Abstract
Medicare offers substantial protection from medical expenditure risk, protection that has increased in recent years. At age 65, out-of-pocket expenditures drop by 33 percent at the mean and 53 percent at the ninety-fifth percentile. Medical-related financial strain, such as difficulty paying bills and collections agency contact, is dramatically reduced. Nonetheless, using a stylized expected utility framework, the gain from reducing out-of-pocket expenditures accounts for only 18 percent of the social costs of financing Medicare. This calculation ignores any direct health benefits from Medicare or any indirect health effects due to reductions in financial stress.
A key goal of health insurance is to protect individuals against the risk of large unexpected medical expenditures. This function is particularly important for seniors, as nearly half of lifetime medical expenses are incurred after age 65 (Alemayehu and Warner 2004). Simulations suggest that in 2009 an age 65 household had a 5 percent chance of lifetime medical expenditures over $310,000 and an average expenditure of almost $200,000 (Webb and Zhivan 2010). Given the potentially devastating financial consequences of a health shock, it is surprising that most of the literature on health insurance focuses on its health impacts and provides a more limited understanding of the risk protection health insurance, in particular Medicare, offers against medical expenditure risk.
While several recent studies demonstrate the risk-protective role of health insurance (Baicker et al. 2013, Finkelstein et al. 2012, Gross and Notowidigdo 2011, and Mazumder and Miller 2014), these studies focus on relatively young populations and thus cannot address the potentially larger risk protective effects of health insurance at older ages. In this paper, we estimate the current impact of Medicare on medical expenditure risk and financial strain. Specifically, we compare medical expenditure risk and financial stress among the young elderly (ages 65 to 80) relative to the near elderly (ages 50 to 64). This comparison lends itself to a credible research design—a regression discontinuity (RD) exploiting age-based eligibility for Medicare. Because Medicare provides nearly universal health insurance coverage for those ages 65 and over, it creates a discontinuity in insurance coverage and generates “as good as random” assignment of coverage for individuals near the age-eligibility threshold.
Our paper contributes to a small literature on the medical expenditure risk protection afforded by Medicare. The two papers that are most similar in spirit to ours are Finkelstein and McKnight (2008)—henceforth, FM—and Englehardt and Gruber (2011), both of which use a difference-in-differences (DID) approach. FM (2008) show that within 5 years of its introduction in the 1960s, Medicare decreased out-of-pocket medical spending by 40 percent among those in the top quartile of spending.1 Englehardt and Gruber (2011) study the introduction of Part-D and find substantial reductions in out-of-pocket drug spending, concentrated among a small group of beneficiaries.2
Even though these earlier papers provide important evidence, the role of Medicare as a whole in reducing exposure to catastrophic medical spending and related financial stress today remains poorly understood. Our paper is the first to use an RD design to explore this issue. The RD design, in turn, allows us to focus on the current impact of Medicare on expenditure risk, since it does not rely on temporal variation as the DID does but instead compares the outcomes of those just eligible versus just ineligible for Medicare based on age. Using the RD, we find that the value of Medicare’s risk protection for the young elderly has increased over time.
The primary contribution of this paper is to combine a highly credible RD research design3 with high quality data to analyze the current impact of Medicare on medical expenditure risk and related financial strain. Although the age 65 RD strategy has been used to estimate the effects of Medicare on health care utilization and health outcomes (Card, Dobkin, and Maestas 2008; Card, Dobkin, and Maestas 2009), the current application is both novel and important for understanding the benefits and costs of Medicare, the second largest social insurance program in the United States. We use 15 years (1996–2010) of the Medical Expenditure Panel Survey (MEPS), a nationally representative dataset containing information on health insurance coverage, and total and out-of-pocket medical spending. Our primary interest is in the more recent period (2007–2010), which allows us to compare the contemporary costs and benefits of the Medicare program. To operationalize expenditure risk, we analyze changes in the observed distribution of out-of-pocket spending (excluding premiums since this is a cost that occurs with certainty, i.e., involves no risk). We also consider the share of the population with medical expenditures that exceed income.
To better understand the impact of Medicare on financial well-being, we use measures of financial strain related to medical expenditures. Specifically, we use three waves (2003, 2007, and 2010) of the Health Tracking Household Survey (HTHS), a nationally representative survey that captures information on medical-related financial strain such as difficulty paying medical bills, the amount owed in medical bills, and contact with a collections agency as a result of these bills.
Ultimately, the impact of Medicare on medical expenditure risk and financial strain is an empirical matter. On the one hand, by providing coverage for previously uninsured individuals, Medicare might decrease exposure to medical expenditure risk. On the other hand, the transition to Medicare might increase exposure for individuals who previously had generous employer sponsored health insurance, particularly those who lack retiree or other wrap-around coverage.4 Therefore, we interpret our findings as capturing changes due to both the increase in coverage and the transition to a new benefits package, where no specific effect sign is predicted by economic theory.5 In practice, since 90 percent of Medicare beneficiaries have very generous supplemental insurance (Kaiser Family Foundation (KFF) 2010; Baicker and Levy 2012), the increase in coverage at age 65 combined with the effective (if not the default) benefit package likely reduces exposure to medical expenditure risk.
Using the 2007–2010 MEPS data, we find that the distribution of out-of-pocket spending shifts significantly to the left at age 65. For example, out-of-pocket expenditures (all in 2010 dollars) drop by 33 percent ($326) at the mean and by 53 percent ($1,730) at the ninety-fifth percentile. The fraction of the population with out-of-pocket medical spending that exceeds income drops by 54 percent, from a base of 7.4 percent.
The declines are smaller, but still significant, if we consider the full 1996–2010 period: out-of-pocket spending at age 65 drops by almost 20 percent at both the mean ($209) and at the ninety-fifth percentile ($722). Robustness checks using data from the Health and Retirement Study (HRS) yield similar results, with 2006 marking a break in trend. Given relatively flat non-elderly cost-sharing (Gruber and Levy 2009), the rapid rise in total medical spending even since 1996 should translate into larger absolute declines in out-of-pocket spending at age 65 over time. Likewise, the large increase in enrollment in Medicare Advantage (MA), which reduces cost-sharing relative to traditional Medicare, from less than 10 percent of beneficiaries in 1996 to nearly 25 percent of beneficiaries in 2010, may contribute to this pattern (Brown et al. 2014, KFF 2014). However, the larger impact of Medicare after 2006 specifically is most consistent with Englehardt and Gruber (2011), which finds an increase in medical expenditure risk protection due to the 2006 introduction of Medicare Part-D, as well as with the recent slowdown in health care spending, which was larger in magnitude between 2007–2010 for Medicare than for private insurance (Executive Office of the President (EOP) 2014).
One potential concern in comparing out-of-pocket spending for those just under versus just over age 65 is that patterns of care could change discretely at age 65. If so, changes in out-of-pocket spending would reflect changes in the timing of care and not risk protection. For example, individuals might delay medical care and thus spending in anticipation of gaining Medicare coverage.6 To the extent such deferral exists, this should bias us against finding reductions in out-of-pocket medical spending due to Medicare. Another potential issue ignored in the literature is that the supply-side incentives for physicians might differ for patients just below relative to above age 65. Clemens and Gottlieb (2014), for example, show that private insurance fees are a multiple of Medicare fees. Consistent with their finding, we show that average total medical spending (defined as the sum of direct payments for care, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources) drops by approximately 35 percent at age 65. While lower prices should mean that, all else equal, doctors prefer privately insured to Medicare-covered patients and might ration care to Medicare beneficiaries, biasing us towards finding risk-protective effects of Medicare, we find little evidence of either a drop in care at age 65 or of deferred care until age 65. Specifically, we find that health care utilization is smooth across the age 65 threshold. In addition, “doughnut RD” estimates of changes in out-of-pocket spending, which exclude individuals right at this age threshold, are quite similar to our main results.7 Thus, either deferred and rationed care perfectly balance out or, more plausibly, these effects are too small on average (even if not for specific subgroups) to affect the main results.
Our finding that Medicare offers substantial protection against large out-of-pocket health expenses is supported by analysis of self-reported financial strain. Using HTHS data, we find that the transition to Medicare at age 65 reduces the likelihood of reporting problems paying medical bills in the past 12 months (by 35 percent) and the amount owed in medical bills (by 33 percent). The likelihood of being contacted by collections agency about medical bills declines by 28 percent and borrowing to pay these bills declines by 35 percent.
To better interpret the economic significance of our results, we perform a welfare analysis, similar to Feldstein and Gruber (1995) and FM (2008), that combines a stylized expected utility framework with the estimated changes in the distribution of out-of-pocket medical spending at age 65. We find that the out-of-pocket expenditure risk protection afforded by Medicare translates into an average welfare gain that covers 18 percent of the program’s social costs. This calculation does not include the stress benefits of reduced financial strain or any health benefits associated with transitioning to Medicare at age 65 (Dobbie and Song 2013 and Card, Dobkin, and Maestas 2009).
I. Study Data
We use pooled data from the Medical Expenditure Panel Survey (MEPS), a nationally representative two-year rotating household panel containing information on health insurance coverage, and total and out-of-pocket medical spending. While our primary focus is on the most recent, post-Part-D data, 2007–2010, we also use the full 15 years of data (1996–2010).
MEPS’s main advantage is its high quality data on health care spending. The MEPS gathers detailed information about health care visits, hospital stays, prescription drug fills, other medical services, out-of-pocket expenses, and sources of other payments (Stanton 2006). A provider component obtains follow-up data on payments by private insurance, Medicaid, Medicare, and other sources.8 Because MEPS is a household survey, it misses extreme spending by individuals in institutional settings (Aizcorbe et al. 2012, Zuvekas and Olin 2009). Since institutional spending is relatively low for those near age 65 (Federal Interagency Forum on Aging-Related Statistics 2012), this omission may not be too problematic. Out-of-pocket spending, our primary interest, is quite accurate in the MEPS, with aggregate estimates understating the National Health Expenditure Accounts (NHEA) by only about 5.5 percent (Bernard et al. 2012); in contrast, MEPS underestimates total health care spending by 17.6 percent in the same period (Bernard et al. 2012). 9 Sample sizes are relatively large—with about 7,000 to 9,000 individuals ages 50 to 80 in a survey year. Finally, in the MEPS we can calculate age in quarters and precisely estimate the age profiles of spending.
There is some dispute as to how well the MEPS captures the distribution of out-of-pocket medical spending, with Hurd and Rohwedder (2012) treating it as the gold-standard and Marshall, McGarry, and Skinner (2010) suggesting that the Health and Retirement Survey (HRS), which shows higher out-of-pocket spending in the right tail of the distribution, is more accurate. As a robustness check, we reproduce our analysis in the HRS and find effects remarkably similar to the MEPS.10 In addition to analyzing all HRS waves (1992–2010), we also focus on the most recent period (2008–2010) and exploit the long panel to investigate heterogeneity in Medicare’s impact by pre-65 insurance status.
Our measure of financial risk from the MEPS—the distribution of out-of-pocket spending—provides only limited insight into medical-related financial stress. To gain additional insight into the financial well-being afforded by Medicare, we use restricted-access data from the Health Tracking Household Survey (HTHS), formerly the Community Tracking Survey, a nationally representative survey conducted by the Center for Studying Health System Changes. We use 3 waves of the HTHS—2003, 2007 and 2010—that include information on health insurance, use of services, and medical-related financial strain, such as difficulty paying medical bills and contact with a collection agency.11 The restricted data allow us to analyze reports of the exact amount of medical bills owed (top-coded at $70,000).12 Together, these survey waves capture about 19,000 individuals ages 50–64 and 11,000 individuals ages 65–80. Unfortunately, the HTHS provides age only in years but despite this cruder measure, the visual analysis shows striking changes in financial strain at age 65.
A. insurance coverage and Generosity
We investigate the relationship between Medicare eligibility and health insurance status along two dimensions: coverage and generosity. In both surveys, coverage is measured as an indicator for whether the respondent reported having any type of health insurance at any month during the year preceding the survey. In the MEPS, we measure insurance generosity using an approach from the literature (Card, Dobkin, and Maestas 2008)—an indicator for whether the respondent reported having two or more health insurance policies in the year preceding the survey.13 This measure, which says little about generosity prior to age 65, captures reported supplemental insurance coverage, which many consider overly generous since it not only provides additional benefits but often fully covers the high cost-sharing and deductibles in traditional Medicare (Baicker and Levy 2012). The HTHS data ask explicitly about supplemental coverage, therefore we can better assess the extent to which individuals transition to a generous source of coverage at age 65.
