Abstract
Objective
Describe the incidence and distribution of appendicular fractures in a cohort of veterans with spinal cord injury (SCI).
Design
Retrospective, observational study of fractures in veterans with a chronic traumatic SCI.
Setting
The Veterans Health Administration (VA) healthcare system.
Participants
Veterans included in the VA Spinal Cord Dysfunction Registry from Fiscal Years (FY) FY2002–FY2007.
Interventions
Not applicable.
Main Outcome Measures
Description of fractures by site and number. Mortality at one year following incident fracture among men with single vs. multiple fractures.
Results
Male and female veterans sustained incident fractures with similar observed frequency (10.5% vs 11.5%). The majority of fractures occurred in the lower extremities for both men and women. In men, a complete extent of injury (compared to incomplete) was associated with 41% greater relative risk (RR) of incident fracture (RR 1.41, 95% confidence interval [1.17, 1.70]) among those with tetraplegia, but not paraplegia. Furthermore, many men (33.9%, n = 434) sustained multiple fractures over the course of the study. There were no differences in mortality between men who sustained a single fracture and those who had multiple fractures.
Conclusions
The extent of injury may be an important predictor of fracture risk for male veterans with tetraplegia. Once a fracture occurs, male veterans with SCI appear to be at high risk for additional fractures.
Keywords: Spinal cord injuries, Osteoporosis, Bone fractures, Epidemiology
Introduction
There are approximately 300,000 individuals in the United States living with a Spinal Cord Injury (SCI), and this number is expected to rise with time.1,2 While the severity of the SCI impacts the degree of bone loss, nearly all persons with SCI lose bone mineral density (BMD) in the long bones below the level of the spinal injury3; additionally, heterotopic ossification (HO), which does occur in persons with SCI, is also associated with bone loss.4 Thus, osteoporosis-related fractures are a major issue in this population.3,5 The exact prevalence of fractures in the SCI population is not known, as some fractures go unrecognized; however, recently it was reported that in male veterans with SCI of at least two years’ duration, there is a 14% five-year incidence of lower extremity fractures.5
A fracture in a person with SCI may have serious consequences. Following a lower extremity fracture, the risk of pressure ulcers, respiratory infections, urinary tract infections, blood clots, depression, and delirium is significantly increased.5 A fracture in a person with SCI also significantly raises the mortality rate above and beyond the original spinal injury.6 However, detailed studies including more recent data on the epidemiology of appendicular fractures in persons with chronic SCI are lacking.
Methods
Persons
The Veterans Health Administration (VA) Spinal Cord Dysfunction (SCD) Registry is an administrative clinical database maintained by individual VA medical centers to track the population of veterans with SCD (including SCI) followed at each center.7 These data are also aggregated at a national level; therefore, the SCD Registry represents veterans with SCD across the United States. All men included in the SCD Registry from fiscal years 2002–2007 with a traumatic SCI of at least two years’ duration were eligible for the analyses. Females represented a very small minority of the VA SCD population (3.0%) and are described separately to minimize heterogeneity in our sample. This study focused on traumatic SCI etiology based on a previous study showing that traumatic causes of SCI were associated with an increased risk for fracture compared with nontraumatic causes of SCI.8 Only those with a minimum of two years’ duration of SCI were included as a new steady-state between bone resorption and bone formation is reached approximately eighteen months to two years following SCI.3,9 Information on etiology, duration, level, and completeness of the SCI was obtained from the Registry. Persons with a missing duration of injury were excluded, as chronicity of the SCI could not be determined. As an indicator of overall health, Charlson comorbidity indices10 were calculated using data available within a year preceding incident fracture. The Charlson comorbidity index quantifies the association of the number and severity of major comorbid conditions (e.g. cardiovascular disease, diabetes, cancer) with 10-year mortality.10 If an individual did not have any VA utilization in the year preceding an incident fracture then the two years prior to an incident fracture were used to calculate the individual's Charlson comorbidity index. Diagnoses were determined using VA Medical SAS Inpatient Datasets and the Outpatient Care File. The full 18-item weighted Charlson comorbidity index was used, excluding the category for paraplegia/tetraplegia. If the person had an International Classification of Diseases, Ninth Revision (ICD-9) code contained within the Charlson comorbidity index, that person was assigned the corresponding comorbidity and was given a score of 1; if the person did not have the comorbidity or if there was no recording of that comorbidity, then that person was given a score of 0. After all individual comorbidities had been assessed for a given person, the comorbidities were summed for their final Charlson comorbidity index aggregate score.
The study was approved by the Veterans Affairs Institutional Review Board and principles of the Declaration of Helsinki were followed.
