parent-child communication. Established coding schemes were used to assess use of theory and describe methods employed to achieve behavioral change; intervention effects were explored in meta-analyses.
Results
Most interventions were conducted with minority parents in group sessions or via self-paced activities; interventions averaged seven hours, and most used theory extensively. Meta-analyses found improvements in sexual health communication: Analysis of 11 controlled trials indicated a medium effect on increasing communication (Cohen's d, 0.5), and analysis of nine trials found a large effect on increasing parental comfort with communication (0.7); effects were positive regardless of delivery mode or intervention dose. Intervention participants were 68% more likely than controls to report increased communication and 75% more likely to report increased comfort.
Conclusions
These findings point to gaps in the range of programs examined in published trials—for example, interventions for parents of sexual minority youth, programs for custodial grandparents and faith-based services. Yet they provide support for the effectiveness of parent-based interventions in improving communication. Innovative delivery approaches could extend programs' reach, and further research on sexual health outcomes would facilitate the meta-analysis of intervention effectiveness in improving adolescent sexual health behaviors.
Even with the ongoing decline in U.S. teenage pregnancies over several decades, some 2,000 teenagers become pregnant every day.1 In addition, an estimated 40% of sexually active adolescent females have an STD.1 Long-standing disparities in teenage pregnancy and STD rates still exist by race and ethnicity.2,3 Educational programs that target parents are an alternative or an enhancement to school-based adolescent sexual health education.4 Parent-based interventions aim to reduce adolescent sexual risk behaviors (e.g., early sexual debut, nonuse of condoms) by bolstering parental protective factors such as parent-child communication about sexual health5 and parental monitoring,6 as suggested by the analytic frameworks of Burrus et al.7 and Hutchinson and Wood.8 For example, one study found that an increased level of sexual risk communication between mothers and daughters (12–19 years old) was associated with reduced levels of sexual intercourse and unprotected sex.9 Although findings from some U.S. intervention trials suggest that improvements in parent-child communication can influence adolescent sexual behaviors,10–14 the empirical evidence to support a causal claim is lacking.
Past reviews of parent-based adolescent sexual health trials have used widely different inclusion criteria and search strategies,15–19 which led to large variations in both the U.S. and the non-U.S. studies examined; as a result, only three trials were included in all reviews. Moreover, these reviews based their conclusions on descriptive findings and the percentages of studies with statistically significant outcomes, and did not include a meta-analysis. New studies have been published since these reviews were completed.
It is not surprising, then, that prior reviews reached different conclusions, some declaring that findings are positive15–17 and others that findings are mixed.18,19 In summarizing 15 trials, Atienzo et al.15 described them as showing significant increases in parent-child communication; parental monitoring and supervision; adolescents' perceptions of rules and of family support; and intentions to postpone intercourse and use contraceptives and condoms. These authors found a reduction in adolescents' self-reported sexual relations associated with parent-based interventions. Wight and Fullerton16 found that interventions were associated with improvements in parent-child interaction and adolescents' sexual knowledge and attitudes; about half of the 44 studies they reviewed reported improvements in adolescent sexual behavior outcomes. Bastien et al.,17 reviewing 23 Africa-based trials, reported positive findings, largely increases in frequency of and parental comfort with sexual health discussions. Akers et al.19 found that among 12 trials, intervention parents showed improved communication, as measured by frequency, quality, intentions, comfort and self-efficacy for communicating; however, no improvements in parental attitudes toward communicating were seen. The Downing et al.18 review of 17 studies found no improvements in parental attitudes toward communication, and reported inconsistent association with adolescent sexual risk behaviors; no association was found between increased parent-child communication and a decline in sexual risk behaviors.
In addition to the need for stronger analytic methods in systematic reviews, it is important to describe the theoretical foundation on which interventions are based. The importance of theory in intervention development and implementation is well established across behavior change interventions in general,20,21 in adolescent sexual health interventions7,8,22 and in parent-based interventions.7,8 Theory is used to explain personal and environmental determinants of behavior related to a specified health problem, create a causal model for bringing about positive outcomes, select intervention methods and practical delivery applications to achieve behavior change, evaluate interventions and describe interventions' critical components.23,24 For example, the theory of planned behavior has been used to understand adolescent and parent behaviors,25 and social cognitive theory has been used to inform intervention components, methods and applications.26
Previous reviews have not adequately described the use of theory in intervention development (e.g., how theory informs determinants, methods and applications) or interventions' doses or delivery mechanisms, in part because published trials do not consistently report methods used to change behavior.27 An examination of the theoretical underpinnings of behavioral determinants, behavior change methods, the application of methods, intervention setting and delivery mode would allow for a more comprehensive description of the critical components of parent-based adolescent sexual health interventions.28 Moreover, a better understanding of these components would provide insight into how personal and environmental factors that influence behavior can be changed29 and how methods (e.g., modeling) and their applications (e.g., a video demonstrating effective parent-child communication) can be successfully implemented.
This review addresses the following research questions: First, what is the range of settings, target populations, delivery modes and doses in parent-based adolescent sexual health interventions? Second, what theories and models have been used to inform the development of such interventions, and to what extent have they been used? Third, what is the range of determinants and behavioral outcomes addressed by these interventions? Fourth, what is the range of theory-based methods and applications that have been used? Finally, what is the impact of such interventions on parent-child communication and adolescent sexual behavior?
Methods
Systematic Review
Trials eligible for inclusion in this review reported findings from parent-based adolescent sexual health interventions, were written in English and were published in peer-reviewed journals between January 1998 and July 2013. We used Kirby and Miller's 2002 descriptive systematic review of this type of intervention as a guide.30 We included all adolescent sexual health intervention trials that targeted parents, and did not limit eligibility to those that focused only on parent-child communication. Since the cultural climate for this topic is vastly different in the United States than in Europe, Africa, Australia and Latin America, we limited the review to U.S. trials.
The search strategy was developed with the assistance of a public health librarian with expertise in conducting and documenting searches for systematic reviews. Databases searched (and interfaces) were Medline (Ovid), PubMed (NLM), PsycINFO (Ovid), CINAHL (EBSCOhost) and ERIC (EBSCOhost). Concepts included in the search were “parent,” “adolescent,” “sexual behavior” and “evaluation.” The search strategy for each database, which differed to account for specialized index terms, was reviewed by the authors and the librarian, and was archived for future inquiries and updates. An exhaustive list is available upon request. We also searched the reference lists of included trials for additional intervention studies and articles related to the development and theoretical underpinnings of the interventions.
Retrieved citations were screened, duplicates were eliminated and the remaining citations were organized in a database (Ref-WORKS). The first author reviewed titles and abstracts and applied the eligibility criteria; full-text articles were reviewed to determine final eligibility. A random sample of 50 titles and abstracts was independently screened by a second reviewer to assess the reliability of the selection procedure.
Data abstracted from each study were study design, sample size, recruitment methods, setting, intervention aims by intended audience, components, delivery mode, dose (number of sessions and duration), behavior change methods and practical applications, theory and measured outcomes. We evaluated the extent of theory use by employing an adaptation of the Michie et al. coding scheme.27 Trials were assigned a level from 0 (theory not mentioned at all) to 4 (theory use described in detail relative to intervention, determinants of behavior and theory-relevant constructs). Theoretical methods and applications were abstracted and coded using the Bartholomew et al. taxonomy.29 This study was approved by the institutional review board of the University of Texas Health Science Center at Houston.
Meta-Analyses
Meta-analyses were performed on subsets of trials from the systematic review that had a contemporaneous control group and conceptual similarity in the outcomes of interest: parent-child sexual health communication and parental comfort with sexual health communication. (Adolescent-level measures—e.g., sexual intercourse, condom use—were too diverse to be included in a meta-analysis.) For these trials, we abstracted the study design, sample size and measurement properties of outcomes (i.e., indicators and types of scales used). To assess estimated effect sizes for the individual trials, we used Cohen's d to calculate standardized mean differences (e.g., the standardized difference in posttest mean scores of parent-child sexual health communication between the intervention and control groups divided by the pooled standard deviation).31 When trials had multiple follow-up points, we used the most proximal follow-up measures beyond immediate postintervention. For trials with more than one intervention group and a single control or comparison group, we selected the parent-only intervention that was theoretically most effective, usually indicated by the authors.
