Abstract
The STAT3 is often dysregulated in genitourinary tumors. In prostate cancer, STAT3 activation correlates with Gleason score and pathological stage and modulates cancer stem cells and epithelial–mesenchymal transition. In addition, STAT3 promotes the progression from carcinoma in situ to invasive bladder cancer and modulates renal cell carcinoma angiogenesis by increasing the expression of HIF1α and VEGF. STAT3 is also involved in the response to tyrosine kinase inhibitors sunitinib and axitinib, in patients with metastatic renal cell carcinoma, and to second-generation androgen receptor inhibitor enzalutamide in patients with advanced prostate cancer. In this review, we describe the role of STAT3 in genitourinary tumors, thus describing its potential for future therapeutic strategies.
Keywords: : drug resistance, genitourinary tumors, metastasis, signal transducer and activator of transcription 3, tumor microenvironment
Regulation of the protein STAT3 is often dysfunctional in genitourinary tumors, including prostate, bladder and kidney cancer. STAT3 is involved in the generation of these tumors and has an effect in their response to treatments. In this review, we describe its role in genitourinary tumors and discuss its potential for use in future therapies.
The STAT proteins are involved in mediating cellular responses to cytokines [1]. STAT family includes seven members (STAT1, STAT2, STAT3, STAT4, STAT5A, STAT5B and STAT6). Among them, STAT3 plays a prominent role in tumor growth and invasion [2]. STAT3 was discovered as an acute phase response factor, due to its ability to increase the expression of liver proteins in response to stress [3]. STAT3 activation (pSTAT3) is determined by the phosphorylation of the tyrosine residue at position 705 by JAK [4]. Once activated, pSTAT3 forms dimers, translocates into the nucleus, and binds to STAT-specific DNA-response elements, called gamma-activated sites to promote the transcription of selected genes.
STAT3 presents three alternative splice isoforms: the isoform 1 or α (producing a 770 aminoacids protein), the isoform 2 (lacking aminoacid 701) and the isoform 3 or β (lacking AAs 723–770 and with a shift from TTCSNTI to FIDAVWK, corresponding to aminoacids 716–722). STAT3α is the more frequent isoform expressed in human carcinomas and is involved in tumor development and metastasis. Otherwise, the β isoform seems to inhibit the transcriptional activation due to α isoform, resulting in tumor growth inhibition [5,6].
The list of STAT3 activators includes IL-6, EGF, S1P, inflammatory OSM, Src family members and growth factor receptors that possess intrinsic tyrosine-kinase activity, such EGFRs, HGF receptor (also known as c-Met) and PDGFR [7–10].
Deregulation of STAT3 signaling has been reported in several solid tumors, including breast [11], head and neck [12], prostate, renal, bladder, pancreas, ovarian and brain cancers and melanoma [13–19]. This review summarizes recent findings on the role of STAT3 in tumor initiation, progression and angiogenesis, focusing on genitourinary tumors.
Role of STAT3 signaling in cancer
STAT3 acts as transcriptional regulator of a variety of tumor-promoting genes. Persistent STAT3 activation may be due to the loss of suppressors of cytokine signaling and protein tyrosine phosphatases expression, as well as to autocrine or paracrine inflammatory stimulation in the tumor microenvironment.
STAT3 activation alone is sufficient to induce cell transformation, showing a strong oncogenic potential and promotes the maintenance of a procarcinogenic inflammatory microenvironment during cancer initiation and progression [20–22]. In addition, STAT3 inhibition has been shown to suppress tumor growth and enhance the sensitivity to drugs in a variety of solid tumors [23,24].
The list of STAT3 target genes includes VEGF, Bcl2, c-myc, cyclin D1, Survivin and WASF3, a member of the WASP/WASF family, which are involved in tumor development and progression [25–29]. WASF3 regulates cell motility by modulating actin cytoskeleton dynamics [66] and promotes invasion through the activation of NFκB and ZEB1 [30]. Furthermore, STAT3 promotes carcinogenesis through the chaperone protein aging-associated gene 8 protein, which contributes to endoplasmic reticulum-associated degradation and promotes carcinogenesis both in vitro and in vivo [31].
The epithelial–mesenchymal transition (EMT) is a process by which epithelial cells transdifferentiate into motile mesenchymal cells. Inappropriate activation of embryonic EMT programs in cancer cells promotes cell plasticity and invasion [32]. Moreover, EMT is implicated in the acquisition of stem cell-like and chemoresistant phenotypes by tumor cells [33]. Interestingly, STAT3 promotes cancer invasion also by modulating EMT [34]. Indeed, STAT3 regulates the expression of transcriptional factors driving EMT and modulates cytoskeleton dynamics during the initiation of the EMT process [34].
Recent studies have revealed persistent STAT3 activation in myeloid and T cells at primary tumor sites contribute to tumor-related immunosuppression, angiogenesis, growth and metastasis [35–39]. In addition, STAT3 signaling plays a crucial role also in other types of stromal cells, such as fibroblasts and endothelial cells, in initiating premetastatic niche formation [40].
Role of STAT3 signaling in prostate cancer
Prostate cancer (PCa) is one of the leading causes of death among men. In the last years, major advances have been made in understanding the genetic mechanisms underlying PCa. STAT3 plays a crucial role in prostate carcinogenesis [41,42], as sustained by the evidence that STAT3 knockdown is associated with inhibited tumor growth in preclinical models [43]. STAT3 signaling is involved in modulating PCa cell survival. Indeed, STAT3 is required for the activation of antiapoptotic proto-oncogenes, such as Bcl-2 and Bcl-3 [44–46] and for the modulation of androgen receptor (AR) expression and activity [47]. Furthermore, in vitro studies showed that STAT3 activation is higher in androgen-insensitive DU145 and PC3 cell lines compared with androgen-sensitive LNCaP cells [48], suggesting for a role of this pathway in the modulation of AR activity [48].