B. Medical Expenditure Risk Measures
We use the empirical distribution of out-of-pocket spending in the MEPS to characterize medical expenditure risk. Although risk is fundamentally an ex ante concept, the distribution of expenditure realizations is one way for an individual to understand the likelihood of facing extreme out-of-pocket costs. We measure changes in the distribution of out-of-pocket spending at age 65, including the mean, different percentiles, and the share of total expenditures paid out-of-pocket. We also consider the share of the population with out-of-pocket expenses that exceed income, an unexplored measure of financial strain.14 The MEPS defines medical expenditures as the sum of direct payments for care, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources. Payments for health insurance premiums and over-the-counter drugs are not included. All medical expenditures are adjusted for inflation using the medical care services (MCS) component of the Consumer Price Index (CPI) and expressed in 2010 dollars.15 Results using the full CPI are very similar. All age-specific means are calculated taking into account survey design.
C. Financial Strain Measures
We use the HTHS to get at subjective measures of financial strain. All 3 waves of the HTHS ask respondents whether in the past 12 months they: (i) had any problems paying medical bills, (ii) were contacted by a collections agency, (iii) had to borrow because of problems paying medical bills or (iv) had to take money out of savings because of these problems. In the last 2 survey waves, they ask respondents about the amount owed in medical bills, the event that caused medical bill problems (e.g., an illness, accident, medical test, or surgical procedure) and whether the respondent filed or thought about filing for bankruptcy in the past 12 months. In general, the rate of bankruptcy filing or thoughts of filing are too low to provide meaningful information. Therefore we focus on items (i)–(iv) and on changes in the amount owed in medical bills.
II. Empirical Strategy: Regression Discontinuity Design
To understand the impact of health insurance on medical expenditure risk, we would, in principle, estimate the following reduced-form equation:
| (1) |
where mi is a measure of medical-related financial exposure (e.g., out-of-pocket spending or difficulty paying medical bills) for individual i; f(agei; λ) is a smooth function representing the age profile of outcome mi, where λ is the vector of polynomial parameters; Ii is an indicator for whether individual i has health insurance coverage; Xi is a vector of demographics characteristics of individual i; and εi is an unobserved error. A fundamental and well-known problem in interpreting β as the causal effect of health insurance on medical expenditure risk is that coverage is endogenous; it both affects and is affected by financial risk, confounding observational comparisons of people by insurance status.
To circumvent this problem, we exploit the age 65 threshold for Medicare eligibility as a credible source of exogenous variation in insurance status. We adopt an RD design, taking advantage of the fact that individuals just above or below age 65 (e.g., 64 or 66) should be similar on observable and unobservable characteristics that affect medical expenditure risk—that is, these characteristics should have smooth age profiles. This strategy assumes that in the absence of Medicare our outcomes of interest should not change discontinuously at 65; therefore any estimated discontinuities are attributed to Medicare. This age 65 Medicare RD offers a well-established research design, albeit one that has been used largely to understand the impact of Medicare on health care use, diagnoses, mortality, and job lock (e.g., see Card, Dobkin, and Maestas 2008; Card, Dobkin, and Maestas 2009; Fairlie, Kapur, and Gates 2010; and Kadiyala and Strumpf 2012). As discussed above, because those who had health insurance prior to transitioning on to Medicare experience some change in their benefits package, the analysis will capture a weighted average effect due to the increase in insurance coverage and the change in benefits package at age 65.
Formally, health insurance coverage can be summarized by:
| (2) |
where coverage depends on individual characteristics, a smooth function of age and an indicator Ti for age 65 or older, due to Medicare eligibility. Combining equations (2) and (1), the resulting reduced-form model for outcome mi is
| (3) |
where ω = α + βγ; h (agei; ρ) = f(∙) + βg(∙) and τ = βπ.16 Assuming the age profiles f(∙) and g(∙) are both continuous at age 65, discontinuities in mi at that age can be attributed to discontinuities in insurance. In other words, if we assume that the age profiles of financial risk are continuous at age 65 in the absence of Medicare’s age-based eligibility rule, then, once we empirically control for such profiles, any estimated discontinuity in our risk measures can be attributed to discontinuities in Medicare coverage. Using the MEPS and the HTHS, we show below that insurance coverage rises discontinuously at age 65. The discontinuity in coverage at age 65 enables us to estimate the reduced form effect of Medicare on financial risk protection. The magnitude of this effect τ depends on the size of the insurance changes at age 65, π, and the causal effect of insurance on mi, β.17
Equation (3) is our main estimating equation. We allow the age profiles, h(agei; ρ), to vary on either side of the age 65 cutoff. For analyses of insurance coverage, mean out-of-pocket spending, the share of total spending paid out-of-pocket, and reports and sources of medical bill problems, we use Ordinary Least Squares (OLS) regressions. To account for potential misspecification of the age-profiles, we adjust our standard errors to allow for an arbitrary correlation at the level of age in quarters in the MEPS or age in years in the HTHS (Lee and Card 2008). Analyses of different points in the distribution of out-of-pocket spending—e.g., spending at the median, seventy-fifth and ninety-fifth percentile—are estimated using quantile regressions. Standard errors for quantile models are estimated using an age-based block bootstrap, analogous to age-based clustering, that randomly samples with replacement the data within each age group and estimates the models on these random samples (Efron and Tibshirani 1994). When an age-block is randomly selected all respondents of this age are included in the estimation. The standard errors are then calculated simply as the standard deviation of the coefficient estimates from 500 bootstrap samples.
All regressions (OLS and quantile) employ survey weighting. In order to increase precision, we pool together several years of data. Importantly, the MEPS samples in most years are not completely independent because households are drawn from the same sample geographic areas and many people are in the sample for two consecutive years.18 Despite this lack of independence, it is valid to pool multiple years of MEPS data and keep all observations in the analysis because each year of the MEPS is designed to be nationally representative.19
A. Other Changes at Age 65
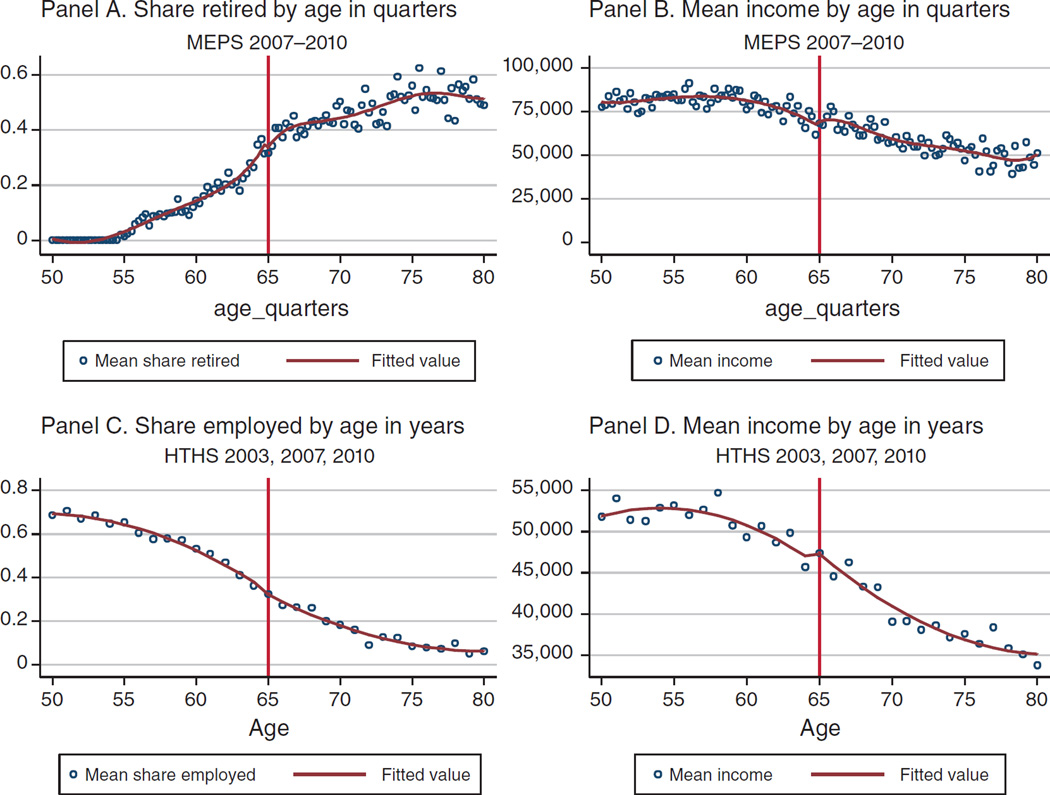
A key assumption of the RD is that observable and unobservable characteristics that affect outcomes have a smooth age profile at the arbitrary threshold used for identification (age 65 for Medicare). An obvious concern in our context is employment, since 65 is a traditional age of retirement. Card, Dobkin, and Maestas (2008) demonstrate that the estimated jumps in employment-related outcomes at age 65 are small in magnitude and statistically insignificant in both the NHIS and the March CPS. In the MEPS and HTHS, we find similar smoothness in employment and retirement rates,20 educational attainment, family income, and geographic location (Figure 1 and Table 1).
Figure 1.
Smoothness of Covariates: MEPS 2007–2010 and HTHS 2003, 2007, 2010
Table 1.
Smoothness of Covariates
| Share employed |
Share retired |
Share married |
Income | Family size |
Share male |
Share with less than HS degree |
Share Hispanic |
|
|---|---|---|---|---|---|---|---|---|
| Panel A. MEPS 2007–2010 | ||||||||
| Age 65+ | 0.01 (0.039) |
−0.036 (0.032) |
0.052*** (0.020) |
2,287 (4,017) |
0.023 (0.057) |
0.005 (0.036) |
0.001 (0.023) |
0.006 (0.011) |
| Mean pre-65 | 0.69 | 0.087 | 0.665 | 44,154 | 2.42 | 0.490 | 0.153 | 0.092 |
| F-statistic | 1.25 | 1.51 | 1.45 | 1.31 | 1.53 | 1.76 | 1.10 | 0.75 |
| Observations | 32,569 | 32,241 | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 |
| Panel B. HTHS 2003, 2007, 2010 | ||||||||
| Age 65+ | −0.014 (0.015) |
0.043** (0.017) |
1,163 (1,381) |
0.045* (0.026) |
−0.09*** (0.011) |
−0.036*** (0.016) |
−0.021 (0.02) |
|
| Mean pre-65 | 0.588 | 0.692 | 51,419 | 2.07 | 0.486 | 0.128 | 0.087 | |
| F-statistic | 1.48 | 3.9 | 1.12 | 2.31 | 1.23 | 3.46 | 4.51 | |
| Observations | 30,172 | 30,172 | 30,172 | 30,172 | 30,172 | 30,172 | 30,172 | |
Notes: Both panels include respondents aged 50 to 80 years. All regressions include a constant, an indicator for ages 65 and above. Regressions in panel A include a fifth-order polynomial; panel B uses a fourth-order polynomial rather than a fifth-order polynomial because of the sparser data, the availability of age in years only, and what appeared to be better parametric fits. Standard errors are clustered at the level of age in quarters in the MEPS and by age in years in the HTHS.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data in panel A are from the 2007–2010 Medical Expenditure Panel Surveys. Panel B data are from the 2003, 2007, and 2010 Health Tracking Household Survey.
Across most outcomes, including the share male, Hispanic, or with less than a high school degree (see Table 1), we cannot reject zero discontinuity at age 65. An important exception in both the 2007–2010 MEPS and the HTHS is the share married, where we find a discontinuous increase at age 65. Using the 2007–2010 March CPS, we do not find a similar discontinuity in marriage at age 65 (available upon request). Across all 11 outcomes in the 2007–2010 MEPS, the change in marriage is the only outcome that is significantly different from zero. In the HTHS, we find a discontinuity in the share married, the share male, and the share with less than a high school degree. As reflected by the F-statistic, however, the parametric fit model is poor: the coarseness of the data, which capture age in years instead of quarters, limits the fit. If we use the full 1996–2010 MEPS sample in order to maximize the power to detect discontinuities, we cannot reject the hypothesis of no discontinuity for any covariate, including the share married (see online Appendix Figure 1 and online Appendix Table 1). Given the general smoothness in the data, our analysis satisfies the continuity assumption of the RD design. And, as discussed below, controlling for marital status, and in the HTHS, gender and education, has little effect on our estimates. Thus, we attribute discrete changes in our measures of risk at age 65 to the change in Medicare eligibility at this age.
B. Sensitivity Checks
We test the sensitivity of our main estimates in several ways. First, we experiment with alternate specifications of the control function, i.e., the age polynomials. While our main specification uses a quadratic in age, which seems to mimic the plots of our outcomes quite well, specifications that employ linear or cubic age terms yield similar results. Second, we show that narrowing the age window to respondents 55 to 75 years old, and thereby limiting the contribution of observations far from the age-65 Medicare threshold, generates similar findings.