Results
Trial Characteristics
A total of 28 parent-based adolescent sexual health intervention trials, reported in 62 articles, met the eligibility criteria (Table 1).10–14,32–54 Interventions most frequently targeted parents of adolescents younger than 16 years old, 18 enrolled mostly minority parents, 20 took place in the community and eight provided self-paced activities at home.
Table 1. Summary of 28 parent-based adolescent sexual health intervention trials.
| Study | Design, sample, recruitment and setting | Aims for parents andyouth | Components and dose | Theoretical methods (applications)* | Theory (level of use)† | Outcome measures and follow-up |
|---|---|---|---|---|---|---|
| Included in meta-analyses | ||||||
| Andersonet al.46 |
Design: Longitudinal, nonrandomized controlled trial N=251 parents and 9–14-year-olds Recruitment: Community meetings for school, agencies Setting: Community centers, schools |
Youth: Increase communication, decision-making skills; delay sexual debut Both: Increase family communication; increase knowledge of puberty, reproduction |
Group sessions (six youth-only, one parents-only, one together) | Guided practice (decision making, shared activities), modeling (parent-child communication video), discussion (communication barriers, confidence), persuasive communication (personalize risk, reproductive knowledge) | Cognitive behavioral model (level 4) |
Outcome: Parent-child communication Follow-up: Immediate |
| Blake et al.45 |
Design: Pretest-posttest N=351 parents and adolescents Recruitment: High schools Setting: School, home |
Parents: Increase understanding of changes, pressures on teenagers; increase communication about sex; improve communication equity; increase ability to help child resist peer pressure, skills to identify and reduce risk Youth: Delay sexual debut |
Parent homework assignments (five), face-to-face, print materials | Active learning, modeling (demonstration), guided practice (rehearsal), discussion (interpersonal challenges, wishes, responses comparison) | Social learning theory, social cognitive theory (level 4) |
Outcomes: Ability to avoid high-risk behaviors, intention to have sex before finishing high school, parent-child sex communication Follow-up: Seven weeks |
| DiIorio et al.11 |
Design: Cluster randomized controlled trial N=582 black mothers and 11–14-year-olds Recruitment: Probability sample from Boys and Girls Clubs Setting: Community |
Mothers: Increase cognitive, behavioral, efficacy skills; increase environmental support Youth: Increase partner communication; delay sexual debut |
Group sessions (seven two-hour sessions every other week for three months; four together and three separate; four community activities for youth) | Guided practice (parenting skills, persuasive communication, risk assessment), modeling, goal setting (communication), tailoring (assessing situations, reinforcing positive behaviors), mobilize social networks (family and community), discussion (motivation, family and school involvement, shared experience, self-regulation, resource recognition), improve physical and emotional states (relaxation activity), self-reevaluation (reflection), shift perspective (parental support of risk reduction behaviors) | Social cognitive theory, problem behavior theory, educational theory (level 4) |
Outcomes: Condom use at last intercourse, mother-reported mother-child communication Follow-up: 24 months |
| DiIorio et al.39 |
Design: Cluster randomized controlled trial N=277 black fathers and 11–14-year-old sons Recruitment: Probability sample from Boys and Girls Clubs Setting: Community |
Fathers: Increase father-son sexuality communication Youth: Delay sexual debut; increase condom use |
Group sessions, print materials, home activities (six two-hour weekly sessions for fathers and one together) | Modeling (demonstration, videotapes), guided practice (role-playing, games, condom skills), discussion and lecture, goal setting | Social cognitive theory (level 4) |
Outcomes: Father-reported sex-related discussion; lifetime sex without a condom; child-reported difference in discussion, behaviors, abstinence Follow-up: Three months |
| Dilorio et al.34 |
Design: Cluster randomized controlled trial N=306 black mothers and 6–12-year-olds Recruitment: Probability sample from Boys and Girls Clubs Setting: Community |
Mothers: Increase confidence, role in promoting resilience in youth Youth: Delay sexual debut |
10 weekly 90-minute group sessions | Tailoring (motivational interviewing), persuasive communication (shifting perspectives, promoting positive attitude), mobilize social networks (sharing, problem solving about educationally marginalized communities), guided practice (skills practice with youth), improve physical and emotional states (relaxation exercise, ice breaker), homework | Ecological model, social cognitive theory (level 4) |
Outcomes: Discussion of general and difficult sex topics, intent to discuss sexual topics with children at earlier age, awareness of children's need for sex education Follow-up: Six months |
| Forehandet al.44 |
Design: Three-arm randomized controlled trial N=1,115 black parents and 9–12-year-olds Recruitment: Housing authority, recreation programs, schools, churches, flyers, referrals, community events Setting: Community |
Parents: Increase awareness of sexual risk behavior, relationship building, monitoring, supervision, communication, reinforcement; help child deal with peer pressure; increase communication self-efficacy, skills to convey values | Group sessions (enhanced group: five 2.5-hour sessions and two boosters at 12 and 24 months) |
Parents: Tailoring (response contingencies), modeling (communication, attitudes, expectations), guided practice (communication), persuasion (promote communication about risk reduction, attitude, parental confidence), reinforcement, discussion (reduce opportunities to engage in risky behavior) Youth: Persuasion (refusal self-efficacy), active learning (refusal skills) |
Social learning theory, problem behavior theory, theory of reasoned action, social cognitive theory (level 4) |
Outcomes: Increase in parent-reported communication and in parent- and child- reported sexual communication Follow-up: Six months |
| Lefkowitzet al.53 |
Design: Pretest-posttest randomized controlled trial with delayed control group N=50 mothers and 11–15-year-olds Recruitment: Schools Setting: Community |
Mothers: Increase open, engaging communication style (act less judgmental, ask open-ended questions, decrease lecturing) | Two 1.5-hour, small-group sessions, handouts | None mentioned | None mentioned |
Outcomes: Sexual health communication comfort, number of topics discussed Follow-up: Immediate |
| McKay et al.43 |
Design: Quasi- experimental N=324 low-income black parents and youth Recruitment: School roster Setting: Schools, churches, park district buildings |
Parents: Strengthen networks; reinforce abstinence; avoid risky situations (parental monitoring, support, communicating values); discuss puberty and HIV/AIDS Youth: Develop social problem-solving and negotiation skills; recognize risk situations; avoid risky situations; improve decision-making, refusal skills |
Group sessions (parent-child and multifamily); multilevel group modalities (12 two-hour weekly sessions) | Cue altering (self-regulation), skill mastery (social skills, communication), self-reevaluation (self-understanding), establish parental monitoring, mobilize social networks (community development, referrals), discussion (parenting strategies and styles, supervision, monitoring) | Model of influences on HIV risk exposure, development theory, triadic theory of influence, social action theory (level 4) |
Outcomes: Increase family communication and communication comfort, improve decision making Follow-up: Immediate |
| Prado and Pantin10 |
Design: Randomized controlled trial N=242 Hispanic parents and youth Recruitment: Referrals from Miami–Dade County Dept. of Juvenile Services, school system Setting: Community, home |
Parents: Increase parental investment, support for youth Youth: Decrease substance use and HIV risk; increase self-efficacy (control), perceived responsibility, social competence, self-regulation, self-control, academic achievement, school bonding |
Parent and child group sessions, family meeting/home visits, supervised peer activities, school counseling, family therapy (eight two-hour sessions and four one-hour family visits over three months) | Mobilize social networks (participatory learning, family support, parental involvement, parent groups), discussion (positive parenting), guided practice (role-playing, communication skills) | Ecodevelopmental theory (level 4) |
