Abstract
Purpose:
To report a case of conjuctival leiomyoma.
Case Report:
An 18-year-old female patient presented with a conjunctival growth in the left eye for a 2-year-period with no change in size. She merely presented for cosmetic reasons. Visual acuity was 20/20 in each eye. The lesion had prominent vessels and was not adherent to the sclera. The growth resembled a benign lesion of the conjunctiva. The tough and vascular tissue was excised and sent for histopathology. The defect was covered by an end to end conjunctival suturing. Histopathology showed the lesion to be conjunctival leiomyoma. Trichome was used to highlight the spindle shaped cells and immuno-histochemistry using anti-smooth muscle actin antibody and Vimentin was applied to confirm the diagnosis.
Conclusion:
This case adds to the total number of cases of conjuctival leiomyoma reported in the literature to date. An ophthalmologist needs to think beyond a common mass when encountering a conjunctival growth extending onto the cornea.
Keywords: Benign, Conjuctival, Leiomyoma, Pterygium
INTRODUCTION
The etiology of conjuctival growths can be very diverse and the histology of lesions can come as a surprise to the ophthalmologists. It is extremely rare to find leiomyoma in the histology of a conjuctival growth; leiomyomas mainly develop in the uterus.[1]
Leiomyoma is a benign tumor that usually arises from the smooth muscles of the stomach, vascular tissue, large and small intestine, subcutaneous tissue and uterus. Orbital leiomyoma has been reported since 1896.[2] The present patient, to the best of our knowledge, is the third case of conjunctival leiomyoma reported in the literature to date. Our aim is to highlight the rare occurrence of conjuctival leiomyoma.
CASE REPORT
An 18-year-old girl presented to the outpatient department complaining of a conjunctival mass in her left eye, which was stable in size for the past 2 years and was not associated with irritation or bleeding. Past history was unremarkable regarding ocular trauma, surgery, or infection. The patient merely presented for cosmetic reasons. Examination revealed visual acuity of 20/20 in both eyes. The left eye had a sessile, nodular conjunctival growth which seemed to be originating from the plica semilunaris and extending towards the nasal limbus [Figure 1]. It had prominent blood vessels and was not adherent to the sclera. The rest of the ocular examination was unremarkable in both eyes. There was no complaint of diplopia; the extra ocular movements were full in all directions in both eyes. The conjunctival growth looked like a benign lesion. She was scheduled for excisional biopsy. The tough and vascular tissue was excised and sent for histopathology and the defect was covered by an end to end conjunctival suturing. Histopathology revealed the lesion to be a leiomyoma [Figures 2 and 3]. On the cut section, the stroma was collagenous and the lesion had spindle shaped cells in a storiform arrangement. The spindle cells had elongated cigar shaped nuclei, clumped chromatin and scanty cytoplasm. Trichome was used to highlight the spindle shaped cells and immuno-histochemistry using anti-smooth muscle actin antibody and Vimentin was done to confirm the diagnosis [Figure 4]. Mitosis and atypia were not seen in the lesion.
Figure 1.
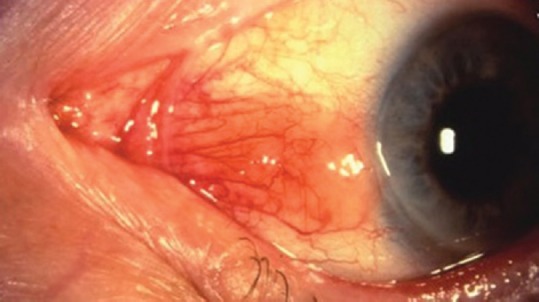
The left eye showing a sessile, nodular conjuctival growth which seems to originate from the plica semilunaris and extends towards the nasal limbus.
Figure 2.