Incident fractures
Fractures were defined using ICD-9 codes.11 Table 1 includes the ICD-9 codes for the fracture sites of interest. A fracture was considered “incident” if there were no encounters with the same 3-digit ICD-9 code within a 120-day time period prior to the date of the identified fracture.8 Pathologic fractures (ICD-9 code 733), ill-defined fractures of the lower extremity, site-unspecified fractures, and multiple fractures that occurred on the same day at discrete sites were excluded. Fractures from high-energy, external traumatic events having a supplemental ICD-9 “E-code”,12 were excluded, except those resulting from an non-specific fall (E-code 888.9), which are described separately.
Table 1.
ICD-9 codes for appendicular fractures
| Fracture Site | ICD-9 Code |
|---|---|
| Scapula | 810.x |
| Clavicle | 811.x |
| Humerus | 812.x |
| Forearm | 813.x |
| Carpal | 814.x |
| Metacarpal | 815.x |
| Phalanges of hand | 816.x |
| Multiple fractures of hand | 817.x |
| Pelvis | 808.x |
| Femoral neck | 820.x, 820.1x, 820.8, 820.9 |
| Trochanteric | 820.20, 820.30 |
| Intertrochanteric | 820.21, 820.31 |
| Subtrochanteric | 820.22, 820.32 |
| Femur | 821.x |
| Patella | 822.x |
| Tibia/Fibula | 823.x |
| Ankle | 824.x |
| Tarsals/Metatarsals | 825.x |
| Phalanges of foot | 826.x |
Mortality
Date of death was obtained from the National Death Index (NDI) of the National Center for Health Statistics13 and the VA Vital Status File.14 NDI records are available approximately 16 months after the conclusion of a given year.14 Mortality was ascertained one year following the incident fracture.
Statistical analysis
For the primary analyses, male veterans were divided into three groups: (1) persons with a single upper extremity fracture, (2) persons with a single lower extremity fracture, and (3) persons with multiple fractures (more than one site-specific fracture on a unique day in the study-eligible time period). For men with multiple fractures within the 6-year study window, baseline characteristics are presented for the persons’ first fracture. Mortality is calculated from the last incident fracture.
Shapiro-Wilk and Kolmogorov-Smirnov tests for normality were performed across each of the three fracture groups (single upper, single lower, and multiple fractures) for the continuous variables age, Charlson comorbidity index, and duration of injury. Bivariate analyses of baseline characteristics were analyzed using χ2 tests (or Fisher's exact test) for categorical variables, ANOVA for continuous variables that met the assumptions for normality, and Kruskal-Wallis for continuous variables that did not meet normality assumptions.
The Bonferonni correction was used to address the multiple testing among the 6 variables examined (age, race/ethnicity, level, extent, and duration of SCI and the Charlson comorbidity index). Statistical significance was set at the 0.0083 (0.05/6) level. All analyses were done using SAS v9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
Within the VA SCD Registry, there were 12,162 male veterans and 296 female veterans with a traumatic SCI of at least two years’ duration identified from fiscal years 2002–2007. There were 1,979 non-E-coded extremity fractures in 1,281 men. The majority of fractures in men, 1,634 (82.6%), occurred at lower extremity sites; 345 (17.4%) fractures occurred at upper extremity sites. There were 34 women (11.5% of women) identified with 58 incident fractures (2.8% of all fractures); among them, there were 14 upper extremity fractures (24.1%) and 44 lower extremity fractures (75.9%). There was no significant difference in the frequency of incident fractures between men and women (10.5% vs 11.5%, respectively, P = 0.60) and no difference in distribution of upper and lower extremity fracture sites based on sex (P = 0.33). The distribution of specific fracture sites among men and women are shown in Table 2. Over 1/3 of men in the cohort sustained multiple incident fractures on unique days over the six-year observation period (Fig. 1). Additionally, 48 E-coded fractures due to non-specific falls were identified.
Table 2.
