Abstract
Phakic intraocular lenses revolutionize refractive surgery and continue to serve as an excellent option for vision correction in patients who are not ideal candidates for laser vision correction. This article will review special indications of phakic intraocular lenses in the clinical practice.
Keywords: Anterior Chamber, Intraocular Lens, Phakic, Posterior Chamber, Special Indications
INTRODUCTION
Phakic intraocular lenses (PIOLs) are clear implantable lenses that are surgically placed either in anterior chamber (AC) or posterior chamber (PC) without removing the natural lens, enabling light to focus on the retina for improved uncorrected visual acuity.[1] PIOLs demonstrate high optical quality and potential gain in visual acuity in myopic patients due to retinal magnification.[2] Correction is not limited by corneal thickness or topography; faster visual recovery and stable refraction are expected.[2,3] As a reversible refractive procedure that preserves accommodative function, PIOL implantation is attractive to both patients and refractive surgeons.[4,5]
INDICATIONS
The principal indication for PIOLs is correction of myopia or myopic astigmatism beyond the range of laser vision correction (LVC).[1]
LOCATION
Three locations for PIOLs have been described. These include: anterior chamber angle-fixated PIOL; anterior chamber iris-fixated PIOL; and posterior chamber PIOL. More specifically, PIOLs approved by Food and Drug Administration (FDA) include iris-fixated PIOL and posterior chamber PIOL for myopia correction.[6,7] Toric PIOLs are also available outside the United States to correct both myopia and astigmatism.[8]
PREREQUISITES FOR PHAKIC INTRAOCULAR LENSES
General criteria should be followed for good predictability and safety. These include: Age >21 years; stable refraction (less than 0.5D change for 1 year); clear crystalline lens; ametropia not appropriate for excimer laser surgery; unsatisfactory vision with contact lenses or spectacles; appropriate pupil size for the specified PIOL; adequate anterior chamber depth (ACD); minimum endothelial cell count (ECC) specified for each PIOL; no ocular pathology such as compromised corneal endothelium, iritis, iris atrophy, rubeosis iridis, cataract, glaucoma, and retinal disorders.[8]
Ancillary Testing
Additional ancillary tests are necessary when using PIOLs such as specular microscopy or confocal microscopy to evaluate ECC and morphology looking for polymegathism and pleomorphism;[9] ACD measurement can be done by ultrasound, anterior segment optical coherence tomography (AS-OCT), optical biometry, slit beam topography, or Scheimpflug imaging,[6,7,10] White-to-white (WTW) diameter is mandatory for selection of the PIOL diameter. However, the best method to measure sulcus-to-sulcus distance is high frequency ultrasound. Other methods such as AS-OCT; slit-beam topography or Scheimpflug imaging can also be used to estimate the sulcus-to-sulcus distance by measuring the WTW diameter and adding 0.5 mm.[11,12]
ANTERIOR CHAMBER IRIS-FIXATED PHAKIC INTRAOCULAR LENSES
Artisan/Verisyse™ and Artiflex/Veriflex™ PIOL [Figures 1 and 2].
Figure 1.

Artisan/Verisyse PIOl (Abbott Medical Optics, Santa Ana, California, USA).
Figure 2.

Artiflex/Veriflex PIOl (Abbott Medical Optics, Santa Ana, California, USA).