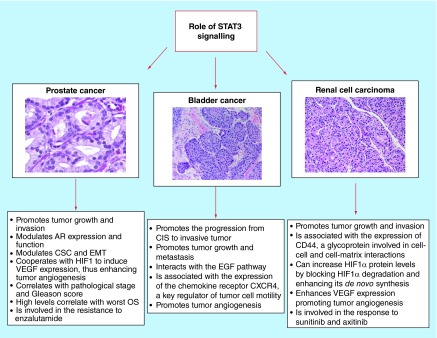
The role of STAT3 signaling in modulating prostate cancer stem cells (PCSCs), EMT and tumor angiogenesis has only recently been investigated (Figure 1). PCSCs have been found in both prostate [49] and PCa. Their presence is associated with high STAT3 activity, low AR expression, higher potential to metastasize and with poor patient outcome [50]. It has been shown that treatment with LLL12, a STAT3 inhibitor, abrogates the propagating of PCSCs in vivo [51]. Furthermore, STAT3 knockdown inhibits sphere formation derived from human PCa cells [43] The crucial role of STAT3 in PCSCs may be explained by its role in the IL-6 signaling, as sustained by the notion that soluble IL-6 receptor fusion protein can significantly reduce CSC number and xenograft tumor growth in in vivo PCa models [43].
Figure 1. . Role of STAT3 in genitourinary tumors.
AR: Androgen receptor; CIS: Carcinoma in situ; CSC: Cancer stem cell; EMT: Epithelial–mesenchymal transition; OS: Overall survival.
STAT3 activators IL-6 and CCL2 chemokine have been shown to play a role in modulating EMT in PCa. The EGF is also involved in EMT programs. The activity of EGF is mediated by several pathways, including STAT3, hypoxia inducible factor (HIF)1α and TWIST1 [52]. TWIST1 is a highly conserved transcription factor that belongs to the basic helix–loop–helix family [53] and represents a key step during PCa development and metastasis due to its role in EMT [54,55]. Notably, TGF-β1 has been shown to upregulate TWIST1, as well as to promote STAT3 activation and HIF1α stabilization, thus contributing to PCa EMT and metastasization [55].
Interestingly, STAT3 is also implicated in promoting PCa angiogenesis [56]. Indeed, STAT3 is required for VEGF signaling [57]. The relationship between STAT3 and AR in PCa is crucial in modulating VEGF transcription, may be due to the presence of AR-binding sites in the promoter of VEGF gene [58]. Moreover, STAT3-induced HIF1α transcription, which cooperates with STAT3 to induce VEGF expression [59].
Activated STAT3 signaling is associated with the clinicopathologic characteristics of PCa, such as high pathological stage and Gleason score [60,61]. In addition, the expression levels of STAT3 activator IL-6 are increased in patients with metastatic PCa compared with patients with nonmalignant diseases [62–64].
STAT3 activation negatively correlated with overall survival (OS) in PCa patients from biochemical relapse [61] and in castration-resistant PCa patients [65]. Furthermore, activated STAT3 is associated with shorter recurrence-free survival in patients who undergo radical prostatectomy or hormonal therapy [61].
Interestingly, STAT3 is involved in the development of drug resistance in patients with PCa. Enzalutamide is a second-generation AR inhibitor. Enzalutamide has been showed to increase the OS of patients with metastatic PCa both in chemo-naive [66] and in patients pretreated with chemotherapy [67]. The identification of the mechanisms underlying primary and acquired resistance to this agent represents a major challenge for uro-oncologists. Antonarakis et al. reported that the presence of AR isoform encoded by splice variant 7 (AR-V7), which is constitutively activated but lacks of the ligand-binding domain targetable by abiraterone and enzalutamide, was associated with drug resistance in 62 patients treated with one of these two agents [68]. In addition, the downregulation of STAT3 seems to reverse the resistance to enzalutamide in PCa cells. Thus, the combination of STAT3 inhibitor AG490 and enzalutamide significantly inhibited tumor growth and induced cell apoptosis [69].
Furthermore, the inhibition of STAT3 signaling using small-molecule inhibitor Stattic has been shown to target both tumor-initiating cells (TICs) and differentiated cells. In this study, STAT3 inhibition caused S-phase accumulation at low-dose levels and massive apoptosis at a relatively high-dose level in PCa cells. STAT3 knockdown led to the disruption of the microvascular niche which TICs and non-TICs depend on. Thus, STAT3 inhibition is predicted to have greater efficacy for PCa treatment [70].
Role of STAT3 signaling in bladder cancer
Bladder cancer (BC) is the fourth most frequent cancer in men in developed countries [71]. Two main distinct forms based on the infiltration of the muscularis propria have been described: nonmuscle invasive tumors and muscle-invasive bladder carcinomas, the latter being characterized by easy access to lymphatics and blood vessels for metastatic dissemination. In addition, low-grade or high-grade tumors can be described, characterized by different biological and clinical behaviors.
In the last years, major advances have been made in understanding the genetic mechanisms underlying BC. FGFR3 or p53 mutations seems to be mutually exclusive in urothelial carcinoma pathogenesis. In particular, FGFR3 gene mutations selectively occur in noninvasive (pTa) BC, while p53 mutations are rare (less than 5%) and are associated with high-grade tumors and invasive (pT1 or more) BC [72]. Generally, papillary pTa urothelial carcinomas show genetic stability, due to the absence of p53 inactivation, with chromosomal changes concerning only chromosome 9.
STAT3 has been implicated in the progression from carcinoma in situ to invasive BC. In particular, STAT3 signaling acts as an important downstream mediator of inflammatory cytokines, such as IL-6 and IL-17, which are released during bladder tumorigenesis due to chronic inflammation (i.e., smoking, persistent urinary tract infections) [73]. Moreover, early expansion of primitive CK14+ expressing cells, driven by STAT3 and other pathways, leads to transition to carcinoma in situ-invasive pathway [74] (Figure 1).