One concern in comparing the distribution of health spending above and below age 65 is that individuals may defer some health spending until they are eligible for Medicare.21 Alternatively, physicians may prefer the higher fees paid by private insurance and ration care to Medicare beneficiaries.22 Although some prior work finds that hospitalizations increase as individuals gain Medicare coverage (Card, Dobkin, and Maestas 2008), the absolute increase is small. We find little evidence of changes in care at age 65 in our MEPS sample as a whole or in the Health and Retirement Survey (HRS). Since we may be underpowered to detect changes in utilization, however, we perform “doughnut-RD” estimates that drop observations right around age 65. While we see no evidence of heaping, the typical rationale for the “doughnut-RD” (Barreca, Lindo, and Waddell 2011), this approach helps deal with deferral or rationing, since those around age 65 are most likely to defer care in anticipation of Medicare coverage or face substitution by doctors for privately insured patients. The doughnut estimates are quite similar to our main results.23
III. Results
A. Medicare Eligibility and Health Insurance Coverage and Generosity
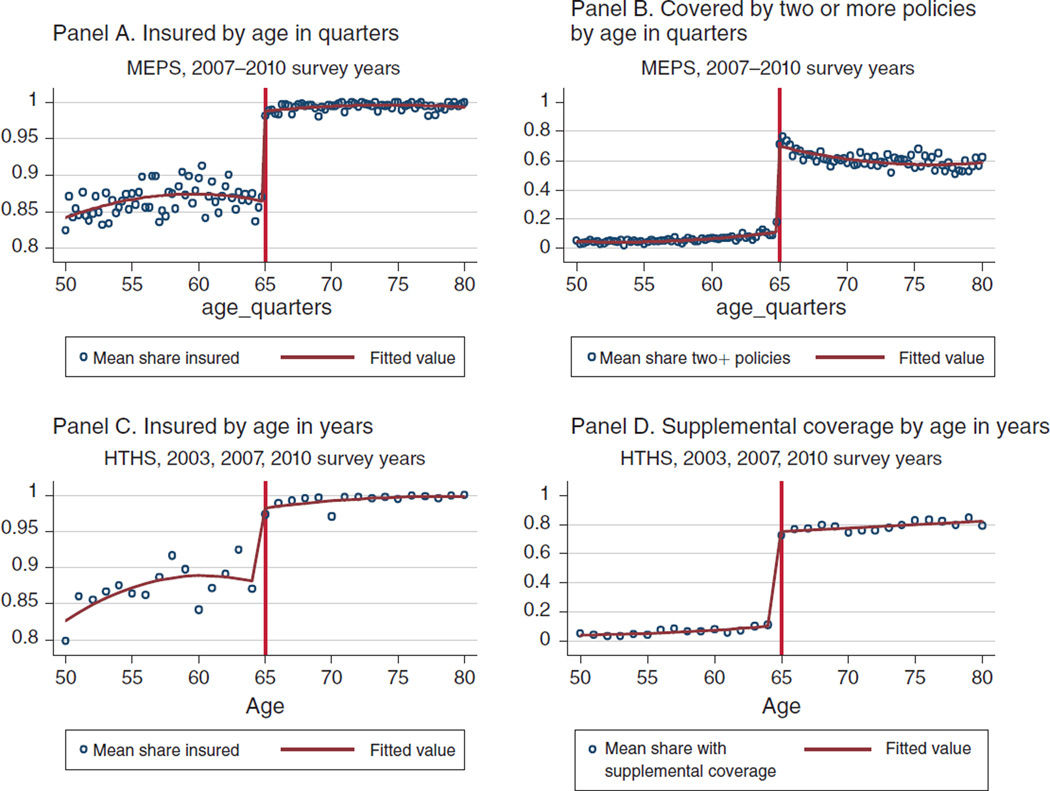
Figure 2 shows the age profile of health insurance coverage and generosity for the MEPS and the HTHS samples. It shows smooth functions fitted to the data before and after age 65. The figure demonstrates that health insurance coverage rises discontinuously at age 65, from 87 percent to 99 percent in the MEPS; the probability of having 2 or more policies also “jump” (see Table 2). There are similar increases in the HTHS. In the MEPS sample, the fraction covered by 2 or more plans increases by about 59 percentage points off a base of only 6 percent. In the HTHS, where we have a direct measure of supplemental coverage, the increase is 64 percentage points off a base of just 6.3 percent. Medicare Advantage and supplemental coverage (not shown) increase at age 65 by 67 percentage points off a base of 6.6 percent.24 While below the 90 percent supplemental coverage in the Medicare Current Beneficiary Survey (KFF 2010), these figures indicate that most individuals transition to a generous health benefits package at age 65 (see online Appendix Figure 2 for a visual display of the distribution of insurance types for those just under and just over age 65. This figure demonstrates the decrease in uninsurance and increase in multiple sources of coverage at age 65).25 As shown in Table 2, the increases are statistically different from zero and stable across alternative specifications of the age polynomial. We use this discontinuous change in coverage and generosity at age 65 to identify the effect of Medicare on medical expenditure risk and financial strain.26
Figure 2.
Change in Health Insurance Coverage and Generosity at Age 65, MEPS and HTHS
Table 2.
Impact of Medicare on Health Insurance Coverage and Generosity
| Quadratic in age |
Linear in age |
Cubic in age |
||||
|---|---|---|---|---|---|---|
| Insured | Covered by 2+ policies |
Insured | Covered by 2+ policies |
Insured | Covered by 2+ policies |
|
| Panel A. MEPS 2007–2010 | ||||||
| Age 65+ | 0.124*** (0.006) |
0.586*** (0.019) |
0.112*** (0.005) |
0.576*** (0.014) |
0.130*** (0.008) |
0.599*** (0.024) |
| Mean pre-65 | 0.865 | 0.059 | 0.865 | 0.059 | 0.865 | 0.059 |
| Relative effect (percent) | 14.34 | 993.22 | 12.95 | 976.27 | 15.03 | 1,015.25 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 |
| Panel B. HTHS 2003, 2007, 2010 | ||||||
| Age 65+ | 0.106*** (0.022) |
0.639*** (0.178) |
0.080*** (0.016) |
0.650*** (0.013) |
0.074** (0.037) |
0.642*** (0.024) |
| Mean pre-65 | 0.869 | 0.063 | 0.869 | 0.063 | 0.869 | 0.063 |
| Relative effect (percent) | 12.20 | 1,014.29 | 9.21 | 1,031.75 | 8.52 | 1,019.05 |
| Observations | 30,172 | 30,172 | 30,172 | 30,172 | 30,172 | 30,172 |
Notes: Both panels include respondents aged 50 to 80. All regressions include a constant, an indicator for ages 65 and above, and a polynomial in age in quarters in the MEPS and in years in the HTHS that is allowed to vary on either side of age 65. The first three columns show the main specification using a quadratic in age. The next three columns use linear age trends and the last three cubic age terms. Standard errors are clustered by age in quarters for the MEPS samples and age in years in the HTHS.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data in panel A are from the 2007–2010 MEPS and in panel B are from the 2003, 2007, and 2010 HTHS.
B. Total Spending and Utilization
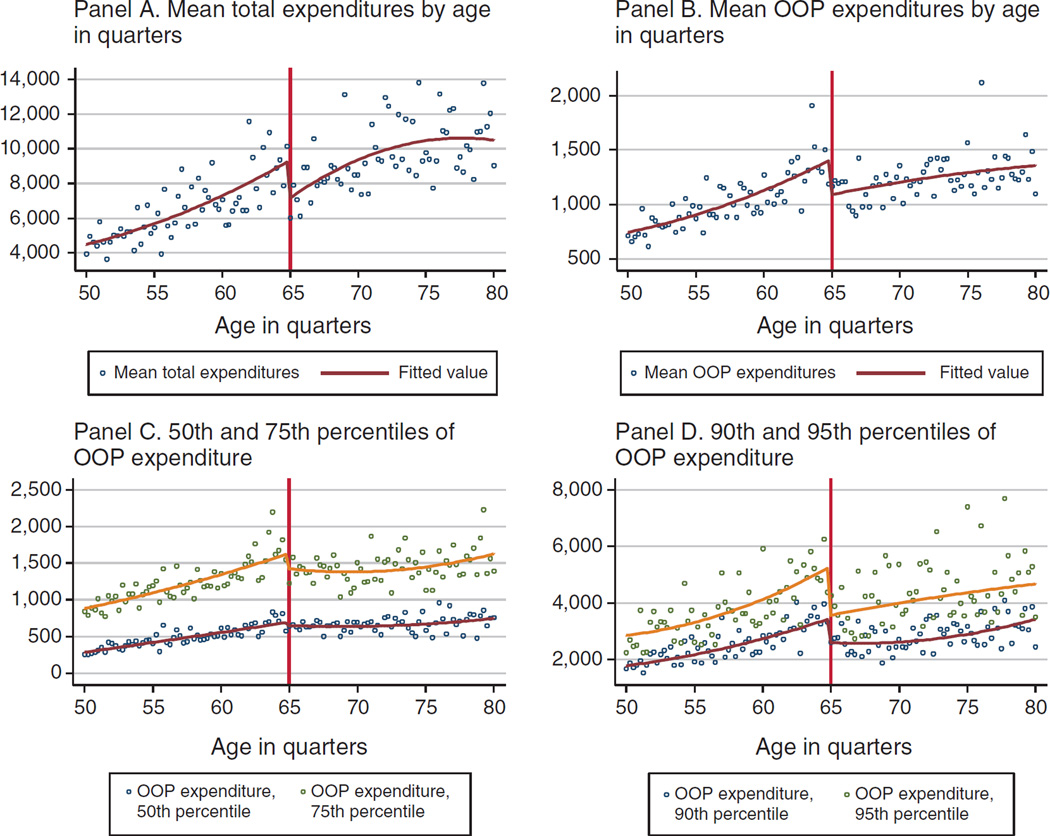
Here we consider the change in average total spending and utilization at age 65. As shown in Figure 3 and Table 3, average total medical spending actually declines at age 65 by about $2,200; a 35 percent decline relative to the average spending of people aged 50–64. Since spending is increasing sharply with age, one might want to use the mean for those closer to age 65. Doing so still implies a larger, nearly 25 percent decline in spending at age 65. We find similar estimates if we use different age polynomials (Table 3, panels B and C), narrower age bands, or doughnut RDs (online Appendix Table 2). The 1996–2010 sample results imply a smaller but still significant decline in spending of $850 or 14 percent (online Appendix Table 3).
Figure 3.
Change in Total and Out-of-Pocket (OOP) Spending: MEPS 2007–2010
Source: MEPS, 2007–2010 survey years
Table 3.
Impact of Medicare on Total Spending and Utilization: MEPS 2007–2010
| Total spending |
Any physician visits |
Any outpatient hospital visits |
Any inpatient visits |
|
|---|---|---|---|---|
| Panel A. Quadratic in age, MEPS 2007–2010 | ||||
| Age 65+ | −2,168** (672) |
0.009 (0.011) |
−0.012 (0.013) |
−0.003 (0.014) |
| Mean pre-65 | 6,376 | 0.805 | 0.228 | 0.081 |
| Relative effect (percent) | −34.01 | 1.12 | −5.26 | −3.70 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 |
| Panel B. Linear trend in age, MEPS 2007–2010 | ||||
| Age 65+ | −1,128** (498) |
0.011 (0.008) |
0.003 (0.011) |
0.013 (0.01) |
| Mean pre-65 | 6,376 | 0.805 | 0.228 | 0.081 |
| Relative effect (percent) | −17.70 | 1.42 | 1.47 | 16.12 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 |
| Panel C. Third-order polynomial, MEPS 2007–2010 | ||||
| Age 65+ | −2,629** (785) |
0.007 (0.013) |
−0.022 (0.017) |
−0.009 (0.017) |
| Mean pre-65 | 6,376 | 0.805 | 0.228 | 0.081 |
| Relative effect (percent) | −41.24 | 0.87 | −9.65 | −11.11 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 |
Notes: All regressions include a constant and an indicator for ages 65 and above and a polynomial in age that is allowed to vary on either side of age 65. Panel A uses a quadratic in age, while panel B uses a linear trend, and panel C uses a cubic in age in quarters. Standard errors are clustered by age in quarters.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data are from the 2007–2010 Medical Expenditure Panel Survey and include respondents ages 50 to 80.
This large and significant drop in average total spending at age 65 runs contrary to the idea of demand-driven deferability of care with constant (pre-insurance) prices. It could, however, result from Medicare’s significant market power and thus ability to pay lower prices (Clemens and Gottlieb 2014). Although a change in prices at age 65 introduces perverse supply-side incentives—all else equal, doctors should prefer privately insured to Medicare-covered patients and might ration care to Medicare beneficiaries—we show below that health care utilization is smooth across the age 65 threshold. Thus, either deferred care and rationed care balance out or, more plausibly, these effects are too small on average to affect the main results. Since we find no significant change in quantities, we suspect that the drop in average total spending is driven by changes in prices at age 65, a hypothesis that deserves further study.