The Artisan lens, marketed as the Verisyse lens (Abbott Medical Optics, Santa Ana, California, USA), is available for correction of myopia in a power range of −3.00 D to −23.50 D and hyperopia in a power range of 1.00 D to 12.00 D.[13] This PIOL has a fixed overall length of 8.5 mm (7.5 mm for pediatric group) made of PMMA with a 5 or 6 mm optic, requiring an entry wound of 5 to 6 mm. It is designed to be placed within the anterior chamber with fine claws in the haptic incorporating iris tissue to hold the IOL in place in a process called “enclavation.” Since this type of PIOL is fixated to the midperipheral iris, it is available in “one-size-fits-all” length. Although the vaulted configuration of the Artisan/Verisyse is designed to ensure a normal aqueous flow, a peripheral iridectomy is necessary to avoid pupillary block glaucoma.[14] This PIOL can be centered over the pupil even if pupil is off center. The iris claw fixation system in the midperiphery also results in total fixation with no rotation on the PIOL, and therefore ideal for the toric versions. For safe implantation of the Artisan PIOL, the anterior chamber depth should be at least larger than 2.8 mm measured from corneal endothelium to the anterior surface of the crystalline lens, and the distance between the PIOL and the endothelium in the periphery must be at least 1.5 mm.[10,15] A minimal endothelial cell density is required according to age: 18 to 25 years of age = 2800 cells/mm2; 26 to 30 years of age = 2650 cells/mm2; 31 to 35 years of age = 2400 cells/mm2; 36 to 45 years of age = 2200 cells/mm2; >45 years of age = 2000 cells/mm2.[3,10,16] The Artisan PIOL is contraindicated in patients with: endothelial cell counts <2000 cell/mm2; ACD <2.8 mm; glaucoma; patients with a history of retinal detachment, macular degeneration or retinopathy; any form of cataract; recurrent or chronic iritis; a fixed pupil size >4.5 mm or scotopic pupil size > 6.0 mm (5 mm PIOL optic) or 7.0 mm (6 mm PIOL optic); convex, bulging or volcano shaped iris; corneal pathology, and age <18 years and pregnancy.[6,7]
The Artiflex/Veriflex Phakic IOLs are foldable models. These iris-fixated PIOL are made of a flexible material and can be inserted through a small, self-sealing wound of approximately 3 mm having the advantage of minimizing surgically induced astigmatism.[17,18] The overall length is 8.5 mm and powers range from −2.0 D to 14.5 D in 0.5 D steps. Toric PIOL designs are also available to enable spherocylindrical correction.[19] The dioptric power range of Artiflex/Veriflex toric PIOL includes a spherical correction from −1.0 D to −13.5 D in combination with a cylindrical correction from −1.0 D to −5.0 D. For safe implantation of Artiflex PIOL, the anterior chamber depth should be at least larger than 3.0 mm measured from corneal endothelium to the anterior surface of the crystalline lens.[13,18] The contraindications reviewed above for the Artisan PIOL also apply to the Artiflex PIOL. A vacuum enclavation system VacuFix is available for all Artisan and Artiflex models. Using the vacuum of a phaco machine and a tip with an aspiration hole, controlled grasping of iris tissue allows an optimal position and centration. Curved VacuFix tips allow an easier reach of the enclavation site especially when working with toric PIOLs.
POSTERIOR CHAMBER PHAKIC INTRAOCULAR LENSES
Visian Implantable Collamer Lens (ICL) STAAR Surgical [Figures 3 and 4]; Epi.Lens, Acri.Tec (Carl Zeiss Meditec, Jena, Germany).
Figure 3.
ICL (STAAR Surgical, Monrovia, CA, USA).
Figure 4.
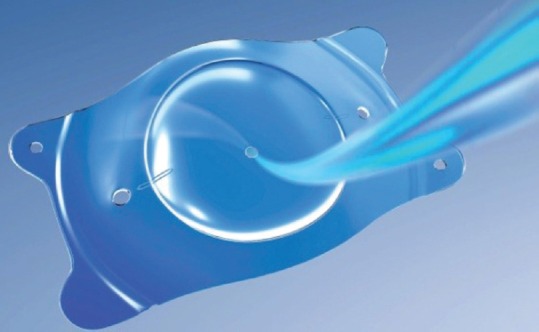
ICL V4c CentraFLOW technology (STAAR Surgical, Monrovia, CA, USA).