Outcomes: STDs, unprotected last intercourse, parent-adolescent communication Follow-up: Six months |
| Schusteret al.37 |
Design: Randomized controlled trial N=569 parents and youth in grades 6–10 Recruitment: Worksite e-mail, newsletters Setting: Worksite |
Parents: Increase communication, monitoring, involvement; increase intention to talk, monitor, influence community norms; improve parent-child relationship | Eight one-hour weekly group education sessions, videos, handouts (six) | Modeling (videotaped role-playing), guided practice (communication skills, healthy relationship formation, effective monitoring), skills practice | Theoretical model based on eight variables (level 4) |
Outcomes: Number of sexual topics discussed, ability to communicate Follow-up: One week |
| Stanton et al.12 |
Design: Randomized controlled three-group, longitudinal trial N=817 black parents and 13–16-year-olds Recruitment: Housing development tenant association members, recreation center staff Setting: Community, home visit |
Parents: Increase parental monitoring, communication about sex, risky behaviors, HIV; promote abstinence, condom, contraceptive use; counsel about alcohol, drugs, pressure | Individual session (60–90 minutes), video (22 minutes) | Active learning (mastery), modeling (video, vicarious role-playing, monitoring), guided practice (skills), persuasion (abstinence, condom, contraceptive use), feedback (reinforcement), discussion (knowledge of alcohol, drugs, pressure) | Social cognitive theory (level 4) |
Outcome: Open communication Follow-up: 24 months |
| Villarruelet al.32 |
Design: Randomized controlled trial N=130 Hispanic parents and youth Recruitment: Flyers, newspaper ad, personal contact, school presentations, community-based programs, health promotion courses Setting: Community |
Parents: Increase general and sexual communication; increase self-efficacy, comfort communicating; increase knowledge (STDs, HIV, pregnancy), support for parental communication | Self-paced materials, computer-based modules (one 40- and one 20-minute session) | Modeling (skills), skill mastery (homework, skills practice), active learning (acquire information), guided practice (skill building, parenting practices, parent-child communication) | Ecodevelopmental theory, theory of planned behavior, theory of reasoned action (level 4) |
Outcomes: Sexual risk communication and communication comfort Follow-up: Three months |
| Woody et al.51 |
Design: Pretest-posttest N=37 mothers Recruitment: News-paper ad, school newsletter, community organizations; $10 enrollment fee Setting: University campus |
Mothers: Provide information; explore thoughts and feelings about providing sex education to child | Group sessions (four 1.5-hour weekly sessions or one six-hour session) | None mentioned | None mentioned |
Outcomes: Restrictive sexual beliefs, communication comfort on sexual topics, attitude toward children's sexual learning Follow-up: 10 weeks |
| Not included in meta-analyses | ||||||
| Barr et al.33 |
Design: Pretest-posttest pilot study N=76 minority parents (the majority black mothers) Recruitment: Letters home from school Setting: Community |
Parents: Increase comfort with and positive outcome expectations for discussing sexuality | One half-hour group session, resource materials | Discussion (communication barriers and tips), persuasive communication (sexual health talk, resources), guided practice (skills, role-playing), discussion (brainstorming), mobilize social networks (partnering with schools and community organizations, advocating sex education) | Health belief model (level 4) |
Outcomes: Communication comfort on sexual health topics, outcome expectations Follow-up: Immediate |
| Bartlett and Shelton50 |
Design: Pretest-posttest N=18 black parents and daughters Recruitment: Middle schools Setting: School |
Parents: Increase maternal support, monitoring Youth: Increase knowledge of HIV, transmission risk, self-protection, assertiveness, condom self-efficacy, racial/ethnic pride Both: Build racial/ethnic pride |
Three one-hour group sessions for parents; 12 hours of group education for youth, service learning–based | None mentioned | None mentioned |
Outcomes: Mean increase in communication scores, protective factors, monitoring Follow-up: Three months |
| Burgess et al.41 |
Design: Pretest-posttest N=6 parents and 14–18-year-olds Recruitment: Court-ordered attendance Setting: Community |
Parents: Reinforce values; discourage early sexual debut, unprotected sex; reduce communication barriers | Four two-hour group sessions over two weeks | Persuasive communication (information), modeling (assertiveness), guided practice (role-play communication, decision making, negotiation), discussion and lecture | Social learningtheory (level 4) |
Outcome: Parent-child communication comfort about sexual health Follow-up: Immediate |
| Causey et al.47 |
Design: Prospective longitudinal quasi-experimental N=1,580 Latino youth and 970 parents Recruitment: Middle schools in high-need communities Setting: Community |
Parents: Increase knowledge, communication, awareness of pregnancy risk and STDs; promote strategies for raising emotionally intelligent children, conflict resolution, handling social pressure Youth: Promote abstinence until marriage, healthy relationships; increase awareness of consequences of sex |
Peer educators, theater, parent workshops; five two-hour sessions for parents; 12 weekly 1.25-hour sessions for youth | Dramatic relief (theater production to reinforce course message), repetition (knowledge retention), participation (family connectedness) | Theory of reasoned action, theory of planned behavior (level 2) |
Outcomes: Implementation outcomes only Follow-up: Six, 12 and 24 months |
| Dancy et al.40 |
Design: Repeated measures nonrandomized controlled trial N=553 low-income black mothers and daughters Recruitment: Convenience sample Setting: Community |
Mothers: Train mothers to be daughters' primary HIV educator | Six weekly two-hour mother-facilitated group sessions; parent facilitators had 12 weeks' intensive training | Modeling (communication), guided practice (mentor and train parents, promote condom use), feedback (role-playing), goal setting (behavioral agreement) | Social cognitive theory, theory of reasoned action/planned behavior, community-as-mother theory (level 4) |
Outcomes: Intention to refuse sex, sexual behavior Follow-up: Six months |
| DuRant et al.48 |
Design: Post-intervention survey telephone interview N=1,132 parents of adolescents Recruitment: Telephone Setting: Community |
Parents: Increase communication with adolescents about sex | Media campaign, public service announcements (TV, radio, billboard) | None mentioned | No specific theory mentioned (level 1) |
Outcome: Intention to talk to children about sex Follow-up: Not reported |
| Evans et al.35 |
Design: Randomized controlled trial N=394 parents and youth Recruitment: Online panel, random-digit-dialing telephone methodology Setting: Community |
Parents: Delay sexual debut by increasing parent-child communication, expectations to delay sex | Media campaign, social marketing using public service announcements (TV, radio, print, Web, outdoor advertising) | Modeling (communication, monitoring, supervision), mobilize social networks (peer support, group families) | Social cognitive theory (level 4) |
Outcome: Parental communication about sex Follow-up: Not reported |
| Green and Documét54 |
Design: Pretest-posttest N=721 parents Recruitment: Flyers, word of mouth Setting: Community |
Parents: Increase parents' comfort in communication about sex and sexual decision making; encourage adolescents to start communicating before puberty | Community-trained and community-facilitated, guidebook, one session | None mentioned | None mentioned |
Outcomes: Comfort with sexual health communication, likelihood of discussing sexuality issues, recognition of need to talk with children at a young age Follow-up: One month |
| Guilamo-Ramos et al.13 |
Design: Randomized controlled trial N=264 black or Hispanic parents of 11–14-year-olds Recruitment: Convenience sample Setting: Clinic |
Parents: Improve communication and parenting strategies | 30-minute parent education and two booster phone calls by social worker, physician endorsement, reference materials | Persuasion (support for abstinence), modeling (initiating conversation, teachable moments, relationship building, communication), discussion (monitoring) | Social learning theory, theory of reasoned action, self-regulation theory, theory of subjective culture, health belief model (level 4) |
