Abstract
Abstract. Background: The validity and reliability of suicide statistics have been questioned and few nationwide studies of deliberate self-harm have been presented. Aim: To calculate rates of deliberate self-harm in Denmark in order to investigate trends and assess the reliability of hospital records. Method: A register study based on all individuals recorded with an episode of deliberate self-harm or probable deliberate self-harm in nationwide registers during 1994–2011. Results: A substantial difference in the rates of deliberate self-harm and probable deliberate self-harm was noted for both genders. The average incidence rate of deliberate self-harm for women and men was 130.7 (95% CI = 129.6–131.8) per 100,000 and 86.9 (95% CI = 86.0–87.8) per 100,000, respectively. The rates of deliberate self-harm for women increased from 137.6 (95% CI = 132.9–142.3) per 100,000 in 1994 to 152.7 (95% CI = 147.8–157.5) in 2011. For a subgroup of younger women aged 15–24 years, an almost threefold increase was observed, IRR = 2.5 (95% CI = 2.4–2.7). The most frequently used method was self-poisoning. Conclusion: The rates of deliberate self-harm and probable deliberate self-harm differed significantly. An increased incidence of deliberate self-harm among young Danish women was observed, despite detection bias. An improved registration procedure of suicidal behavior is needed.
Keywords: deliberate self-harm, suicidal behavior, incidence rates, hospital records, nationwide
Member countries of the World Health Organization (WHO) have agreed that surveillance on numbers of suicide and suicide attempt should be a top priority among suicide preventive initiatives (Saxena & Setoya, 2014; WHO, 2014).
Although more studies have been conducted within suicidology over recent decades, the validity and reliability of statistics have been questioned and detection bias is commonly suggested (Bertolote & Fleischmann, 2005; Gray et al., 2014; Kapusta, Tran, & Rockett, 2011; Tollefsen, Hem, & Ekeberg, 2012). In order to avoid underreporting, registration of both fatal and nonfatal suicidal outcomes should be standardized within individual countries and between countries (Data and Surveillance Task Force of the National Action Alliance for Suicide & Prevention, 2014; De Leo et al., 2013; Kapusta et al., 2011).
Despite general uncertainty in international estimates, the prevalence of suicide attempts has been reported to increase in some countries (Christiansen, Larsen, Agerbo, Bilenberg, & Stenager, 2013; Nock et al., 2008; Perry et al., 2012; Ting, Sullivan, Boudreaux, Miller, & Camargo, 2012). Large national and cross-national studies have reported variation in rates according to gender, age, and method (Christiansen et al., 2013; Nock et al., 2008; Perry et al., 2012). Few studies have attempted to calculate the rates of hospital-treated deliberate self-harm on a national level (Christiansen et al., 2013; Perry et al., 2012). A Finnish study based on national hospitals discharge records found an incidence rate (IR) of first episode of suicide attempt of 44 per 100,000 for both genders during 1996–2003 (Haukka, Suominen, Partonen, & Lonnqvist, 2008). Reports from the US noted an increase over time in rates of contacts by poisoning, hence a proxy of attempted suicide (Spiller, Appana, & Brock, 2010).
Previous studies of attempted suicide have been based on selected localities, such as one or more hospitals, a specific city, or province (Christiansen et al., 2013; Haukka et al., 2008). Other studies have estimated rates of suicide attempt based on local or regional data obtained from emergency rooms and local hospital discharge records (Bergen, Hawton, Waters, Cooper, & Kapur, 2010) or databases, with varying validity (Bossuyt & Van Casteren, 2007; Saberi-Zafaghandi, Hajebi, Eskandarieh, & Ahmadzad-Asl, 2012). Still, measurement of national IRs is important; both in order to observe the development of suicidal behavior as an indicator of public health, but also in order to survey recording procedures as part of an on-going registration (De Leo et al., 2013).
Suicide attempt is a significant risk factor for subsequent suicidal behavior but also linked to poor psychosocial outcome in general (Carroll, Metcalfe, & Gunnell, 2014; Goldman-Mellor, Caspi, & Harrington, 2014) and it represents a costly imbalance for both the individual and society. Thus, accurate rates are needed to target suicide prevention strategies on various levels.
The aim of this study was to examine rates and trends in deliberate self-harm based on nationwide registers in Denmark in the period 1994 to 2011.
Method
Individual-level register data on the entire population living in Denmark from January 1, 1994, through December 31, 2011, were obtained. Each individual in Denmark has a unique, personal identification (ID) number, which is assigned upon birth or migration into the country. Data from various administrative registries can be linked for each individual using this ID number. Somatic and psychiatric hospital contacts in Denmark are reported to the National Registry of Patients and the Psychiatric Central Research Registry including information on date of admission and discharge, diagnosis, reason for contact (e.g., suicide attempt or accident; Lynge, Sandegaard, & Rebolj, 2011; Mors, Perto, & Mortensen, 2011). Diagnoses were recorded according to the 10th revision of WHO International Classification of Diseases (ICD). From 1995 onward the hospital registers also cover contacts to emergency department and outpatient facilities.