Zhang et al. investigated the inhibitory effects of STAT3 silencing on human T24 BC cells in in vitro and in vivo models. In this study, the downregulation of STAT3 or Survivin, an inhibitor of apoptosis, suppressed the proliferation of BC cells. Moreover, no additive effects were recorded by the STAT3 and Survivin joined knockdown, suggesting that they both belong to the same pathway in T24 cells [75].
CDC91L1, also called phosphatidylinositol glycan class U, is an oncogene overexpressed in BC and is an independent predictor of recurrence for nonmuscle invasive tumors. Cell division cycle 91-like 1 is activated by a chromosomal translocation and leads to persistent STAT3 activation [76].
EGF and its receptor EGFR are overexpressed in BC. In particular, EGFR expression is limited to the basal cell layer in the healthy urothelium, while it is expressed in both deep and superficial cell layers in both low- and high-grade BCs [77]. In response to EGF, STAT3 becomes activated and induces MMP-1 transcription by interacting with c-JUN, a component of the transcription factor activator protein-1 [78]. Interestingly, MMP-1 expression correlates with tumor high grade and invasiveness, thus suggesting that STAT3 activation is directly related to malignant behavior of T24 BC cells [79].
The establishment of a proangiogenic tumor environment is the consequence of a deregulated high expression of proangiogenic factors or an inadequate inhibition of angiostatic factors. Among the receptors for CXC chemokines, CXCR4, a receptor for CXC chemokine CXCL12/SDF-1, is involved in the maintenance of leukocyte trafficking during homeostasis and is key regulator of cell motility in BC. In the study led by Shen et al., higher CXCR4 expression correlated with STAT3 phosphorylation. In addition, STAT3 inhibitor Stattic inhibited CXCL12-triggered STAT3 phosphorylation and, consequently, cell motility and invasion in T24 BC cells [79].
Role of STAT3 signaling in renal cell carcinoma
Renal cell carcinoma (RCC) is one of the most lethal urologic cancers [80]. In the last decade, a better understanding of the role of VEGF and mammalian target of rapamycin pathways has led to the introduction of several agents to the therapeutic landscape of metastatic RCC. Nevertheless, the rate of complete responses is still low [81], and alternative targets should be investigated in in vitro and in vivo studies.
STAT3 is involved in RCC carcinogenesis, growth and tumor angiogenesis (Figure 1). Masuda et al. quantified STAT3 and p53 mRNA expressions in a series of 47 Japanese patients with RCC. They found that the levels of STAT3 and p53 mRNA expressions were lower in tumor tissues compared with nontumor tissues and did not correlate with RCC histology and stage [82]. On the other hand, Guo et al. investigated the immunoprofile of phosphorylated STAT3 in a series of 88 RCCs with different histologies and 21 normal renal tissues. They reported that activated STAT3 was recorded in about 60% of ccRCC, 57% of papillary RCC and 33% of chromophobe RCC. Moreover, the nuclear expression of its phosphorylated form was enhanced in ccRCC, papillary RCC and urothelial carcinoma compared with tumor with inferior malignant potential (chromophobe) or benign tumor (oncocytoma) [83].
Furthermore, Zhou et al. analyzed the gene expression profiles of 60 clear cell RCC (ccRCC). Their results were matched with normal renal samples from The Cancer Genome Atlas. They found that fatty acid-binding protein 7 was one of the most commonly overexpressed genes in ccRCC and was able to promote tumor growth through the activation of STAT3 and ERK signaling pathways [84].
CD44 transmembrane glycoproteins is a ubiquitous cell surface adhesion molecule involved in cell–cell and cell–matrix interactions. CD44 was originally described as a mediator of lymphocyte homing to peripheral lymphoid tissues and is closely correlated with tumor cell proliferation, metastasis and patient outcome [85]. Qin et al. analyzed the expression of CD44 and activated STAT3 in a series of 75 RCC carcinoma and paired adjacent nontumor renal tissue samples from patients with localized ccRCC who underwent a nephrectomy. They found that CD44 was highly expressed in almost 50% or RCC and was associated with tumor grade, size and stage. They also observed a strong correlation between the expression of CD44 and pSTAT3. The simultaneous presence CD44 and pSTAT3 overexpression was recorded in 42.66% of tumor samples and had an additive negative impact on patient OS [86].
STAT3 has been shown to act as a potential modulator of HIF-mediated VEGF expression in RCC [87]. Activated STAT3 can increase HIF1α protein levels by blocking HIF1α degradation and enhancing its de novo synthesis. In addition, STAT3 can activate HIF1 target genes by binding to HIF1 target gene promoters and forming complexes with coactivators CREB-binding protein and p300, and RNA polymerase II [88]. In accordance with these findings, STAT3 inhibitor WP1066 has been shown to induce apoptosis, and inhibit the basal and hypoxia-induced expression of HIF1α and HIF2α, as well as VEGF secretion in RCC cell lines [89].
Tumor-associated macrophages play a vital role in the carcinogenesis and progression of RCC [90]. Tumor-associated macrophages release angiogenic cytokines that modulate RCC angiogenesis by activating NF-κB and STAT3 signaling. STAT3 is also involved in IL-6-induced proliferation of RCC cells [89] and in the activation of RCC cancer cells mediated by macrophages, thus representing an emerging target for the treatment of RCC.
STAT3 signaling pathway has been also associated with response to treatment in RCC. Single nucleotide polymorphisms in the STAT3 gene have been associated with better response to IFN-α [91]. On the other hand, inhibited STAT3 activity enhanced the antitumor effects of VEGFR-tyrosine kinase inhibitor sunitinib [92]. In addition, VEGFR-tyrosine kinase inhibitor axitinib has been shown to modulate antitumor immunity by downregulating STAT3 expression and reversing the RCC-induced immunosuppression mediated by myeloid-derived suppressor cells [93].
