Abstract
Objective/Background
Autonomic dysreflexia is a potentially life-threatening condition which afflicts a significant proportion of individuals with spinal cord injuries (SCI). To date, the safety and efficacy of several commonly used interventions for this condition have not been studied.
Design
A retrospective chart review of the safety of a previously implemented nursing driven inpatient autonomic dysreflexia protocol.
Methods
Seventy-eight male patients with SCI who experienced autonomic dysreflexia while inpatient at our Veterans Affairs SCI unit over a 3–1/2-year period were included. The safety of a nursing driven protocol utilizing conservative measures, nitroglycerin paste, and oral hydralazine was evaluated.
Outcome Measures
Occurrence of adverse events and relative hypotensive events during all episodes treated with the protocol, and efficacy of attaining target blood pressure for all episodes with protocol adherence and for initial episode experienced by each patient.
Results
Four hundred forty-five episodes of autonomic dysreflexia were recorded in the study period, with 92% adherence to the protocol. When the protocol was followed, target blood pressure was achieved for 97.6% of all episodes. Twenty-three total adverse events occurred (5.2% of all episodes). All adverse events were due to hypotension and only 0.9% required interventions beyond clinical monitoring. Of each patient's initial autonomic dysreflexia episode, 97.3% resolved using the protocol without need for further escalation of care.
Conclusion
This inpatient nursing driven-protocol for treating autonomic dysreflexia utilizing conservative measures, nitroglycerin paste and oral hydralazine achieved target blood pressure with a high success rate and a low incidence of adverse events.
Keywords: Autonomic dysreflexia, Spinal cord injuries, Hydralazine, Nitroglycerin
Introduction
Autonomic dysreflexia (AD) is a clinical syndrome characterized by episodes of relative hypertension that occurs in individuals with spinal cord injury (SCI) due to cascades of deregulated sympathetic discharges.1 This condition occurs most commonly in individuals with lesions at or above the level of sympathetic splanchnic outflow (T6), with incidence increasing with more clinically complete SCI.2 AD is triggered by a variety of noxious stimuli (or rarely non-noxious stimuli3) below the level of injury—leading to increase in spinal cord mediated reflex sympathetic discharge and vasoconstriction. Due to loss of descending autonomic control, post-injury changes within the spinal cord and hypersensitivity of peripheral receptors, these sympathetic signals multiply unchecked.4 The most common causes of AD are over-distention of the bladder and bowel,5 though multiple other potential provoking stimuli have been identified.6,7 The signs and symptoms of AD include a sudden increase in systolic blood pressure (SBP) of at least 20 mmHg from baseline,5 and may also include accompanying bradycardia, headache, blurred vision, nasal congestion, anxiety, diaphoresis, flushing, and piloerection above the neurologic level.8
The primary treatment of AD focuses on removing the offending stimuli and preventing the complications of hypertensive emergency.1 If not addressed, these complications can include headache, seizures, stroke and even death.9 When conservative measures fail and systolic blood pressure climbs over 150 mmHg, pharmacologic treatment is recommended.10 While a myriad of pharmacologic options have been tried anecdotally,11,12 few studies detail their protocols or safety. Previous research with limited patients has evaluated calcium channel blockers (nifedipine13,14), alpha blockers (prazosin,15 terazosin16), angiotensin converting enzyme inhibitors (captropril12), and prostaglandin E2.17 Past case reports have also described the successful use of beta blockers (metoprolol18) and vasodilators (sodium nitroprusside).18 Despite their common use and recommendations in practice guidelines,10 there are no formal studies to date that have evaluated the use of vasodilators such as hydralazine and nitroglycerin paste in the treatment of AD. Additionally, most research has involved prophylaxis or treatment of AD induced by urological procedures, rather than the full range of possible clinical etiologies. Finally, while advocated as first line treatment, the safety of conservative (non-pharmacologic) management at the onset of an episode of AD has not been assessed.
The primary objective of this study was to evaluate the safety of a nursing driven protocol utilizing conservative management, nitroglycerin paste and hydralazine to treat AD. We additionally aimed to evaluate the efficacy of the protocol to achieve target blood pressures and characterize the episodes of AD in terms of duration, minimum and maximum blood pressure in relation to injury duration/level/severity (as determined by the International Standards for Neurological Classification of SCI-ISNCSCI19). This study represents the largest sample to date evaluating the safety of a protocoled treatment algorithm, employing conservative and pharmacologic interventions, for the management of AD.