Online Appendix Figure 3 and Table 3 show that the likelihood of a physician visit, an outpatient hospital visit, or an inpatient stay is essentially unchanged at age 65. This is true across alternate specifications of the age polynomials (Table 3, panels B and C) and when we narrow the age window to 55 to 75 or perform donut RD estimates (online Appendix Table 2, panels A–D). Likewise, we find no evidence to support a change in utilization at age 65 in the full 1996–2010 MEPS (online Appendix Table 3 and online Appendix Figure 4). These conclusions are unchanged if we analyze total visits or the log (or inverse hyperbolic sine) of visits (not shown for brevity). A key implication is that deferability (or rationing) may not be a big issue in the sample over-all—a fact consistent with Card, Dobkin, and Maestas’ (2008) findings for outpatient care, where changes in the likelihood of a doctor’s visit at age 65 are on the order of 1 percentage point or 1.5 percent relative to the pre-65 mean.27
Online Appendix Table 4, which documents utilization changes at age 65 in more detail, shows that our findings are not anomalous. Panel A shows the NHIS results from Card, Dobkin, and Maestas (2008) while the other panels show our results from the MEPS and the HRS for different time periods and age groups. Relative to the mean, the Card, Dobkin, and Maestas (2008) results are small overall but large for some racial/ethnic subgroups. Our MEPS and HRS results show a similar pattern. When restricted to the same time period and ages as Card, Dobkin, and Maestas (2008), we find larger and more precise effects. For this subsample the increase in doctor visits is statistically significant for all groups except non-Hispanic blacks (online Appendix Table 4, panel C). Unlike Card, Dobkin, and Maestas (2008), we find no evidence of an increase in hospitalizations at age 65 in the MEPS or the HRS, however we generally cannot rule out their effects either.
Since we may be underpowered to detect changes in the timing of care and, perhaps more importantly, Card, Dobkin, and Maestas (2008) find a 10 percent increase in hospitalizations that we do not find here, we conclude that to the extent such behavior exists it will cause us to underestimate the risk protective benefit of Medicare. Moreover, in Section IV, we show that the moral hazard costs implied by the Card, Dobkin, and Maestas (2008) estimates are small relative to the risk protection benefits of Medicare.
C. Medicare Eligibility and Medical Expenditure Risk
Next, we analyze changes in the distribution of out-of-pocket medical spending at age 65. Figure 3 presents the RD graphs for different parts of the distribution of spending and Table 4 the corresponding RD estimates. We find a discontinuous drop of $326 in the mean of out-of-pocket spending, a drop of almost 33 percent relative to the mean prior to age 65. The sharp drop in out-of-pocket spending at age 65 increases as we move to higher percentiles of the distribution. At the median, the decline is small—roughly $47. At the seventy-fifth percentile the decline is about $210 or almost 18 percent relative to the pre-65 mean, while at the ninetieth and ninety-fifth percentiles the declines are $865 (36 percent) and $1,730 (52 percent), respectively. Together with online Appendix Figure 5, which shows all the RD percentile estimates, these estimates imply that the effects of Medicare on out-of-pocket costs are concentrated at the top quartile of the spending distribution. As one might expect, Medicare offers risk protection through declines in high, catastrophic medical spending.
Table 4.
Impact of Medicare on Out-of-Pocket Spending in the MEPS: 2007–2010
| Mean | Median | 75th percentile |
90th percentile |
95th percentile |
Share out-of-pocket |
Share out-of-pocket costs that exceed income |
|
|---|---|---|---|---|---|---|---|
| Panel A. Quadratic in age, MEPS 2007–2010 | |||||||
| Age 65+ | −326** (98) |
−47 (42) |
−210** (102) |
−865*** (166) |
−1,730*** (398) |
−0.02 (0.015) |
−0.040*** (0.009) |
| Mean pre-65 | 1,003 | 464 | 1,188 | 2,403 | 3,724 | 0.327 | 0.074 |
| Relative effect (percent) | −32.55 | −10.07 | −17.64 | −36.00 | −52.84 | −6.12 | −53.86 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 | 29,378 | 32,569 |
| Panel B. Linear trend in age, MEPS 2007–2010 | |||||||
| Age 65+ | −255*** (61) |
−66** (27) |
−242*** (65) |
−843*** (108) |
−1,391*** (266) |
−0.037*** (0.011) |
−0.032*** (0.006) |
| Mean pre-65 | 1,003 | 464 | 1,188 | 2,403 | 3,724 | 0.327 | 0.074 |
| Relative effect (percent) | 25.44 | −14.37 | −20.40 | −35.10 | −37.35 | −11.31 | −43.94 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 | 29,378 | 32,569 |
| Panel C. Third-order polynomial in age, MEPS 2007–2010 | |||||||
| Age 65+ | −348** (125) |
−141** (56) |
−352*** (125) |
−1,145*** (240) |
−2,090*** (470) |
−0.019 (0.02) |
−0.031*** (0.011) |
| Mean pre-65 | 1,003 | 464 | 1,188 | 2,403 | 3,724 | 0.327 | 0.074 |
| Relative effect (percent) | −34.75 | −30.44 | −29.64 | −47.65 | −63.88 | −5.81 | −41.41 |
| Observations | 32,569 | 32,569 | 32,569 | 32,569 | 32,569 | 29,378 | 32,569 |
Notes: All regressions include a constant, an indicator for ages 65 and above, and a polynomial in age in quarters that is allowed to vary on either side of age 65. Panel A uses a quadratic in age, while panel B uses a linear trend, and panel C uses a cubic in age in quarters. Standard errors for OLS regressions (mean out-of-pocket spending and share out of pocket) are clustered by age in quarters. Standard errors for quantile regressions are based on a block bootstrap with 500 draws, where the block is age in quarters.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data are from the 2007–2010 Medical Expenditure Panel Survey and include respondents aged 50 to 80.
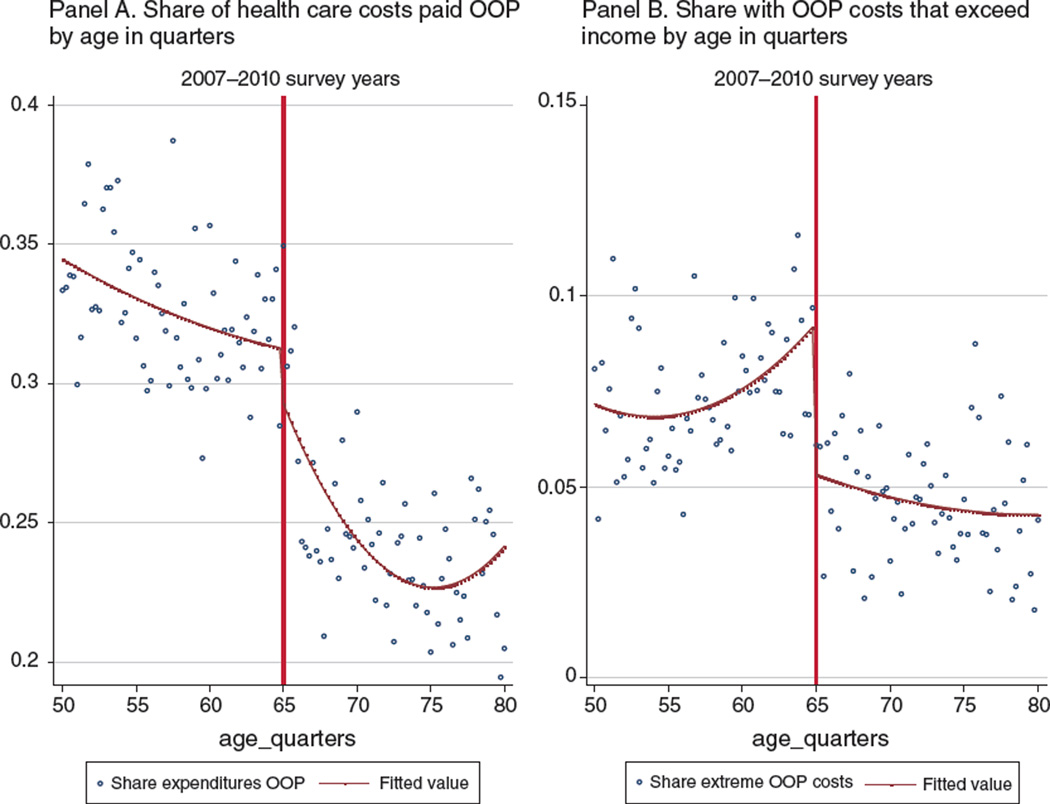
Table 4 and Figure 4 also show changes in the share of total expenditures paid out-of-pocket and the share of the population with out-of-pocket spending that exceeds income. The share of spending paid out-of-pocket drops by approximately 2 percentage points or about 6 percent off the mean share of 33 percent below age 65, although this estimate is not statistically distinguishable from zero (Table 4). The share of the population with out-of-pocket expenditures that exceed income, a proxy for “catastrophic” out-of-pocket medical costs, drops precipitously—by more than 50 percent, from a pre-65 mean of 7.4 percent to 3.4 percent (Table 4 and Figure 4). This drop cannot be explained by changes in income, as income is smooth across the age 65 threshold (Figure 1).
Figure 4.
Impact of Medicare on Relative Out-of-Pocket (OOP) Health Care Costs: MEPS 2007–2010
Estimates using linear or cubic age trends (panels B and C of Table 4) tend to straddle those from our preferred specification with quadratic age trends. With linear age trends, the declines in out-of-pocket spending are $255 (25 percent) at the mean and $843 (35 percent) and $1,391 (37 percent) at the ninetieth and ninety-fifth percentiles, respectively. The decline in the share of spending paid out-of-pocket is statistically significant and almost 4 percentage points or 11 percent. Using cubic age trends, the declines in out-of-pocket spending are $348 (35 percent) at the mean and $1,145 (48 percent) and $2,091 (64 percent) at the ninetieth and ninety-fifth percentiles, respectively. Further analysis of the share of spending paid out of pocket reveals that the mean decline is driven by changes in the right tail of the distribution (see online Appendix Table 5). At age 65, the share with out-of-pocket spending that exceeds income declines by about 3 percentage points (or 40 percent) in both specifications. Results in online Appendix Table 6, which control for marital status, are virtually identical as are those in online Appendix Table 7, which use narrower age bands (panel A) or doughnut RDs (panels B–D). Online Appendix Figure 6 shows that the estimates are robust to the choice of the age bandwidth.
Estimates from the 1996–2010 MEPS (online Appendix Table 8 and online Appendix Figure 7) are considerably smaller in magnitude: relative to 2007–2010, the estimated decline in out-of-pocket spending is about two-thirds of the decline at the mean and 55 percent of the decline at the ninetieth percentile. The smaller effects prior to 2007 are consistent with Englehardt and Gruber (2011), which find that the 2006 introduction of Medicare Part-D reduced medical expenditure risk. Separately analyzing categories of spending and time periods, we find that about 41 percent ($69 of $169) of the larger decline in out-of-pocket spending in 2007–2010 relative to 1996–2006 is attributable to prescription drugs (available upon request). The decline in health care spending growth since 2007, which has been larger for Medicare than for private insurance, may contribute to this pattern as well (EOP 2014).28
D. Medicare Eligibility and Financial Strain
While the observed changes in out-of-pocket spending at age 65, particularly those at the right tail of the distribution, indicate that Medicare offers important risk-protection to seniors, the precise numbers are difficult to put into context. To provide further meaning to these changes, we use the HTHS to measure changes in self-reported financial strain.