Recently, data concerning the inhibition of RCC growth and metastasis via AKT/mammalian target of rapamycin, ERK and JAK2/STAT3 pathway inhibition induced by simvastatin have opened a novel therapeutic perspective for these patients [94], also these data should be confirmed in randomized trials.
Conclusion & future perspectives
Constitutively phosphorylated STAT3 has been implicated in several human tumors, including genitourinary cancers (Figure 1). Based on its involvement in tumor growth, metastasis and response to therapy, as well as in epigenetic regulation, CSCs and premetastatic niches, STAT3 has emerged as ideal molecular target for cancer therapy. The prominent role of STAT3, compared with other STAT members, as a therapeutic target for genitourinary cancer is sustained by its activity in both tumor, stromal and immune cells, which also promote tumor development and progression. In addition, the STAT3 inhibitors are associated with a potentially lower risk of related toxicities due to the transient status of STAT3 signaling in normal cells and to the minimal effects of STAT3 inhibition in mature cells.
STAT3 is placed at the crossroads of multiple signaling pathways. Small-molecule drugs to target STAT3 signaling have been developed over the last years and are in various phases of ongoing clinical study. Several strategies have been evaluated to target directly STAT3 or inhibiting STAT3 protein or indirectly through blockade of the upstream components of this pathway. However, a specific anti-STAT3 inhibitor is not yet clinically available. Furthermore, the combination of STAT3 inhibitors with approved or emerging antiangiogenic or immunotherapeutic agents should be investigated in patients with genitourinary tumors.
Extensive clinical studies are trying to identify anti-STAT3 drugs with high single-agent activity. However, the variety of STAT3 functions, together with its striking overall similarity with STAT1 and to the wide range of upstream activators converging on the JAK–STAT3 pathway, are enabling to identify a single target that may be effective for cancer therapy in patients with genitourinary tumors.
In conclusion, these data suggest that STAT3 signaling pathway is crucial in the carcinogenesis, growth, metastasis and response to treatment of genitourinary tumors. The identification and development of novel more selective agents will be an important scientific and clinical challenge in the therapeutic scenario of this population in the near future.
Executive summary.
STAT3 promotes tumor growth, invasion and angiogenesis in prostate, bladder and renal tumors.
In prostate cancer, STAT3 activation correlates with pathological stage and Gleason score and modulates androgen receptor expression and function, as well as cancer stem cell and epithelial–mesenchymal transition.
Is involved in the resistance to enzalutamide.
Promotes the progression from carcinoma in situ to invasive bladder tumor.
In bladder cancer, STAT3 interacts with the EGF pathway and is associated with the expression of CD44, a glycoprotein involved in cell–cell and cell–matrix interactions.
In renal cell carcinoma, STAT3 cooperates with HIF1 to induce VEGF expression. STAT3 can increase HIF1α protein levels by blocking HIF1α degradation and enhancing its de novo synthesis.
Footnotes
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Open Access
This work is licensed under the Creative Commons Attribution 4.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Darnell JE, Jr, Kerr IM, Stark GR. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science. 1994;264:1415–1421. doi: 10.1126/science.8197455. [DOI] [PubMed] [Google Scholar]; • These authors elucidated the biological functions of STAT family members and their role in the IFN-α and IFN-γ pathways.
- 2.Yu H, Jove R. The STATs of cancer-new molecular targets come of age. Nat. Rev. Cancer. 2004;4(2):97–105. doi: 10.1038/nrc1275. [DOI] [PubMed] [Google Scholar]
- 3.Raz R, Durbin JE, Levy DE. Acute phase response factor and additional members of the interferon-stimulated gene factor 3 family integrate diverse signals from cytokines, interferons, and growth factors. J. Biol. Chem. 1994;269(39):24391–24395. [PubMed] [Google Scholar]
- 4.Silva CM. Role of STATs as downstream signal transducers in Src family kinase-mediated tumorigenesis. Oncogene. 2004;23(48):8017–8023. doi: 10.1038/sj.onc.1208159. [DOI] [PubMed] [Google Scholar]
- 5.Zammarchi F, de Stanchina E, Bournazou E, et al. Antitumorigenic potential of STAT3 alternative splicing modulation. Proc. Natl Acad. Sci. USA. 2011;108(43):17779–17784. doi: 10.1073/pnas.1108482108. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Elucidated at molecular level the splicing regulation that shifts the expression from STAT3α to STAT3β. This suggests a potential target for more focused therapy in order to shift the balance between the two splicing isoforms.
- 6.Ng IH, Ng DC, Jans DA, Bogoyevitch MA. Selective STAT3-α or -β expression reveals spliceform-specific phosphorylation kinetics, nuclear retention and distinct gene expression outcomes. Biochem. J. 2012;447(1):125–136. doi: 10.1042/BJ20120941. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Showed the different behavior of two STAT3 alternative splicing products. This suggests the role of future drugs targeting a specific STAT3 isoforms.