Methods
The AD protocol was initiated on the Veterans Affairs (VA) Puget Sound SCI Unit in June 1999 as a clinical treatment protocol that adhered to current best practice guidelines. Inpatient nursing staff documented treatments and outcomes as part of the protocol charting. Approval was obtained from our institutional review board for a retrospective review of the safety of this protocol in treatment of AD for inpatients with SCI.
Subjects
Seventy-eight males with SCI hospitalized in the SCI unit with episodes of AD while inpatient between June 1999 and January 2003 were included in the study. Nursing staff recorded details for episodes of AD in a standardized template which was analyzed for purposes of this study. Full demographics appear in Table 1.
Table 1.
Patient demographics
| Sex | |
| Male | 78 (100%) |
| ASIA impairment scale | |
| A | 45 (58.4%) |
| B | 18 (23.4%) |
| C | 6 (7.8%) |
| D | 9 (10.4%) |
| Neurologic Level of injury | |
| C1–C4 | 17 (21.8%) |
| C5–C8 | 46 (59.0%) |
| T1–T7 | 15 (19.2%) |
| Age* | |
| Mean age (min, max, SD) | 55.9 years (25, 81, 13.0) |
| Initial cause of injury | |
| Motor vehicle collision | 32 (41.0%) |
| Diving | 13 (16.7%) |
| Fall | 12 (15.4%) |
| Other trauma | 9 (11.5%) |
| Gunshot wound | 6 (7.7%) |
| Medical | 6 (7.7%) |
| Years since injury, n = 72 | |
| 0–5 years | 18 (25.0%) |
| 5–10 years | 4 (5.6%) |
| > 10 years | 50 (69.4%) |
| Mean (SD) | 20.6 years (15.7) |
| Median (min, max) | 20 years (0,58) |
*Age at time of first AD episode while inpatient during the study period.
Autonomic dysreflexia protocol
The AD protocol was designed using the Consortium for Spinal Cord Medicine's clinical practice guideline: “Acute Management of Autonomic Dysreflexia: Adults with Spinal Cord Injury Presenting to Health-Care Facilities,”10 as well as the clinical experience of three full-time SCI boarded physicians in coordination with an inpatient SCI nurse manager. This protocol was designed to be carried out by nursing staff independent from physicians except in the event of protocol failure or adverse event. The beginning of an AD episode was clinically defined by either 1) The presence of patient symptoms of AD and systolic blood pressure elevation greater than 150 mmHg or 2) The presence of systolic blood pressure elevated above 150 mmHg as measured on routine vital sign checks. Once the patient met the clinical definition for an episode of AD, the protocol was initiated as described in Figure 1. AD episodes were defined as resolved if systolic blood pressure persisted below 150 mmHg. If there was recurrence of an AD episode (as defined above) within 2 hours of a previously resolved episode, clinical recurrence was noted and the length of the episode and interventions were grouped to encompass both linked events. Any deviations from the protocol were documented.
Figure 1.
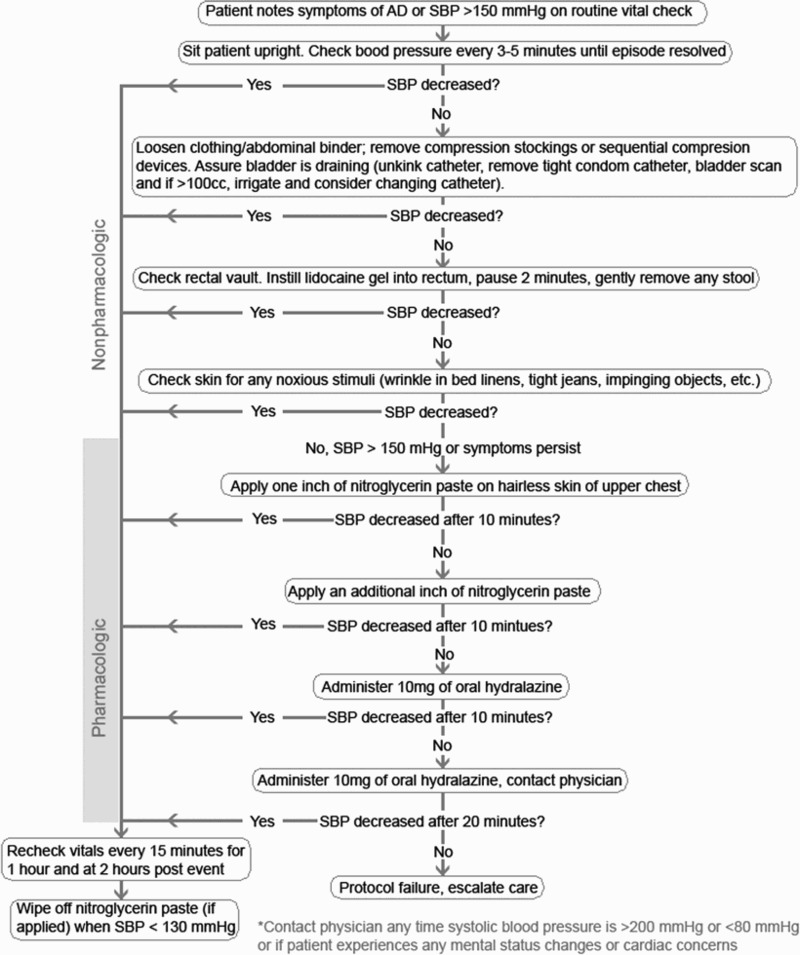
Flowchart of nursing driven protocol for addressing autonomic dysreflexia.
Adverse events were defined as systolic blood pressure less than 70 mmHg, diastolic blood pressure less than 40 mmHg, cardiovascular event (myocardial infarction, cerebrovascular accident, etc.), retinal detachment, arrhythmia, need for IV medication, medical instability necessitating transfer to the intensive care unit, or death. Protocol failure was defined as inability to lower systolic blood pressure less than 150 mmHg or continuation of symptoms after the protocol was completed.