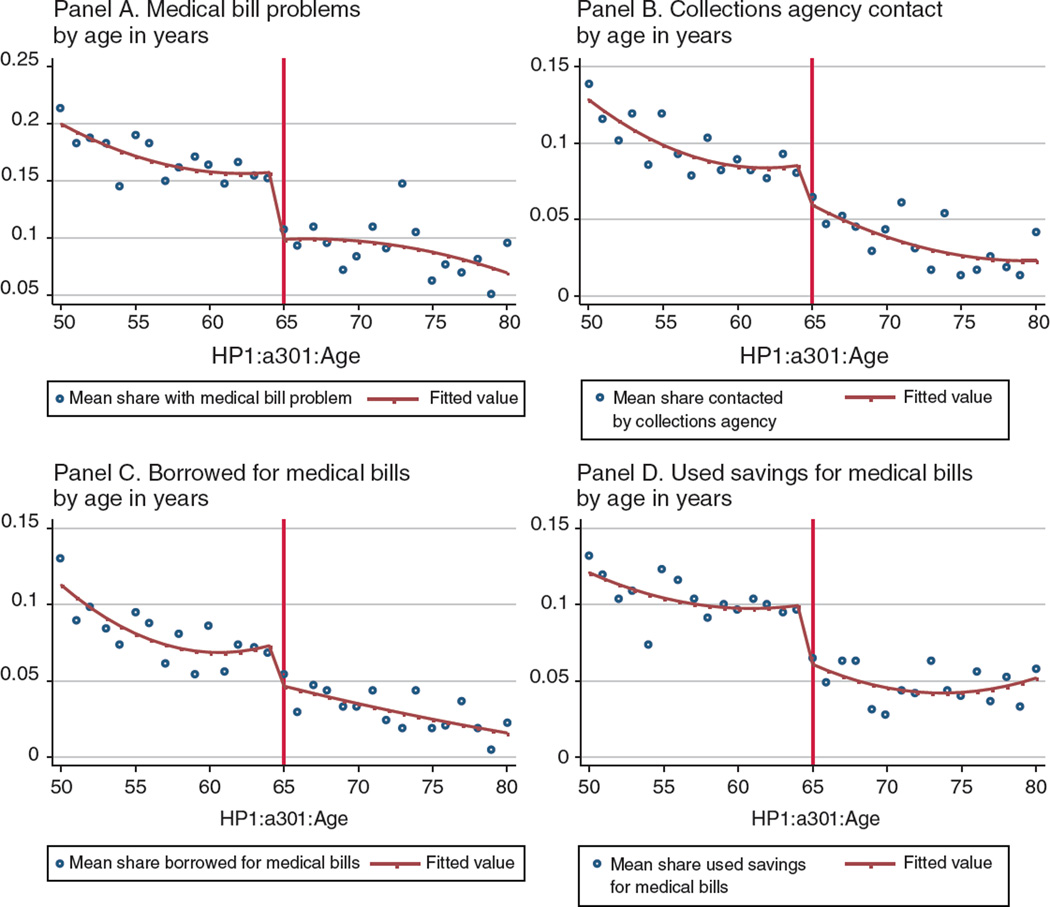
Figure 5 and the corresponding estimates in Table 5 show discontinuous changes at age 65 in reported problems paying medical bills, medical-bill related collections agency contact, borrowing to pay these bills, and using savings to pay these bills. Prior to age 65, 17 percent of respondents report problems paying medical bills. At age 65, the fraction reporting problems declines by 6 percentage points or 35 percent. Estimates using linear or cubic age terms (in Table 5, panels B and C) suggest smaller, although still sizeable, declines in medical bill problems. Estimates controlling for marital status, gender, and education in online Appendix Table 9 are quite similar. Estimates using only respondents ages 55 to 75 or from the doughnut RDs in online Appendix Table 10 are roughly the same as the main estimates or ever larger.
Figure 5.
Impact of Medicare on Medical Bill Problems and Collections Activity, HTHS: 2003, 2007, 2010
Table 5.
Impact of Medicare on Medical Bill Problems in the Past 12 Months: HTHS 2003, 2007, 2010
| Medical bill problems |
Collection agency contact |
Borrowed to pay medical bills |
Savings to pay medical bills |
Delayed major pur- chase due to medical bills |
Amount owed |
90th percentile of amount owed |
IHS amount owed |
|
|---|---|---|---|---|---|---|---|---|
| Panel A. Quadratic in age | ||||||||
| Age 65+ | −0.060*** (0.012) |
−0.028*** (0.009) |
−0.029*** (0.010) |
−0.040*** (0.009) |
−0.044*** (0.011) |
−117.96 (198) |
−305.88 (356) |
−0.330*** (0.070) |
| Mean pre-65 | 0.171 | 0.099 | 0.082 | 0.105 | 0.092 | 936 | 1,000 | 936.05 |
| Relative effect | −35.09 | −28.28 | −35.37 | −38.10 | −47.83 | −12.60 | −30.59 | 33 |
| Observations | 30,088 | 30,079 | 30,088 | 30,065 | 30,067 | 14,072 | 14,072 | 14,072 |
| Panel B. Linear trend in age | ||||||||
| Age 65+ | −0.041*** (0.008) |
−0.017** (0.007) |
−0.011 (0.008) |
−0.038*** (0.007) |
−0.028*** (0.009) |
−51.52 (153) |
−111.35 (210) |
−0.230*** (0.054) |
| Mean pre-65 | 0.171 | 0.099 | 0.082 | 0.105 | 0.092 | 936 | 1,000 | 936.05 |
| Relative effect | −23.98 | −17.17 | −13.41 | −36.19 | −30.43 | −5.50 | −11.14 | 23 |
| Observations | 30,088 | 30,079 | 30,080 | 30,065 | 30,067 | 14,072 | 14,072 | 14,072 |
| Panel C. cubic in age | ||||||||
| Age 65+ |
−0.042*** (0.010) |
−0.022* (0.011) |
−0.017 (0.012) |
−0.022** (0.010) |
−0.032** (0.013) |
−333.6 (214) |
65.15 (460) |
−0.334*** (0.095) |
| Mean pre-65 | 0.171 | 0.099 | 0.082 | 0.105 | 0.092 | 936 | 1,000 | 936.05 |
| Relative effect | −24.56 | −22.22 | −20.73 | −20.95 | −34.78 | −35.64 | 6.52 | 33 |
| Observations | 30,088 | 30,079 | 30,080 | 30,065 | 30,067 | 14,072 | 14,072 | 14,072 |
Notes: Questions about amounts owed were only asked in 2007 and 2010. All regressions include a constant, an indicator for ages 65 and above, and a polynomial in age in years that is allowed to vary on either side of age 65. Panel A uses a quadratic in age, while panel B uses a linear trend, and panel C uses a cubic in age in quarters. Standard errors are clustered by age in years.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data are from the 2003, 2007, and 2010 waves of the Health Tracking Household Survey and are restricted to respondents aged 50 to 80.
Consistent with the decline in perceived problems paying medical bills, the fraction contacted by collection agencies about these bills declines by 2.8 percentage points or about 30 percent off a base of 9.9 percent. The declines are a bit smaller (17–22 percent) using alternative polynomials, while the narrower age band and doughnut RDs yield larger declines (32–36 percent). The fraction borrowing to pay these bills declines by 2.9 percentage points (35 percent off a base of 8.2 percent; significant at the 10 percent level). The fraction using savings to pay medical bills declines by 4 percentage points (38 percent off a mean of 10.5 percent; significant at the 1 percent level). Using the more restricted age group or the doughnut RDs, the estimated declines in borrowing or using savings are similar and in many cases a bit larger.
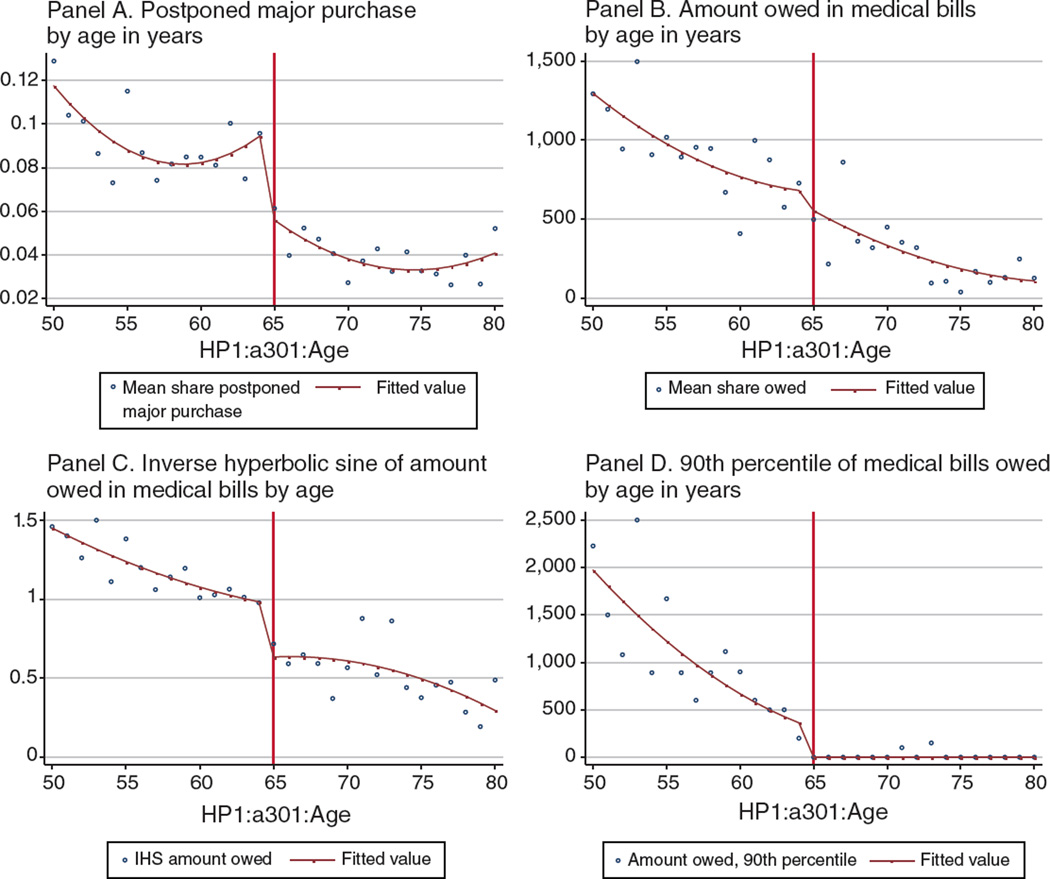
Interpreting declines in the likelihood of borrowing or using savings to pay medical bills is somewhat difficult. The implications of borrowing to smooth consumption may be quite different from borrowing that depletes a retirement nest egg. Since we find large declines in the likelihood of delaying major purchases as a result of medical bills at age 65 (4 percentage points off a base of just 9 percent prior to age 65; see column 5, Table 5 and panel A of Figure 6), these changes in borrowing and savings do not seem to reflect consumption smoothing. However, more detail is needed to fully understand these patterns.
Figure 6.
Impact of Medicare on the Amount Owed in Medical Bills HTHS: 2003, 2007, 2010
Finally, we analyze changes in the amount owed in medical bills (see Figure 6 and the last 3 columns of Table 5). Medical debt is a stock but the rate at which individuals acquire debt or at which existing debt grows may change at age 65. In addition, individuals may be more likely to report newly acquired debt rather than their current stock of debt.29 We find a statistically insignificant change of about $120 off a base of $936 owed in medical bills prior to age 65. At the ninetieth percentile, the change is more than 2.5 times larger or $306, although it is also quite imprecise. To deal with skew, we analyze the inverse hyperbolic sine, , of the amount owed. This transformation is defined at zero and like the natural log yields a parameter that can be interpreted as an elasticity (Pence 2006). With this specification, we estimate a 33 percent decline in the amount owed at age 65, further evidence that Medicare has a meaningful impact on medical liabilities. Using a cubic in age yields an almost identical decline (33 percent) while linear age trends yield a smaller but still sizeable decline of 23 percent (panels B and C). The estimated decline using the narrower age band or the doughnut RDs (online Appendix Table 10) is about 40 percent. The larger estimates from doughnut RDs may result from netting out the impact of deferred care, which increases the likelihood of problems paying (and amounts owed in) medical bills. Failure to account for deferral will understate Medicare’s protection against medical-related financial strain.
E. Heterogeneity in Medicare’s Impact on Risk Exposure and Financial Strain
The effect of Medicare is likely to vary by socioeconomic status. Tables 6 and 7 break out the key MEPS and HTHS results by education group. The first panel in both tables shows that Medicare has the largest effect on insurance coverage for those with less than a high school education, who also have the lowest pre-64 coverage average. In contrast, those with more education tend to hold multiple insurance policies after age 65.
Table 6.