- 7.Zhong Z, Wen Z, Darnell JE., Jr Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science. 1994;264(5155):95–98. doi: 10.1126/science.8140422. [DOI] [PubMed] [Google Scholar]
- 8.West NR, Murray JI, Watson PH. Oncostatin-M promotes phenotypic changes associated with mesenchymal and stem cell-like differentiation in breast cancer. Oncogene. 2014;33(12):1485–1494. doi: 10.1038/onc.2013.105. [DOI] [PubMed] [Google Scholar]
- 9.Guo L, Chen C, Shi M, et al. Stat3-coordinated Lin-28-let-7-HMGA2 and miR-200-ZEB1 circuits initiate and maintain oncostatin M-driven epithelialmesenchymal transition. Oncogene. 2013;32(45):5272–5282. doi: 10.1038/onc.2012.573. [DOI] [PubMed] [Google Scholar]
- 10.Wen Z, Zhong Z, Darnell JE. Maximal activation of transcription by Stat1 and Stat3 requires both tyrosine and serine phosphorylation. Cell. 1995;82(2):241–250. doi: 10.1016/0092-8674(95)90311-9. [DOI] [PubMed] [Google Scholar]
- 11.Garcia R, Yu CL, Hudnall A, et al. Constitutive activation of Stat3 in fibroblasts transformed by diverse oncoproteins and in breast carcinoma cells. Cell Growth Differ. 1997;8(12):1267–1276. [PubMed] [Google Scholar]
- 12.Grandis JR, Drenning SD, Chakraborty A, et al. Requirement of Stat3 but not Stat1 activation for epidermal growth factor receptor-mediated cell growth in vitro. J. Clin. Invest. 1998;102(7):1385–1392. doi: 10.1172/JCI3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cattaneo E, Magrassi L, De-Fraja C, et al. Variations in the levels of the JAK/STAT and ShcA proteins in human brain tumors. AntiCancer Res. 1998;18(4A):2381–2387. [PubMed] [Google Scholar]
- 14.Flørenes VA, Lu C, Bhattacharya N, et al. Interleukin-6 dependent induction of the cyclin dependent kinase inhibitor p21WAF1/CIP1 is lost during progression of human malignant melanoma. Oncogene. 1999;18(4):1023–1032. doi: 10.1038/sj.onc.1202382. [DOI] [PubMed] [Google Scholar]
- 15.Kirkwood JM, Farkas DL, Chakraborty A, et al. Systemic interferon-alpha (IFN-alpha) treatment leads to Stat3 inactivation in melanoma precursor lesions. Mol. Med. 1999;5(1):11–20. [PMC free article] [PubMed] [Google Scholar]
- 16.Lou W, Ni Z, Dyer K, et al. Interleukin-6 induces prostate cancer cell growth accompanied by activation of stat3 signaling pathway. Prostate. 2000;42(3):239–242. doi: 10.1002/(sici)1097-0045(20000215)42:3<239::aid-pros10>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 17.Magrassi L, De-Fraja C, Conti L, et al. Expression of the JAK and STAT superfamilies in human meningiomas. J. Neurosurg. 1999;91(3):440–446. doi: 10.3171/jns.1999.91.3.0440. [DOI] [PubMed] [Google Scholar]
- 18.Pansky A, Hildebrand P, Fasler-Kan E, et al. Defective Jak-STAT signal transduction pathway in melanoma cells resistant to growth inhibition by interferon-alpha. Int. J. Cancer. 2000;85(5):720–725. doi: 10.1002/(sici)1097-0215(20000301)85:5<720::aid-ijc20>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 19.Schrell UM, Koch HU, Marschalek R, et al. Formation of autocrine loops in human cerebral meningioma tissue by leukemia inhibitor factor, interleukin-6, and oncostatin M: inhibition of meningioma cell growth in vitro by recombinant oncostatin M. J. Neurosurg. 1998;88(3):541–548. doi: 10.3171/jns.1998.88.3.0541. [DOI] [PubMed] [Google Scholar]
- 20.Bromberg JF, Wrzeszczynska MH, Devgan G, et al. Stat3 as an oncogene. Cell. 1999;98(3):295–303. doi: 10.1016/s0092-8674(00)81959-5. [DOI] [PubMed] [Google Scholar]
- 21.Catlett-Falcone R, Landowski TH, Oshiro MM, et al. Constitutive activation of Stat3 signaling confers resistance to apoptosis in human U266 myeloma cells. Immunity. 1999;10(1):105–115. doi: 10.1016/s1074-7613(00)80011-4. [DOI] [PubMed] [Google Scholar]
- 22.Kujawski M, Kortylewski M, Lee H, Herrmann A, Kay H, Yu H. Stat3 mediates myeloid cell-dependent tumor angiogenesis in mice. J. Clin. Invest. 2008;118(10):3367–3377. doi: 10.1172/JCI35213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burke WM, Jin X, Lin HJ, et al. Inhibition of constitutively active Stat3 suppresses growth of human ovarian and breast cancer cells. Oncogene. 2001;20(55):7925–7934. doi: 10.1038/sj.onc.1204990. [DOI] [PubMed] [Google Scholar]
- 24.Chiu HC, Chou DL, Huang CT, et al. Suppression of STAT3 activity sensitizes gefitinib-resistant non small cell lung cancer cells. Biochem. Pharmacol. 2011;81(11):1263–1270. doi: 10.1016/j.bcp.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Vinkemeier U. Getting the message across, STAT! Design principles of a molecular signaling circuit. J. Cell Biol. 2004;167(2):197–201. doi: 10.1083/jcb.200407163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gorlich D. Transport into and out of the cell nucleus. EMBO J. 1998;17(10):2721–2727. doi: 10.1093/emboj/17.10.2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ma J, Zhang T, Novotny-Diermayr V, et al. A novel sequence in the coiled-coil domain of Stat3 essential for its nuclear translocation. J. Biol. Chem. 2003;278(31):29252–29260. doi: 10.1074/jbc.M304196200. [DOI] [PubMed] [Google Scholar]
- 28.Frank DA. STAT3 as a central mediator of neoplastic cellular transformation. Cancer Lett. 2007;251(2):199–210. doi: 10.1016/j.canlet.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 29.Suetsugu S, Takenawa T. Regulation of cortical actin networks in cell migration. Int. Rev. Cytol. 2003;229:245–286. doi: 10.1016/s0074-7696(03)29006-9. [DOI] [PubMed] [Google Scholar]
- 30.Teng Y, Ross JL, Cowell JK. The involvement of JAK-STAT3 in cell motility, invasion, and metastasis. JAKSTAT. 2014;3(1):e28086. doi: 10.4161/jkst.28086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sun B, Kawahara M, Ehata S, Nagamune T. AAG8 promotes carcinogenesis by activating STAT3. Cell Signal. 2014;26(9):1863–1869. doi: 10.1016/j.cellsig.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 32.Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014;15(3):178–196. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Elucidated the role of STAT3 and other pathways in modulating epithelial–mesenchymal transition.