Overall distribution of fracture sites by sex
| Fracture Site | Men n (%) | Women n (%) |
|---|---|---|
| Upper Extremity | 345 (17.4) | 14 (24.1) |
| Scapula | 3 (0.9) | 0 (0.0) |
| Clavicle | 38 (11) | 1 (2.9) |
| Humerus | 96 (27.8) | 3 (8.8) |
| Forearm | 55 (15.9) | 2 (5.9) |
| Carpal | 42 (12.2) | 0 (0.0) |
| Metacarpal | 59 (17.1) | 4 (11.8) |
| Phalanges of Hand | 51 (14.8) | 1 (2.9) |
| Multiple Hand | 1 (0.0) | 0 (0.0) |
| Lower Extremity | 1634 (82.6) | 44 (75.9) |
| Pelvis | 39 (0.1) | 0 (0.0) |
| All Hip | 253 (15.2) | 1 (2.94) |
| Femoral Neck | 169 (10.1) | 0 (0.0) |
| Trochanteric | 18 (1.1) | 0 (0.0) |
| Intertrochanteric | 10 (0.6) | 0 (0.0) |
| Subtrochanteric | 56 (3.4) | 1 (2.9) |
| Femur | 419 (25.1) | 4 (11.8) |
| Patella | 26 (1.6) | 1 (2.9) |
| Tibia/Fibula | 542 (32.5) | 9 (26.5) |
| Ankle | 206 (12.4) | 5 (14.7) |
| Tarsal/Metatarsal | 105 (6.3) | 2 (5.9) |
| Phalanges of Foot | 44 (2.6) | 1 (2.9) |
| All Fractures | 1979 (100.0) | 58 (100.0) |
Figure 1.
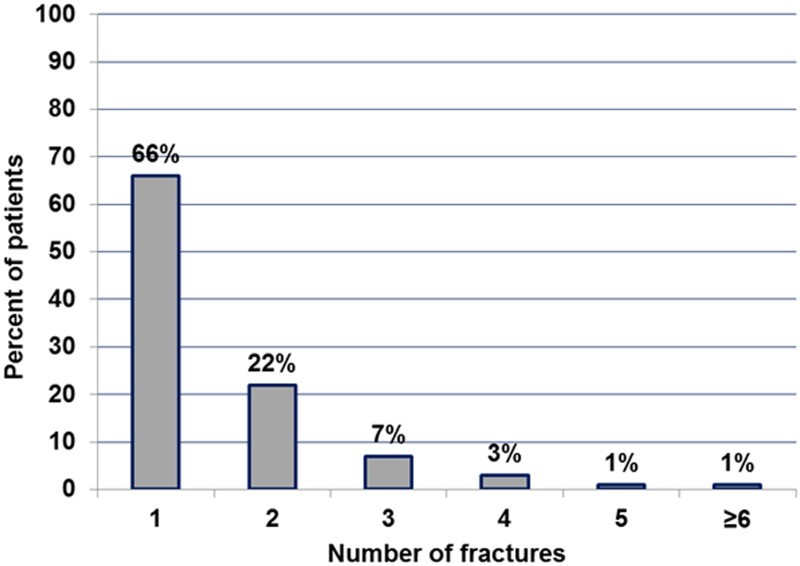
Percentage of men with single and multiple fractures.
The derivation of the final analytic sample is shown in Fig. 2. Descriptive statistics for men in the cohort by fracture group (single upper extremity, single lower extremity, multiple fractures) are shown in Table 3. There were no significant differences in age, race/ethnicity, and duration of SCI based upon the fracture group (Table 3). There were significant differences between the fracture groups based on level and extent of SCI as well as the Charlson comorbidity indices (Table 3). Among men with a known level and extent of injury, upper extremity fractures were more common in those with tetraplegia and incomplete injuries; lower extremity fractures were more common in those with complete injuries. Charlson comorbidity indices were higher among men with single upper extremity fractures. When comparing all men with single site-specific fractures to men with multiple fractures, there were no significant differences in age (P = 0.93), race/ethnicity (P=0.62), level (P=0.12), extent (P=0.88), or duration (P=0.26) of SCI, as well as Charlson comorbidity indices (0.94 vs 0.73, P=0.04, data not shown).
Figure 2.