Statistical analysis
IBM SPSS statistical software (Version 19.0, IBM Corp., Armonk, NY) was used for data analysis. All recorded episodes of AD were used to calculate frequencies of episode characteristics [American Spinal Injury Association Impairment Scale (AIS)],19 neurologic level, presenting symptom, and suspected cause) as well as mean initial vital signs. Mean maximum blood pressures, mean drop in systolic blood pressure from initial presentation, and occurrence of rebound episode within 2 hours of seemingly resolved episodes were calculated for both the events which followed the protocol and those with protocol deviations. Frequencies were calculated for resolution of AD and adverse events at each step in the treatment protocol. The total frequency of adverse events was calculated for both the episodes where the protocol was followed as well as all recorded episodes (including those with protocol deviations) in a model to test real world applicability. Episodes where systolic blood pressure dropped to between 70 and 79 mmHg were classified as relative hypotensive events; we performed additional chart review for each of these episodes to rule out the occurrence of other adverse events. Due to several individuals having a disproportionately high number of AD episodes, we limited some analyses to the first episode of AD that occurred for each patient. Using this method, the efficacy of the protocol was evaluated by determining the frequency of patients successfully achieving target blood pressure when the protocol was used.
Results
Over the study period, 445 AD events were logged (episodes characteristics in Tables 2 and 3). Of these, 35 (7.8%) demonstrated deviation from the AD protocol and were thus excluded from protocol specific analyses of the study (effective n = 410). The most common reasons for protocol deviation were the administration of an alternative medication or administering a protocol medication in an order not consistent with the protocol. All 445 events were subsequently analyzed in an intention to treat model for real world applicability of protocol implementation.
Table 2.
Autonomic dysreflexia episode characteristics
| Percentage of total episodes per ASIA Impairment Scale | |
| A | 61.6% |
| B | 29.7% |
| C | 4.7% |
| D | 4.0% |
| Percentage of total episodes per neurologic level | |
| C1–C4 | 17.3% |
| C5–C8 | 74.4% |
| T1–T7 | 8.3% |
| Mean (SD) initial SBP | 188.1 mmHg (26.0) |
| Mean (SD) initial DBP (n = 444) | 102.5 mmHg (18.1) |
| Mean (AD) initial HR (n = 430) | 75.1 (19.1) |
| Presenting symptom* | |
| Headache | 50.9% |
| Asymptomatic | 30.8% |
| Flushing | 8.1% |
| Sweating | 7.8% |
| Piloerection | 1.5% |
| Nasal congestion | 0.7% |
| Blurred vision | 0.2% |
| Nursing identified presumed cause of AD | |
| Unknown | 64.5% |
| Urinary retention | 10.5% |
| Full bowel | 6.5% |
| Post op | 5.6% |
| Bowel care | 5.4% |
| UTI | 2.5% |
| Musculoskeletal pain | 2.5% |
| Abdominal pain | 2.0% |
| Urinary stone | 0.2% |
| Bladder spasm | 0.2% |
n = 445 unless indicated otherwise. *n = 158. Remainder of presenting symptoms unspecified.
