Abstract
Purpose:
To compare the effectiveness, safety and stability of the results of transepithelial photorefractive keratectomy (tPRK) with conventional photorefractive keratectomy (PRK) for low to moderate myopia.
Methods:
In this prospective non-randomized case-control study, patients with low to moderate myopia were assigned to the tPRK group (cases) or the PRK group (controls). In the tPRK group, eyes were treated using the Amaris excimer laser (SCHWIND eye-tech-solutions GmbH and Co. KG, Germany). Outcome measures included postoperative pain using McGill Pain Questionnaire, epithelial healing time, uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), manifest refraction, and safety and efficacy indexes which were compared between the study groups.
Results:
Three hundred forty eyes of 170 patients were enrolled in this study. Each study group comprised of 170 eyes of 85 patients. There was a significant difference between the two groups regarding the postoperative pain scores in favor of the tPRK group (P = 0.04). The tPRK group had a shorter epithelial healing time than the conventional PRK group postoperatively (P = 0.01). Mean UCVA was significantly better in the case group than in the control group at the postoperative month 2 (P = 0.01). Regarding the safety and efficacy indexes, the tPRK group had better results than the conventional PRK group (P < 0.01 for both comparisons).
Conclusion:
Transepithelial PRK seems to be superior to conventional PRK for treatment of low to moderate myopia in terms of postoperative pain, epithelial healing time, visual recovery and safety and efficacy indexes.
Keywords: Conventional Photorefractive Keratectomy, Transepithelial Photorefractive Keratectomy, Myopia
INTRODUCTION
Photorefractive keratectomy (PRK) has commonly been used as an effective, safe and reasonable method for treatment of patients with low to moderate myopia since 1983.[1,2,3,4,5,6] Moreover, PRK is appropriate for subjects with refractive errors who are not eligible candidates for laser in situ keratomileusis (LASIK) due to thin corneas, subtle topographic irregularities and epithelial basement membrane disease.[7,8] Corneal haze, epithelial healing irregularity and pain are known adverse effects of PRK.[9,10] Transepithelial PRK (tPRK) using Amaris excimer laser is a modified and alternative method to conventional PRK.[11] The unique feature of this technique is that it can be applied as one step, non-touch surgery using the transepithelial PRK nomogram of the Amaris laser with minimum induced trauma to the eye.[12]
To the best our knowledge, there are few studies on the outcomes of tPRK.[12,13] Our previous experience with these tools differed from published literature. Herein, we compared the outcomes of tPRK with those of conventional PRK with respect to the postoperative pain, healing time and visual acuity recovery.
METHODS
In this prospective, non-randomized, controlled trial, patients with mild to moderate myopia with or without astigmatism who underwent PRK between January 2013 and May 2013 were enrolled. Patients were divided into two groups; the case group for whom tPRK was performed and the age-matched control group who received conventional alcohol-assisted PRK. Mild myopia was defined as a spherical equivalent refraction of −0.50 to −3.00 D and moderate myopia as a spherical equivalent refraction between −3.25 and −6.00 D in at least one eye.[14] The study protocol was approved by the institutional review board of Baqiyatallah university of Medical Sciences, Tehran, Iran and signed informed consent was obtained from all patients.
Patients were excluded if they failed to meet any of the above inclusion criteria or for the following reasons: unstable standard cycloplegic refraction, preoperative best corrected visual acuity (BCVA) less than 20/20, eyes unsuitable for PRK based on preoperative assessment of ocular topography e.g. corneal dystrophy with topographic irregularity, pellucid marginal degeneration, forme fruste keratoconus, corneal warpage, severe dry eye syndrome, previous corneal or intraocular surgery, history of current eyelid disease, or any form of keratitis. Patients were requested to discontinue contact lens wear for a minimum of 4 days (soft lenses) or a minimum of 3 weeks (rigid gas permeable lenses) prior to the preoperative evaluation.
All patients had a complete preoperative eye examination including uncorrected visual acuity (UCVA) and BCVA assessment, manifest and cycloplegic refraction, slit lamp biomicroscopy (Carl Zeiss Meditec AG Göschwitzer Straße, Jena, Germany) to evaluate the anterior segment and the fundus, and applanation tonometry.