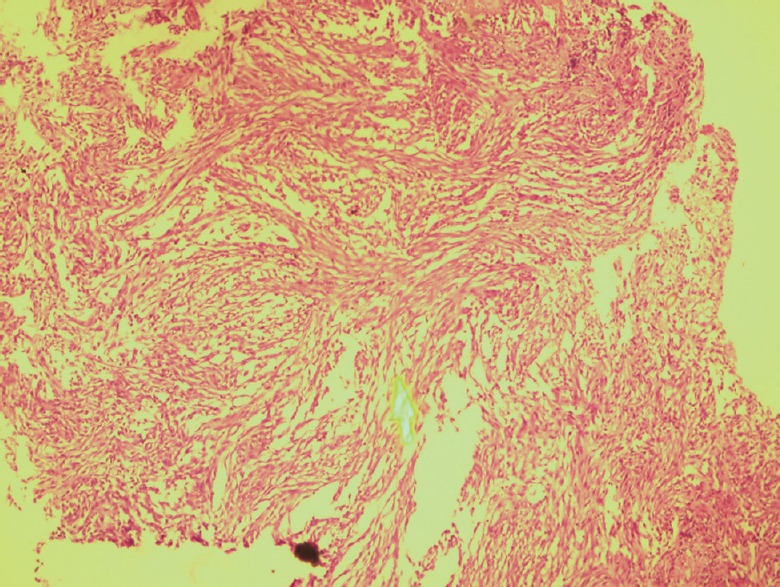
The histopathology shows the lesion to be leiomyoma. The stroma was collagenous and the lesion had spindle shaped cells having cigar shaped nuclei, in a storiform arrangement (Hematoxylin and eosin staining, ×10).
Figure 3.
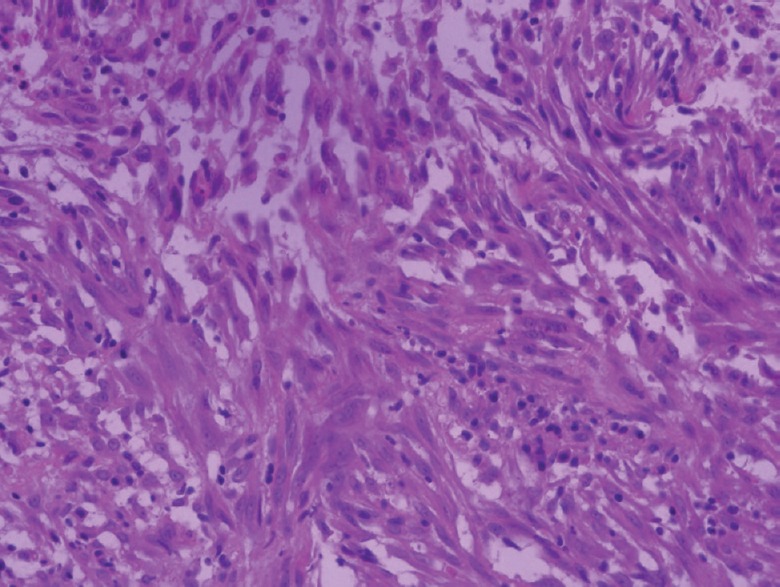
The spindle shaped cells of conjuctival leiomyoma had elongated nuclei, clumped chromatin and scanty cytoplasm (Hematoxylin and eosin staining, ×40).
Figure 4.
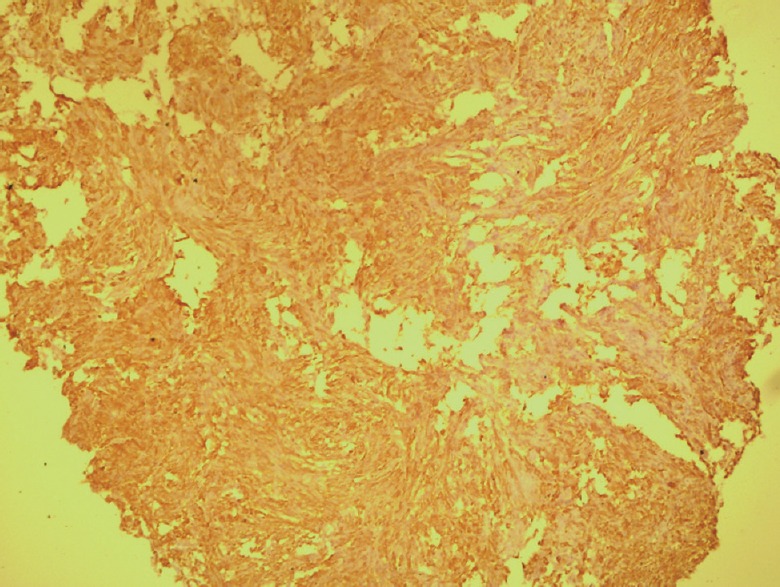
The figure shows positivity of smooth muscle fibers for SMA (smooth muscle actin) confirming the diagnosis of conjuctival leiomyoma.