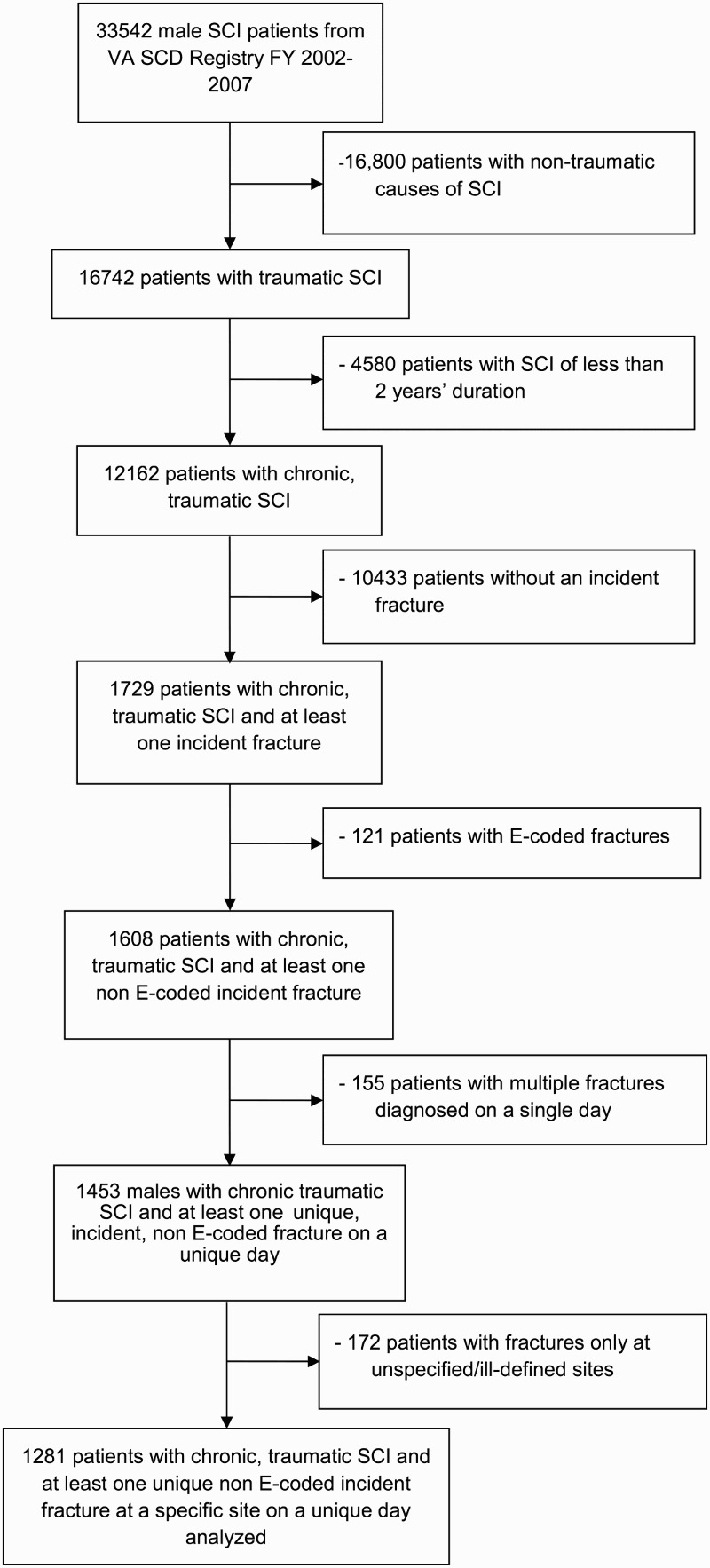
Derivation of final analytic sample.
Table 3.
Baseline characteristics of male veterans by fracture group
| Characteristic |
Fracture Group |
P-valuea | ||
|---|---|---|---|---|
| Single Upper Extremity (n = 183) | Single Lower Extremity (n = 664) | Multiple Fractures (n = 434) | ||
| Age (years), mean ± sd | 56.2 ± 12.3 | 56.6 ± 12.3 | 56.5 ± 11.6 | 0.84 |
| Race/ethnicity, n (%) | - | - | - | 0.94 |
| White | 106 (57.9) | 387 (58.3) | 262 (60.4) | - |
| Black | 21 (11.5) | 76 (11.4) | 41 (9.4) | - |
| Other | 1 (0.5) | 4 (0.6) | 4 (0.9) | - |
| Missing | 55 (30.1) | 197 (29.7) | 127 (29.3) | - |
| Level of Injuryb, n (%) | - | - | - | <0.001 |
| Paraplegia | 75 (41.0) | 381 (57.4) | 255 (58.8) | - |
| Tetraplegia | 77 (42.1) | 252 (38.0) | 143 (32.9) | - |
| Unknown | 31 (16.9) | 31 (4.7) | 36 (8.3) | - |
| Extent of Injuryc, n (%) | - | - | - | <0.001 |
| Complete | 29 (15.4) | 287 (43.2) | 168 (38.7) | - |
| Incomplete | 102 (55.7) | 246 (37.0) | 175 (40.3) | - |
| Missing | 52 (28.4) | 131 (19.7) | 91 (21.0) | - |
| Duration of Injury (years), mean ± sd | 21.0 ± 13.1 | 24.1 ± 14.2 | 24.4 ± 13.5 | 0.01 |
| Charlson Comorbidity Index,d mean ± sd | 1.2 ± 2.0 | 0.87 ± 1.9 | 0.73 ± 1.5 | 0.007 |
aANOVA for normally distributed continuous variables, Kruskal-Wallis for continuous variables not meeting normality assumptions, and χ2/Fisher's exact test for categorical variables. Due to multiple comparisons, statistical significance was set to P < 0.0083.
bAmong men with incident fracture, 711 (55.5%) of men had paraplegia, 472 (36.8%) had an incomplete injury, and information on level of injury was missing for 98 (7.6%) patients.
cAmong men with incident fracture, 484 (37.8%) of men had a complete injury, 523 (40.8%) had an incomplete injury, and information on extent of injury was missing for 274 (21.4%) patients.
dDoes not include index component for paraplegia/tetraplegia.