Nomenclature
The nomenclature of suicidal behavior is a controversy among experts and relates significantly to an aspect of definition (Silverman, Berman, Sanddal, O'Carroll, & Joiner, 2007). The terminology applied in this paper is deliberate self-harm and it matches the definition of suicide attempt according to WHO defined as (Platt et al. 1992):
An act with a non-fatal outcome, in which an individual deliberately initiates a non-habitual behavior that without intervention from others will cause self-harm, or deliberately ingests a substance in excess of the prescribed or generally recognized therapeutic dosage, and which is aimed at realizing changes which the subject desired via the actual or expected physical consequences (p. 99)
Although this definition is widely accepted, it does not address degree of intention adequately (Platt et al., 1992; Silverman et al., 2007).
Measures of Deliberate Self-Harm
Persons were considered as having had an episode of deliberate self-harm when this had been recorded as the main or subdiagnosis, ICD-10: X60–X84, or where the reason for contact was listed as being deliberate self-harm. Data on contacts were included from both the Psychiatric Research Register and the National Patient Register.
It is well established that deliberate self-harm episodes are under-recorded in Danish hospital registries (Helweg-Larsen, 2006; Nordentoft, 2007). Thus, an operational definition of probable deliberate self-harm was included. This category covered self-harm regardless of intent, for example, poisoning by drugs, biological and nonmedical substances as well as lesions on the hand and forearm. In addition, the following combinations of ICD diagnoses were included: a main diagnosis of a mental disorder, ICD-10: F00-F99, representing organic, psychotic, affective, anxiety, eating, and personality disorders, mental retardation, autism, and behavioral disorders together with one of the following subdiagnoses: S51, S55, S59, S61, S65, S69 (cutting by sharp objects), T36–T50 (poisoning by pharmaceuticals), T52–T60 (poisoning by nonpharmaceuticals) as well as all admissions with a main diagnosis of T39, T40 (poisoning by mild analgesics; except T40.1), T42, T43, and T58 (poisoning by opioids, psychotropics, and by carbon monoxide). While this definition captures more deliberate self-harm it also includes accidents; as many as 30% of cases might not be intentional episodes of deliberate self-harm (Helweg-Larsen, 2006). However, the same definition has been applied previously (Madsen, Agerbo, Mortensen, & Nordentoft, 2013). The guideline for registration in emergency settings is the T39 code in addition to contact code four (deliberate self-harm) given by the Danish health-care authorities (Statens Serum Institut, 2014).
We assessed for double recordings, for example, when the same persons had been registered with an episode of deliberate self-harm twice during the same hospital admission, for instance, in relation to transfers between different units. However, this implies that if a person who was admitted for an episode of deliberate self-harm had another self-harm episode while in admission, this was not considered. Persons who died by suicide during a hospitalization following an episode of deliberate self-harm were considered as suicides and not as episodes of deliberate self-harm.
We distinguished between the following methods of deliberate self-harm: poisonings (T36–T65, X60–69), hanging (X70), drowning (X71), firearms (X72–X74), explosives, fire and burning (X75–X77), sharp objects (S50–S69, X78–79), jumping from high places (X80), moving object (X81–X82), and other methods (X83–X84). S and T diagnoses refer to cases where episodes of deliberate self-harm were identified through the reason to contact variable, stating suicide attempt. If multiple methods were used, the method was determined based on the main diagnosis.
Population Investigated
For the analysis, the entire population aged 10 years and older living in Denmark was observed from January 1, 1994, through December 31, 2011. We applied a cohort design where people migrating in or out of the country were included or excluded on the date of the respective event. Likewise, persons dying were censored on the date of death. During preliminary analysis a minor peak in episodes of deliberate self-harm among infants, toddlers, and young children was noted. We considered this finding as indicative of accidents rather than deliberate self-harm (Alander, Dowd, Bratton, & Kearns, 2000). In order, to ensure a certain level of maturity we thus decided to examine deliberate self-harm in persons aged 10 years or older.
Calculations
Rates of deliberate self-harm were calculated by single calendar year and age increments for men and women. For each age group and gender, the number of events was divided by the population at risk. The exact numbers of person–days spent by each person in the general population in the same age group and gender strata were presented as person–years. Rates were calculated per 100,000 person–years and with 95% confidence intervals. The IR was defined as any episode of deliberate self-harm recorded, that is, several episodes could be recorded for the same individual. Trends in rates were calculated as incidence rates ratios (IRR).
Ethical Considerations
Although personal ID numbers were linked to register data, no information was personally identifiable for researchers. Approval from the Danish Protection Agency was obtained. Further ethical approval was not needed.
Results
In total, 56,995 episodes of deliberate self-harm among women were identified over the observed 43,603,346 person–years in the period from 1994 to 2011. The mean age was 33.9 years (SD = 16.7, range = 10–101, median = 30). For men, 36,847 episodes of deliberate self-harm with a mean age of 36.8 years (SD = 15.5, range 10–101, median = 35) were recorded during 42,385,189 person–years. Mean number of episodes of deliberate self-harm by the same individual per calendar year was 1.3 for women (range = 1–45) and 1.2 (range = 1–24) for men.