- 33.Puisieux A, Brabletz T, Caramel J. Oncogenic roles of EMT-inducing transcription factors. Nat. Cell Biol. 2014;16(6):488–494. doi: 10.1038/ncb2976. [DOI] [PubMed] [Google Scholar]
- 34.Wendt MK, Balanis N, Carlin CR, Schiemann WP. STAT3 and epithelial-mesenchymal transitions in carcinomas. JAKSTAT. 2014;3(1):e28975. doi: 10.4161/jkst.28975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat. Immunol. 2010;11(10):889–896. doi: 10.1038/ni.1937. [DOI] [PubMed] [Google Scholar]
- 36.Kortylewski M, Kujawski M, Wang T, et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat. Med. 2005;11(12):1314–1321. doi: 10.1038/nm1325. [DOI] [PubMed] [Google Scholar]
- 37.Kortylewski M, Xin H, Kujawski M, et al. Regulation of the IL-23 and IL-12 balance by Stat3 signaling in the tumor microenvironment. Cancer Cell. 2009;15(2):114–123. doi: 10.1016/j.ccr.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kujawski M, Kortylewski M, Lee H, Herrmann A, Kay H, Yu H. Stat3 mediates myeloid cell-dependent tumor angiogenesis in mice. J. Clin. Invest. 2008;118(10):3367–3377. doi: 10.1172/JCI35213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang L, Yi T, Kortylewski M, Pardoll DM, Zeng D, Yu H. IL-17 can promote tumor growth through an IL-6-Stat3 signaling pathway. J. Exp. Med. 2009;206(7):1457–1464. doi: 10.1084/jem.20090207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deng J, Liu Y, Lee H, et al. S1PR1-STAT3 signaling is crucial for myeloid cell colonization at future metastatic sites. Cancer Cell. 2012;21(5):642–654. doi: 10.1016/j.ccr.2012.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dhir R, Ni Z, Lou W, DeMiguel F, Grandis JR, Gao AC. Stat3 activation in prostatic carcinomas. Prostate. 2002;51(4):241–246. doi: 10.1002/pros.10079. [DOI] [PubMed] [Google Scholar]
- 42.Ni Z, Lou W, Leman ES, Gao AC. Inhibition of constitutively activated Stat3 signaling pathway suppresses growth of prostate cancer cells. Cancer Res. 2000;60(5):1225–1228. [PubMed] [Google Scholar]
- 43.Schroeder A, Herrmann A, Cherryholmes G, et al. Loss of androgen receptor expression promotes a stem-like cell phenotype in prostate cancer through STAT3 signaling. Cancer Res. 2014;74(4):1227–1237. doi: 10.1158/0008-5472.CAN-13-0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li L, Xie H, Liang L, et al. Increased PrLZ-mediated androgen receptor transactivation promotes prostate cancer growth at castration-resistant stage. Carcinogenesis. 2013;34(2):257–267. doi: 10.1093/carcin/bgs337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang D, He D, Xue Y, et al. PrLZ protects prostate cancer cells from apoptosis induced by androgen deprivation via the activation of Stat3/Bcl-2 pathway. Cancer Res. 2011;71(6):2193–2202. doi: 10.1158/0008-5472.CAN-10-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ahlqvist K, Saamarthy K, Syed Khaja AS, Bjartell A, Massoumi R. Expression of Id proteins is regulated by the Bcl-3 proto-oncogene in prostate cancer. Oncogene. 2013;32(12):1601–1608. doi: 10.1038/onc.2012.175. [DOI] [PubMed] [Google Scholar]
- 47.Ueda T, Bruchovsky N, Sadar MD. Activation of the androgen receptor N-terminal domain by interleukin-6 via MAPK and STAT3 signal transduction pathways. J. Biol. Chem. 2002;277(9):7076–7085. doi: 10.1074/jbc.M108255200. [DOI] [PubMed] [Google Scholar]
- 48.Mora LB, Buettner R, Seigne J, et al. Constitutive activation of Stat3 in human prostate tumors and cell lines: direct inhibition of Stat3 signaling induces apoptosis of prostate cancer cells. Cancer Res. 2002;62(22):6659–6666. [PubMed] [Google Scholar]
- 49.Stoyanova T, Cooper AR, Drake JM, et al. Prostate cancer originating in basal cells progresses to adenocarcinoma propagated by luminal-like cells. Proc. Natl Acad. Sci. USA. 2013;110(50):20111–20116. doi: 10.1073/pnas.1320565110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Markert EK, Mizuno H, Vazquez A, Levine AJ. Molecular classification of prostate cancer using curated expression signatures. Proc. Natl Acad. Sci. USA. 2011;108(52):21276–21281. doi: 10.1073/pnas.1117029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kroon P, Berry PA, Stower MJ, et al. JAK-STAT blockade inhibits tumor initiation and clonogenic recovery of prostate cancer stem-like cells. Cancer Res. 2013;73(16):5288–5298. doi: 10.1158/0008-5472.CAN-13-0874. [DOI] [PubMed] [Google Scholar]