Table 3.
Variations in AD episode characteristics per protocol adherence
| Protocoled (n = 410 unless otherwise noted) | Protocol deviations (n = 35 unless otherwise noted) | All AD events | |
|---|---|---|---|
| Mean (SD) max SBP | 200.0 mmHg (24.2), n = 409 | 205.3 mmHg (18.1) | 200.4 mmHg (27.6), n = 444 |
| Mean (SD) max DBP | 109.1 mmHg (19.5), n = 409 | 109.4 mmHg (15.4) | 109.1 mmHg (19.1), n = 444 |
| Mean (SD) SBP drop from initial | 76.3 mmHg (36.6) | 60.6 mmHg (41.0) | 75.1 mmHg (37.2) |
| Rebound AD episodes | 12.4% | 31.4% | 14.0% |
| Percent attaining target BP | 97.6% | 57.1% | 94.4% |
| Mean (SD) episode duration | 63.1 min (76.0) n = 408 | 130.6 min (112.9) | 68.3 min (81.3), n = 439 |
| Relative hypotension percentage | 2.9% | 5.7% | 3.3% |
| Adverse events | 5.4% | 2.9% | 5.2% |
Of these 410 events of protocol adherence, 43 (10.5%) were successfully treated with only nonpharmacologic intervention. 157 events (38.3%) were successfully managed with the first one inch dose of nitroglycerin paste after conservative measures had failed. One hundred forty-two (34.6%) events required application of a second one-inch dose of nitroglycerin paste for AD resolution. Forty-three (10.5%) events required one dose of 10 mg hydralazine PO and 15 (3.6%) of events resolved after a second 10 mg of hydralazine. Ten events, (2.4%) required further escalation of care beyond the protocol. The relative efficiency of each step in the protocol in resolving an episode of AD is presented in Table 4. In total, 97.6% of events of AD charted were successfully treated when using this nursing driven protocol. The 10 events that did not meet the efficacy endpoint required additional PO or topical short acting antihypertensive agents.
Table 4.
Percentage of successful resolution of autonomic dysreflexia per step in the treatment protocol
| Step in protocol | Number of events at this step | Number of events resolved at this step | Relative resolution this step | Cumulative resolution |
|---|---|---|---|---|
| Nonpharmacologic | 410 | 43 | 10.5% | 10.5% |
| First 1″ NTP | 367 | 157 | 42.8% | 48.8% |
| Second 1″ NTP | 210 | 142 | 67.6% | 83.4% |
| First 10 mg of hydralazine | 68 | 43 | 63.2% | 93.9% |
| Second 10 mg of hydralazine | 25 | 15 | 60.0% | 97.6% |
| Additional antihypertensive agents after protocol | 10 | 10 | 100% | 100% |
Of the 445 total events, the mean number of events per individual was 5.7 (SD of 10.5, range 1–70). There were six individuals with greater than 15 events during the study period (mean number of events of this group = 34.7, SD 24.3). Excluding these six individuals, the mean number of events decreased to 3.3 (SD 3.3). Due to the large range in number of events per individual, efficacy of the protocol was evaluated using the first recorded AD event of each patient in an effort to eliminate bias in estimates due to correlation from repeated observation in the same patient (Table 5).
Table 5.
Efficacy of protocol when fully implemented for first recorded episode of autonomic dysreflexia per patient
| Protocol adherence | 94.9% | |
| Protocol success (n = 74) | 97.3% | |
| Adverse events | 6.4% | |
| Relative hypotension | When protocol followed (n = 74) = 1.4% | Including protocol deviations = 2.6% |
n = 78 unless otherwise noted.