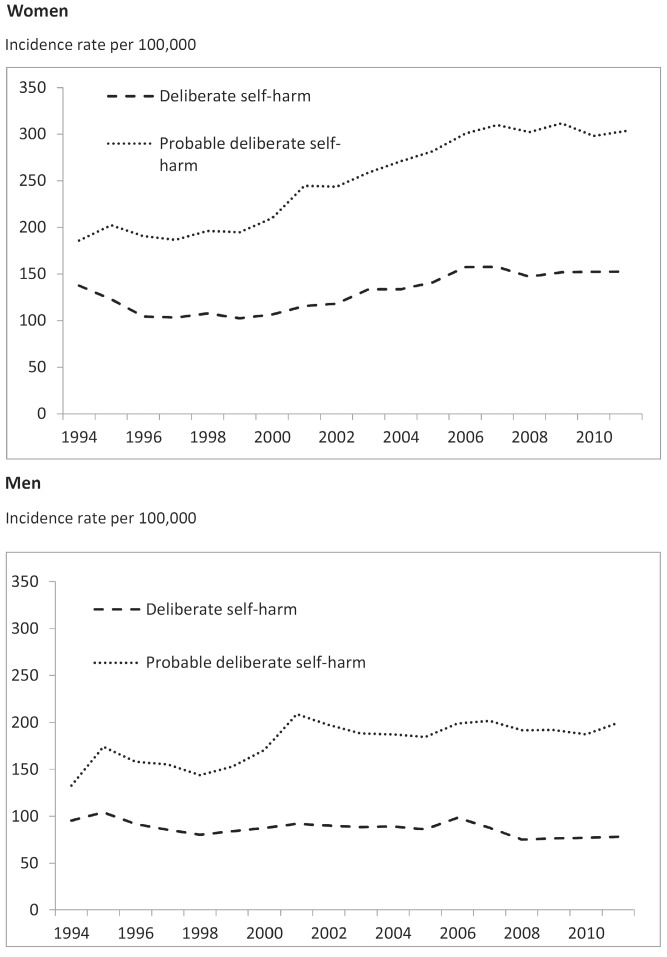
During 1994–2011, the average IR of deliberate self-harm was 130.7 (95% CI = 129.6–131.8) per 100,000 for women, whereas the rate for probable deliberate self-harm was 250.5 (95% CI = 249.0–252.0]. The average IR for men was 86.9 per 100,000 (95% CI = 86.0–87.8) and 179.5 (95% CI = 178.2–180.8) for deliberate self-harm and probable deliberate self-harm, respectively (Figure 1).
Figure 1. lncidence rates by calendar year of registered episodes of deliberate self-harm and probable deliberate self-harm for women and men aged 10+ living in Denmark during 1994–2011.
Trend Over Time
A substantial difference in the IRs for deliberate self-harm and probable deliberate self-harm was noted for both men and women (Figure 1). Furthermore, a steady increase in the IR of women was noted over time; rates of deliberate self-harm increased from 137.6 (95% CI = 132.9–142.3) per 100,000 in 1994 to 152.7 (95% CI = 147.8–157.5) in 2011 (Figure 1).The rate of probable deliberate self-harm increased from 186.0 (95% CI = 180.5–191.5) in 1994 to 303.4 per 100,000 (95% CI = 296.6–310.2) in 2011. An opposite trend was noted for men with regard to rates of deliberate self-harm. Their IR actually decreased from 95.3 (95% CI = 91.3–99.4) per 100,000 to 78.3 (95% CI = 74.8–81.8) from 1994 to 2011, while the IR of probable deliberate self-harm opposed this trend by increasing significantly from 132.8 (95% CI = 128.1–137.5) per 100,000 to 199.5 (95% CI = 193.9–205.1).