The ICL is the most implanted posterior chamber PIOL for correction of myopia ranging from −3.0 D to −23.0 D.[20] It is a rectangular single-block made of collamer and available in 4 diameters (12.1 mm; 12.6 mm; 13.2 mm; 13.7 mm), with the variable optical zone depending on the optical power (4.65 to 5.8 mm for negative lenses and 5.5 mm for positive lenses). The PIOL is foldable and can be injected through an incision size of 3.2 mm. Once delivered into the anterior chamber, four footplates of the lens are tucked under the iris into the sulcus. The Visian ICL 4 model implantation requires two peripheral iridotomies prior to surgery to prevent pupillary block glaucoma although often a single peripheral iridectomy is all that is needed. The ICL is designed as a sulcus-supported lens and for this reason; sulcus-to-sulcus distance is mandatory for an appropriate selection of the lens diameter. The correct lens size is correlated to the amount of vaulting of the lens optic over the crystalline lens, which should be 1.0 + 0.5 corneal thickness to reduce complications.[21] Outside the USA, the Visian ICL is also available for correcting hyperopic error ranging from +3.00 D to +12.00 D. A toric ICL design also enables spherocylindrical correction ranging spherical powers in 0.5 D steps from −3.00 D to −20.00 D with astigmatism correction up to 6 D in 0.5 D steps.
A new ICL model with a central hole (ICL V4c STAAR Surgical) is available in Europe for correcting myopia with equal safety, efficacy and predictability. The central 360 micrometer hole, called KS-Aquaport, differentiates ICL V4c from the conventional ICL V4b.CentraFLOW technology allows a more natural flow of aqueous humor, eliminating the need for an iridectomy.[22] Toric PIOLs with the CentraFLOW technology are also available and enable spherocylindrical correction. The ICL has axis marks at specific meridians. It is designed to be aligned with the 180-degree meridian, with only a minor adjustment.[14,22] For a safe implantation, STAAR recommends a minimal ECC according to age and ACD of 3.2 mm: 21 to 25 years of age = 3800 cells/mm2; 26 to 30 years of age = 3375 cells/mm2; 31 to 35 years of age = 2975 cells/mm2; 36 to 40 years of age = 2625 cells/mm2; 41 to 45 years of age = 2325 cells/mm2; >45 years of age = 2050 cells/mm2.[23,24,25] The STAAR ICL PIOL is contraindicated when: anterior chamber depth (ACD) <3.0 mm; anterior chamber angle < grade II; inadequate ECC and pregnancy.[23,24,26,27]
ANTERIOR CHAMBER ANGLE-FIXATED PHAKIC INTRAOCULAR LENSES
Alcon AcrySof Cachet Phakic IOL [Figures 5 and 6].
Figure 5.
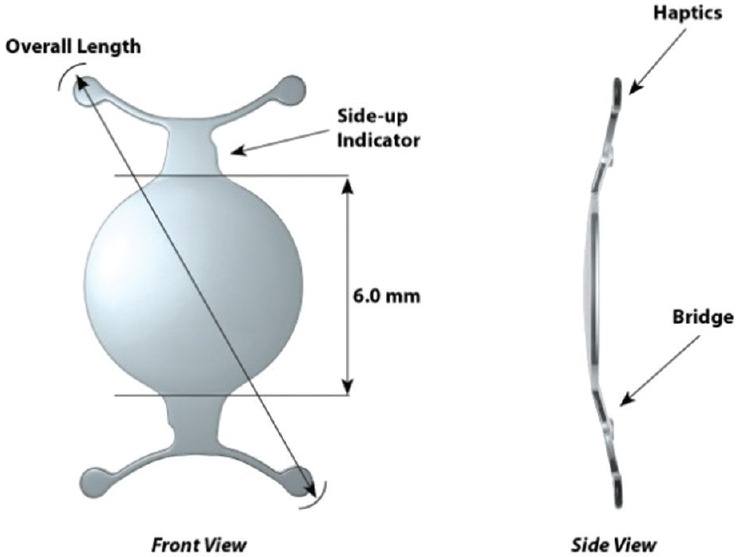
Acrysof cachet PIOL (Alcon laboratories, Inc, Fort Worth, TX, USA).
Figure 6.