Adverse events
Of all recorded episodes of AD, 23 adverse events occurred in 13 different patients. For these adverse events, the protocol was followed with 95.6% adherence. 14 of the adverse events (60.9%) were due to systolic blood pressure less than 70 mmHg and 17 (73.9%) were due to diastolic blood pressure less than 40 mmHg—notably eight events met both of these criteria. In total, 22.7% of the adverse events occurred prior to pharmacological intervention, 31.8% after application of the first inch of nitroglycerin paste but before the second, 40.9% after the second inch of nitroglycerin paste but before hydralazine, and one adverse event (4.5%) occurred during after the initial 10 mg dose of hydralazine.
Further interventions outside of clinical observation were required for only four events (17.4%), occurring in four individuals. During one event, an individual required midodrine when he experienced hypotension after being treated nonpharmacologically. A second patient required 1L of intravenous normal saline (following 1 inch of nitroglycerin) to achieve relative normotension. In the remaining two adverse events, both individuals were transferred to the intensive care unit due to rapid blood pressure fluctuation. The first individual was treated with the protocol through receipt of the second inch of nitroglycerin paste. Systolic blood pressure dropped from 264 mmHg at initial presentation to 74 mmHg. The second individual had SBP drop from 200 mmHg to 40 mmHg after receiving one inch of nitroglycerin paste. None of these adverse events resulted in permanent sequelae for any of the patients.
Protocol failures
Of the 410 events in which the protocol was followed, 10 (2.4%) were considered protocol failures due to inability to attain the target of systolic blood pressure less than 150 mmHg at completion of the protocol. Characteristics of these protocol failures appear in Table 6. Two of these events required only observation to ensure patient clinical stability, while the remaining eight required further pharmacological intervention. For pharmacologic treatment, five episodes required an additional one to two inches of nitroglycerin paste while one received an additional 5 mg of PO hydralazine. One episode required an additional 10 mg of PO hydralazine along with an additional two inches of nitroglycerin paste. The final episode required 50 mg of PO hydralazine and a total of 16 inches of nitroglycerin paste.
Table 6.
Protocol failure episode characteristics, (SD), n = 10
| Initial SBP | 186.8 mmHg (22.8) |
| Initial DBP | 102.9 mmHg (15.1) |
| Initial HR | 81.6 mmHg (22.7) |
| Mean max SBP | 217.9 mmHg (17.2) |
| Mean max DBP | 126.6 mmHg (37.0) |
| Mean SBP drop from initial | 74.0 mmHg (37.7) |
| Rebound AD episode (incidence) | 50% |
| Mean episode duration | 68.3 min (81.3) |
| Relative hypotension (incidence) | 10% |
| Adverse Events (incidence) | 0% |
The 10 protocol failures occurred in seven different individuals. One individual had 4 associated protocol failures; however, he had a total of 36 events recorded (failure rate of 11.1%). All 10 events occurred in individuals with AIS grade A or B injuries (71% and 29% respectively).
Discussion
Although guidelines exist for the management of episodes of AD in SCI populations, there is a paucity of data describing their outcomes with regard to safety and efficacy other than when used to prevent or treat episodes caused by urological procedures. Our study suggests that inpatients with SCI, experiencing an episode of AD, can be safely and effectively managed with a nursing driven protocol utilizing conservative management, and pharmacologic interventions of nitroglycerin paste and hydralazine. Of 410 AD episodes managed within protocol guidelines, 5.4% experienced adverse events. The majority of these were hypotension as defined solely by vital sign parameters. All but four adverse events (0.9% of all episodes) were self-limited and resolved with observation alone. Two events required limited intervention to support blood pressure (normal saline or midodrine) and two required transfer to the ICU for fluctuations in blood pressure. This appears to be a safe approach to management, though no comparable study exists to define relative safety. The protocol was effective, with 97.3% of patients achieving the target blood pressure following their first episode of AD during the study period. Given the relatively small number of failures observed during the protocol, we were unable to identify patient factors associated specifically with these failures.
Our study is unique in the number of patients enrolled and, to our knowledge, represents the first evaluation of safety and efficacy of an AD protocol designed using current guidelines. As such there are limited data to which we can compare outcomes. Previous research has been conducted on single agents with smaller numbers of episodes and patients. Small studies of nifedipine (n = 4 and 12) report this agent maybe useful for management of active AD.13,14 Captopril was reported to be 94% successful with no episodes of hypotension in 33 events of AD.12 Prazosin has been reported to be effective for the prophylaxis of AD.15
Our study is also unique in that a nursing-driven protocol is employed. This potentially offers several advantages over a physician driven protocol. First, appropriate treatment can be delivered more rapidly to patients with active AD, potentially reducing overall episode length and severity, and minimizing associated complications. Second, physician time may be better utilized by managing episodes that are not successfully managed within the protocol. Third, a standardized protocol with clear parameters and decision points may be applied to lower resourced settings such as skilled nursing facilities, hospitals without physicians trained in SCI care, and rehabilitation units without in-house call available.