Deliberate Self-Harm by Age
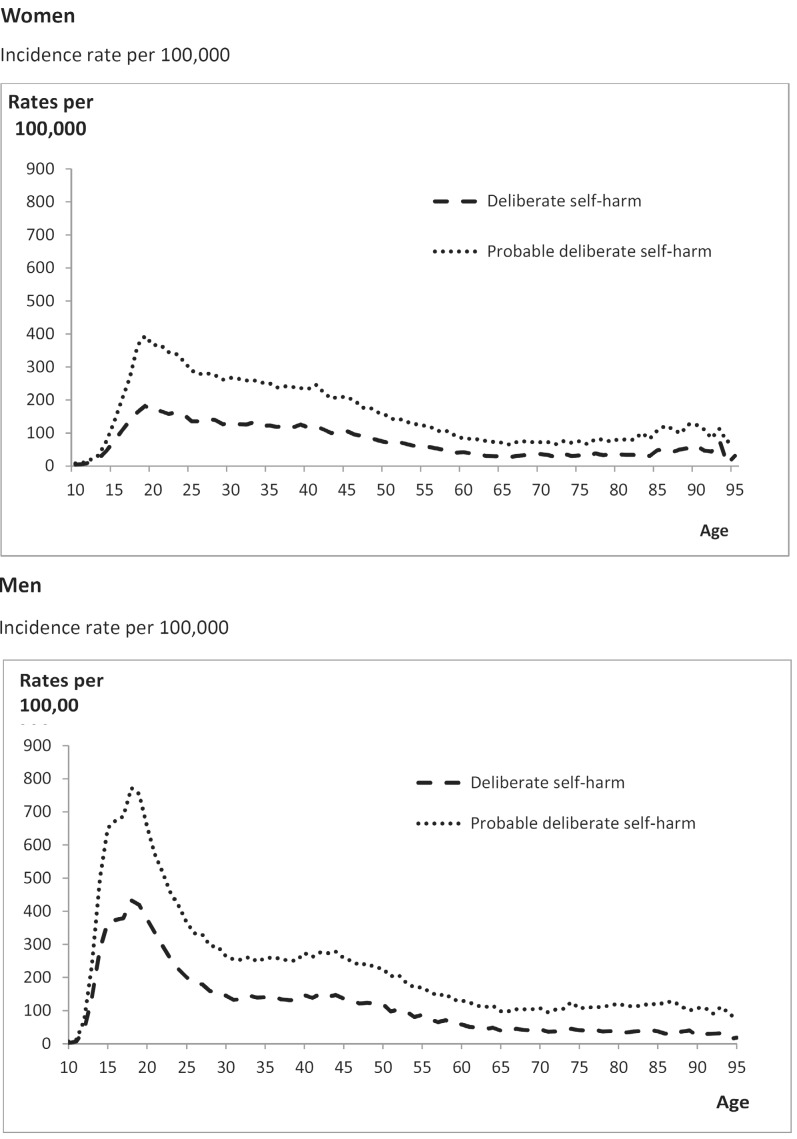
The distribution of deliberate self-harm by single age increments in Figure 2 shows that high rates are found among younger age groups for both genders.
Figure 2. lncidence rates by age of registered episodes of deliberate self-harm and probable deliberate self-harm for women and men aged 10+ living in Denmark during 1994–2011.
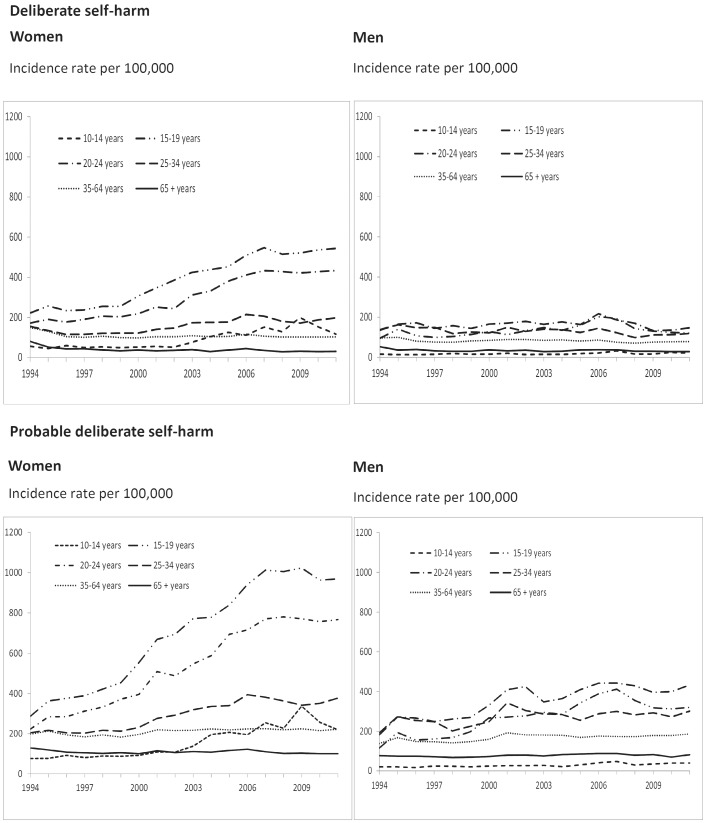
By examining the trend in the IR over time by age groups, an increase in both registered deliberate self-harm and probable deliberate self-harm for women was observed (Figure 3). For young women aged 15–19 years, the IR for deliberate self-harm increased from 221.6 (95% CI = 198.5–244.6) in 1994 to 543.8 (95% CI = 509.2–578.5) per 100,000 in 2011. The IR of probable deliberate self-harm for the same age group increased from 287.1 (95% CI = 260.9–313.3) to 968.9 (95% CI = 922.7–1015.1) per 100,000. Similarly, the IR for women aged 20–24 years increased over the studied period, that is, from 171.9 (95% CI = 152.9–191) to 432.9 (95% CI = 401.5–464.3) per 100,000 while rates of probable deliberate self-harm increased from 223.6 (95% CI = 201.8–245.3) to 766.8 (95% CI = 725–808.6) per 100,000.