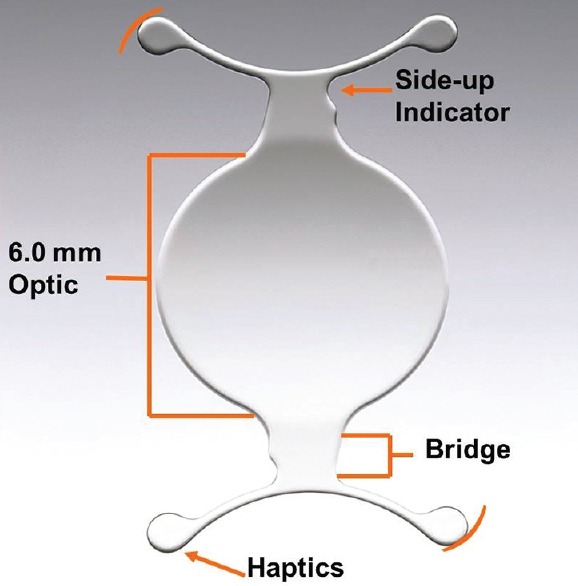
Acrysof cachet PIOL (Alcon laboratories, Inc, Fort Worth, TX, USA).
The most recent angle supported lens is the AcrySof Cachet (Alcon Laboratories, Inc., Fort Worth, TX, USA). The AcrySof Cachet is a single piece foldable hydrophobic acrylic lens that can be implanted in the anterior chamber through a 2.6 mm clear corneal incision. It is designed to achieve predictable positioning in the AC, stable vaulting and low compression forces on the irido-corneal angle. This lens can be used for correcting myopia ranging from −6.00 D to −16.50 D and is available in 0.5 D increments. It has a meniscus type optic with a 6.0 mm optic diameter and 12.5 mm overall length.[28]
SPECIAL INDICATIONS FOR PHAKIC INTRAOCULAR LENSES
Phakic Intraocular Lenses in Keratoconus
Stable keratoconus
PIOLs can be used to correct myopia and compound myopic astigmatism in eyes with keratoconus (KCN), which has been stable for 2 years. PIOL implantation is a suitable refractive surgical option for stable KCN. It may be especially indicated for the management of high ametropia[29] and Toric PIOL implantation is beneficial according to measures of safety, efficacy, predictability and stability for KCN. The refractive stability suggests viability of the procedure as a surgical option.[30] A study from Tokyo, Japan (Minamiaoyama Eye Clinic) which was conducted between May 2005 and December 2007 demonstrated that PIOL implantation is a good option for correction of refractive error of KCN when BSCVA is not affected.[30,31]
Unstable keratoconus
Topographic stability can be achieved by collagen crosslinking (CXL) and intrastromal corneal ring segments (ICRS). Combined CXL, ICRS and PIOL implantation is a safe, predictable and effective treatment in eyes with progressive KCN. Favorable results can be assessed in terms of visual acuity, postoperative residual refractive error, and keratometry values.[31,32]
Clinical studies have demonstrated significant improvement in unaided visual performance with good safety for toric PIOLs. Such treatment modalities offer an alternative in selected contact lens intolerant KCN patients for treating myopic astigmatism before considering corneal transplantation. Further refinements in positioning and implantation of toric PIOLs and pre-operative assessments may allow the greater use of refractive techniques for the future management of unstable KCN. Furthermore, in advanced KCN, deep anterior lamellar keratoplasty (DALK) can be performed followed by PIOL for residual refractive error.[33]
Phakic Intraocular Lenses Post-corneal Transplant
A successful corneal graft requires both clarity and an acceptable refraction. A clear corneal graft may be an optical failure if high astigmatism or spherical error limits visual acuity. PIOLs can be implanted post-keratoplasty with adequate ECC and ACD. Posterior chamber PIOLs are usually preferred over anterior chamber PIOLS to avoid endothelium decompensation and allow small incision size. PIOLs are a versatile option for correcting high refractive errors, resulting in improved unaided and best-corrected visual acuity, as well as rapid visual rehabilitation. Studies indicate that PIOL implantation is a viable treatment for refractive error after keratoplasty in patients who are intolerant to contact lens and LVC are contraindicated. However, LVC for high refractive error correction can be unpredictable post corneal transplant.[34]
Correction of Residual Refraction in Pseudophakia
Implantation of the PIOL has also been found to be an effective and predictable option for enhancing postoperative refractive results and reducing spectacle dependence after cataract surgery.[35] Piggyback insertion of a PIOL appears to be effective and predictable in correcting refractive error in pseudophakic eyes. Piggyback implantation can be performed as a primary or secondary surgical procedure. Principal indications being primary hyperopia, symptomatic pseudophakic hyperopia, and symptomatic pseudophakic myopia. PIOLs can be implanted in the anterior chamber; ciliary sulcus and capsular bag. Limitations are interlenticular opacities (ILO); iris chafing; pigment dispersion; and IOL dislocation. Implantation of a phakic posterior chamber IOL may be an alternative to currently available methods of managing pseudophakic ametropia.[36,37]