Outcomes: Rates of transition to sexual activity, frequency of sex, oral sex Follow-up: Nine months |
| Klein et al.52 |
Design: Pretest-posttest N=174 minority parents of 10–12-year-olds Recruitment: Community- and school-based workshops Setting: Community (schools, churches, local agencies) |
Parents: Increase parental competence and confidence in communicating with children about sex and sexuality | Community workshops (four main and two optional sessions) | None mentioned | None mentioned |
Outcome: Parental comfort in communicating about sexual health Follow-up: 10 weeks |
| Ledermanet al.38 |
Design: Randomized comparison N=192 mostly minority parents and adolescents Recruitment: Invitations to school districts, presentations at professional conferences, letters, flyers, phone calls to parents Setting: Middle school |
Parents: Strengthen family communication; reduce risk by improving social control and adolescents' self-control | Group education (four 2.5-hour weekly sessions, partly together and partly separate), three booster sessions | Discussion, modeling (communication), guided practice (role-playing), tailoring (personalize information) | Social learning theory, behavioral cognitive theories (level 4) |
Outcomes: Increase in parental rules about sex and other risky behaviors, and in knowledge of prevention and resistance responses in adolescents Follow-up: One, six, 12 and 18 months |
| Murry et al.14 |
Design: Cluster randomized controlled trial N=332 rural black parents and 11-year-olds Recruitment: Telephone, letter Setting: Community |
Parents: Improve communication, discipline, monitoring, involvement, adaptive racial socialization; establish expectations for alcohol use and sex Youth: Promote importance of household rules, adaptive behaviors for dealing with racism, forming future goals Both: Increase family cohesion, communication, positive youth-family involvement |
Group sessions (separate and together; seven one-hour weekly sessions) | Guided practice (role-playing, guided activities, adaptive racial socialization, communication), discussions (vigilant parenting), modeling (monitoring, control, establishing expectations), personalize risk (video about high-risk situations) | Cognitive model of adolescent health risk behavior (level 4) |
Outcomes: Parental monitoring, sexual activity, condom use Follow-up: Immediate, 27 and 65 months |
| O'Donnellet al.36 |
Design: Randomized controlled trial N=268 black and Hispanic parents and adolescent females Recruitment: Brochures sent home from school Setting: Home |
Parents: Increase awareness of youths' risks and positive parenting practices; delay sexual debut and drinking; increase self-efficacy and communication of values | Self-paced materials, four audio CDs mailed to home over six months | Modeling (desired attitudes, behaviors, teachable moments, real-life situations), tailoring (storytelling), guided practice (proactive communication about alcohol and sex, monitoring, setting rules, values, expectations that support safety) | Theory of planned behavior, diffusion of innovation, social development theory, gender theory (level 4) |
Outcome: Parent-child communication Follow-up: Three months |
| O'Donnellet al.42 |
Design: Randomized controlled trial N=846 low-income minority parents and youth in grades 5–6 Recruitment: Schools Setting: Home |
Parents: Identify teachable moments, communicate values and expectations, set rules; recognize and respond to adolescent development and warning signs; increase parental accessibility | Self-paced materials, three audio CDs mailed to home over six months | Belief persuasion (abstinence promotion), modeling (desired attitudes and behaviors, conversation initiation) | Theory of planned behavior, diffusion of innovation, social development theory (level 4) |
Outcomes: Family support, family rules, behavioral risk, parent-reported communication Follow-up: Three months |
| Silitsky and Jones49 |
Design: Pretest-posttest N=121 mothers Recruitment: Letters, questionnaires Setting: Community |
Mothers: Help parents talk to their children about sex, HIV | 1.5-hour workshop | None mentioned | Communication theory (level 2) |
Outcome: Maternal-child HIV and sexual health communication Follow-up: Immediate |
Theoretical methods and applications were standardized using intervention mapping and behavior change techniques.
Interventions used a variety of delivery modes and were most frequently offered over multiple face-to-face sessions. Eighteen trials employed multiple group sessions—either sessions for parents only, separate parent and child sessions, sessions for parents and children together, or a combination. Eight interventions used mixed delivery modes (brief individual sessions, self-paced materials and media exposure). The dose ranged from 30 minutes to 24 contact hours, and averaged about seven hours.
Of the 23 theory-based trials, 20 reported extensive use of theory (categorized as level 4), including 12 that employed social cognitive theory, the most frequently used.26 Twenty theoretical models and frameworks were reported as underlying intervention development and dissemination. Theories informed multiple aspects of the interventions by providing a framework for targeting parents as a potential influence on adolescent behavior (e.g., ecodevelopmental theory);55 constructs that influence parental behaviors (e.g., social cognitive theory); and delivery mode, setting, methods, applications and dissemination (e.g., diffusion of innovation). Planned behavior56 and reasoned action57 theories were used in seven trials.13,32,36,40,42,44,47 Thirteen trials reported using constructs from more than one theory, model or framework,11,13,32,34,36–38,40,42–45,47 and one trial reported using five theories.13
Interventions employed a variety of methods to meet objectives: Nineteen used modeling and discussion, 16 used guided practice, seven used verbal persuasion and five used message tailoring. These methods were delivered via face-to-face interactions, videos, CDs and homework. Most theory-driven methods were based in social cognitive theory (e.g., modeling, guided practice, enactment, verbal persuasion, and physiological and affective change).29 Detailed explanations of how the theoretical models were operationalized in intervention activities and of the process used to select theory, methods and applications were rarely given in the publications.
Determinants and Behavioral Outcomes
Interventions targeted several parent-level behavioral determinants to increase parent-child sexual health communication. Fifteen interventions targeted parental self-efficacy for communication, 11 targeted communication skills and attitudes toward communication, and 10 focused on positive outcome expectations. Interventions focused on other parental practices as well: increasing monitoring (14), facilitating setting and enforcing family rules (11), increasing parental involvement and support (10), and mobilizing social networks (five). Some interventions aimed at preparing parents to teach effective refusal and negotiation skills (six); help youth improve decision making, self-regulation and self-control, and increase their awareness of parental values and behavioral expectations (five); and help them improve their self-efficacy, social problem solving and coping with peer pressure (four). Authors often did not report the methods or applications used to improve parents' ability to address these key adolescent behavioral determinants.
All 28 interventions aimed to improve effective parent-child communication; however, they addressed different domains of communication, targeted different behavioral determinants and used a variety of methods and applications. Each intervention reported a positive effect on at least one parent or adolescent outcome. Fifteen interventions reported a positive impact on parent-child communication frequency, and 11 on parental comfort with communication about sex, the most frequently reported parent-level outcome. Of the interventions that measured adolescent outcomes, five reported positive outcomes for reducing sexual risk (e.g., decreased sexual activity), and five for increasing condom use.
Results of Meta-Analyses
Eleven trials were selected for meta-analysis of parent-child sexual health communication, and nine for meta-analysis of parental comfort with sexual health communication (Table 1). Seven trials were included in both meta-analyses. All included interventions were conducted either face-to-face or through self-paced activities.