Figure 3. lncidence rates by age group and calendar year of deliberate self-harm and probable deliberate self-harm for women living in Denmark during 1994–2011.
The trend for men was also characterized by increasing rates; young men aged 20–24 years had an IR of 134.5 (95% CI = 118–151) in 1994 and 146.6 (95% CI = 128.6–164.5) per 100,000 in 2011. An increasing trend was also noted for rates of probable deliberate self-harming episodes, which rose from 181.4 (95% CI = 162.3–200.6) per 100,000 to 433.4 (402.6–464.2).
Deliberate Self-Harm Among Adolescents and Young Adults
Data for the age groups of 15–19 and 20–24 years were combined to study the observed increase into more detail; an almost threefold higher rate of deliberate self-harm was observed for young women in 2011, IRR = 2.5 (95% CI = 2.4–2.7), p < .001, for 2011 measured relative to 1994. For young men, the IRR was 1.1 (95% CI = 1.1–1.2), p < .001.
Methods of Deliberate Self-Harm
For the entire sample, the most frequently used method was self-poisoning followed by sharp objects (Figure 4). A similar distribution of methods was observed for adolescents and young adults aged 15–24 years. Seemingly, much of the observed increase in the deliberate self-harm rate was related to poisoning.
Figure 4. Incidence rates pr. 100.000 by means of deliberately self-harming methods for women and men in all age groups as well as for those aged 15-24 years living in Denmark during 1994–2011*Note. Other include drowning, jumping, moving objects, weapon, and unspecific means.
Discussion
Using Danish register data we were able to calculate national rates of deliberate self-harm based on all registered hospital contacts of episodes of deliberate self-harm and probable deliberate self-harm over the period between 1994 and 2011. This is, to our knowledge, one of the few attempts of estimating the national IR for deliberate self-harm.
Main Findings
An increase in the IR of deliberate self-harm was observed over recent years, especially among young women. This trend was confirmed by being observed both for deliberate self-harm as well as probable deliberate self-harm. Deliberate self-harming episodes are predominantly carried out using self-poisoning; this method is being increasingly used by young women in the age group of 15–24 years. We demonstrated differences in rates between deliberate self-harm and probable deliberate self-harm, hence identifying the risk of detection bias.
Increasing IRs of deliberate self-harm have been noted in other countries using data from both national databases as well as emergency records over the same decades (Spiller et al., 2010; Ting et al., 2012). Nevertheless, conflicting trends have also been reported; an Irish study using nationwide register data detected an initial decrease in rates from 2003 to 2006 and a later increase from 2006 to 2009 (Perry et al., 2012). Also, a Belgian study with two separate follow-up periods and a limited sample identified through general practitioner records did not detect significant changes in age-specific IRs over time (Bossuyt & Van Casteren, 2007). Yet other countries have reported decreasing trends over comparable periods albeit using data from selected hospital records or selected emergency departments (Bergen et al., 2010; Kjartansdottir, Bergmann, Arnadottir, & Bjornsson, 2012).
The increase in the IR over time was particularly marked among adolescents and young women. A similar trend has been reported for other countries albeit with shorter or over different periods (Corcoran, Keeley, O'Sullivan, & Perry, 2004; Levinson, Haklai, Stein, & Gordon, 2006; Perry et al., 2012). The fact that adolescents and young women account for a majority of deliberate self-harm is well known internationally (Hawton & van Heeringen, 2009). Cross-national and national reports have identified female gender and younger age to be associated with increased risk and rates of deliberate self-harm (Borges et al., 2010; Nock et al., 2008). A recent WHO multicenter study found the highest rates of deliberate self-harm among women aged 20–24 years, an overall female-to-male ratio of 2:1, and that analgesics were the most frequent used method of self-poisoning (Flavio et al., 2013). An increase in deliberate self-harm by drug poisoning of younger age groups has been reported in recent international studies (Haukka et al., 2008; Hawton, Rodham, Evans, & Harriss, 2009; Kjartansdottir et al., 2012; Spiller et al., 2010). This increase has, for instance, motivated a pack size restriction for mild analgesics sold as over-the-counter drugs in pharmacies in several European countries (Gunnell et al., 1997; Hawton et al., 2013). This was implemented in Denmark in 2013 (Danish Ministry of Health, 2013).
We found a difference in rates with respect to deliberate self-harm and probable deliberate self-harm. The under-recording of deliberate self-harm in the Danish registers has been pointed out (Morthorst, Krogh, Erlangsen, Alberdi, & Nordentoft, 2012). In general, data quality is a major concern in suicidal research; the coverage and quality of data vary strongly from country to country (Kapusta et al., 2011). People who get in contact with emergency departments owing to deliberate self-harm actions often require clinical procedures with a life-saving focus rather than uniform administrative surveillance. This may lead to differences in registration and surveillance procedures (De Leo et al., 2013), which often make the registration of deliberate self-harm without additional coding of intent less reliable than, for instance, completed suicide (Tollefsen et al., 2012).