The Role of Phakic Intraocular Lenses in Presbyopia
Presbyopia implantable phakic contact lens
Correcting presbyopia is an essential challenge for refractive surgeons. This is not so much to do with restoring accommodation, but more a question of giving patients an opportunity of living without spectacles for distant and near vision. This opens the door to a number of alternatives to real accommodation surgery.[38] A recent advancement in presbyopia correction is a multifocal implantable phakic refractive IOL [Presbyopia Implantable Phakic Contact Lens (IPCL)]. This Novel PC-PIOL is for correction of presbyopia in patients aged between 40 and 55 years without cataract in addition to myopia, hyperopia and astigmatism ranges from +10D to − 25D, 8D cylinder with near additions between +1.50D and +3.50D. IPCL is a hydrophilic acrylic lens, which can be inserted through a 2.8 mm incision. The advantage of the PC-PIOL is reversibility of the procedure with good unaided vision. Limitations are optical defects, decreased contrast sensitivity, haloes, as well as the usual PIOL complications. Long-term outcomes are required to assess the safety and efficacy for this new PC-PIOL.[39]
Phakic Intraocular Lenses Post-laser Vision Correction
The advantages of this technique are straight forward. The PIOL corrects residual refraction post LVC. It eliminates dependency on CL and glasses and it is the treatment of choice if LVC enhancement is contraindicated. Additionally, there are less optical defects, less aberrations, better contrast sensitivity and improved quality of vision.
PHAKIC INTRAOCULAR LENSES IN THE PEDIATRIC AGE GROUP
Pediatric refractive surgery was developed with the aim of finding a solution for those cases of amblyopia where compliance is poor and conventional treatments are ineffective. PIOL can be implanted to correct high anisometropia in amblyopic children who were non-compliant with traditional medical treatment including spectacles or contact lenses, due to social circumstances or neurobehavioral disorders.[40] The principal indications are high myopic or hyperopic anisometropia; bilateral high ametropia; and secondary high refractive amblyopia.
When refractive surgery is considered for treating a case of anisometropic ametropia with severe amblyopia, the associated refractive error is normally high in the affected eye, −10.00 D of myopia or 6.00 D of hyperopia. For this reason, excimer laser refractive surgery is not possible in a great number of patients because significantly large amounts of tissue ablation would be required, which can lead to corneal biomechanical instability and/or an increase in corneal higher order aberrations resulting in decreased visual quality. PIOL implantation is a good option in such cases because these types of lenses have proven to provide excellent visual recovery and postoperative visual quality. Potential complication is intraocular surgery in children is more prone to inflammation. An additional important factor to be considered is the myopic shift that occurs as the patient ages, particularly with lens implantation in young children or in cases with high myopia. Additional correction with glasses or contact lenses may be necessary over time, or in extreme cases, the PIOL can be exchanged. Before considering PIOL implantation in pediatric patients, the risks, benefits and alternatives, as well as the necessity for long-term follow-up should be carefully weighed. Careful patient selection and follow-up of these patients in order to monitor the corneal endothelium is essential, as well as instructions to the parents. Eye rubbing should be avoided. Different models of IOLs have been successfully implanted in children with severe anisometropic amblyopia, but concern remains regarding unforeseen long-term side effects.[41,42]