All surgical procedures were performed by a single surgeon (M-N). After povidone iodine scrub was applied on the lashes and eyelids, a closed loop lid speculum equipped with suction was placed. One drop of proparacaine 0.50% was instilled in the eye. In the case group, laser ablative surgery was performed in a single step using the tPRK nomogram (Amaris laser's ORK-CAM software, SCHWIND eye-tech-solutions, Kleinostheim, Germany).
In the control group, 17% ethyl alcohol in an 8–9 mm well was placed on the cornea for 15 seconds. Cornea was irrigated using balanced salt solution and dry polyvinyl alcohol sponge (Merocel; Beaver-Visitec International, Inc., Waltham, USA) was used to peel off the epithelium. Subsequently, laser ablation was done in both groups using ablation profile of the laser's software. The optical zone varied between 6.5 mm and 7mm in both groups, and the transition zone was calculated based on the patient's age, refractive error, and keratometric readings using the nomogram. Then, mitomycin C 0.02% was applied on the ablated stroma in corneas with an ablation depth of more than 30 μm. The duration of mitomycin C application was approximately 35 seconds.
After laser ablation, a high water content bandage contact lens Senofilcon A (Acuvue ®; Johnson and Johnson Vision Care, Inc., Jacksonville, USA) was placed on the cornea and topical antibiotic and corticosteroid eye drops were instilled. Postoperatively, patients received betamethasone and chloramphenicol eye drops four times a day and preservative free artificial tears every two hours. Chloramphenicol eye drops were discontinued after one week, but betamethasone eye drops were tapered off over 4 to 6 weeks. Patients were followed up daily until the corneal epithelium completely healed. Epithelial healing was assessed daily at the slit lamp, with fluorescein staining when needed. The therapeutic contact lens was removed if there was no epithelial defect.
Postoperatively, visual acuity (expressed in logMAR) and refractive outcomes were analyzed at months 2 and 6. Furthermore, an examiner who was masked to the type of surgery performed postoperative examinations including manifest refraction and slit lamp examination. Moreover, a masked nurse interviewed the patients to record the pain score they had experienced at the postoperative day 1 using a 5-point Present Pain Intensity (PPI) scale of the standard long form McGill Pain Questionnaire (LF-MPQ). Accordingly, pain severity was scored as follows: 1 = mild, 2 = discomforting, 3 = distressing, 4 = horrible, 5 = excruciating. Corneal haze was graded according to a study by Fantes et al[15] as follows: 0 = no haze; 0.50 = trace haze on oblique illumination; 1 = corneal cloudiness not interfering with the visibility of fine iris details; 2 = mild dimness of fine iris details; 3 = moderate obliteration of iris details, 4 = details of the lens and iris not discernible.
Safety of the procedure was defined as the percentage of eyes losing more than 2 lines of BCVA. Safety index was considered as mean postoperative BCVA/mean preoperative BCVA ratio. Efficacy was defined as the percentage of the eyes achieving a UCVA of 0.50 LogMAR (20/40) or better postoperatively. Efficacy index was defined as mean postoperative UCVA/mean preoperative BCVA ratio.[16,17]
Statistical analysis was performed using SPSS software (version 18.0, SPSS, Inc., IBM, Chicago, IL, USA). An unpaired t-test was used to compare the mean spherical equivalent (SE) refraction. The postoperative data were analyzed using Mann–Whitney U test to compare the epithelial healing time and the postoperative pain scores between the study groups. P- values less than 0.05 were considered as significant.
RESULTS
Three hundred and forty eyes of 170 patients were enrolled in the study including 170 eyes of 85 patients in each group. The case group included 31 (36.5%) male and 54 (63.5%) female subjects with a mean age of 28 ± 7 (range, 19–51) years. The control group consisted of 28 (33%) male and 57 (67%) female patients, with a mean age of 28.3 ± 7 (range, 19–50) years. Mean preoperative spherical equivalent refraction was −3.06 ± 1.5 diopters (D) in the case group and −2.9 ± 1.9 D in the control group. There was no statistically significant difference in the baseline manifest refraction between the two groups (P = 0.62). Mean preoperative BCVA (LogMAR) was 0.01 ± 0.05 (≃ 20/20) in the case group and 0.00 ± 0.04 (≃ 20/20) in the control group (P = 0.81).