To arrive at a single, independent outcome measure for each trial, a hierarchical approach was implemented that favored adolescent-reported measures, which were considered more relevant to sexual health behavior than parent-reported measures. For example, Evans et al.35 found that only 33% of sons aged 10–14 agreed with their mothers' reports of mother-son sexual communication. When adolescent-reported measures were not available, parent-reported measures were used, a strategy that has been employed in previous meta-analyses.58
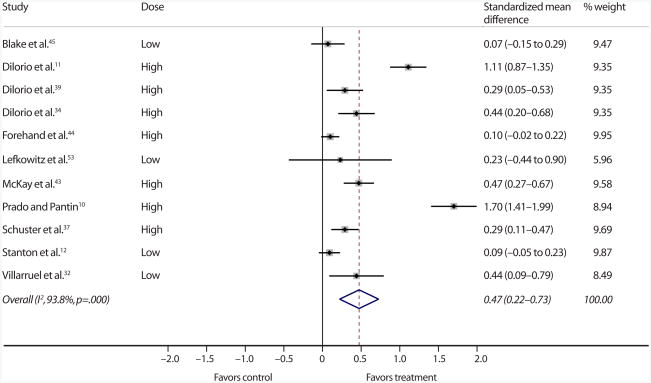
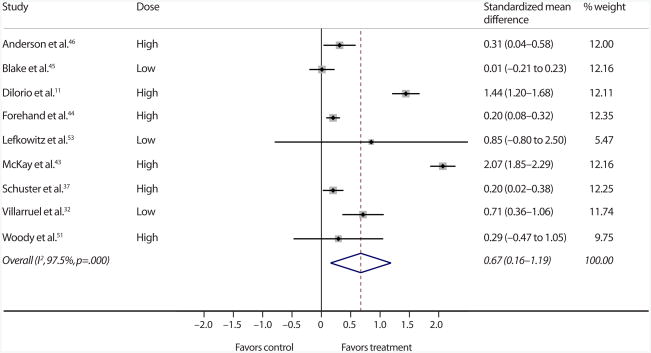
Cohen's d59 indicated that the intervention groups were significantly more likely than the control or comparison groups to report positive effects. However, there was a range (0.1–1.7) in effect sizes for parent-child sexual health communication (Figure 1). The Cohen's d for overall intervention impact on this outcome was 0.5, signifying a medium effect size.60 The range of effect sizes for parental comfort with sexual health communication was even wider (0.01–2.1), and the overall effect was large (0.7—Figure 2).60 These overall impacts mean that an intervention group parent was 68% more likely than a control group parent to have an increased communication score, and was 75% more likely to report increased comfort with communication.61 The data suggest a positive direction of effect across all intervention delivery modes—short, self-paced, short group and long group—and show that self-paced, lower dose interventions were not consistently less effective than higher dose interventions.
Figure 1. Standardized mean differences representing estimated effects on parent-child sexual health communication of 11 parent-based trials selected for a meta-analysis.
Notes: The size of the shaded box for each study represents the relative weight assigned to the study in calculating the overall standardized mean difference; the weight is based on the precision of the study's estimated effect (i.e., the narrowness of the confidence interval), as assessed in a random effects analysis. For complete references (indicated by superscripts), see end of text. High-dose interventions were three or more hours in length; low-dose ones were less than three hours. Figures in parentheses are 95% confidence intervals.
Figure 2. Standardized mean differences representing estimated effects on parental comfort with sexual health communication of nine parent-based trials selected for a meta-analysis.
Notes: The size of the shaded box for each study represents the relative weight assigned to the study in calculating the overall standardized mean difference; the weight is based on the precision of the study's estimated effect (i.e., the narrowness of the confidence interval), as assessed in a random effects analysis. For complete references (indicated by superscripts), see end of text. High-dose interventions were three or more hours in length; low-dose ones were less than three hours. Figures in parentheses are 95% confidence intervals.
Because of the inconsistencies in outcome measures, dose, delivery modes and setting, tests for heterogeneity between studies indicated, as expected, a high level of inconsistency when we evaluated the same effect across trials (I2, 94% for parent-child sexual health communication and 98% for parental comfort with communication). To address the high level of heterogeneity, we used a random effects model to weight the results of the individual studies before calculating the summary measure.
Discussion
Setting and Target Population
The parent-based adolescent sexual health programs examined in this review most frequently occurred in a community setting with parents of minority youth. Our findings point to several gaps in the range of published parent-based trials. We found no trials that targeted mothers and sons, although 24% of youth live in single-mother households.62 Nor did we identify trials targeting fathers and daughters, despite evidence that paternal communication about sex influences adolescent sexual behaviors separately from maternal communication,63 and has been suggested to be qualitatively different.64 Moreover, fathers are also in need of education and skill building in sexual health communication.65 In addition, no trials were found that were developed for faith-based organizations or services, despite evidence that faith-based programs can improve health outcomes and program reach.66 Finally, no interventions were identified that targeted parents of lesbian, gay, bisexual or transgender youth or of youth living with custodial grandparents, both of which are high-risk adolescent groups.67–69
Dose and Delivery Mode
Most of the included interventions were resource- and dose-heavy. This poses several concerns related to the challenges of disseminating resource-intensive programs and expanding their reach. First, intensive face-to-face group sessions require substantial funding, extensive procedural manuals, training of facilitators to assure program fidelity, community-level planning and laborious coordination. Second, interventions that require attendance at multiple sessions often face recruitment and retention challenges. For instance, at-risk populations may have a high level of life chaos and feel that the intervention is irrelevant or unhelpful in addressing their prioritized needs.70
Indeed, the meta-analyses indicate that the effects of the interventions using self-paced, lower dose, easily disseminated modes of delivery (e.g., computer-based) were not consistently smaller than those of high-dose interventions. This provides some support, albeit tenuous, for the development and testing of a range of low-dose intervention delivery modes that could increase reach to the parents of the highest risk groups by reducing barriers associated with face-to-face modalities. Our systematic review found that most parent-based interventions relied on group-based, multisession delivery modes. One promising way to increase reach is through the use of technology. Computer-based programs can reduce common barriers, such as work and family obligations, time and transportation. Use of the Internet bypasses access barriers, is familiar and comfortable to young parents, allows for individualized and tailored messages, engages active learning and is accessible even to low-income households.71,72 While there are challenges to disseminating high-dose interventions, further research is needed to determine if low-dose ones and methods other than face-to-face approaches can lead to similar positive outcomes and whether those outcomes can be sustained over time.
Use of Theory
Although most interventions used theory extensively to develop their scopes and aims, others did not indicate any use of theory in development, implementation or dissemination. Still other interventions employed theory to target a certain audience by race or ethnicity (e.g., community-as-mother theory) or by gender (e.g., gender theory). Theory was used to determine which constructs to target and to understand behavioral pathways.20 We found that well-constructed interventions that reported high theory use most frequently employed constructs from more than one theory or framework. Several trials cited theory to support targeting their intervention to parents as a means to change adolescent sexual health behaviors and outcomes, yet they did not explicitly specify theoretical methods and applications. Some trials described using the theory of planned behavior. However, a previous systematic review of the use of this theory found that it was employed most frequently to understand behavior, but not to design intervention components, methods or applications.25
While there are systematic ways to use theory to develop interventions, few parent-based youth sexual health intervention trials explicitly described this process in their publications, and few trials appear to use theory to determine appropriate methods, practical applications or delivery modes of the interventions.29 Another study shows that social cognitive theory and self-regulation theory are commonly used to inform behavior change methods (e.g., modeling, persuasion, self-monitoring).73 However, using social cognitive theory may not increase intervention effectiveness,74 and frequently trials did not report the application of the theoretical methods used.
Most interventions aimed to increase effective parent-child sexual health communication. Yet other parental constructs, such as parental attitudes, parent-child relationship quality and monitoring, have been correlated with adolescent sexual behaviors. For instance, in other research, youth who perceived parental permissiveness were more likely to engage in sexual behaviors, whereas perception of parental disapproval reduced the level of sexual risk behaviors.75–77 Additionally, parental nurturing and supportiveness have been associated with delay of sexual debut and condom and contraceptive use,78,79 and effective parental monitoring has been found to reduce situational opportunity.80,81 These examples highlight the importance of addressing multiple protective parenting practices when developing parent-based adolescent sexual health interventions. While the current study provides evidence that an intervention can improve parent-child sexual health communication, our findings do not allow us to conclude that improving communication directly affects adolescent sexual behaviors or outcomes.