We recognize several limitations of this study. First, a nursing-driven protocol may also hold several disadvantages when compared to physician management. It is possible that nurses inadvertently treated essential hypertension, or other causes of hypertension, instead of AD. One would expect that essential hypertension treated according to protocol guidelines would demonstrate higher rates of pharmacologic intervention, asymptomatic presentation, and recurrence after protocol conclusion. We did observe 30.8% of episodes reported as asymptomatic, but did not observe frequent recurrence of hypertension in the time expected for the effect of protocol interventions to have ceased. Additionally, even if essential hypertension was present in some of the patients treated with this protocol it did not seems to result in adverse outcomes and we would expect that ideally facilities utilizing similar protocols would have physicians review patients with frequent recurrences.
A second limitation is the possibility that nursing-driven protocols under-diagnose underlying etiologies and potentially increase recurrence of episodes by not addressing the precipitating cause. We did note that in 64.5% of episodes, nursing did not define a clear etiology, but we do not have similar data on physician identification of AD etiologies to compare to. We also did not observe high recurrence rates, except in 6 patients who experienced more than 15 episodes.
A third limitation is the likelihood that many patients were not tracked using the protocol if they responded rapidly to conservative management. This would explain the lower than expected percentage of episodes managed effectively with conservative care alone. However, we would expect the inclusion of these less-severe episodes in the current analysis to result in better overall safety and efficacy of the protocol.
A fourth limitation is that the patient population was entirely based at a Veterans Affairs SCI Unit, exclusively male, with relatively long duration of SCI, and often had recently had a surgical procedure performed. It is possible, for example, that female patients with lower average blood pressures20,21 would have more frequent and severe adverse events with this protocol's recommended interventions. Furthermore, patients with more recent injuries might have altered physiology, requiring a different approach.
Conclusions
In conclusion, we found that patients with SCI experiencing AD had a high success rate and few adverse events when episodes were managed with a nursing driven protocol utilizing conservative management, nitroglycerin paste and hydralazine. Further studies will be needed to clarify the interventions and protocol parameters that provide the best possible efficacy and safety, and to identify the differences needed in the management of different populations with SCI.
Acknowledgments
This work was supported with resources and use of facilities at the VA Puget Sound Health Care System. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
References
- 1.Krassioukov A, Warburton DE, Teasell R, Eng JJ; Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil 2009;90(4):682–95. doi: 10.1016/j.apmr.2008.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen D, Apple DF, Hudson LM, Bode R. Medical complications during acute rehabilitation following spinal cord injury-current experience of the Model Systems. Arch Phys Med Rehabil 1999;80(11):1397–401. doi: 10.1016/S0003-9993(99)90250-2 [DOI] [PubMed] [Google Scholar]
- 3.Khurana RK. Orthostatic hypotension-induced autonomic dysreflexia. Neurology 1987;37(7):1221. doi: 10.1212/WNL.37.7.1221 [DOI] [PubMed] [Google Scholar]
- 4.Krenz NR, Meakin SO, Krassioukov AV, Weaver LC. Neutralizing intraspinal nerve growth factor blocks autonomic dysreflexia caused by spinal cord injury. J Neurosci 1999;19(17):7405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teasell RW, Arnold JMO, Krassioukov A, Delaney GA. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil 2000;81(4):506–16. doi: 10.1053/mr.2000.3848 [DOI] [PubMed] [Google Scholar]