Complete injury (compared to incomplete) was associated with an additional 41% risk of appendicular fracture in men with tetraplegia (relative risk (RR) = 1.41 95% CI = [1.17, 1.70]); however, among men with paraplegia, there was no increase in the RR of fracture with having a complete injury (RR = 1.01 95%CI = [0.87, 1.18]).
There were few (n = 48) E-coded fractures for non-specific falls. Most commonly, non-specific falls resulted in fractures of the tibia/fibula (data not shown).
There were 63 (7.4%) deaths among men with a single site-specific fractures and 31 (7.1%) in those with multiple fractures, a difference which was also not significant (P=0.94).
Discussion
Male veterans with chronic traumatic SCI had a substantial number of appendicular fractures; female veterans, who represented a small minority of the population of interest, sustained fractures at a similar frequency. Among men, there were significant differences in the number and sites of fractures based on the extent and level of SCI as well as the presence of other comorbid conditions. Over one-third of men in this cohort had multiple incident fractures over the 6-year time period of this study; multiple fractures were not associated with SCI-related factors (i.e. duration, level, or extent of SCI), age, race/ethnicity, or Charlson comorbidity indices.
In the current study, men and women appeared to sustain fractures at a similar frequency. In a Danish study comparing non-veteran men and women with SCI, women were found to have a higher relative risk of fracture compared to men15; however, this was a cross-sectional study that included more women (n = 322 vs n = 34), included individuals with nontraumatic SCI and fractures were ascertained by self-report, which may account for the differences. The findings that the majority of fractures occurred in the lower extremities for both men and women are in accord with the overall distribution of fractures reported in previous studies.8,15–19 The most common fracture site within the lower extremity among both men and women was the tibia/fibula. This observation is in agreement with two prior studies16,20 but is in contrast to other reports which found supracondylar femur fractures,18,21 femur fractures,15 or fractures about the hip19 to be most common, although tibial fractures are often second in prevalence.22 Clinical studies following a SCI indicate that bone loss severity progresses caudally, such that the loss of bone in the tibia is greater than in the femur,22,23 which is consistent with the findings of this study. That the frequency of upper and lower extremity fractures was similar between men and women differs from a prior report that upper extremity fractures (“arm” fractures) were more common in men.24
Single upper extremity fractures were more common in men with tetraplegia, incomplete injuries, and in men with higher Charlson comorbidity indices. The association of higher Charlson comorbidity index with upper extremity fractures is in agreement with a previous report from the non-SCI literature in nonambulatory persons on dialysis that found fractures in general to be more common in those with higher Charlson comorbidities.25 The finding that tetraplegia was associated with a higher percentage of upper extremity fractures is not surprising as only those with tetraplegia have upper extremity involvement and bone density is lower in these persons who are unable to use these limbs for exercise.26 The reasons why upper extremity fractures were more common with incomplete injuries are not clear.
A complete extent of injury was associated with an increased relative risk of fracture, but only in those with tetraplegia. This finding is in accord several prior studies showing an association with between motor and sensory complete SCI and fracture incidence.27,28 The lack of this association in those with paraplegia may be due to the fact that complete injuries are more common in paraplegia.29
Our finding of substantial numbers of additional fractures over time (more than 1/3 of the population) in male veterans with a SCI is similar to several historical reports with very small sample sizes17,30 and a more recent report finding that 34.6% of individuals with traumatic SCI sustained two or more fractures over an 11-year time period.16 The findings that age was not associated with multiple fractures is in agreement with a cross-sectional study of persons with traumatic SCI31 and extends these findings to suggest that race/ethnicity and higher burden of comorbid disease are also not associated with multiple incident fractures. While duration of injury was not associated with multiple fractures in the current study, one previous report suggested that longer duration of SCI is associated with multiple fractures over time.31 Multiple fractures were more common in those with paraplegia and persons with paraplegia may be at increased risk of osteoporosis (and thus fracture) compared to persons with tetraplegia because they are more likely to have lower motor neuron injuries and greater muscle atrophy.23