Limitations and Strengths
The Danish register data are collected for administrative purposes, not research. Although the Danish National Board of Health encourages a standardized and consistent registration of deliberate self-harm (Statens Serum Institut, 2014), a substantial under-recording is taking place. By including the category of probable deliberate self-harm, we identify more episodes of deliberate self-harm at the expense of measure validity; likely cases of unintentional self-harm are also present in this group, which as stated may add up to as much as 30% of misclassified cases of deliberate self-harm (Helweg-Larsen, 2006), hence implying a risk of overestimation. Both options include the risk of detection bias; however, underestimation is thought to be most prominent (Nordentoft & Sogaard, 2005) and this definition of probable deliberate self-harm has been implied in previous studies (Erlangsen et al., 2014; Madsen et al., 2013).
People seeking hospital care after an episode of deliberate self-harm are a subgroup of all people with deliberate self-harm. Some people might seek medical advice from their general practitioner after an episode of deliberate self-harm while yet others might for various reasons not seek any health care at all (Bertolote & Fleischmann, 2009; Hawton et al., 2009). Hence the persons examined in this study may not be representative of all persons who deliberately self-harm at the risk of affecting the external validity.
The current study examined deliberate self-harms in persons aged 10 years or older. Suicidal behavior does occur, albeit seldom, in young children (Goldman-Mellor et al., 2014; Pelkonen & Marttunen, 2003). Age 10 was used as cutoff in order to ensure a certain level of maturity while allowing us to examine the prevalence of self-harm among very young individuals. However, the data did not allow us to distinguish between records of accidental self-injuries and suicidal behavior with sufficient certainty in younger children, unless of course there was a registration of contact code two for accidents, in which case the contact was not included in the calculations.
One of the main strengths of the study is that the Danish nationwide registers provide us with a unique opportunity to survey epidemiological trends on an entire population level (Lynge et al., 2011; Mors et al., 2011). The possibility to merge data on an individual level owing to personal ID numbers makes analyses even more accurate and sophisticated by having access to multiples registers. In general, the reported confidence intervals were narrow, which indicates less uncertainty in the estimates.
The trends observed in this study were reflected in both examined outcomes, which add strength to the validity of the finding. Furthermore, the increasing trend over time observed for women aged 15–24 years seems valid given that no change was observed for other age groups; we have no reason to assume misreporting over time for a specific age group.
Clinical Implications
The WHO has encouraged accurate registration and surveillance (Saxena & Setoya, 2014; WHO, 2014) and we have shown that there still remains an evitable challenge to registration procedures even in a Western country with straightforward administrative policies. The Comprehensive Mental Health Action Plan 2013–2020 along the WHO stresses the need for targeted suicide preventions addressing trends suicidal behavior. In Denmark, these findings evoke concern. Subsequent interventions aiming to reduce deliberate self-harm should focus on younger age groups and take action by addressing the female gender. Previous studies have shown that pack size restriction on mild analgesics is effective in reducing self-harm (Hawton et al., 2013), and in 2013 this measure was implemented in Denmark. Moreover, therapeutic interventions and access to health care such as treatment offered in Centers of Excellence in Suicide Prevention in Denmark must still be provided and developed (Erlangsen et al., 2014).
Conclusion
In sum, the increasing trend in the rate of deliberate self-harm, particularly among adolescents and young women, is demonstrated. This high-risk group needs to be factored in suicide prevention strategies as both pre- and postvention. Although evidence has been provided for intensive psychotherapy in young age groups presenting with self-harm, we may also have to focus on nationwide screening initiatives or surveillance of young people with failure to thrive in order to prevent engagement in suicidal behavior. Regarding the validity of data, the difference in rates with respect to deliberate self-harm and probable deliberate self-harm emphasizes the need for improvement of registration procedures of suicidal behavior in Denmark.
Acknowledgments
The authors have no declaration of interest to report.
Biographies
Britt Morthorst is an MSc and PhD student at the Faculty of Health Sciences Copenhagen, Denmark. She has conducted clinical intervention trials in suicide prevention. An ongoing project focuses on means restriction, in which she leads a study on pack size restriction of mild analgesics sold in Danish pharmacies.
Bodil Soegaard is Master in Health Science and Clinical Therapist at the Centre of Suicide Prevention Aabenraa, Denmark. She is also a research assistant at the Focused Research Unit of Psychiatry, Aabenraa Region of Southern Denmark.
Merete Nordentoft is a professor in clinical psychiatry. She has supervised 30 PhD students and was a principal investigator for 12 large randomized controlled trials and many epidemiology studies. She has received distinguished prizes such as from the Centre of Global Excellence 2012 and is national leading expert in suicide prevention.
Annette Erlangsen, PhD, is Associate Professor and Program Leader for Research on Suicide Prevention at the Research Unit, Mental Health Centre Copenhagen, Denmark. Her research focus is on risk populations and interventions using register data. She is currently Secretary–Treasurer of the International Academy of Suicide Research.
