Abstract
BACKGROUND
Administration of caffeine or caffeinated coffee in laboratory and ambulatory settings results in small to moderate acute increases in blood pressure (BP). However, habitual coffee intake has not been linked conclusively to long-term increases in basal BP, and findings are inconsistent by sex. This study examined longitudinal relations of habitual coffee use to resting BP and pulse pressure.
METHODS
In a sample of 2,442 participants from the Baltimore Longitudinal Study of Aging (BLSA), coffee consumption was used to predict resting systolic and diastolic BP and pulse pressure using longitudinal mixed-effects regression models adjusted for age, education, antihypertensive, and antihyperlipidemic use, smoking, and body mass index (BMI). Analyses were stratified by sex (865 women and 1,577 men), and age and BMI were examined as possible effect modifiers.
RESULTS
In men, we identified a significant three-way interaction among coffee intake (nonlinear), baseline age, and length of follow-up for systolic BP (SBP) and pulse pressure. A significant interaction of coffee intake and BMI (nonlinear) was also noted for SBP in men. There were no significant relations of coffee intake to BP or pulse pressure in women.
CONCLUSION
Greater coffee intake in men was associated with steeper age-related increases in SBP and pulse pressure, particularly beyond 70 years of age and in overweight to obese men.
Keywords: blood pressure, caffeine, coffee, hypertension, pulse pressure
Coffee intake is the primary source of dietary caffeine in men and women, accounting for 85 and 82% of their total consumption, respectively.1 The average daily intake of coffee in the United States is ~1.75 cups, with the highest 10% of coffee drinkers consuming more than seven cups of coffee per day.2 Prior investigations have consistently indicated a relation between caffeine intake (e.g., similar to two cups of coffee) and acute elevations in blood pressure (BP),3 sympatho-adrenomedullary activation4 and hypothalamic–pituitary–adrenal activity,5 even among habitual coffee drinkers. Pressor effects associated with caffeine dosing are also observed in natural settings using ambulatory BP monitoring.6 Increases in peripheral vascular resistance have been implicated as the mechanism by which acute caffeine administration leads to acute elevations in BP.7
Results of some, though not all, case–control studies have found that coffee drinkers generally have higher levels of BP than nondrinkers8 or that heavy coffee drinkers have higher BP than moderate coffee drinkers.9 Negative findings have been attributed to tolerance that develops, with regular use, to acute BP increases observed after coffee administration.10 Furthermore, findings relating coffee intake to long-term increases in basal BP have been inconclusive.11 Indeed, few longitudinal investigations have examined potential relations of regular coffee intake to hypertension risk.
Results of one investigation, conducted in men, noted that consumption of over five cups of coffee per day at baseline increased risk of incident hypertension.12 Significant systolic and diastolic reductions were also found in men (n = 340) who reduced their coffee intake over a 6-year follow-up period.13 However, these effects were rendered nonsignificant after adjusting for body mass index (BMI), smoking, alcohol use, and physical activity. One study relating caffeine consumption to hypertension in women examined data from the Nurses’ Health prospective cohort study of 155,594 healthy women followed for 12 years.14 Although no association was found between coffee consumption and incident hypertension, there was a significant inverted U-shaped association between caffeine consumption and incident hypertension risk. Participants in the third quintile of caffeine consumption exhibited a 12–13% increased risk of hypertension, compared to those in the lowest quintile. A similar inverse U-shaped relation has also been reported for coffee consumption in a sample of Dutch women.15
Women exhibit different patterns of coffee intake than men16 and an estrogen-induced extended caffeine half-life.17 This suggests that associations of coffee intake to cardiovascular outcomes should be examined separately in men and women. Furthermore, the potential role of demographic and lifestyle variables in moderating relations between caffeine ingestion and health is poorly understood. Coffee intake is associated with BMI;18 greater BMI may accentuate the negative health effects of coffee consumption. Furthermore, coffee intake decreases with age,16 and age may moderate the impact of caffeine on cardiovascular health differently in older vs. younger consumers.19 In this article, we examined the longitudinal relations of habitual coffee intake to concomitant measures of resting BP in men vs. women, while evaluating potential interactions with age and BMI. Because some data suggest that coffee consumption decreases arterial compliance,20 we also examined pulse pressure as an endpoint.
METHODS
Participants were enrolled in the Baltimore Longitudinal Study of Aging (BLSA). Founded in 1958, the BLSA is a prospective study of community-dwelling volunteers. Volunteers return to the National Institute on Aging in Baltimore, MD every 2–3 years to undergo extensive physiological and psychological testing. Participant data were excluded for those consuming excessive alcohol (>14 drinks/week), diagnosed with dementia, cerebrovascular diseases including stroke, and renal failure across all assessment visits. After exclusions, 2,442 participants with self-reported coffee intake, smoking, BMI, and BP data were available for analyses. A priori power analyses were conducted using G*POWER, version 3.021 based on known available sample sizes for men (n = 1,577) and women (n = 865). In both men and women, the analyses were powered to detect a small Cohen’s f2 estimate (f2 = 0.005 for men, f2 = 0.009 for women) at conventional levels of power (0.80) and α (.05) with 31 predictors. These effect size estimates were particularly conservative because they (i) do not account for the repeat visit data and (ii) include the maximal number of predictors before backward elimination procedures, which were used for the final presented analyses.