- 52.Fang LY, Izumi K, Lai KP, et al. Infiltrating macrophages promote prostate tumorigenesis via modulating androgen receptor-mediated CCL4-STAT3 signaling. Cancer Res. 2013;73(18):5633–5646. doi: 10.1158/0008-5472.CAN-12-3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thisse B, el Messal M, Perrin-Schmitt F. The twist gene: isolation of a Drosophila zygotic gene necessary for the establishment of dorsoventral pattern. Nucleic Acids Res. 1987;15(8):3439–3453. doi: 10.1093/nar/15.8.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang J, Mani SA, Donaher JL, et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117(7):927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 55.Shiota M, Zardan A, Takeuchi A, et al. Clusterin mediates TGF-beta-induced epithelial-mesenchymal transition and metastasis via Twist1 in prostate cancer cells. Cancer Res. 2012;72(20):5261–5272. doi: 10.1158/0008-5472.CAN-12-0254. [DOI] [PubMed] [Google Scholar]
- 56.Bishop JL, Thaper D, Zoubeidi A. The multifaceted roles of STAT3 signaling in the progression of prostate cancer. Cancers (Basel) 2014;6(2):829–859. doi: 10.3390/cancers6020829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kujawski M, Kortylewski M, Lee H, Herrmann A, Kay H, Yu H. Stat3 mediates myeloid cell-dependent tumor angiogenesis in mice. J. Clin. Invest. 2008;118(10):3367–3377. doi: 10.1172/JCI35213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Eisermann K, Broderick CJ, Bazarov A, Moazam MM, Fraizer GC. Androgen up-regulates vascular endothelial growth factor expression in prostate cancer cells via an Sp1 binding site. Mol. Cancer. 2013;12:7. doi: 10.1186/1476-4598-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gray MJ, Zhang J, Ellis LM, et al. HIF-1alpha, STAT3, CBP/p300 and Ref-1/APE are components of a transcriptional complex that regulates Src-dependent hypoxia-induced expression of VEGF in pancreatic and prostate carcinomas. Oncogene. 2005;24(19):3110–3120. doi: 10.1038/sj.onc.1208513. [DOI] [PubMed] [Google Scholar]
- 60.Horinaga M, Okita H, Nakashima J, Kanao K, Sakamoto M, Murai M. Clinical and pathologic significance of activation of signal transducer and activator of transcription 3 in prostate cancer. Urology. 2005;66(3):671–675. doi: 10.1016/j.urology.2005.03.066. [DOI] [PubMed] [Google Scholar]
- 61.Liu X, He Z, Li C-H, Huang G, Ding C, Liu H. Correlation analysis of JAK-STAT pathway components on prognosis of patients with prostate cancer. Pathol. Oncol. Res. 2012;18(1):17–23. doi: 10.1007/s12253-011-9410-y. [DOI] [PubMed] [Google Scholar]
- 62.Akimoto S, Okumura A, Fuse H. Relationship between serum levels of interleukin-6, tumor necrosis factor-alpha and bone turnover markers in prostate cancer patients. Endocr. J. 1998;45(2):183–189. doi: 10.1507/endocrj.45.183. [DOI] [PubMed] [Google Scholar]
- 63.Adler HL, McCurdy MA, Kattan MW, Timme TL, Scardino PT, Thompson TC. Elevated levels of circulating interleukin-6 and transforming growth factor-beta1 in patients with metastatic prostatic carcinoma. J. Urol. 1999;161(1):182–187. [PubMed] [Google Scholar]
- 64.Nakashima J, Tachibana M, Horiguchi Y, et al. Serum interleukin 6 as a prognostic factor in patients with prostate cancer. Clin. Cancer Res. 2000;6(7):2702–2706. [PubMed] [Google Scholar]
- 65.Tam L, McGlynn LM, Traynor P, Mukherjee R, Bartlett JMS, Edwards J. Expression levels of the JAK/STAT pathway in the transition from hormone-sensitive to hormone-refractory prostate cancer. Br. J. Cancer. 2007;97(3):378–383. doi: 10.1038/sj.bjc.6603871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N. Engl. J. Med. 2014;371(5):424–433. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 2012;367(13):1187–1197. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 68.Antonarakis ES, Lu C, Wang H, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl. J. Med. 2014;371(11):1028–1038. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Elucidated the role of androgen receptor isoform encoded by splice variant 7 (AR-V7), which is constitutively activated but lacks of the ligand-binding domain targetable by abiraterone and enzalutamide, being involved in the resistance to these agents.