The trials frequently did not justify their use of theory, their choice of theory82 or the process employed to determine the most appropriate theory, methods and applications. Despite the proliferation of parent-based adolescent sexual health interventions and related systematic reviews, this review highlights important gaps in our understanding of the range of intervention characteristics and effects on parent and adolescent behavior. By using the Michie et al. theory coding scheme,27 we were able to quantify the extent of theory use. In using the Bartholomew et al. taxonomy,29 we were able to assess the methods and applications used to implement the interventions. Many interventions characterized by high theory use described using methods we would expect to see. For instance, interventions used modeling and guided practice operationalized through applications such as video demonstrations and role-playing to improve skills, and persuasion and discussion operationalized through applications such as persuasive messages and small group discussion to change beliefs about and attitudes toward communication.
To improve parent-based adolescent sexual health programming, a better understanding of theory use and how to determine intervention effects is necessary. It is critical that we identify effective methods and practical applications of interventions when developing and evaluating parent-based initiatives. While understanding the theoretical constructs and methods of an intervention is helpful, reporting the parameters and applications of the methods is an essential next step,29 albeit beyond the scope of this study. The use of existing taxonomies to select methods and applications that operationalize theory may strengthen an intervention.
Meta-Analyses
Consistent with a previous descriptive systematic review,19 our meta-analyses revealed that intervention group parents and their adolescents reported significant increases in the amount of and comfort with parent-child sexual health communication in most of the primary studies. However, effect sizes ranged widely across trials. All but one trial53 with a large effect scored 4 for theory use (highest). Further analysis is needed to determine the extent to which the size of the effect differs depending on theory use, methods, applications and dose. We identified some potential sources of heterogeneity, including inconsistencies in outcome measures, dose, intervention modalities and setting. This may be more important in conducting meta-analyses of community-based, parent-based adolescent sexual health intervention trials than the heterogeneity of the findings themselves.83 Developing consensus on the optimal outcome measures would reduce inconsistencies in evaluating effects and allow for further analysis across trials. Nonetheless, the estimates for communication and comfort suggested the same positive direction of effect across all trials, regardless of delivery mode. Indeed, compared with control parents, intervention parents had an elevated likelihood of reporting increased communication and comfort with communication.
While some of the trials measured adolescent-level outcomes, too few consistently measured outcomes to allow us to pool them and assess their effects on adolescent behaviors. Additional trials that measure adolescent behavioral outcomes are needed before it is possible to assess the impact of parent-based intervention effects on adolescent-level outcomes. The data suggest a positive direction of effects for parent-level outcomes, and these were not consistently smaller for low-dose than for higher dose interventions. However, the evidence of positive effects is not as strong for short, self-paced interventions as for long, group-based ones. Further research is needed to determine whether low-dose interventions or delivery modalities other than the traditional group, multisession format result in positive, sustained effects.
Limitations
The high levels of heterogeneity observed in the meta-analyses suggest caution when interpreting the findings. We believe this heterogeneity is related to wide variations in participant type, trial design, sample size, mode of intervention delivery and communication measures used; we compensated for it by using a random effects model and by subdividing trials into groups with similar outcomes.
Further, there is a risk of publication bias since negative trial findings are less likely to be submitted and published, and thus were not included in this study. To reduce study limitations related to inclusion bias, our systematic search strategy was conducted in collaboration with a public health librarian. Use of standardized intervention descriptions, as outlined by Bartholomew et al.29 and Michie et al.,27 facilitated the consistent characterization of theory use, methods and applications. We observed general patterns of theory use, which may support further exploration of such use in intervention development. For example, five of the six trials with the largest effect sizes in both meta-analyses scored highest in theory use. Although this aspect was central to the descriptive systematic review, and the extent of theory use was categorized, it was not included in the meta-analyses. In addition, searching only English-language journals may have led to the exclusion of pertinent trials published in other languages. By restricting selection to peer-reviewed publications to assure reporting quality, we may have missed relevant gray literature, particularly that which might have reported negative findings. Finally, because of the sensitive nature of the topic, recruiting an adequate sample size may be a general challenge for sexual health researchers.
Conclusions
Our findings provide preliminary support for the effectiveness of parent-based interventions on parent-child sexual health communication, and point to future research needs.7 Lower dose, barrier-reducing interventions, such as self-paced ones, hold promise for the dissemination of parent-based interventions, have been reported to be acceptable to minority families32 and warrant further exploration. More studies with longer follow-up periods that measure adolescent risk behaviors and sexual health outcomes, such as cases of STDs and pregnancy, are needed, and future trials should provide justification for the use of a particular intervention development theory. Greater analysis of the use of theory to understand barriers and design interventions, to explore mediating pathways and moderators, and to examine the impact of theory use on adolescent and parent outcomes would advance the science of implementation research.24,82 Developers and researchers who use theory to design interventions should report, using a standard taxonomy, the theoretical constructs and methods employed to promote change,23,29 and should include the practical applications of those methods to populations and settings. Furthermore, a study of all children in a household could help determine if programs that target parents have the potential for exponential effects on multiple children. Finally, a cost analysis of parent-based interventions would be useful to help determine the potential reach of effective programs.
Acknowledgments
The authors thank Helena VonVille for her valuable contributions to the development and documentation of the search and citation management and selection, and Melissa Peskin for cross-checking trial inclusion screening. Shirley Bluethmann was supported by the Susan G. Komen Foundation (grant KG111378) and the Cancer Education and Career Development Program at the School of Public Health, University of Texas Health Science Center at Houston, funded by the National Cancer Institute (grant R25T 2R25CA57712). The findings and conclusions of this article are those of the authors and do not necessarily represent the official positions of the funding organizations.
Contributor Information
Diane Santa Maria, Department of Nursing Systems, University of Texas School of Nursing, Houston.
Christine Markham, Division of Health Promotion and Behavioral Sciences, University of Texas School of Public Health, Houston.
Patricia Dolan Mullen, Division of Health Promotion and Behavioral Sciences, University of Texas School of Public Health, Houston.
Shirley Bluethmann, Center for Health Promotion and Prevention Research, University of Texas School of Public Health.