Table 1 and Figure 1 show the postoperative results. The mean time of complete epithelial healing was significantly shorter in the case group (2.90 ± 0.42 days) as compared to the control group (3.30 ± 0.72 days) (P = 0.01). The mean subjective postoperative pain score at 24 hours was significantly lower in the case group compared to the control group (P = 0.04). After two months, the mean UCVA was significantly better in the case group than in the control group (P < 0.01), while there was no statistically significant difference between the two groups in UCVA at the postoperative month 6 [Table 1]. The majority of eyes had mild corneal stromal haze and only one patient had a haze grade 3 in the conventional PRK group [Table 1].
Table 1.
Postoperative results of transepithelial PRK versus conventional PRK
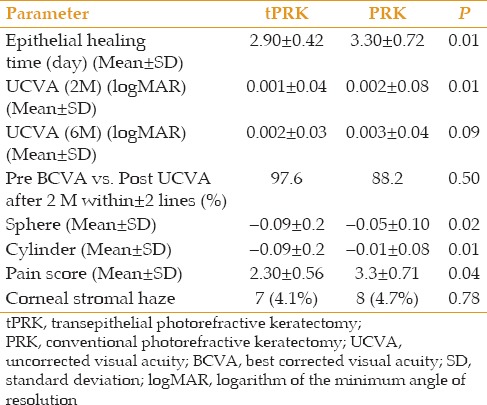
Figure 1.
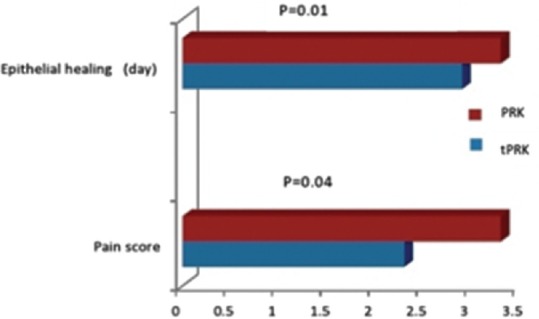
Corneal epithelial wound healing and pain score after photorefractive keratectomy (PRK) using a conventional and transepithelial (tPRK) procedures.
In the case group, spherical refraction decreased from −3.06 ± 1.5D to −0.09 ± 0.2D and cylindrical refraction decreased from −0.98 ± 1.1D to −0.09 ± 0.2D postoperatively. In the control group, spherical refraction decreased from −2.9 ± 1.9D to −0.05 ± 0.10D and cylindrical refraction changed from −1.2 ± 1.2D to −0.01 ± 0.08D after surgery. There were significant differences in the mean spherical and cylindrical refraction between the two groups postoperatively (P < 0.05).
In the transepithelial group, two months postoperation was associated with a higher percentage of UCVA within ± 2 lines of the preoperative BCVA (97.6% vs 88.2%) [Table 1]. Mean efficacy index was 0.20 ± 0.16 in the tPRK group and 0.13 ± 0.9 in the conventional PRK group (P < 0.01). Mean safety index was 1.36 ±0.11 in the tPRK group and 0.98 ± 0.22 in the conventional PRK group (P < 0.05). Despite this significant difference, the safety index approached 1.00 in the control group postoperatively, indicating that the visual outcome was satisfactory in this group. None of the patients were lost to follow-up. There were no early postoperative complications such as infection or recurrent erosion.
DISCUSSION
The present study assessed the visual outcomes and safety of tPRK versus conventional PRK for low to moderate myopia. We found that tPRK was better than conventional PRK regarding epithelial healing time, postoperative pain, safety and efficacy indexes and visual acuity recovery.
In a recent study comparing tPRK and conventional PRK, the average period to complete healing was 2.5 days in the transepithelial group versus 3.7 days in the conventional PRK.[12] Similarly in the current study, the epithelial healing period was shorter in the cases than in the controls. It could be due to the difference in epithelial denuding area and ablation area between the two groups; in tPRK, the epithelial removal size is equal to the ablation size, whereas in the conventional PRK, the epithelial removal size is more than the ablation size that could defer re-epithelialization.[12,13]
Patients’ perception of pain was another indicator for better postoperative outcome in the tPRK group in the present study. Fadlallah et al[12] found lower difference of pain score in the tPRK method compared to the conventional PRK. However, the pain score in their study was lower than our study. The major reason for the higher pain score in our study is the fact that we checked pain on the first postoperative day, while they reported pain score 48 hours postoperatively.