DISCUSSION
Conjuctival leiomyoma is one of the rarest tumors of the eye. A MEDLINE search using keywords “Conjuctival Leiomyoma” revealed just one reported case by Brannan et al in 2003.[3] The second case report by Ghayoor et al[2] was published in a regional journal. This case adds to the total number of cases of conjuctival leiomyoma reported in the literature to date. Although leiomyoma is common elsewhere in the body, it has rarely been reported in the eye.
Leiomyoma is a benign smooth muscle tumour and can arise anywhere in the body. In more than 95% of the cases, female genital tract is involved.[4] Leiomyoma in the orbit is the most common amongst the ocular leiomyomas. It involves both the anterior and posterior parts of the orbit along with the capsulopalpebral muscle of Hessor. Orbital leiomyoma is not radio sensitive and its incomplete resection can lead to recurrence.[5] Leiomyoma has also been reported to originate from the uveal tract.[6] Ciliary body is known to be affected by leiomyoma.[3] Leiomyoma has a propensity to affect the peripheral choroid rather than the posterior choroid.[7] Heegaard and Prause reported a case of caruncle leiomyoma in 1998.[8]
In our patient, the tumor moved freely over the sclera and the ocular examination was unremarkable. Therefore, the possibility of a uveal tumor with trans-scleral spread was ruled out. However, it has been reported in literature that leiomyomas arising from the supraciliary space can spare the underlying uveal tract and erode the sclera.[3]
The differential diagnosis on histopathology includes melanotic neoplasms, peripheral nerve sheath tumors, nodular fasciitis and fibrous histiocytoma. The histology of the mentioned lesions is usually characteristic.[3] Immuno-histochemistry, in some cases, can be a useful diagnostic aid. The conjunctival leiomyoma in this case stained strongly with smooth muscle markers (anti-smooth muscle actin antibody) [Figure 4].
The conjunctival leiomyoma may arise from smooth muscles or the pericytes of the conjuctival blood vessels. Conjunctival Leiomyosarcoma has also been reported, which may originate from previous undiagnosed leiomyoma.[9] This lays emphasis on the fact that these benign lesions may turn malignant; hence follow-up of patients with conjunctival leiomyoma is mandatory.
In conclusion, it is required for a clinician to think beyond common conjunctival masses when encountering a conjunctival growth extending toward the cornea.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nath K, Shukla BR. Orbital leiomyoma and its origin. Br J Ophthalmol. 1963;47:369–371. doi: 10.1136/bjo.47.6.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghayoor I, Jafri A, Tabassum G, Zubair F. Conjunctival leiomyoma – A case report. Pak J Ophthalmol. 2013;29:177–179. [Google Scholar]
- 3.Brannan SO, Cheung D, Trotter S, Tyler AJ, Reuser TQ. A conjunctival leiomyoma. Am J Ophthalmol. 2003;136:749–750. doi: 10.1016/s0002-9394(03)00399-4. [DOI] [PubMed] [Google Scholar]
- 4.Enzinger FM, Weiss SW. Soft tissue tumors. St. Louis: C.V. Mosby; 1983. pp. 281–297. [Google Scholar]
- 5.Gündüz K, Günalp I, Erden E, Erekul S. Orbital leiomyoma: Report of a case and review of the literature. Surv Ophthalmol. 2004;49:237–242. doi: 10.1016/j.survophthal.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Shields JA, Shields CL, Eagle RC, Jr, De Potter P. Observations on seven cases of intraocular leiomyoma. The 1993 Byron Demorest Lecture. Arch Ophthalmol. 1994;112:521–528. doi: 10.1001/archopht.1994.01090160097028. [DOI] [PubMed] [Google Scholar]
- 7.Shields CL, Shields JA, Varenhorst MP. Transscleral leiomyoma. Ophthalmology. 1991;98:84–87. doi: 10.1016/s0161-6420(91)32336-4. [DOI] [PubMed] [Google Scholar]
- 8.Heegaard S, Prause JU. Leiomyoma of the caruncle. Acta Ophthalmol Scand. 1998;76:731–733. doi: 10.1034/j.1600-0420.1998.760621.x. [DOI] [PubMed] [Google Scholar]
- 9.Guerriero S, Sborgia A, Giancipoli G, Fiore MG, Ross R, Piscitelli D. A rare case of primitive epithelioid leiomyosarcoma of the conjunctiva. Orbit. 2011;30:169–171. doi: 10.3109/01676830.2011.574771. [DOI] [PubMed] [Google Scholar]