SUMMARY
Several studies have demonstrated that The Artisan/Verisyse, Artiflex/Veriflex and Visian ICL have a good predictability, stability, and long term safety. While the learning curve is lower with the Visian ICL, there is a possibility of lens exchange due to incorrect size and vaulting problems. Lenses made of PMMA require a larger wound and significant induced astigmatism is expected. Several models are available and recent application of PIOLS for stable KCN, KCN with CXL and ISCRS, post-keratoplasty and presbyopia have been reported with good results. With precautions taken, we believe that the improvements in lens designs and implantation techniques and publication of long term clinical results have led to greater adoption and use of PIOLS for a variety of indications. Realizing that LVC alone cannot address all refractive errors, multiple options are now available and more will likely be on the way. The surgeons must use their experience, and published data to decide which PIOL to choose for the appropriate patient's circumstance.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Moya T, Javaloy J, Montés-Micó R, Beltrán J, Muñoz G, Montalbán R. Implantable collamer lens for myopia: Assessment 12 years after implantation. J Refract Surg. 2015;31:548–556. doi: 10.3928/1081597X-20150727-05. [DOI] [PubMed] [Google Scholar]
- 2.El Danasoury MA, El Maghraby A, Gamali TO. Comparison of iris-fixed Artisan lens implantation with excimer laser in situ keratomileusis in correcting myopia between -9.00 and -19.50 diopters: A randomized study. Ophthalmology. 2002;109:955–964. doi: 10.1016/s0161-6420(02)00964-8. [DOI] [PubMed] [Google Scholar]
- 3.Alio JL, Peña-García P, Pachkoria K, Alio JL, 2nd, El Aswad A. Intraocular optical quality of phakic intraocular lenses: Comparison of angle-supported, iris-fixated, and posterior chamber lenses. Am J Ophthalmol. 2013;156:789–799. doi: 10.1016/j.ajo.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Joosse MV, Snoek C, van Minderhout HM. Comparison of wavefront-guided photorefractive keratectomy and foldable iris-fixated phakic intraocular lens implantation for low to moderate myopia. J Cataract Refract Surg. 2011;37:370–377. doi: 10.1016/j.jcrs.2010.08.051. [DOI] [PubMed] [Google Scholar]
- 5.Schechter RJ. Image magnification, contact lenses, and visual acuity. Ann Ophthalmol. 1978;10:1665–1668. [PubMed] [Google Scholar]
- 6.Menezo JL, Peris-Martinez C, Cisneros AL, Marti´nez-Costa R. Phakic intraocular lenses to correct high myopia: Adatomed, Staar, and Artisan. J Cataract Refract Surg. 2004;30:33–44. doi: 10.1016/j.jcrs.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 7.Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, et al. Phakic intraocular lens implantation for the correction of myopia: A report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:2244–2258. doi: 10.1016/j.ophtha.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Fechner PU, Strobel J, Wichmann W. Correction of myopia by implantation of a concave Worst-iris claw lens into phakic eyes. Refract Corneal Surg. 1991;7:286–298. [PubMed] [Google Scholar]
- 9.Fechner PU, Heijde GL van der, Worst JG. Intraocular lens for the correction of myopia of the phakic eye. Klin Monatsbl Augenheilkd. 1988;193:29–34. doi: 10.1055/s-2008-1050218. [DOI] [PubMed] [Google Scholar]