The rate of visual recovery was investigated and compared between the study groups. Fadlallah et al[12] reported significantly better UCVA in the tPRK group than in the PRK (P = 0.01) and LASIK (P = 0.008) groups. We found similar results as the tPRK group was superior to the conventional PRK group regarding UCVA at postoperative month 2. Lee et al[19] reported 27 patients who had laser epithelial keratomileusis (LASEK) in one eye and conventional PRK in the other eye for low to moderate myopia. Mean UCVA was 20/25 or better in 56% of patients three months after PRK. In our study, we noticed the UCVA of ≥20/25 in 84.7% of patients in the control group two months after PRK. It may be concluded that better visual acuity and faster visual recovery after tPRK in the present study were seemingly due to the absence of epithelial removal in this group.
Carones et al[20] reported lower corneal haze at one month and better corneal regularity index at 3 months in eyes in which the epithelium was removed using 20% alcohol. Similar method was used in our study in the conventional PRK group. However, when the mean change in the postoperative UCVA was compared with the preoperative BCVA, a significant difference was noticed after tPRK compared with conventional PRK. These results suggest that tPRK may give slightly better overall visual outcomes than conventional PRK for low to moderate myopia.
There was a significant difference between the safety and efficacy indexes between the two groups at 2 months which showed superiority of tPRK group versus conventional PRK group in short term period. Conversely, the conventional PRK group showed a slightly better UCVA than the tPRK group at 6 months; however this difference was not statistically significant.
The current study had a few limitations. We evaluated pain intensity only on postoperative day one. Pain typically peaks during the first 24 hours after PRK surgery, and subsides after approximately 3 days, coinciding with corneal re-epithelialization.[21] Secondly, the size of epithelial defects and the rate of epithelial healing were not assessed by an image analysis software which could be more reliable. Thirdly, we did not randomize the patients into two groups; the type of the procedure was chosen based on the patient's preference (after detailed description of the methods and procedures). The strengths of our study included a large sample size, stability of vision after six months and no reports pertaining adverse events in patient associated with any of the treatment methods.
In conclusion, this study highlighted the advantages of tPRK technique using Schwind Amaris nomogram over conventional PRK. Transepithelial PRK seems to be a safe and effective technique for treatment of mild to moderate myopia. A randomized prospective study with a longer follow-up period is required to confirm the results of the current study.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983;96:710–715. doi: 10.1016/s0002-9394(14)71911-7. [DOI] [PubMed] [Google Scholar]
- 2.Seiler T, Holschbach A, Derse M, Jean B, Genth U. Complications of myopic photorefractive keratectomy with the excimer laser. Ophthalmology. 1994;101:153–160. doi: 10.1016/s0161-6420(94)31371-6. [DOI] [PubMed] [Google Scholar]
- 3.Gartry DS, Kerr Muir MG, Marshall J. Excimer laser photorefractive keratectomy; 18-month follow-up. Ophthalmology. 1991;99:1209–1219. doi: 10.1016/s0161-6420(92)31821-4. [DOI] [PubMed] [Google Scholar]
- 4.Seiler T, Wollensak J. Myopic photorefractive keratectomy with excimer laser; one-year follow-up. Ophthalmology. 1991;98:1156–1163. doi: 10.1016/s0161-6420(91)32157-2. [DOI] [PubMed] [Google Scholar]
- 5.Epstein D, Fagerholm P, Hamberg-Nystrom H, Tengroth B. Twenty-four-month follow-up of excimer laser photorefractive keratectomy for myopia; refractive andvisual acuity results. Ophthalmology. 1994;101:1558–1563. doi: 10.1016/s0161-6420(94)31150-x. [DOI] [PubMed] [Google Scholar]