- 6.Scott MB, Morrow JW.. Phenoxybenzamine in neurogenic bladder dysfunction after spinal cord injury. II. Autonomic dysreflexia. J Urol 1978;119(4):483–4 [DOI] [PubMed] [Google Scholar]
- 7.Abouleish EI, Hartley ES, Palmer SM.. Can epidural fentanyl control autonomic hyperreflexia in a quadriplegic parturient? Anesth Analg 1989;68(4):523–6. doi: 10.1213/00000539-198904000-00019 [DOI] [PubMed] [Google Scholar]
- 8.Karlsson A. Autonomic dysreflexia. Spinal cord 1999;37(6):383–91. doi: 10.1038/sj.sc.3100867 [DOI] [PubMed] [Google Scholar]
- 9.Kursh ED, Freehafer A, Persky L.. Complications of autonomic dysreflexia. J Urol 1977;. 118:70–2. [DOI] [PubMed] [Google Scholar]
- 10.Linsenmeyer TA, Baker ER, Cardenas DD, Mobley T, Perkash I, Vogel LC, et al. Acute management of autonomic dysreflexia: Individuals with spinal cord injury presenting to health-care facilities. Consortium for spinal cord medicine clinical practice guidelines. 2nd ed. Clinical Practice Guidelines: Spinal Cord Medicine 2001: Consortium for Spinal Cord Medicine. [Google Scholar]
- 11.Braddom RL, Rocco JF.. Autonomic dysreflexia: a survey of current treatment. Am J Phys Med Rehabil 1991;70(5):234–41. doi: 10.1097/00002060-199110000-00002 [DOI] [PubMed] [Google Scholar]
- 12.Esmail Z, Shalansky KF, Sunderji R, Anton H, Chambers K, Fish W.. Evaluation of captopril for the management of hypertension in autonomic dysreflexia: a pilot study. Arch Phys Med Rehabil 2002;83(5):604–8. doi: 10.1053/apmr.2002.30911 [DOI] [PubMed] [Google Scholar]
- 13.Thyberg M, Ertzgaard P, Gylling M, Granerus G. Effect of nifedipine on cystometry-induced elevation of blood pressure in patients with a reflex urinary bladder after a high level spinal cord injury. Paraplegia 1994;32:308–13. doi: 10.1038/sc.1994.53 [DOI] [PubMed] [Google Scholar]
- 14.Lindan R, Leffler EJ, Kedia KR. A Comparison of the efficacy of an alpha-I-adrenergic blocker in the slow calcium channel blocker in the control of autonomic dysreflexia. Paraplegia 1985;23:34–8. doi: 10.1038/sc.1985.6 [DOI] [PubMed] [Google Scholar]
- 15.Krum H, Louis WJ, Brown DJ, Howes LG.. A study of the alpha-1 adrenoceptor blocker prazosin in the prophylactic management of autonomic dysreflexia in high spinal cord injury patients. Clin Auton Res 1992;2(2):83–8. doi: 10.1007/BF01819662 [DOI] [PubMed] [Google Scholar]
- 16.Vaidyanathan S, Soni BM, Sett P, Watt JWH, Oo T, Bingley J. Pathophysiology of autonomic dysreflexia: long-term treatment with terazosin in adult and paediatric spinal cord injury patients manifesting recurrent dysreflexic episodes. J Urol 1999;162(3):968–9. doi: 10.1097/00005392-199909010-00120 [DOI] [PubMed] [Google Scholar]
- 17.Frankel H, Mathias CJ. Severe hypertension in patients with high spinal cord lesions undergoing electro-ejaculation managment with prostaglandin E2. Paraplegia 1980;18:293–9. doi: 10.1038/sc.1980.52 [DOI] [PubMed] [Google Scholar]
- 18.Pasquina PF, Houston RM, Belandres PV.. Beta blockade in the treatment of autonomic dysreflexia: a case report and review. Arch Phys Med Rehabil 1998;79(5):582–4. doi: 10.1016/S0003-9993(98)90077-6 [DOI] [PubMed] [Google Scholar]
- 19.Maynard FM, Bracken MB, Creasey GJFD, Dittuno JF, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997;35(5):266–74. doi: 10.1038/sj.sc.3100432 [DOI] [PubMed] [Google Scholar]
- 20.Khoury S, Yavows SA, O'brien TK, Sowers JR.. Ambulatory blood pressure monitoring in a nonacademic setting: effects of age and sex . Am J Hypertens 1992;5(9):616–23. [DOI] [PubMed] [Google Scholar]
- 21.Wiinberg N, Høegholm A, Christensen HR, Bang LE, Mikkelsen KL, Nielsen PE, et al. 24-h ambulatory blood pressure in 352 normal Danish subjects, related to age and gender. Am J Hypertens 1995;8(10):978–86. doi: 10.1016/0895-7061(95)00216-2 [DOI] [PubMed] [Google Scholar]