Impact of Medicare on Insurance and Spending by Education Group in the MEPS 2007–2010
| Medicare’s impact by educational attainment |
||||||
|---|---|---|---|---|---|---|
| Less than 12 years of education |
12 years of education |
More than 12 years of education |
||||
| Dependent variable | Any coverage | 2+ plans | Any coverage | 2+ plans | Any coverage | 2+ plans |
| Panel A. Insurance coverage and generosity | ||||||
| Age 65+ | 0.234** (0.023) |
0.433** (0.047) |
0.145** (0.016) |
0.548** (0.027) |
0.085** (0.010) |
0.654** (0.024) |
| Mean pre-65 | 0.71 | 0.09 | 0.84 | 0.06 | 0.91 | 0.05 |
| Relative effect | 32.96 | 481.11 | 17.26 | 913.33 | 9.34 | 1,308 |
| Observations | 7,603 | 7,603 | 10,524 | 10,524 | 15,164 | 15,164 |
| Dependent variable | Total spending |
OOP spending |
Total spending |
OOP spending |
Total spending |
OOP spending |
| Panel B. Total and out-of-pocket (OOP) spending | ||||||
| Age 65+ | 1,470 (1,356) |
−29 (99) |
−2,484* (1,423) |
−326** (102) |
−3,230** (986) |
−378*** (154) |
| Mean pre-65 | 6,221 | 707 | 6,333 | 895 | 6,372 | 1,119 |
| Relative effect | 23.62 | −4.17 | −39.22 | −36.42 | −50.69 | −33.78 |
| Observations | 7,603 | 7,603 | 10,524 | 10,524 | 15,164 | 15,164 |
Notes: Panel A considers the likelihood of any coverage (columns 1, 3, and 5) or the likelihood of 2 or more policies (columns 2, 4, and 6). Panel B considers total spending (columns 1, 3, and 5) or out-of-pocket spending (columns 2, 4, and 6). Across all outcomes, the first two columns are for those with less than 12 years of education, the third and fourth columns are for those with exactly 12 years of education, and the last two columns are for those with more than 12 years of education. All regressions include a constant, an indicator for ages 65 and above, and a quadratic in age in quarters that is allowed to vary on either side of age 65. Standard errors are clustered by age in quarters.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data are from the 2007–2010 Medical Expenditure Panel Survey and include respondents aged 50 to 80.
Table 7.
Impact of Medicare on Insurance and Medical Bill Problems by Education Group in the HTHS 2003, 2007, and 2010
| Medicare’s impact by educational attainment |
||||||
|---|---|---|---|---|---|---|
| Less than 12 years of education |
12 years of education |
More than 12 years of education |
||||
| Dependent variable | Any coverage |
2+ plans |
Any coverage |
2+ plans |
Any coverage |
2+ plans |
| Panel A. Insurance coverage and generosity | ||||||
| Age 65+ | 0.223** (0.051) |
0.501** (0.069) |
0.069** (0.032) |
0.600** (0.029) |
0.079** (0.018) |
0.706** (0.017) |
| Mean pre-65 | 0.694 | 0.134 | 0.848 | 0.07 | 0.918 | 0.046 |
| Relative effect | 32.13 | 373.88 | 8.14 | 857.14 | 8.61 | 1,535 |
| Observations | 3,507 | 3,507 | 10,366 | 10,366 | 16,299 | 16,299 |
| Dependent variable | Bill | Collections | Bill | Collections | Bill | Collections |
| Panel B. Medical bill problems and collections activity | ||||||
| Age 65+ | −0.153*** (0.044) |
−0.070 (0.043) |
−0.038 (0.038) |
−0.0004 (0.021) |
−0.038** (0.017) |
−0.028** (0.017) |
| Mean pre-65 | 0.262 | 0.157 | 0.203 | 0.126 | 0.136 | 0.073 |
| Relative effect | −58.40 | −44.59 | −18.72 | −0.32 | −27.94 | −38.36 |
| Observations | 3,485 | 3,481 | 10,332 | 10,330 | 16,271 | 16,268 |
| Dependent variable | Delay | Debt change | Delay | Debt change | Delay | Debt change |
| Panel C. Delayed major purchase and amount owed | ||||||
| Age 65+ | −0.097*** (0.039) |
−0.776 (0.506) |
−0.026 (0.038) |
−0.112 (0.254) |
−0.038** (0.016) |
−0.255 (0.017) |
| Mean pre-65 | 0.13 | 1,647 | 0.105 | 1,145 | 0.078 | 687 |
| Relative effect | −74.62 | −77.60 | −24.76 | −11.20 | −48.72 | −25.50 |
| Observations | 3,475 | 1,428 | 10,329 | 4,754 | 16,263 | 7,890 |
Notes: Panel A considers the likelihood of any coverage (columns 1, 3, and 5) or the likelihood of 2 or more policies (columns 2, 4, and 6). Panel B considers medical bill problems (columns 1, 3, and 5) or collections activity (columns 2, 4, and 6) and panel C considers delaying purchases (columns 1, 3, and 5) and the IHS of debt (columns 2, 4, and 6). Across all outcomes, the first two columns are for those with less than 12 years of education, the third and fourth columns are for those with exactly 12 years of education, and the last two columns are for those with more than 12 years of education. Questions about amounts owed were only asked in 2007 and 2010. All regressions include a constant, an indicator for ages 65 and above, and a quadratic in age in years that is allowed to vary on either side of age 65. Standard errors are clustered by age in years.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Source: Data are from the 2003, 2007, and 2010 waves of the Health Tracking Household Survey and are restricted to respondents aged 50 to 80.
Interestingly, the decline in out-of-pocket spending is concentrated in the more educated (panel B of Table 6), while reductions in financial strain effects are concentrated in the least educated (panels B and C of Table 7). Specifically, at age 65, out-of-pocket spending falls by about a third ($325–$378) for those with 12 years of schooling or more. Among those with less than 12 years of schooling, out-of-pocket spending declines by an insignificant 4 percent ($29) at age 65. In contrast, the likelihood of medical bill problems declines by about 58 percent at age 65 among those with less than 12 years of schooling but by 19 percent among those with 12 years of schooling. These findings may reflect differences in deferred care. Changes in utilization, although not statistically significant for any group, are largest for those with less than 12 years of schooling (not shown).
To further explore the heterogeneity of our results, we use the long panel in the HRS to investigate how effects differ by pre-65 insurance status. We find a decrease in out-of-pocket spending at age 65 that is concentrated at the right tail of the spending distribution and in the most recent time period (2008–2010; see online Appendix Table 11, panel B); reassuringly the HRS effects relative to the mean are very similar to those in the MEPS. Online Appendix Table 12 restricts to respondents with multiple observations before and after the transition to Medicare and shows results by pre-65 insurance status. Declines in out-of-pocket spending at age 65 are larger for those who were continuously insured prior to age 65 (that is, who report at least one source of coverage at every interview before turning 65). Among those who were not continuously insured prior to age 65, we find no statistically significant decline in mean out-of-pocket spending and much smaller and insignificant declines at the ninetieth and ninety-fifth percentiles. This pattern may be attributable to the sizeable and significant increases in utilization among those who were not continuously insured prior to age 65, due perhaps to improved access to or pent up demand for health care.
IV. Welfare Gain from Reductions in Out-of-Pocket Expenditure Risk
To interpret the economic significance of the estimated changes in out-of-pocket medical expenditures at age 65, we use a stylized expected utility framework to simulate the insurance value of Medicare. This approach is similar to the one used by Feldstein and Gruber (1995), FM (2008), Engelhardt and Gruber (2011), and Shigeoka (2014). It assumes a utility u(c) where c is nonhealth consumption and a budget constraint of c = y − m, where y is income and m out-of-pocket expenditure. m is a random variable with probability density function f(m) and support [0, m̄]. f(m) depends both on random health shocks and the nature of health insurance held (if any). Expected utility is given by
| (4) |
To calculate the welfare change associated with Medicare, we compare an individual’s risk premium (or certainty equivalence) under the pre- and post-65 spending distributions f(m). Following the literature, f(m) is based on the empirical distribution of medical spending in the MEPS. The risk premium (π) is the maximum amount that a risk-averse individual would be willing to pay to completely insure against the random variable m:
| (5) |
A decrease in risk exposure for the elderly relative to the near elderly would appear as a decline in the risk premium; this decline provides a dollar measure of the insurance value (and hence welfare gain) from Medicare coverage:
| (6) |
We use quantile estimates from (3) to simulate the expenditure distribution faced by individuals just below and above age 65 and to calculate the risk premium for both groups using (5). We focus on the results from the 2007–2010 sample in order to compare the contemporary costs and benefits of the program.30
As shown in Table 4 and Figure 3, Medicare shifts both the variance and mean level of out-of-pocket spending. However, the change in the mean of out-of-pocket spending for those just above relative to just below age 65 represents a transfer from the government to the insured and not a change in risk. To calculate a mean-preserving change in risk due to Medicare, for those 65 and older, we subtract out the mean reduction in out-of-pocket spending due to Medicare from individual income. This excludes from the calculation the private benefits from a transfer payment and will enable a comparison of social benefits to social costs.
In practice, the computation of (6) is as follows. First, we use the estimated parameters in (3), shown in online Appendix Figure 5, to simulate for each individual i in the sample the conditional (on individual’s characteristics X) quantiles (superscript j) of the out-of-pocket spending distribution pre-65 (without Medicare),
| (7) |
and post-65 (with Medicare):
| (8) |
for i = 1,…, N and j = 1,…, 99. The coefficients are estimated using 50–80-year-olds, but we focus on 64–66-year-olds for the prediction in order to better estimate the change in risk premium around the age 65 threshold. We set the very bottom of the distribution (j = 0) equal to 0 so that each person has 100 points of equal probability of occurrence in the out-of-pocket spending distribution. Following the literature, we truncate predicted out-of-pocket spending from below at zero and from above at 99 percent of individual income. We use this truncation because marginal utility goes to infinity as consumption (or income minus out-of-pocket spending in this case) goes to 0 in the CRRA model. Since out-of-pocket health spending can exceed income and, as discussed above, the share of such cases drops precipitously at age 65 (see Figure 4 and Table 4), this truncation underestimates the welfare value of Medicare.31
We calculate the risk premium without Medicare for each person using
| (9) |
where j indexes the quantile from the distribution. Similarly, the risk premium with Medicare for each person is
| (10) |
where μ is the estimate in Table 4 of the change in the mean out-of-pocket expenditures from Medicare ($326) for the 2007–2010 sample. Following the literature, we specify a constant relative risk aversion (CRRA) utility function, i.e., , where ρ is the Arrow-Pratt relative-risk aversion parameter. There is no consensus on what the coefficient of risk aversion is but the literature uses three as the benchmark, which McClellan and Skinner (2006) determine to be the value that best replicates observed spending among the low-income pre-Medicare population using the Panel Survey of Income Dynamics.32 For this reason, we focus on the results for a CRRA of three but discuss the sensitivity of the results (see online Appendix Table 13) to different risk aversion parameter values and truncations.
Using this method and a CRRA of three, we find an average decline in the risk premium (or a welfare gain) due to Medicare of $312 per person. As expected, the higher the coefficient of risk aversion, the higher the welfare gain; the gain varies from a negative $77 with a CRRA of 1 to $458 with a CRRA of 5.33
To put these welfare gains into perspective, we compare them to the social costs of the program. These costs include: the cost of raising revenue for the program, and the efficiency costs from the moral hazard effect of health insurance. Congressional Budget Office (CBO) estimates that increasing the Medicare eligibility age (MEA) by 1 year (to age 66) would save $21 billion dollars or $5,882 per Medicare beneficiary (CBO 2012).34 Using the consensus value for the deadweight loss per dollar of revenue raised of 30 cents (Poterba 1996), these figures imply an annual social program cost of $1,765 per recipient. Therefore, using the $312 average gain from reducing expenditure risk, the risk-protection afforded by Medicare at age 65 accounts for about 18 percent of the social costs of financing the program.35
The results in this paper suggest no moral hazard costs related to health insurance. That is, we fail to reject zero change in utilization at age 65 (see Table 3) and the “doughnut-RD” exercise points to limited strategic timing in or rationing of health care due to Medicare. However, since we may be underpowered to detect changes in utilization, we use estimates from the literature to calculate the moral hazard costs of Medicare. Card, Dobkin, and Maestas (2008) use hospital discharge data and find an increase of 8 percent in the discharge rate. Off an average discharge rate of 1,443 per 10,000 people in their sample, this implies an increase of roughly 0.01 stays per person at age 65.36 Using the 2007–2010 MEPS, we find that the average price for a hospital stay (calculated as total spending divided by number of stays) at age 64 is $2,052. Based on these estimates, the moral hazard costs of Medicare are relatively low—about $21 per person—and would not significantly change the cost-benefit analysis above.
Finally, this calculation ignores any impact of stress-reduction (from the reduced financial strain documented in Section IV) on health and any direct health improvements from Medicare. Dobbie and Song (2013), for example, find that bankruptcy protection decreases five-year mortality by 1.1 percentage points, suggesting that reduced financial strain has important health effects. Card, Dobkin, and Maestas (2009) find significant Medicare-induced mortality declines among those with emergent, nondeferrable conditions, specifically, a 20 percent reduction in 7-day mortality relative to hospital admission. Using standard value of life estimates, if Medicare extends life by an extra week between ages 64 and 65, the welfare gains due to medical expenditure risk reduction at age 65 more than fully balance the social costs of the program.37
V. Conclusion
Using the discontinuity in Medicare coverage at age 65, we demonstrate that Medicare plays an important role in protecting against medical expenditure risk. Using HTHS data, we show that both the fraction of the population reporting medical bill problems and collection agency contacts associated with medical bills decline by about a third at age 65. Likewise, the amount owed in medical bills declines by 33 percent (with a pre-65 mean amount owed of about $900).