- 6.Dutt S, Steinert RF, Raizman MB, Puliafito CA. One year results of excimer laser photorefractive keratectomy for low to moderate myopia. Arch Ophthalmol. 1994;112:1427–1436. doi: 10.1001/archopht.1994.01090230041018. [DOI] [PubMed] [Google Scholar]
- 7.Ambrósio R, Jr, Wilson S. LASIK vs LASEK vs PRK: Advantages and indications. Semin Ophthalmol. 2003;18:2–10. doi: 10.1076/soph.18.1.2.14074. [DOI] [PubMed] [Google Scholar]
- 8.Steinert RF, Bafna S. Surgical correction of moderate myopia: Which method should you choose? II. PRK and LASIK are the treatments of choice. Surv Ophthalmol. 1998;43:157–179. doi: 10.1016/s0039-6257(98)00027-7. [DOI] [PubMed] [Google Scholar]
- 9.Assouline M, Renard G, Arne JL, David T, Lasmolles C, Malecaze F, et al. A prospective randomized trial of topical soluble 0.1% indomethacin versus 0.1% diclofenac versus placebo for the control of pain following excimer laser photorefractive keratectomy. J Ophthalmic Surg Lasers. 1998;29:365–374. [PubMed] [Google Scholar]
- 10.McCarty CA, Garrett SK, Aldred GF, Taylor HR. Assessment of subjective pain following photorefractive keratectomy. Melbourne Excimer Laser Group. J Refract Surg. 1996;12:365–369. doi: 10.3928/1081-597X-19960301-11. [DOI] [PubMed] [Google Scholar]
- 11.Gimbel HV, DeBroff BM, Beldavs RA, van Westenbrugge JA, Ferensowicz M. Comparison of laser and manual removal of corneal epithelium for photorefractive keratectomy. J Refract Surg. 1995;11:36–41. doi: 10.3928/1081-597X-19950101-10. [DOI] [PubMed] [Google Scholar]
- 12.Fadlallah A, Fahed D, Khalil K, Dunia I, Menassa J, El Rami H, et al. Transepithelial photorefractive keratectomy: Clinical results. J Cataract Refract Surg. 2011;37:1852–1857. doi: 10.1016/j.jcrs.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 13.Aslanides IM, Padroni S, Arba Mosquera S, Ioannides A, Mukherjee A. Comparison of single-step reverse Transepithelial all-surface laser ablation (ASLA) to alcohol-assisted photorefractive keratectomy. Clin Ophthalmol. 2012;6:973–980. doi: 10.2147/OPTH.S32374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bar Dayan Y, Levin A, Morad Y, Grotto I, Ben-David R, Goldberg A, et al. The changing prevalence of myopia in young adults: A 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci. 2005;46:2760–2765. doi: 10.1167/iovs.04-0260. [DOI] [PubMed] [Google Scholar]
- 15.Fantes FE, Hanna KD, Waring GO. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990;108:665–675. doi: 10.1001/archopht.1990.01070070051034. [DOI] [PubMed] [Google Scholar]
- 16.Koch D, Kohnen T, Obstbaum S. Format for reporting refractive surgical data. J Cataract Refract Surg. 1998;24:285–287. doi: 10.1016/s0886-3350(98)80305-2. [DOI] [PubMed] [Google Scholar]
- 17.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advance keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 18.Rouland JJ, Courtas D, Labalette P, Margaron F, Cailliau D. Influence of meteorological parameters on wound healing after photorefractive keratectomy (PRK) Invest Ophthalmol Vis Sci. 2003;44:3843. [Google Scholar]
- 19.Lee JB, Seong GJ, Lee JH, Seo KY, Lee YG, Kim EK. Comparison of laser epithelial keratomileusis and photorefractive keratectomy for low to moderate myopia. J Cataract Refract Surg. 2001;27:565–570. doi: 10.1016/s0886-3350(00)00880-4. [DOI] [PubMed] [Google Scholar]
- 20.Carones F, Fiore T, Brancato R. Mechanical vs alcohol epithelial removal during photorefractive keratectomy. J Refract Surg. 1999;15:556–562. doi: 10.3928/1081-597X-19990901-08. [DOI] [PubMed] [Google Scholar]
- 21.McCarty CA, Garrett SK, Aldred GF, Taylor HR. Assessment of subjective pain following photorefractive keratectomy. Melbourne Excimer Laser Group. Refract Surg. 1996;12:365–369. doi: 10.3928/1081-597X-19960301-11. [DOI] [PubMed] [Google Scholar]