References
- Alander S. W., Dowd M. D., Bratton S. L., & Kearns G. L. (2000). Pediatric acetaminophen overdose: Risk factors associated with hepatocellular injury. Archives of Pediatrics & Adolescent Medicine, , 346–350. [DOI] [PubMed] [Google Scholar]
- Bergen H., Hawton K., Waters K., Cooper J., & Kapur N. (2010). Epidemiology and trends in non-fatal self-harm in three centres in England, 2000 to 2007. British Journal of Psychiatry, , 493–498. [DOI] [PubMed] [Google Scholar]
- Bertolote J. M., & Fleischmann A. (2005). Suicidal behavior prevention: WHO perspectives on research. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, , 8–12. [DOI] [PubMed] [Google Scholar]
- Bertolote J. M., & Fleischmann A. (2009). Suicide thoughts, suicide plans and attempts in the general population on different continents In Wasserman D. & Wasserman C. (Eds.), The Oxford textbook of suicidology and suicide prevention: A global perspective, (pp. 99–104). Oxford, UK: Oxford University Press. [Google Scholar]
- Borges G., Nock M. K., Haro Abad J. M., Hwang I., Sampson N. A., Alonso J., … Kessler R. C. (2010). Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. The Journal of Clinical Psychiatry, , 1617–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossuyt N. & Van Casteren V. (2007). Epidemiology of suicide and suicide attempts in Belgium: Results from the sentinel network of general practitioners. International Journal of Public Health, , 153–157. [DOI] [PubMed] [Google Scholar]
- Carroll R., Metcalfe C., & Gunnell D. (2014). Hospital management of self-harm patients and risk of repetition: Systematic review and meta-analysis. Journal of Affective Disorders, , 476–483. [DOI] [PubMed] [Google Scholar]
- Christiansen E., Larsen K. J., Agerbo E., Bilenberg N., & Stenager E. (2013). Incidence and risk factors for suicide attempts in a general population of young people: A Danish register-based study. The Australian and New Zealand Journal of Psychiatry, , 259–270. [DOI] [PubMed] [Google Scholar]
- Corcoran P., Keeley H. S., O'Sullivan M., & Perry I. J. (2004). The incidence and repetition of attempted suicide in Ireland. European Journal of Public Health, , 19–23. [DOI] [PubMed] [Google Scholar]
- Danish Ministry of Health (2013). Hovedpinepiller i store pakninger kommer på recept [Large packs of headache medication available on prescription only] http://www.sum.dk/Aktuelt/Nyheder/Psykiatri/2013/April/Hovedpinepiller-i-store-pakninger-kommer-paa-recept.aspx
- Data and Surveillance Task Force of the National Action Alliance for Suicide and Prevention (2014). Improving national data systems for surveillance of suicide-related events. American Journal of Preventive Medicine, , S122–S129.25145729 [Google Scholar]
- De Leo D., Milner A., Fleischmann A., Bertolote J., Collings S., Amadeo S., … Wang X. (2013). The WHO START Study. Crisis, , 156–163. [DOI] [PubMed] [Google Scholar]
- Erlangsen A., Lind B. D., Stuart E. A., Qin P., Stenager E., Larsen K. J., … Nordentoft M. (2014). Short-term and long-term effects of psychosocial therapy for people after deliberate self-harm: A register-based, nationwide multicentre study using propensity score matching. The Lancet Psychiatry. Advance online publication 10.1016/S2215-0366(14)00083-2 [DOI] [PubMed] [Google Scholar]
- Flavio M., Martin E., Pascal B., Stephanie C., Gabriela S., Merle K., … Anita R. R. (2013). Suicide attempts in the county of Basel: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour. Swiss Medical Weekly, , w13759. [DOI] [PubMed] [Google Scholar]
- Goldman-Mellor S. J., Caspi A., & Harrington H. (2014). Suicide attempt in young people: A signal for long-term health care and social needs. JAMA Psychiatry, , 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray D., Coon H., McGlade E., Callor W. B., Byrd J., Viskochil J., … McMahon W. M. (2014). Comparative analysis of suicide, accidental, and undetermined cause of death classification. Suicide and Life-Threatening Behavior, , 304–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Hawton K., Murray V., Garnier R., Bismuth C., Fagg J., … Simkin S. (1997). Use of paracetamol for suicide and non-fatal poisoning in the UK and France: Are restrictions on availability justified? Journal of Epidemiology and Community Health, , 175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haukka J., Suominen K., Partonen T., & Lonnqvist J. (2008). Determinants and outcomes of serious attempted suicide: A nationwide study in Finland, 1996-2003. American Journal of Epidemiology, , 1155–1163. [DOI] [PubMed] [Google Scholar]
- Hawton K., Bergen H., Simkin S., Dodd S., Pocock P., Bernal W., … Kapur N. (2013). Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: Interrupted time series analyses. British Medical Journal, , f403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K., Rodham K., Evans E., & Harriss L. (2009). Adolescents who self harm: A comparison of those go to general hospital and those who do not. Child and Adolescent Ment Health, , 24–30. [Google Scholar]