There was no increased mortality for men with additional fractures over time compared to those with single fractures. This is in contrast to the non-SCI literature, which reported an increased risk of mortality, especially for men, if an additional fracture was sustained following a first osteoporotic fracture.32
Study limitations
There were several limitations to this study. A large number of fractures occurring at unspecified and ill-defined sites were excluded (485 of 2,464 fractures initially identified in the cohort, 19.7%); the effect of this is not known. Although data on age was missing for less than 1% of persons, there was a high frequency of missing data for race/ethnicity, level, and extent of injury; however, sensitivity analyses of the SCI Registry have shown that those with missing information do not differ significantly across any of the other covariates. Further, since ICD-9 codes and not direct physician documented chart data were used to identify comorbid conditions for the Charlson comorbidity index, it is possible that important comorbid conditions were not included as an ICD-9 code. This may have underestimated the association of comorbid conditions with mortality among those with multiple fractures. Those missing duration of injury and those with a duration of injury of less than two years were excluded from the analyses. This is a limitation because longer duration of injury is an important predictor of both lower BMD33 and impaired bone strength.34 It is possible that the epidemiology of fractures differs in those with an acute SCI (< 2 years duration) from what is reported here. The cohort included was from FY2002–2007 and the current composition of the Veteran population with SCI in VHA may be different due in part to an influx of new SCI injuries from conflicts in Iraq and Afghanistan, an increase in the number of women in the military, and the aging of veterans35; therefore, the findings described here may not accurately describe fractures in this population as it exists today. E-codes are a subset of the ICD-9 classification system that further describe an injury as due to an external cause (the major ones include accidents, poisoning and adverse effects of drugs, accidental falls, late effects of accidents, self-injuries, assaults, or suicide). For the purposes of this study, only E-codes from non-specific falls were included. However, in this administrative database it is possible that some of the E-coded fractures were misclassified.36 ASIA scores were not uniformly recorded in the time period of the study and thus were not included. Based on our previous work,37 the development of HO following an incident fracture was exceedingly rare, therefore, we did not examine the association of HO with incident fracture. BMD was not included; it has been reported that low BMD is a predictor of the number of fractures in SCI.31,38 Physical therapy modalities, such as functional electrical stimulation,39 standing frames,40 and body-weight-supported treadmill training,41 have potential effects on osteoporosis and muscle changes after spinal cord injury; there was no information on the use of these devices or modalities. Finally, at present, the power of the study to detect differences in mortality rates is only 5.4%. The sample size in the study would have been sufficient in detecting a small effect size (h = 0.17) between mortality rates in persons with single fracture vs. those with multiple fractures. To detect the extremely small effect size observed in this study (h = 0.01), 35,000 persons with fracture would have needed to be observed.
There are also important strengths to this study. First, this is the largest series to date to examine the frequency and distribution of fractures in persons with chronic SCI. Furthermore, it includes information on the substantial frequency of additional fractures occurring following an initial fracture.
Conclusions
In male veterans with chronic traumatic SCI and tetraplegia, a complete extent of injury significantly raises the risk of fracture. Multiple fractures are common in male veterans, but do not appear to increase mortality in the short term. However, the contribution of multiple fractures to excess morbidity and long term mortality in this population should be addressed in future studies. There were few female veterans with chronic traumatic SCI who sustained incident fractures in the time period examined and their observed fracture percentage was similar to males with SCI.
ORCID
Laura D. Carbone http://orcid.org/0000-0003-3370-4680
Disclaimer statements
Contributors None.
Funding This work was supported in part with funding from the Veterans Health Administration (VA Merit Review IIR 11-103-3) and the Rheumatology Research Foundation (Ephraim P. Engleman Resident Preceptorship Award).
Conflict of interest All authors report no conflicts of interest.
Ethics approval None.
Acknowledgments
The content does not reflect the views of the Veterans Health Administration or the United States government.
References
- 1.National Spinal Cord Injury Statistical C Spinal cord injury facts and figures at a glance 2012 [cited 2013 July 30]. Available from: https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202012%20Feb%20Final.pdf.