References
- 1.Hamilton BE, et al. Annual summary of vital statistics: 2010–2011. Pediatrics. 2013;131(3):548–558. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kost K, Henshaw S, Carlin L. U S Teenage Pregnancies, Births and Abortions: National and State Trends and Trends by Race and Ethnicity. New York: Guttmacher Institute; 2010. [Google Scholar]
- 3.Keppel KG. Ten largest racial and ethnic health disparities in the United States based on Healthy People 2010 objectives. American Journal of Epidemiology. 2007;166(1):97–103. doi: 10.1093/aje/kwm044. [DOI] [PubMed] [Google Scholar]
- 4.Kirby D. Emerging Answers 2007: Research Findings on Programs to Reduce Teen Pregnancy and Sexually Transmitted Diseases. Washington, DC: National Campaign to Prevent Teen and Unplanned Pregnancy; 2007. [Google Scholar]
- 5.Whitaker DJ, Miller KS. Parent-adolescent discussions about sex and condoms: impact on peer influences of sexual risk behavior. Journal of Adolescent Research. 2000;15(2):251–273. [Google Scholar]
- 6.DiClemente RJ, et al. Parental monitoring: association with adolescents' risk behaviors. Pediatrics. 2001;107(6):1363–1368. doi: 10.1542/peds.107.6.1363. [DOI] [PubMed] [Google Scholar]
- 7.Burrus B, et al. Person-to-person interventions targeted to parents and other caregivers to improve adolescent health: a community guide systematic review. American Journal of Preventive Medicine. 2012;42(3):316–326. doi: 10.1016/j.amepre.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Hutchinson MK, Wood EB. Reconceptualizing adolescent sexual risk in a parent-based expansion of the theory of planned behavior. Journal of Nursing Scholarship. 2007;39(2):141–146. doi: 10.1111/j.1547-5069.2007.00159.x. [DOI] [PubMed] [Google Scholar]
- 9.Hutchinson MK, et al. The role of mother-daughter sexual risk communication in reducing sexual risk behaviors among urban adolescent females: a prospective study. Journal of Adolescent Health. 2003;33(2):98–107. doi: 10.1016/s1054-139x(03)00183-6. [DOI] [PubMed] [Google Scholar]
- 10.Prado G, Pantin H. Reducing substance use and HIV health disparities among Hispanic youth in the USA: the Familias Unidas program of research. Intervención Psicosocial. 2011;20(1):63–73. doi: 10.5093/in2011v20n1a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiIorio C, et al. Keepin' it R.E.A.L.!: results of a mother-adolescent HIV prevention program. Nursing Research. 2006;55(1):43–51. doi: 10.1097/00006199-200601000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Stanton B, et al. Randomized trial of a parent intervention: Parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics & Adolescent Medicine. 2004;158(10):947–955. doi: 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- 13.Guilamo-Ramos V, et al. A parent-based intervention to reduce sexual risk behavior in early adolescence: building alliances between physicians, social workers, and parents. Journal of Adolescent Health. 2011;48(2):159–163. doi: 10.1016/j.jadohealth.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murry VM, et al. Intervention induced changes on parenting practices, youth self-pride and sexual norms to reduce HIV-related behaviors among rural African American youths. Journal of Youth and Adolescence. 2011;40(9):1147–1163. doi: 10.1007/s10964-011-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atienzo EE, et al. Interventions with parents to modify sexual behavior in adolescents. Salud Pública de México. 2011;53(2):160–171. doi: 10.1590/s0036-36342011000200009. in Spanish. [DOI] [PubMed] [Google Scholar]
- 16.Wight D, Fullerton D. A review of interventions with parents to promote the sexual health of their children. Journal of Adolescent Health. 2013;52(1):4–27. doi: 10.1016/j.jadohealth.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Bastien S, Kajula LJ, Muhwezi WW. A review of studies of parent-child communication about sexuality and HIV/AIDS in sub-Saharan Africa. Reproductive Health. 2011;8(1):25. doi: 10.1186/1742-4755-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Downing J, et al. A systematic review of parent and family-based intervention effectiveness on sexual outcomes in young people. Health Education Research. 2011;26(5):808–833. doi: 10.1093/her/cyr019. [DOI] [PubMed] [Google Scholar]
- 19.Akers AY, Holland CL, Bost J. Interventions to improve parental communication about sex: a systematic review. Pediatrics. 2011;127(3):494–510. doi: 10.1542/peds.2010-2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michie S, et al. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology. 2008;57(4):660–680. [Google Scholar]
- 21.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 22.Buhi ER, Goodson P. Predictors of adolescent sexual behavior and intention: a theory-guided systematic review. Journal of Adolescent Health. 2007;40(1):4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 23.Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. Journal of Public Health Dentistry. 2011;71(Suppl. 1):S20–S33. doi: 10.1111/j.1752-7325.2011.00223.x. [DOI] [PubMed] [Google Scholar]
- 24.Painter JE, et al. The use of theory in health behavior research from 2000 to 2005: a systematic review. Annals of Behavioral Medicine. 2008;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 25.Hardeman W, et al. Application of the theory of planned behaviour in behaviour change interventions: a systematic review. Psychology & Health. 2002;17(2):123–158. [Google Scholar]
- 26.Bandura A. Social cognitive theory. In: Van Lange PAM, Kruglanski AW, Higgins ET, editors. Handbook of Theories of Social Psychology. Thousand Oaks, CA: Sage Publications; 2011. pp. 349–373. [Google Scholar]
- 27.Michie S, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 28.Rossi PH, Lipsey MW, Freeman HE. Evaluation: A Systematic Approach. seventh. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 29.Bartholomew LK, et al. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco: Jossey-Bass; 2011. [Google Scholar]
- 30.Kirby D, Miller BC. Interventions designed to promote parent-teen communication about sexuality. New Directions for Child and Adolescent Development. 2002;97:93–110. doi: 10.1002/cd.52. [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M, et al. Introduction to Meta-Analysis. West Sussex, England: Wiley; 2011. [Google Scholar]
- 32.Villarruel AM, Loveland-Cherry CJ, Ronis DL. Testing the efficacy of a computer-based parent-adolescent sexual communication intervention for Latino parents. Family Relations. 2010;59(5):533–543. doi: 10.1111/j.1741-3729.2010.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barr EM, Moore MJ, Howard A. A pilot project to increase parent comfort communicating with their children about sexual health. American Journal of Sexuality Education. 2012;7(3):253–266. [Google Scholar]
- 34.DiIorio CK, McCarty F, Pluhar E. Set the P.A.C.E.!: results of an HIV prevention intervention for mothers of young children. Journal of HIV/AIDS & Social Services. 2011;10(3):290–310. [Google Scholar]
- 35.Evans WD, et al. Effects of media messages on parent-child sexual communication. Journal of Health Communication. 2012;17(5):498–514. doi: 10.1080/10810730.2011.635772. [DOI] [PubMed] [Google Scholar]
- 36.O'Donnell L, et al. Especially for daughters: parent education to address alcohol and sex-related risk taking among urban young adolescent girls. Health Promotion Practice. 2010;11(3, Suppl):70S–78S. doi: 10.1177/1524839909355517. [DOI] [PubMed] [Google Scholar]
- 37.Schuster MA, et al. Evaluation of Talking Parents, Healthy Teens, a new worksite based parenting programme to promote parent-adolescent communication about sexual health: randomised controlled trial. BMJ. 2008;337(7664):273–277. doi: 10.1136/bmj.39609.657581.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lederman RP, Chan W, Roberts-Gray C. Parent-Adolescent Relationship Education (PARE): program delivery to reduce risks for adolescent pregnancy and STDs. Behavioral Medicine. 2008;33(4):137–143. doi: 10.3200/BMED.33.4.137-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DiIorio C, et al. REAL men: a group-randomized trial of an HIV prevention intervention for adolescent boys. American Journal of Public Health. 2007;97(6):1084–1089. doi: 10.2105/AJPH.2005.073411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dancy BL, et al. African American adolescent females: mother-involved HIV risk-reduction intervention. Journal of HIV/AIDS & Social Services. 2009;8(3):292–307. doi: 10.1080/15381500903130488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burgess V, Dziegielewski SF, Green CE. Improving comfort about sex communication between parents and their adolescents: practice-based research within a teen sexuality group. Brief Treatment and Crisis Intervention. 2005;5(4):379–390. [Google Scholar]
- 42.O'Donnell L, et al. Saving Sex for Later: an evaluation of a parent education intervention. Perspectives on Sexual and Reproductive Health. 2005;37(4):166–173. doi: 10.1363/psrh.37.166.05. [DOI] [PubMed] [Google Scholar]