- Hawton K., & van Heeringen K. (2009). Suicide. Lancet, , 1372–1381. [DOI] [PubMed] [Google Scholar]
- Helweg-Larsen K. (2006). Selvmord i Danmark [Suicide in Denmark] Copenhagen: Statens Institut for Folkesundhed. [Google Scholar]
- Kapusta N. D., Tran U. S., & Rockett I. H. (2011). Declining autopsy rates and suicide misclassification: A cross-national analysis of 35 countries. Archives of General Psychiatry, , 1050–1057. [DOI] [PubMed] [Google Scholar]
- Kjartansdottir I., Bergmann O. M., Arnadottir R. S., & Bjornsson E. S. (2012). Paracetamol intoxications: A retrospective population-based study in Iceland. Scandinavian Journal of Gastroenterology, , 1344–1352. [DOI] [PubMed] [Google Scholar]
- Levinson D., Haklai Z., Stein N., & Gordon E. S. (2006). Suicide attempts in israel: Age by gender analysis of a national emergency departments database. Suicide and Life-Threatening Behavior, , 97–102. [DOI] [PubMed] [Google Scholar]
- Lynge E., Sandegaard J. L., & Rebolj M. (2011). The Danish National Patient Register. Scandinavian Journal of Public Health, , 30–33. [DOI] [PubMed] [Google Scholar]
- Madsen T., Agerbo E., Mortensen P. B., & Nordentoft M. (2013). Deliberate self-harm before psychiatric admission and risk of suicide: Survival in a Danish national cohort. Social Psychiatry and Psychiatric Epidemiology, , 1481–1489. [DOI] [PubMed] [Google Scholar]
- Mors O., Perto G. P., & Mortensen P. B. (2011). The Danish Psychiatric Central Research Register. Scandinavian Journal of Public Health, , 54–57. [DOI] [PubMed] [Google Scholar]
- Morthorst B., Krogh J., Erlangsen A., Alberdi F., & Nordentoft M. (2012). Effect of assertive outreach after suicide attempt in the AID (assertive intervention for deliberate self harm) trial: Randomised controlled trial. British Medical Journal, , e4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M. K., Borges G., Bromet E. J., Alonso J., Angermeyer M., Beautrais A., … Williams D. (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry, , 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordentoft M. (2007). Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groups. Faculty of Health Sciences, Copenhagen University Hospital, Psychiatric Center Bispebjerg. [PubMed] [Google Scholar]
- Nordentoft M., & Sogaard M. (2005). Registration, psychiatric evaluation and adherence to psychiatric treatment after suicide attempt. Nordic Journal of Psychiatry, , 213–216. [DOI] [PubMed] [Google Scholar]
- Pelkonen M., & Marttunen M. (2003). Child and adolescent suicide: Epidemiology, risk factors, and approaches to prevention. Paediatric Drugs, , 243–265. [DOI] [PubMed] [Google Scholar]
- Perry I. J., Corcoran P., Fitzgerald A. P., Keeley H. S., Reulbach U., & Arensman E. (2012). The incidence and repetition of hospital-treated deliberate self harm: Findings from the world's first national registry. PLoS.One., , e31663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt S., Bille-Brahe U., Kerkhof A., Schmidtke A., Bjerke T., Crepet P., … Michel K. (1992). Parasuicide in Europe: The WHO/EURO multicentre study on parasuicide. I. Introduction and preliminary analysis for 1989. Acta Psychiatrica Scandinavica, , 97–104. [DOI] [PubMed] [Google Scholar]
- Saberi-Zafaghandi M. B., Hajebi A., Eskandarieh S., & Ahmadzad-Asl M. (2012). Epidemiology of suicide and attempted suicide derived from the health system database in the Islamic Republic of Iran: 2001-2007. Eastern Mediterranean Health Journal, , 836–841. [DOI] [PubMed] [Google Scholar]
- Saxena S., & Setoya Y. (2014). World Health Organization's Comprehensive Mental Health Action Plan 2013-2020. Psychiatry and Clinical Neurosciences, , 585–586. [DOI] [PubMed] [Google Scholar]
- Silverman M. M., Berman A. L., Sanddal N. D., O'Carroll P. W., & Joiner T. E. (2007). Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide and Life-Threatening Behavior, , 248–263. [DOI] [PubMed] [Google Scholar]
- Spiller H. A., Appana S., & Brock G. N. (2010). Epidemiological trends of suicide and attempted suicide by poisoning in the US: 2000−2008. Legal Medicine, , 177–183. [DOI] [PubMed] [Google Scholar]
- Statens Serum Institut (2014). Fællesindhold for basisregistrering af sygehuspatienter [Joint manual for registation of hospital patients] Retrieved from http://sundhedsdatastyrelsen.dk/da
- Ting S. A., Sullivan A. F., Boudreaux E. D., Miller I., & Camargo C. A. Jr. (2012). Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. General Hospital Psychiatry, , 557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tollefsen I., Hem E., & Ekeberg O. (2012). The reliability of suicide statistics: A systematic review. BMC Psychiatry, , 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2014). Preventing suicide: A global imperative. Geneva, Switzerland: Author. [Google Scholar]