- 2.Selvarajah S, Hammond ER, Haider AH, Abularrage CJ, Becker D, Dhiman N, et al. The burden of acute traumatic spinal cord injury among adults in the United States: an update. J Neurotrauma 2014;31(3):228–38. doi: 10.1089/neu.2013.3098 [DOI] [PubMed] [Google Scholar]
- 3.Jiang SD, Dai LY, Jiang LS. Osteoporosis after spinal cord injury. Osteoporos Int 2006;17(2):180–92. doi: 10.1007/s00198-005-2028-8 [DOI] [PubMed] [Google Scholar]
- 4.Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. J Am Acad Orthop Surg 2009;17(11):689–97. [DOI] [PubMed] [Google Scholar]
- 5.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Morbidity following lower extremity fractures in men with spinal cord injury. Osteoporos Int 2013;24(8):2261–7. doi: 10.1007/s00198-013-2295-8 [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Islam N, Carbonell RG, Rojas OJ. Specific binding of immunoglobulin G with bioactive short peptides supported on antifouling copolymer layers for detection in quartz crystal microgravimetry and surface plasmon resonance. Anal Chem 2013;85(2):1106–13. doi: 10.1021/ac302874s [DOI] [PubMed] [Google Scholar]
- 7.Smith BM, Evans CT, Ullrich P, Burns S, Guihan M, Miskevics S, et al. Using VA data for research in persons with spinal cord injuries and disorders: lessons from SCI QUERI. J Rehabil Res Dev 2010;47(8):679–88. doi: 10.1682/JRRD.2009.08.0117 [DOI] [PubMed] [Google Scholar]
- 8.Logan WC Jr., Sloane R, Lyles KW, Goldstein B, Hoenig HM. Incidence of fractures in a cohort of veterans with chronic multiple sclerosis or traumatic spinal cord injury. Arch Phys Med Rehabil 2008;89(2):237–43. doi: 10.1016/j.apmr.2007.08.144 [DOI] [PubMed] [Google Scholar]
- 9.Garland DE, Stewart CA, Adkins RH, Hu SS, Rosen C, Liotta FJ, et al. Osteoporosis after spinal cord injury. J Orthop Res 1992;10(3):371–8. doi: 10.1002/jor.1100100309 [DOI] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 11.National Center for Health S The International Classification of Diseases: 9th Revision, Clinical Modification: ICD-9-CM: US Department of Health and Human Services Public Health Service Health Care Financing Administration; 1989.
- 12.Merion M. Assigning E Codes for external causes King of Prussia, PA: Merion Matters; 2007 [updated April 13, 2007 February 20, 2014]. Available from: http://health-information.advanceweb.com/Article/Assigning-E-Codes-for-External-Causes-1.aspx.
- 13.National Center for Health Statistics National death index (1981).
- 14.Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr 2006;4:2. doi: 10.1186/1478-7954-4-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vestergaard P, Krogh K, Rejnmark L, Mosekilde L. Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 1998;36(11):790–6. doi: 10.1038/sj.sc.3100648 [DOI] [PubMed] [Google Scholar]
- 16.Frotzler A, Cheikh-Sarraf B, Pourtehrani M, Krebs J, Lippuner K. Long-bone fractures in persons with spinal cord injury. Spinal Cord 2015;53(9):701–4. [DOI] [PubMed] [Google Scholar]
- 17.Freehafer AA, Mast WA. Lower extremity fractures in patients with spinal-cord injury. J Bone Joint Surg Am 1965;47:683–94. [PubMed] [Google Scholar]
- 18.Comarr AE, Hutchinson RH, Bors E. Extremity fractures of patients with spinal cord injuries. Am J Surg 1962;103:732–9. doi: 10.1016/0002-9610(62)90256-8 [DOI] [PubMed] [Google Scholar]
- 19.Nottage WM. A review of long-bone fractures in patients with spinal cord injuries. Clin Orthop Relat Res 1981;155:65–70. [PubMed] [Google Scholar]
- 20.Akhigbe T, Chin AS, Svircev JN, Hoenig H, Burns SP, Weaver FM, et al. A retrospective review of lower extremity fracture care in patients with spinal cord injury. J Spinal Cord Med 2015;38(1):2–9. doi: 10.1179/2045772313Y.0000000156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cochran TP, Bayley JC, Smith M. Lower extremity fractures in paraplegics: pattern, treatment, and functional results. J Spinal Disord 1988;1(3):219–23. doi: 10.1097/00002517-198803000-00007 [DOI] [PubMed] [Google Scholar]
- 22.Dauty M, Perrouin Verbe B, Maugars Y, Dubois C, Mathe J. Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone 2000;27(2):305–9. doi: 10.1016/S8756-3282(00)00326-4 [DOI] [PubMed] [Google Scholar]
- 23.Eser P, Frotzler A, Zehnder Y, Wick L, Knecht H, Denoth J, et al. Relationship between the duration of paralysis and bone structure: a pQCT study of spinal cord injured individuals. Bone 2004;34(5):869–80. doi: 10.1016/j.bone.2004.01.001 [DOI] [PubMed] [Google Scholar]