- 69.Liu C, Zhu Y, Lou W, Cui Y, Evans CP, Gao AC. Inhibition of constitutively active Stat3 reverses enzalutamide resistance in LNCaP derivative prostate cancer cells. Prostate. 2014;74(2):201–209. doi: 10.1002/pros.22741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Han Z, Wang X, Ma L, et al. Inhibition of STAT3 signaling targets both tumor-initiating and differentiated cell populations in prostate cancer. Oncotarget. 2014;5(18):8416–8428. doi: 10.18632/oncotarget.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Foster CS, Ross JS. Pathologyof the urachus. In: Foster CS, Ross JS, editors. Pathologyof the Urinary Bladder. Saunders; Philadelphia, PA, USA: 2004. pp. 183–267. [Google Scholar]
- 72.van Rhijn BWG, van der Kwast TH, Vis AN, et al. FGFR3 and P53 characterize alternative genetic pathways in the pathogenesis of urothelial cell carcinoma. Cancer Res. 2004;64(6):1911–1914. doi: 10.1158/0008-5472.can-03-2421. [DOI] [PubMed] [Google Scholar]
- 73.Ho PL, Lay EJ, Jian W, Parra D, Chan KS. Stat3 activation in urothelial stem cells leads to direct progression to invasive bladder cancer. Cancer Res. 2012;72(13):3135–3142. doi: 10.1158/0008-5472.CAN-11-3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ho PL, Kurtova A, Chan KS. Normal and neoplastic urothelial stem cells: getting to the root of the problem. Nat. Rev. Urol. 2012;9(10):583–594. doi: 10.1038/nrurol.2012.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang B, Lu Z, Hou Y, Hu J, Wang C. The effects of STAT3 and survivin silencing on the growth of human bladder carcinoma cells. Tumour Biol. 2014;35(6):5401–5407. doi: 10.1007/s13277-014-1704-8. [DOI] [PubMed] [Google Scholar]
- 76.Guo Z, Linn JF, Wu G, et al. CDC91L1 (PIG-U) is a newly discovered oncogene in human bladder cancer. Nat. Med. 2004;10(4):374–381. doi: 10.1038/nm1010. [DOI] [PubMed] [Google Scholar]
- 77.Cheng J, Huang H, Zhang ZT, et al. Overexpression of epidermal growth factor receptor in urothelium elicits urothelial hyperplasia and promotes bladder tumor growth. Cancer Res. 2002;62(14):4157–4163. [PubMed] [Google Scholar]
- 78.Itoh M, Murata T, Suzuki T, et al. Requirement of STAT3 activation for maximal collagenase-1 (MMP-1) induction by epidermal growth factor and malignant characteristics in T24 bladder cancer cells. Oncogene. 2006;25(8):1195–1204. doi: 10.1038/sj.onc.1209149. [DOI] [PubMed] [Google Scholar]
- 79.Shen HB, Gu ZQ, Jian K, Qi J. CXCR4-mediated Stat3 activation is essential for CXCL12-induced cell invasion in bladder cancer. Tumour Biol. 2013;34(3):1839–1845. doi: 10.1007/s13277-013-0725-z. [DOI] [PubMed] [Google Scholar]
- 80.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 81.Iacovelli R, Alesini D, Palazzo A, et al. Targeted therapies and complete responses in first line treatment of metastatic renal cell carcinoma. A meta-analysis of published trials. Cancer Treat. Rev. 2014;40:271–275. doi: 10.1016/j.ctrv.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 82.Masuda A, Kamai T, Abe H, Arai K, Yoshida K. Is Stat3 and/or p53 mRNA expression a prognostic marker for renal cell carcinoma? Biomed. Res. 2009;30(3):171–176. doi: 10.2220/biomedres.30.171. [DOI] [PubMed] [Google Scholar]
- 83.Guo C, Yang G, Khun K, et al. Activation of Stat3 in renal tumors. Am. J. Transl. Res. 2009;1(3):283–290. [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou J, Deng Z, Chen Y, et al. Overexpression of FABP7 promotes cell growth and predicts poor prognosis of clear cell renal cell carcinoma. Urol. Oncol. 2015;33(3):113.e9–113.e17. doi: 10.1016/j.urolonc.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 85.Marhaba R, Zöller M. CD44 in cancer progression: adhesion, migration and growth regulation. J. Mol. Histol. 2004;35(3):211–231. doi: 10.1023/b:hijo.0000032354.94213.69. [DOI] [PubMed] [Google Scholar]
- 86.Qin J, Yang B, Xu BQ, et al. Concurrent CD44s and STAT3 expression in human clear cell renal cellular carcinoma and its impact on survival. Int. J. Clin. Exp. Pathol. 2014;7(6):3235–3244. [PMC free article] [PubMed] [Google Scholar]
- 87.Jung JE, Lee HG, Cho IH, et al. STAT3 is a potential modulator of HIF-1-mediated VEGF expression in human renal carcinoma cells. FASEB J. 2005;19(10):1296–1298. doi: 10.1096/fj.04-3099fje. [DOI] [PubMed] [Google Scholar]
- 88.Pawlus MR, Wang L, Hu CJ. STAT3 and HIF1α cooperatively activate HIF1 target genes in MDA-MB-231 and RCC4 cells. Oncogene. 2014;33(13):1670–1679. doi: 10.1038/onc.2013.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Horiguchi A, Oya M, Marumo K, Murai M. STAT3, but not ERKs, mediates the IL-6-induced proliferation of renal cancer cells, ACHN and 769P. Kidney Int. 2002;61(3):926–938. doi: 10.1046/j.1523-1755.2002.00206.x. [DOI] [PubMed] [Google Scholar]
- 90.Santoni M, Massari F, Amantini C, et al. Emerging role of tumor-associated macrophages as therapeutic targets in patients with metastatic renal cell carcinoma. Cancer Imm. Immunother. 2013;62(12):1757–1768. doi: 10.1007/s00262-013-1487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ito N, Eto M, Nakamura E, et al. STAT3 polymorphism predicts interferon-alfa response in patients with metastatic renal cell carcinoma. J. Clin. Oncol. 2007;25(19):2785–2791. doi: 10.1200/JCO.2006.09.8897. [DOI] [PubMed] [Google Scholar]
- 92.Xin H, Zhang C, Herrmann A, Du Y, Figlin R, Yu H. Sunitinib inhibition of Stat3 induces renal cell carcinoma tumor cell apoptosis and reduces immunosuppressive cells. Cancer Res. 2009;69(6):2506–2013. doi: 10.1158/0008-5472.CAN-08-4323. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Elucidated the role of STAT3 in the activity of sunitinib in renal cell carcinoma, thus providing a potential biomarker for the efficacy of this agent.
- 93.Yuan H, Cai P, Li Q, et al. Axitinib augments antitumor activity in renal cell carcinoma via STAT3-dependent reversal of myeloid-derived suppressor cell accumulation. Biomed. Pharmacother. 2014;68(6):751–756. doi: 10.1016/j.biopha.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 94.Fang Z, Tang Y, Fang J, et al. Simvastatin inhibits renal cancer cell growth and metastasis via AKT/mTOR, ERK and JAK2/STAT3 pathway. PLoS One. 2013;8(5):e62823. doi: 10.1371/journal.pone.0062823. [DOI] [PMC free article] [PubMed] [Google Scholar]