- 43.McKay MM, et al. Family-level impact of the CHAMP Family Program: a community collaborative effort to support urban families and reduce youth HIV risk exposure. Family Process. 2004;43(1):79–93. doi: 10.1111/j.1545-5300.2004.04301007.x. [DOI] [PubMed] [Google Scholar]
- 44.Forehand R, et al. Efficacy of a parent-based sexual-risk prevention program for African American pre-adolescents: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2007;161(12):1123–1129. doi: 10.1001/archpedi.161.12.1123. [DOI] [PubMed] [Google Scholar]
- 45.Blake SM, et al. Effects of a parent-child communications intervention on young adolescents' risk for early onset of sexual intercourse. Family Planning Perspectives. 2001;33(2):52–61. [PubMed] [Google Scholar]
- 46.Anderson NL, et al. Evaluating the outcomes of parent-child family life education. Scholarly Inquiry for Nursing Practice. 1999;13(3):211–234. [PubMed] [Google Scholar]
- 47.Causey K, et al. Using theater arts to engage Latino families in dialogue about adolescent sexual health: the PATH-AT program. Journal of Health Care for the Poor and Underserved. 2012;23(1):347–357. doi: 10.1353/hpu.2012.0036. [DOI] [PubMed] [Google Scholar]
- 48.DuRant RH, et al. An evaluation of a mass media campaign to encourage parents of adolescents to talk to their children about sex. [accessed June 1, 2013];Journal of Adolescent Health. 2006 38(3):298.e1–298.e9. doi: 10.1016/j.jadohealth.2004.11.133. http://www.jahonline.org/article/S1054-139X%2804%2900445-8/abstract?cc=y. [DOI] [PubMed] [Google Scholar]
- 49.Silitsky C, Jones SG. Mothers' voices: enhancing mother-child communication for HIV prevention. Journal of HIV/AIDS Prevention in Children & Youth. 2004;6(2):33–46. [Google Scholar]
- 50.Bartlett R, Shelton T. Feasibility and initial efficacy testing of an HIV prevention intervention for black adolescent girls. Issues in Mental Health Nursing. 2010;31(11):731–738. doi: 10.3109/01612840.2010.505313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woody JD, Randall AD, D'Souza HJ. A sex education program for mothers: effects, parent characteristics, and practice insights. American Journal of Sexuality Education. 2007;3(1):39–64. [Google Scholar]
- 52.Klein JD, et al. Evaluation of the Parents as Primary Sexuality Educators program. Journal of Adolescent Health. 2005;37(3, Suppl):S94–S99. doi: 10.1016/j.jadohealth.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 53.Lefkowitz ES, Sigman M, Au TK. Helping mothers discuss sexuality and AIDS with adolescents. Child Development. 2000;71(5):1383–1394. doi: 10.1111/1467-8624.00234. [DOI] [PubMed] [Google Scholar]
- 54.Green HH, Documét PI. Parent peer education: lessons learned from a community-based initiative for teen pregnancy prevention. Journal of Adolescent Health. 2005;37(3, Suppl):S100–S107. doi: 10.1016/j.jadohealth.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 55.Szapocznik J, et al. An ecodevelopmental framework for organizing the influences on drug abuse: a developmental model of risk and protection. In: Glantz MD, Hartel CR, editors. Drug Abuse Origins and Interventions. Washington, DC: American Psychological Association; 1999. pp. 331–366. [Google Scholar]
- 56.Ajzen I. Theory of planned behavior. In: Van Lange PAM, Kruglanski AW, Higgins ET, editors. Handbook of Theories of Social Psychology. Thousand Oaks, CA: Sage Publications; 2011. pp. 438–460. [Google Scholar]
- 57.Fishbein M, Middlestadt SE, Hitchcock PJ. Using information to change sexually transmitted disease-related behaviors. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. New York: Springer Science+Business Media; 1994. pp. 61–78. [Google Scholar]
- 58.Semaan S, et al. A profile of U.S.-based trials of behavioral and social interventions for HIV risk reduction. Journal of Acquired Immune Deficiency Syndromes. 2002;30(Suppl. 1):S30–S50. [PubMed] [Google Scholar]
- 59.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Routledge Academic; 2013. [Google Scholar]
- 60.Warner RM. Applied Statistics: From Bivariate Through Multivariate Techniques. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- 61.McGough JJ, Faraone SV. Estimating the size of treatment effects: moving beyond p values. Psychiatry. 2009;6(10):21–29. [PMC free article] [PubMed] [Google Scholar]
- 62.Mather M. Data Brief. Washington, DC: Population Reference Bureau; 2010. [ccessed Jan. 1, 2014]. U.S. children in single-mother families. http://www.prb.org/pdf10/single-motherfamilies.pdf. [Google Scholar]
- 63.Guilamo-Ramos V, et al. Paternal influences on adolescent sexual risk behaviors: a structured literature review. [accessed June 1, 2013];Pediatrics. 2012 130(5):e1313–e1325. doi: 10.1542/peds.2011-2066. http://pediatrics.aappublications.org/content/130/5/e1313.full.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wilson EK, Dalberth BT, Koo HP. “We're the heroes!”: fathers' perspectives on their role in protecting their preteenage children from sexual risk. Perspectives on Sexual and Reproductive Health. 2010;42(2):117–124. doi: 10.1363/4211710. [DOI] [PubMed] [Google Scholar]
- 65.Ohalete N, Georges J, Doswell W. Tales from the “hood”: placing reproductive health communication between African American fathers and children in context. ABNF Journal. 2010;21(1):14–20. [PubMed] [Google Scholar]
- 66.DeHaven MJ, et al. Health programs in faith-based organizations: Are they effective? American Journal of Public Health. 2004;94(6):1030–1036. doi: 10.2105/ajph.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith GC, Palmieri PA. Risk of psychological difficulties among children raised by custodial grand-parents. Psychiatric Services. 2007;58(10):1303–1310. doi: 10.1176/appi.ps.58.10.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Garofalo R, et al. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101(5):895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- 69.Bratteli M, Bjelde K, Pigatti L. Grandparent and kinship foster care: implications of licensing and payment policies. Journal of Gerontological Social Work. 2008;51(3-4):228–246. [PubMed] [Google Scholar]
- 70.Pyatak EA, et al. Conducting intervention research among underserved populations: lessons learned and recommendations for researchers. Archives of Physical Medicine and Rehabilitation. 2013;94(6):1190–1198. doi: 10.1016/j.apmr.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lightfoot M. HIV prevention for adolescents: Where do we go from here? American Psychologist. 2012;67(8):661–671. doi: 10.1037/a0029831. [DOI] [PubMed] [Google Scholar]
- 72.Mitchell SJ, et al. Internet and mobile technology use among urban African American parents: survey study of a clinical population. [accessed June 1, 2013];Journal of Medical Internet Research. 2014 16(1):e9. doi: 10.2196/jmir.2673. http://www.jmir.org/2014/1/e9/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baumeister RF, Vohs KD, Tice DM. The strength model of self-control. Current Directions in Psychological Science. 2007;16(6):351–355. [Google Scholar]
- 74.Prestwich AS, et al. Does theory influence the effectiveness of health behavior interventions? Meta-analysis. Health Psychology. 2014;33(5):465–474. doi: 10.1037/a0032853. [DOI] [PubMed] [Google Scholar]
- 75.Dittus PJ, Jaccard J. Adolescents' perceptions of maternal disapproval of sex: relationship to sexual outcomes. Journal of Adolescent Health. 2000;26(4):268–278. doi: 10.1016/s1054-139x(99)00096-8. [DOI] [PubMed] [Google Scholar]
- 76.Cox MF. Maternal demandingness and responsiveness as predictors of adolescent abstinence. Journal of Pediatric Nursing. 2007;22(3):197–205. doi: 10.1016/j.pedn.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 77.Parkes A, et al. Is parenting associated with teenagers' early sexual risk-taking, autonomy and relationship with sexual partners? Perspectives on Sexual and Reproductive Health. 2011;43(1):30–40. doi: 10.1363/4303011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Miller KS, et al. Family communication about sex: What are parents saying and are their adolescents listening? Family Planning Perspectives. 1998;30(5):218–222. 235. [PubMed] [Google Scholar]
- 79.Donenberg GR, Paikoff R, Pequegnat W. Introduction to the special section on families, youth, and HIV: family-based intervention studies. Journal of Pediatric Psychology. 2006;31(9):869–873. doi: 10.1093/jpepsy/jsj102. [DOI] [PubMed] [Google Scholar]
- 80.Li X, Feigelman S, Stanton B. Perceived parental monitoring and health risk behaviors among urban low-income African-American children and adolescents. Journal of Adolescent Health. 2000;27(1):43–48. doi: 10.1016/s1054-139x(99)00077-4. [DOI] [PubMed] [Google Scholar]
- 81.Baptiste DR, et al. Determinants of parental monitoring and preadolescent sexual risk situations among African American families living in urban public housing. Journal of Child and Family Studies. 2007;16(2):261–274. [Google Scholar]
- 82.Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implementation Science. 2010;5(1):14. doi: 10.1186/1748-5908-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Higgins JP. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. International Journal of Epidemiology. 2008;37(5):1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]