- 24.Shackelford M, Farley T, Vines CL. A comparison of women and men with spinal cord injury. Spinal Cord 1998;36(5):337–9. doi: 10.1038/sj.sc.3100510 [DOI] [PubMed] [Google Scholar]
- 25.Ma MKM, Yap DYH, Yip TPS, Lui SL, Lo WK. Charlson Co-morbidity Index and albumin significantly associated with fracture risk in peritoneal dialysis patients. Nephrology 2013;18(5):365–8. doi: 10.1111/nep.12056 [DOI] [PubMed] [Google Scholar]
- 26.Jones LM, Legge M, Goulding A. Intensive exercise may preserve bone mass of the upper limbs in spinal cord injured males but does not retard demineralisation of the lower body. Spinal Cord 2002;40(5):230–5. doi: 10.1038/sj.sc.3101286 [DOI] [PubMed] [Google Scholar]
- 27.Gifre L, Vidal J, Carrasco J, Portell E, Puig J, Monegal A, et al. Incidence of skeletal fractures after traumatic spinal cord injury: a 10-year follow-up study. Clin Rehabil 2014;28(4):361–9. doi: 10.1177/0269215513501905 [DOI] [PubMed] [Google Scholar]
- 28.Pelletier C, Dumont F, Leblond J, Noreau L, Giangregorio L, Craven B. Self-report of one-year fracture incidence and osteoporosis prevalence in a community cohort of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil 2014;20(4):302–9. doi: 10.1310/sci2004-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman WP, Geisler FH. Injury severity as primary predictor of outcome in acute spinal cord injury: retrospective results from a large multicenter clinical trial. Spine J 2004;4(4):373–8. doi: 10.1016/j.spinee.2003.12.006 [DOI] [PubMed] [Google Scholar]
- 30.Freehafer AA, Hazel CM, Becker CL. Lower extremity fractures in patients with spinal cord injury. Paraplegia 1981;19(6):367–72. doi: 10.1038/sc.1981.69 [DOI] [PubMed] [Google Scholar]
- 31.Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M. Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 2001;39(4):208. doi: 10.1038/sj.sc.3101139 [DOI] [PubMed] [Google Scholar]
- 32.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009;301(5):513–21. doi: 10.1001/jama.2009.50 [DOI] [PubMed] [Google Scholar]
- 33.Hammond ER, Metcalf HM, McDonald JW, Sadowsky CL. Bone mass in individuals with chronic spinal cord injury: associations with activity-based therapy, neurologic and functional status, a retrospective study. Arch Phys Med Rehabil 2014;95(12):2342–9. doi: 10.1016/j.apmr.2014.07.395 [DOI] [PubMed] [Google Scholar]
- 34.Edwards WB, Simonian N, Troy KL, Schnitzer TJ. Reduction in torsional stiffness and strength at the proximal tibia as a function of time since spinal cord injury. J Bone Min Res 2015;30(8):1422–30. doi: 10.1002/jbmr.2474 [DOI] [PubMed] [Google Scholar]
- 35.Curtin CM, Suarez PA, Di Ponio LA, Frayne SM. Who are the women and men in Veterans Health Administration's current spinal cord injury population? J Rehabil Res Dev 2012;49(3):351–60. doi: 10.1682/JRRD.2010.11.0220 [DOI] [PubMed] [Google Scholar]
- 36.Schwartz RJ, Nightingale BS, Boisoneau D, Jacobs LM. Accuracy of e-codes assigned to emergency department records. Acad Emerg Med 1995;2(7):615–20. doi: 10.1111/j.1553-2712.1995.tb03599.x [DOI] [PubMed] [Google Scholar]
- 37.Bethel M, Bailey L, Weaver F, Le B, Burns SP, Svircev JN, et al. Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury. Spinal Cord 2015;53(5):402–7. doi: 10.1038/sc.2015.5 [DOI] [PubMed] [Google Scholar]
- 38.Zehnder Y, Luthi M, Michel D, Knecht H, Perrelet R, Neto I, et al. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int 2004;15(3):180–9. doi: 10.1007/s00198-003-1529-6 [DOI] [PubMed] [Google Scholar]
- 39.Hammond ER, Metcalf HM, McDonald JW, Sadowsky CL. Bone mass in individuals with chronic spinal cord injury: associations with activity-based therapy, neurologic and functional status, a retrospective study. Arch Phys Med Rehabil 2014;95(12):2342–9. doi: 10.1016/j.apmr.2014.07.395 [DOI] [PubMed] [Google Scholar]
- 40.Masani K, Alizadeh-Meghrazi M, Sayenko DG, Zariffa J, Moore C, Giangregorio L, et al. Muscle activity, cross-sectional area, and density following passive standing and whole body vibration: A case series. J Spinal Cord Med 2014;37(5):575–81. doi: 10.1179/2045772314Y.0000000255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coupaud S, Jack L, Hunt K, McLean A, Allan D. Muscle and bone adaptations after treadmill training in incomplete spinal cord injury: a case study using peripheral quantitative computed tomography. J Musculoskelet Neuronal Interact 2009;9(4):288–97. [PubMed] [Google Scholar]