- 10.Doors M, Cals DW, Berendschot TT, de Brabander J, Hendrikse F, Webers CA, et al. Influence of anterior chamber morphometrics on endothelial cell changes after phakic intraocular lens implantation. J Cataract Refract Surg. 2008;34:2110–2118. doi: 10.1016/j.jcrs.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 11.Baikoff G. Anterior segment OCT and phakic intraocular lenses: A perspective. J Cataract Refract Surg. 2006;31:1827–1835. doi: 10.1016/j.jcrs.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 12.Baikoff G, Lutun E, Ferraz C, Wei J. Analysis of the eye's anterior segment with optical coherence tomography. Static and dynamic study. J Fr Ophtalmol. 2005;28:343–352. doi: 10.1016/s0181-5512(05)81064-2. [DOI] [PubMed] [Google Scholar]
- 13.Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN, Thompson VM. U.S. Verisyse Study Group. Three-year results of Artisan/Verisyse phakic intraocular lens implantation. Results of the United States Food And Drug Administration clinical trial. Ophthalmology. 2008;115:464–472. doi: 10.1016/j.ophtha.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 14.Hassaballa MA, Macky TA. Phakic intraocular lenses outcomes and complications: Artisan vs Visian ICL. Eye. 2011;25:1365–1370. doi: 10.1038/eye.2011.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Budo C, Hessloehl JC, Izak M, Luyten GP, Menezo JL, Sener BA, et al. Multicenter study of the Artisan phakic intraocular lens. J Cataract Refract Surg. 2000;26:1163–1171. doi: 10.1016/s0886-3350(00)00545-9. [DOI] [PubMed] [Google Scholar]
- 16.Kohnen T, Kook D, Morral M, Güell JL. Phakic intraocular lenses: Part 2: Results and complications. J Cataract Refract Surg. 2010;36:2168–2194. doi: 10.1016/j.jcrs.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Izák M. Surgical Trauma, not Lens Design, Responsible for Myopia Claw IOL Irritation. Ocular Surgery News. 1998;38 [Google Scholar]
- 18.Coullet J, Guëll JL, Fournié P, Grandjean H, Gaytan J, Arné JL, et al. Iris-supported phakic lenses (rigid vs foldable version) for treating moderately high myopia: Randomized paired eye comparison. Am J Ophthalmol. 2006;142:909–916. doi: 10.1016/j.ajo.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 19.Dick HB, Budo C, Malecaze F, Güell JL, Marinho AA, Nuijts RM, et al. Foldable Artiflex phakic intraocular lens for the correction of myopia: Two-year follow-up results of a prospective European multi-center study. Ophthalmology. 2009;116:671–677. doi: 10.1016/j.ophtha.2008.12.059. [DOI] [PubMed] [Google Scholar]
- 20.Ghoreishi M1, Masjedi A, Nasrollahi K, Rahgozar A, Jenab K, Fesharaki H. Artiflex versus STAAR® implantable contact lenses for correction of high myopia. Oman J Ophthalmol. 2011;4:116–119. doi: 10.4103/0974-620X.91266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boxer Wachler BS, Scruggs RT, Yuen LH, Jalali S. Comparison of the Vision ICL and Verisyse phakic intraocular lenses for myopia from 6.00 to 20.00D. J Refract Surg. 2009;25:765–770. doi: 10.3928/1081597X-20090813-02. [DOI] [PubMed] [Google Scholar]
- 22.Higeros-Esteban A, Ortiz-Gomariz A, Gutierés-Ortega R, Villa-Collar, Abad-Montes JP, Fernandes P, et al. Intraocular pressure after implantation of the Vision Implantable Collamer Lens With Centra-FLOW without iridotomy. Am J Ophthalmology. 2013;156:800–805. doi: 10.1016/j.ajo.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 23.Sanders DR, Vukich JA, Doney K, Gaston M. Food and Drug Administration Clinical trial of the Implantable Contact Lens for moderate to high myopia. Ophthalmology. 2003;110:255–266. doi: 10.1016/s0161-6420(02)01771-2. [DOI] [PubMed] [Google Scholar]
- 24.Gimbel, Howard V, et al. Management of myopic astigmatism with phakic intraocular lens implantation. J Cataract Refract Surg. 2004;28:883–886. doi: 10.1016/s0886-3350(01)01098-7. [DOI] [PubMed] [Google Scholar]
- 25.Dejaco-Ruhswurm I, Scholz U, Pieh S, Hanselmayer G, Lackner B, Italon C, et al. Long-term endothelial changes in phakic eyes with posterior chamber intraocular lenses. J Cataract Refract Surg. 2002;28:1589–1593. doi: 10.1016/s0886-3350(02)01210-5. [DOI] [PubMed] [Google Scholar]