Based on 2007–2010 MEPS data, we demonstrate that the distribution of out-of-pocket spending shifts significantly to the left at age 65. For example, out-of-pocket expenditures (all in 2010 dollars) drop by 33 percent ($326) at the mean and by 53 percent ($1,730) at the ninety-fifth percentile. The declines are smaller, but still significant if we consider the 1996–2010 period: out-of-pocket spending at age 65 drops by almost 20 percent at both the mean ($200) and the ninety-fifth percentile ($722). These results are robust to different strategies to deal with misspecification of functional form. They are unlikely to be substantially affected by potential rationing or deferability in health care utilization. Moreover, we find similar results if we use HRS data. A welfare calculation indicates that the reductions in out-of-pocket expenditure risk at age 65 translate into a welfare gain of 18 percent of Medicare’s social costs, not including any health benefits from lower financial stress or any direct health improvements.
How do our findings of the risk protective benefits of Medicare today compare to the Finkelstein and McKnight (2008)—referred to as FM—estimate from the introduction of Medicare in 1965? Both studies find similar relative reductions in out-of-pocket spending attributable to Medicare (on the order of 30–40 percent). While we find that these benefits account for about 18 percent of Medicare’s social costs, FM’s estimates put this number at 38 percent. Most of this difference is due to the large increase in Medicare’s cost since its introduction—the cost per beneficiary in our analysis ($1,394 in 2000 dollars) is almost 3 times the one used by FM ($537 in 2000 dollars). In addition, both studies find that the risk-reducing benefits of Medicare are concentrated in the top quartile of the spending distribution.
Several key differences between FM and the current study suggest some important nuances. FM uses a different empirical strategy—a difference-in-differences (DID) in contrast to the regression discontinuity (RD) approach used here. The DID versus RD comparison suggests two reasons why our results imply that Medicare may provide greater risk protection today than when it was first introduced almost 50 years ago. First, the RD provides average treatment effects for those just around the age 65 eligibility threshold. In contrast, FM calculate the average treatment effect of Medicare for individuals ages 65 to 74. Given that medical expenditure (and risk) increases sharply with age, the risk protection from Medicare should be greater at later ages. Second, because the transition to Medicare today increases coverage (and presumably generosity) on a much smaller scale than in 1965, our work should imply larger average effects.38 In other words, the change in expenditure risk we estimate comes from a smaller share of the population. Any rescaling— something we do not do because of changes in both coverage and generosity at age 65—would increase the magnitude of our estimates and the implied risk protection from Medicare today.
Our findings are important for policy. Several recent proposals to address rising Medicare spending and long-term federal budget shortfalls involve increasing the Medicare Eligibility age (MEA).39 Based on our findings, those 65 and 66-year-olds no longer eligible for Medicare would face a substantial decline in insurance coverage and increase in out-of-pocket expenditures and medical-related financial stress. Those in the right tail of the expenditure distribution would see an increase of several thousand dollars per year in out-of-pocket medical expenses and a consequent substantial financial loss. Accounting for the persistence in health status, those faced with a negative health shock might have high costs for multiple years, increasing the policy’s financial consequences.
While the Affordable Care Act (ACA) should attenuate the expenditure risk consequences of increasing the MEA, its success will be limited by the decision of many states, including large states such as Texas, Florida, and Louisiana, to opt-out of the Medicaid expansion. Even though recent enrollment reports have shown a decrease in the number of uninsured by 5 to 9 million people due to the ACA (through Medicaid expansions and the introduction of health insurance exchanges), the proportion of US adults lacking insurance was still high at 13.4 percent in May 2014 (Blumenthal and Collins 2014). In Texas, Florida, and Louisiana over 15 percent of the population remains uninsured.40 How the ACA will affect the financial consequences of increasing the MEA depends not only on how effective it is in reducing uninsurance but also on the relative generosity of the coverage newly gained. If those ages 65 and 66-years-old who are not eligible for insurance via Medicaid are unable to afford private options or can only afford plans that are substantially less generous than Medicare, increasing the MEA would increase their exposure to medical expenditure risk.
Acknowledgments
This work was funded by the National Institute on Aging (NIA R21-AG044737), the Commonwealth Fund’s Affordable Health Insurance Program, RAND’s Center for the Study of Aging (NIA P30 AG012815), and USC’s Resource Center for Minority Aging Research (NIA P30AG043073) and USC’s Roybal Center for Financial Decision Making (NIA P30AG024962). We thank Mahshid Abir, Abby Alpert, Sanjay Arora, Maria Casanova, Eileen Crimmins, Mark Friedberg, Dana Goldman, Arie Kapteyn, Adriana Lleras-Muney, Michael Menchine, Kathleen Mullen, David Powell, James P. Smith, Neeraj Sood, Daniel Waxman, Julie Zissimopoulos, three anonymous referees, and participants of the monthly USC Resource Center for Minority Aging Research (RCMAR) meetings, the Society of Econometrics annual summer meeting, the NBER Summer Institute Aging workshop, the All-California Labor Economics conference, and the European Conference on Household Finance for many helpful comments. Mikhail Zaydman provided excellent research assistance. All mistakes are our own.
Footnotes
Go to http://dx.doi.org/10.1257/pol.20140262 to visit the article page for additional materials and author disclosure statement(s) or to comment in the online discussion forum.
Although not centrally focused on medical expenditure risk, McWilliams et al. (2007) uses propensity score methods to compare changes in a range of outcomes, including expenditures, for previously (before age 65) insured and uninsured beneficiaries. This paper finds that as the previously uninsured gain Medicare coverage at age 65, they have a significant differential decrease in the odds of incurring high out-of-pocket medical spending.
Using a very different approach—a dynamic random utility model of the demand for health insurance— Khwaja (2010) concludes that the primary benefit of Medicare is insurance against high expenditures with smaller benefits in terms of improved health and longevity.
The only other paper we know of that uses an RD design to estimate the effect of insurance on medical expenditure risk is Shigeoka (2014), which analyzes a patient cost-sharing program in Japan.
In addition, if doctors overprovide expensive, high-tech care to insured patients (Wagstaff and Lindelow 2008), then medical expenditure risk could increase with coverage.
Because Medicare affects two dimensions of insurance at age 65—coverage and generosity—we cannot use an IV strategy.
Deferral, or what looks like deferral, could be caused by decreased treatment costs, increased income due to Medicare subsidies, and/or greater access to providers at age 65.
Results from the HRS show a similar pattern (discussed in Section III) as do sensitivity analyses focusing on individuals with nondeferrable medical conditions (available upon request).
Unfortunately, while the follow-up surveys supplement self-reported payment information, they do not update self-reported utilization (Zuvekas and Olin 2009). That is, the quantity of care from the household survey is taken as given and it is only expenditures that get updated/validated.
These comparisons adjust the NHEA for differences in the MEPS sample frame, i.e., noninstitutionalized households, as well as differences in included services (e.g., over-the-counter medicines are not captured in the MEPS), service category definitions, and so on. More than half of the remaining 17.6 percent (or $240 billion) difference in total health care spending is accounted for by physician and hospital spending and another 20 percent by “other medical equipment” such as ambulance services and durable medical equipment. See Bernard et al. (2012) for details.
We use the RAND HRS, version M (http://www.rand.org/labor/aging/dataprod/hrs-data.html), which contains harmonized versions of the variables of interest across all survey waves.
Earlier years of this survey do not ask directly about medical-related financial strain.
The publicly available data categorizes the amounts into 4 bins, top-coded at $10,000.
Because it does not capture Medicare Advantage (MA), this measure may underestimate benefit generosity at age 65. In 2006, the average net value of an MA plan exceeded traditional Medicare by $55 to $71 per month, depending on the plan type. See Merlis (2008) for details.
This measure is defined only for nonmissing values of income and out-of-pocket medical expenditures. Moreover, changes in this variable at age 65 are not driven by discontinuous changes in income.
For details of the MCS, see http://www.bls.gov/cpi/cpifact4.htm.
Assuming covariate smoothness holds, an assumption we partially test below, individual characteristics, Xi, are not needed but can be included to increase precision.
The variable age is measured as a deviation from age 65, therefore τ can be interpreted as the discontinuous change on outcome mi at age 65 (see Lee and Lemieux 2010), which makes the comparison between the RD graphs and tables easier.
See MEPS-HC Methodology Reports for more details at http://www.meps.ahrq.gov.
Bootstrapped standard errors that specify a common variance structure to reflect the complex sample design of the MEPS are generally smaller than those obtained from either clustering by age or the age-block bootstrap. Thus, we opt for a more conservative approach to inference.
The retirement question in the MEPS measures the fraction that reports having ever retired from any job or business. It is asked only of those ages 55 and older. Given it is not conditional on ever working the question yields somewhat low fractions retired, even at older ages.
In principle those with generous insurance might schedule some procedures prior to transitioning to Medicare. We know of no evidence in support of this theoretical possibility.
Of course, this depends on the physicians’ outside options. Physicians who treat primarily uninsured or Medicaid covered individuals will receive higher payments from Medicare.
Analyzing individuals who had unanticipated, nondeferrable health events to isolate the effect of Medicare on medical expenditure risk from any behavioral effect on the timing of care, we find larger risk-protective effects (available upon request). Our interest here is in the risk-protective value of Medicare for the whole population and not simply those who had a bad health shock.
Specifically, the HTHS allows us to look at Medicare plus a supplemental public or private plan or Medicare Advantage coverage. Restricting to just supplemental coverage, we still see a 64 percentage point increase in generosity (i.e., having two or more insurance plans) off a base of 6.4 percent in the HTHS data (not shown).
The Medicare Current Beneficiary Survey (MCBS) provides a more detailed breakdown of specific sources of Medicare coverage. For example, see http://kff.org/medicare/issue-brief/medigap-reform-setting-the-context/. The MCBS only includes respondents covered by Medicare.
At age 65 adults without disability who meet the financial limits are eligible for Supplemental Security Income (SSI) and in many states SSI delivers Medicaid. These are not driving forces in our study, since we do not find a significant discontinuous change in Medicaid coverage at age 65 (results available upon request), or a significant change in average income (see Figure 1), suggesting that these changes apply to too small of a fraction of the population to matter here.
This lack of evidence for intertemporal shifting of health care utilization is consistent with analysis of young adults as they age off of their parent’s insurance plans (Anderson, Dobkin, and Gross 2012) and of insurance transitions among the general population (Long, Marquis, and Rodgers 1998).
Other potential contributors include the rapid rise in total medical spending coupled with flat cost-sharing over time (Gruber and Levy 2009), and the growth in Medicare Advantage from less than 10 percent of beneficiaries in 1996 (Brown et al. 2014) to almost 25 percent in 2010 (KFF 2014). Brown et al. (2014) find that beneficiaries are more satisfied with (presumably lower average) out-of-pocket costs in Medicare Advantage plans than in traditional Fee-for-Service plans. Neither of these contributors explains the larger estimates since 2006 specifically, however. For example, MA enrollment increased from 1996–1999, declined rapidly, and since 2003 has been increasing.
This is consistent with “backward telescoping,” meaning more recent events are dated back in time. De Nicola and Gine (2011) show evidence of this in self-reported purchases.
This analysis carries the limitations of a static framework that ignores savings or borrowing to pay for a negative health shock and the idea that Medicare may affect savings and consumption decisions over the life cycle. Given that our estimates are cross-sectional—we don’t take into account serially correlated health shocks, for example—the static framework is an appropriate simplification. It also allows us to compare our results to the existing literature.
Using larger truncations of 60–80 percent of income, as done in the literature, further exacerbates bias.
As McClellan and Skinner (2006) point out, the simulation and determination of three as the best measure of relative-risk aversion also relies on parameter choices related to the relative value of medical spending in bad health and the “necessary” medical spending in bad and good health.
The welfare gain can be negative because, for those over 65, we subtract from the distribution of out-of-pocket spending the mean reduction in out-of-pocket spending due to Medicare (see equation 11). For some combinations of out-of-pocket spending truncation and CRRA parameters the reduction in mean out-of-pocket spending dominates the effect of the shift in the distribution of spending (or reduction in risk), resulting in a negative welfare benefit estimate. Specifically, individuals with very low risk aversion (e.g., a CRRA of 1) or with out-of-pocket spending that is less than 60 percent of income (except those with very high risk aversion, e.g., a CRRA of 5), value the risk reduction from Medicare less than the mean reduction in out-of-pocket expenditures.