- 26.Sanders DR, Doney K, Poco M. United States Food and Drug Administration clinical trial of the Implantable Collamer Lens (ICL) or moderate to high myopia: Three-year follow-up. Ophthalmology. 2004;111:1683–1692. doi: 10.1016/j.ophtha.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 27.Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M. Four year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009;127:845–850. doi: 10.1001/archophthalmol.2009.67. [DOI] [PubMed] [Google Scholar]
- 28.Mastropasqua L, Toto L, Vecchiarino L, Doronzo E, Mastropasqua R, Di Nicola M. AcryS of cachet phakic intraocular lens in myopic patients: visual performance, wavefront error, and lens position. J Refract Surg. 2012;28:267–274. doi: 10.3928/1081597X-20120222-01. [DOI] [PubMed] [Google Scholar]
- 29.Alio JL, Sanz-Diez P. Phakic Intraocular lenses in Keratoconus. Int J Kerat Ect Cor Dis. 2015;4:103–106. [Google Scholar]
- 30.Kamiya K, Shimizu K, Kobashi H, Igarashi A, Komatsu M, Nakamura A, et al. Three-year follow-up of posterior chamber toric phakic intraocular lens implantation for the correction of high myopic astigmatism in eyes with keratoconus. Br J Ophthalmol. 2015;99:2:177–183. doi: 10.1136/bjophthalmol-2014-305612. [DOI] [PubMed] [Google Scholar]
- 31.Naoko Kato, MD, Ikuko Toda, MD, Yoshiko Hori-Komai, MD, Chikako Sakai, BS, Hiroyuki Arai, MD, Kazuo Tsubota., MD Phakic Intraocular Lens for Keratoconus; AJO. 2011 Mar;118(3):605–605-e2. doi: 10.1016/j.ophtha.2010.08.043. [DOI] [PubMed] [Google Scholar]
- 32.Izquierdo L, Jr, Henriquez MA, McCarthy M. Artiflex phakic intraocular lens implantation after corneal collagen cross-linking in keratoconic eyes. J Refract Surg. 2011;27:482–487. doi: 10.3928/1081597X-20101223-02. [DOI] [PubMed] [Google Scholar]
- 33.Hashem AN, El Danasoury AM, Anwar HM. Axis alignment and rotational stability after implantation of the toric implantable collamer lens for myopic astigmatism. J Refract Surg. 2009;25:S939–S943. doi: 10.3928/1081597X-20090915-08. [DOI] [PubMed] [Google Scholar]
- 34.Alfonso JF, Lisa C, Abdelhamid A, Montés-Micó R, Poo-López A, Ferrer-Blasco T. Posterior chamber phakic intraocular lenses after penetrating keratoplasty. J Cataract Refract Surg. 2009;35:1166–73. doi: 10.1016/j.jcrs.2009.02.027. doi: 10.1016/j.jcrs.2009.02.027. [DOI] [PubMed] [Google Scholar]
- 35.Chiou AG, Bovet J, de Courten C. Pseudophakic ametropia managed with a phakic posterior chamber intraocular lens. J Cataract Refract Surg. 2001;27:1516–1518. doi: 10.1016/s0886-3350(00)00858-0. [DOI] [PubMed] [Google Scholar]
- 36.Falzon K, Stewart OG. Correction of undesirable pseudophakic refractive error with the Sulcoflex intraocular lens. J Refract Surg. 2012;28:619. doi: 10.3928/1081597X-20120809-01. [DOI] [PubMed] [Google Scholar]
- 37.Kahraman G, Amon M. New supplementary intraocular lens for refractive enhancement in pseudophakic patients. J Cataract Refract Surg. 2010;36:1090–1094. doi: 10.1016/j.jcrs.2009.12.045. [DOI] [PubMed] [Google Scholar]
- 38.Garg A. Multifocal Phakic Implant For Presbyopia Correction. Journal of the Bombay Ophthalmologists' Association. 2005:14–2. [Google Scholar]
- 39.Monte-Mico R, Alio J. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg. 2003;29:703–711. doi: 10.1016/s0886-3350(02)01648-6. [DOI] [PubMed] [Google Scholar]
- 40.Tychsen L, Hoekel J, Ghasia F, Yoon-Huang G. Phakic intraocular lens correction of high ametropia in children with neurobehavioral disorders. J AAPOS. 2008;12:282–289. doi: 10.1016/j.jaapos.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 41.Pirouzian A, Ip KC, O’Halloran HS. Phakic anterior chamber intraocular lens (Verisyse™) implantation in children for treatment of severe ansiometropia myopia and amblyopia: Six-month pilot clinical trial and review of literature. Clin Ophthalmol. 2009;3:367–371. doi: 10.2147/opth.s5710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pirouzian A. Pediatric phakic intraocular lens surgery: Review of clinical studies. Curr Opin Ophthalmol. 2010;21:249–254. doi: 10.1097/ICU.0b013e32833a9a9f. [DOI] [PubMed] [Google Scholar]