In 2012, there were 3.57 million 65-year-olds (Census Bureau’s American Fact Finder).
It is important to note that this cost-benefit analysis is complicated by the fact that the transition to age 65 is related not only to insurance changes due to Medicare but also due to supplemental insurance. Since we only consider the financing costs of Medicare, this calculation would be an overestimate if the benefits come, in fact, from supplemental insurance acquired after age 65.
Card, Dobkin, and Maestas (2008) find an increase in doctor visits as well. Since the increase is small (1.3 percentage points or 1.5 percent) and doctor visits are cheap compared to hospital stays, this negligibly affects our estimates.
For example, using the $100,000 value of a year of life suggested in Cutler (2004), one extra week is valued at $1,923 (100,000 divided by 52 weeks) whereas the per recipient social cost of the program at age 65 net of the risk-protection benefit is just $1,453 or $1,765–$312.
At its introduction, Medicare increased health insurance coverage by 75 percentage points (Finkelstein 2007), while the corresponding increase at age 65 today is only 12 percentage points.
E.g., Emanuel 2012, Murray and King 2012, and Herger 2012.
Contributor Information
Silvia Helena Barcellos, Center for Economic and Social Research (CESR), University of Southern California (USC), 635 Downey Way, Los Angeles, CA 90089 (silvia.barcellos@usc.edu).
Mireille Jacobson, The Paul Merage School of Business, University of California, Irvine, CA 92697-3125 and National Bureau of Economic Research (NBER) (mireille@uci.edu).
REFERENCES
- Alemayehu Berhanu, Warner Kenneth E. The Lifetime Distribution of Health Care Costs. Health Services Research. 2004;39(3):627–642. doi: 10.1111/j.1475-6773.2004.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizcorbe Ana, Liebman Eli, Pack Sarah, Cutler David M, Chernew Michael E, Rosen Allison B. Measuring health care costs of individuals with employer-sponsored health insurance in the U.S.: A comparison of survey and claims data. Statistical Journal of the IAOS. 2012;28(1–2):43–51. doi: 10.3233/SJI-2012-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Michael, Dobkin Carlos, Gross Tal. The Effect of Health Insurance Coverage on the Use of Medical Services. American Economic Journal: Economic Policy. 2012;4(1):1–27. [Google Scholar]
- Baicker Katherine, Levy Helen. The Insurance Value of Medicare. New England Journal of Medicine. 2012;367(19):1773–1775. doi: 10.1056/NEJMp1210789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker Katherine, Taubman Sarah L, Allen Heidi L, Bernstein Mira, Gruber Jonathan H, Newhouse Joseph P, Schneider Eric C, et al. The Oregon Experiment—Effects of Medicaid on Clinical Outcomes. New England Journal of Medicine. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barcellos Silvia Helena, Jacobson Mireille. The Effects of Medicare on Medical Expenditure Risk and Financial Strain: Dataset. American Economic Journal: Economic Policy. 2015 doi: 10.1257/pol.20140262. http://dx.doi.org/10.1257/pol.20140262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreca Alan I, Lindo Jason M, Waddell Glen R. Heaping Induced Bias in Regression-Discontinuity Designs; National Bureau of Economic Research (NBER) Working Paper 17408; 2011. [Google Scholar]
- Bernard Didem, Cowan Cathy, Selden Thomas, Cai Liming, Catlin Aaron, Heffler Stephen. Reconciling Medical Expenditure Estimates from the MEPS and NHEA, 2007. Medicare and Medicaid Research Review. 2012;2(4):E1–E20. doi: 10.5600/mmrr.002.04.a09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal David, Collins Sara R. Health Care Coverage under the Affordable Care Act—A Progress Report. New England Journal of Medicine. 2014;371(3):275–281. doi: 10.1056/NEJMhpr1405667. [DOI] [PubMed] [Google Scholar]
- Brown Jason, Duggan Mark, Kuziemko Ilyana, Woolston William. How does Risk Selection Respond to Risk Adjustment? New Evidence from the Medicare Advantage Program. American Economic Review. 2014;104(10):3335–3364. doi: 10.1257/aer.104.10.3335. [DOI] [PubMed] [Google Scholar]
- Card David, Dobkin Carlos, Maestas Nicole. The Impact of Nearly Universal Insurance Coverage on Health Care Utilization: Evidence from Medicare. American Economic Review. 2008;98(5):2242–2258. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card David, Dobkin Carlos, Maestas Nicole. Does Medicare Save Lives? Quarterly Journal of Economics. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens Jeffrey, Gottlieb Joshua D. In the Shadow of a Giant: Medicare’s Influence on Private Physician Payments; National Bureau of Economic Research (NBER) Working Paper 19503; 2014. [Google Scholar]
- Congressional Budget Office (CBO) Raising the Ages of Eligibility for Medicare and Social Security. Washington, DC: CBO; 2012. Jan, [Google Scholar]
- Cutler David M. Your Money or Your Life: Strong Medicine for America’s Health care System. New York: Oxford University Press; 2004. [Google Scholar]
- de Nicola Francesca, Gine Xavier. How Accurate Are Recall Data? Evidence from Coastal India; World Bank Working Paper 6009; 2012. [Google Scholar]
- Dobbie Will, Song Jae. Debt Relief and Debtor Outcomes: Measuring the Effects of Consumer Bankruptcy Protection; National Bureau of Economic Research (NBER) Working Paper 20520; 2013. [Google Scholar]
- Efron Bradley, Tibshirani Robert J. An Introduction to the Bootstrap: Monographs on Statistics and Applied Probability. Vol. 57. New York: Chapman and Hall; 1994. [Google Scholar]
- Emanuel Ezekiel J. Entitlement Reform for the Entitled. New York Times Opinionator. 2012 May 20; http://opinionator.blogs.nytimes.com/2012/05/20/entitlement-reform-for-the-entitled/ [Google Scholar]
- Engelhardt Gary V, Gruber Jonathan. Medicare Part D and the Financial Protection of the Elderly. American Economic Journal: Economic Policy. 2011;3(4):77–102. [Google Scholar]
- Executive Office of the President (EOP) The Economic Report of the President. Council of Economic Advisers; 2014. Recent Trends in Health Care Costs, Their Impact on the Economy, and the Role of the Affordable Care Act; pp. 147–178. http://www.whitehouse.gov/sites/default/files/docs/erp_2014_chapter_4.pdf. [Google Scholar]
- Fairlie Robert W, Kapur Kanika, Gates Susan M. Is Employer-Based Health Insurance a Barrier to Entrepreneurship?; RAND Corporation Working Paper, WR-637-1-EMKF; 2010. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Washington, DC: U.S. Government Printing Office; 2012. [Google Scholar]
- Feldstein Martin, Gruber Jonathan. A Major Risk Approach to Health Insurance Reform. In: Poterba James M., editor. Tax Policy and the Economy. Vol. 9. Cambridge: MIT Press; 1995. pp. 103–130. [Google Scholar]
- Finkelstein Amy N. The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare. Quarterly Journal of Economics. 2007;122(1):1–37. [Google Scholar]
- Finkelstein Amy N, Taubman Sarah, Wright Bill, Bernstein Mira, Gruber Jonathan, Newhouse Joseph P, Allen Heidi, et al. The Oregon Health Insurance Experiment: Evidence from the First Year. Quarterly Journal of Economics. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein Amy N, McKnight Robin. What did Medicare Do? The Initial Impact of Medicare on Mortality and Out of Pocket Medical Spending. Journal of Public Economics. 2008;92(7):1644–1668. [Google Scholar]
- Gross Tal, Notowidigdo Matthew J. Health Insurance and the Consumer Bankruptcy Decision: Evidence from Expansions of Medicaid. Journal of Public Economics. 2011;95(7–8):767–778. [Google Scholar]
- Gruber Jonathan, Levy Helen. The Evolution of Medical Spending Risk. Journal of Economic Perspectives. 2009;23(4):25–48. doi: 10.1257/jep.23.4.25. [DOI] [PubMed] [Google Scholar]
- Herger Wally. Medicare Reform Crucial for Economic Health. Washington Times. 2012 Dec 11; http://www.washingtontimes.com/news/2012/dec/11/medicare-reform-crucial-for-economic-health/ [Google Scholar]
- Hurd Michael D, Rohwedder Susann. The Level and Risk of Out-of-Pocket Health Care Spending; Michigan Retirement Research Center Working Paper 2009-218; 2012. [Google Scholar]
- Kadiyala Srikanth, Strumpf Erin. How Does Health Insurance Impact Health? The Case of Medicare and Cancer Detection. 2012 http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2138454.
- Kaiser Family Foundation (KFF) Medicare Chartbook. (4th) 2010 http://kff.org/medicare/report/medicare-chartbook-2010/
- Kaiser Family Foundation (KFF) Medicare Advantage Fact Sheet. 2014 http://kff.org/medicare/fact-sheet/medicare-advantage-fact-sheet/
- Khwaja Ahmed. Estimating Willingness to Pay for Medicare Using a Dynamic Life-Cycle Model of Demand for Health Insurance. Journal of Econometrics. 2010;156(1):130–147. [Google Scholar]
- Lee David S, Card David. Regression Discontinuity Inference With Specification Error. Journal of Econometrics. 2008;142(2):655–674. [Google Scholar]
- Lee David S, Lemieux Thomas. Regression Discontinuity Designs in Economics. Journal of Economic Literature. 2010;48(2):281–355. [Google Scholar]
- Long Stephen H, Marquis M Susan, Rodgers Jack. Do People Shift Their Use of Health Services over Time to Take Advantage of Insurance? Journal of Health Economics. 1998;17(1):105–115. doi: 10.1016/s0167-6296(97)00014-3. [DOI] [PubMed] [Google Scholar]
- Marshall Samuel, McGarry Kathleen M, Skinner Jonathan S. The Risk of Out-of-Pocket Health Care Expenditure at the End of Life; National Bureau of Economic Research (NBER) Working Paper 16170; 2010. [PMC free article] [PubMed] [Google Scholar]
- Mazumder Bhashkar, Miller Sarah. The Effects of the Massachusetts Health Reform on Financial Distress; Federal Reserve Bank of Chicago Working Paper 2014-01; 2014. [Google Scholar]
- McClellan Mark, Skinner Jonathan. The Incidence of Medicare. Journal of Public Economics. 2006;90(1):257–276. [Google Scholar]
- McWilliams J Michael, Meara Ellen, Zaslavsky Alan M, Ayanian John Z. Use of Health Services by Previously Uninsured Medicare Beneficiaries. New England Journal of Medicine. 2007;357(2):143–153. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- Merlis Mark. The Value of Extra Benefits Offered by Medicare Advantage Plans in 2006. Menlo Park, CA: Kaiser Family Foundation; 2008. [Google Scholar]
- Murray Sara, King Neil., Jr Romney Offers Medicare Plan. Wall Street Journal. 2012 Feb 25; [Google Scholar]
- Pence Karen M. The Role of Wealth Transformations: An Application to Estimating the Effect of Tax Incentives on Savings. B. E. Journal of Economic Analysis and Policy. 2006;5(1):1–26. [Google Scholar]
- Poterba James M. Government Intervention in the Markets for Education and Health Care: How and Why? In: Fuchs Victor., editor. Individual and Social Responsibility: Child Care, Education, Medical Care, and Long-term Care in America. Chicago: University of Chicago Press; 1996. pp. 277–308. [Google Scholar]
- Quealy Kevin, Sanger-Katz Margot. Who Would Have Health Insurance if Medicaid Expansion Weren’t Optional. New York Times. 2014 Nov 3; [Google Scholar]
- RAND. RAND HRS Data Documentation, Version M. RAND Center for the Study of Aging. 2013 Aug [Google Scholar]
- Shigeoka Hitoshi. The Effect of Patient Cost Sharing on Utilization, Health, and Risk Protection. American Economic Review. 2014;104(7):2152–2184. [Google Scholar]
- Stanton Mark A. The High Concentration of US Health Care Expenditure. Agency for Healthcare Research and Quality (AHRQ) Publication 06-0060. 2006 [Google Scholar]
- Wagstaff Adam, Lindelow Magnus. Can Insurance Increase Financial Risk? The Curious Case of Health Insurance in China. Journal of Health Economics. 2008;27(4):990–1005. doi: 10.1016/j.jhealeco.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Webb Anthony, Zhivan Natalia A. What Is the Distribution of Lifetime Health Care Costs from Age 65?; Boston College Center for Retirement Research Working Paper 10-4; 2010. [Google Scholar]
- Zuvekas Samuel H, Olin Gary L. Accuracy of Medicare Expenditures in the Medical Expenditure Panel Survey. Inquiry. 2009;46(1):92–108. doi: 10.5034/inquiryjrnl_46.01.92. [DOI] [PubMed] [Google Scholar]