Because the BLSA uses continuous enrollment procedures, participants have differential start times, numbers of visits, and follow-up times. Table 1 presents cumulative sample sizes by number of visits. The length of follow-up ranged from 0 to 41 years. All participants provided written informed consent, and all procedures followed institutional guidelines. The Institutional Review Board of the University of Maryland, Baltimore County (Baltimore, MD) also approved these data analyses.
Table 1.
Cumulative sample size by number of visits
| Number of visits | Men (n = 1,577) | Women (n = 865) |
|---|---|---|
| n (Percentage of sample) | n (Percentage of sample) | |
| 1 | 1,577 (100.0) | 865 (100.0) |
| 2 | 1,295 (82.1) | 654 (75.6) |
| 3 | 1,074 (68.1) | 501 (57.9) |
| 4 | 902 (57.2) | 380 (43.9) |
| 5 | 734 (46.5) | 287 (33.2) |
| 6 | 583 (37.0) | 223 (25.8) |
| 7 | 433 (27.5) | 165 (19.1) |
| 8 | 339 (21.5) | 123 (14.2) |
| 9 | 255 (16.2) | 74 (8.6) |
| 10 | 203 (12.9) | 39 (4.5) |
| 11 | 155 (9.8) | 14 (1.6) |
| 12 | 109 (6.9) | 6 (0.69) |
| 13 | 65 (3.9) | 1 (0.001) |
| 14 | 44 (2.8) | — |
| 15 | 25 (1.6) | — |
| 16 | 11 (0.70) | — |
| 17 | 5 (0.32) | — |
| 18 | 1 (0.001) | — |
Measures
During each BLSA visit, participants rotate through various examination procedures. Data relevant to the present analyses were collected over the course of 2½ days and included medical history and physical examination, anthropometry, basal BP, and assessment of health-related behaviors (e.g., coffee, cigarette use).
Blood pressure
At each study visit, BP was measured in the morning by trained nursing staff at least 90 min after breakfast. After a 5-min rest period, a mercury sphygmomanometer with an appropriate-sized occluding cuff was used to measure BP three times from each arm while patients sat in an upright position. The BP values used in this study are the average of the second and third measurements from both the right and left arms. Levels of systolic BP (SBP) and diastolic BP (DBP) were defined by Korotkoff phases I and V, respectively. Pulse pressure was computed as SBP − DBP.
Coffee intake
Daily coffee intake was obtained from participant responses on a history and physical questionnaire administered at each BLSA visit. It was measured in cups of coffee (7 oz cups) consumed daily, on average, since the last BLSA visit. Self-reported caffeine use has been found to be significantly associated with salivary caffeine (r = 0.31) and paraxanthine (r = 0.42).22 Though significant, the low magnitudes of these values demonstrate the considerable degree of error involved in self-reported caffeine intake. Furthermore, other sources of caffeine consumption were regrettably not assessed in the BLSA. However, these measurement limitations only indicate that the present study is likely to underestimate the effect of coffee intake on BP increases.23
Covariates
Baseline age (in years) was calculated as participant’s age at the first BLSA visit at which data are available for all variables of interest. Length of follow-up (i.e., time since baseline) was calculated in years each participant actively participated in the BLSA. Education was assessed in years. BMI was computed as weight (kg)/height (meters × meters). Current smoking status was assessed during the physical examination at each BLSA visit. A brief questionnaire assessing the use of any type of tobacco (e.g., cigarettes, cigars, pipe tobacco) and the daily frequency of each type was completed with the help of nursing staff. The variable entered in the present analyses was a collapsed measure indicating whether participants ever smoked across all visits (coded as “1”) vs. never (coded as “0”). Current medication use was assessed based on medications participants brought to their examination. Additionally, a review of medications active at the previous visit was conducted, and discrepancies or changes were noted and addressed. For the present analyses, antihypertensive and antihyperlipidemic use were coded as a single time-dependent variable, with “1” indicating taking one or both types of these cardiovascular medications and “0” indicating taking neither type of medication currently.
Baseline age, education, and smoking status were analyzed time-independently. All other covariates, including length of follow-up, BMI, and medication use, were analyzed time-dependently using concurrent values.
Data analyses
Data were analyzed using linear mixed-effects regression models (SAS PROC MIXED). Mixed-effects regression is the most appropriate statistical method for repeated measurements in the BLSA, due to lack of uniformity of measurement intervals both within and across participants. The analysis accounts for these inconsistencies in measurement intervals, remains unaffected by randomly missing data, and accounts for the correlation among repeated measurements on the same participants.24
Longitudinal changes were estimated in these analyses by modeling rate of change for each participant based on all data points available for that individual. The rate of change for the entire group was first modeled, followed by individual deviation from the group rate. Time since baseline was entered as a random effect in each model. For each sex, time-dependent coffee intake was entered continuously into three separate models predicting either SBP, DBP, or pulse pressure. The set of covariates (age, length of follow-up, education, antihypertensive and antihyperlipidemic use, smoking, BMI) and coffee intake were entered into each of the mixed-effects models. Additionally, to control for nonlinear effects of BMI on BP, the squared term for BMI was entered into each model, as well as all two- and three-way interactions among coffee intake and BMI. Finally, to test for potential nonlinear effects of coffee intake, the squared term for coffee intake was entered into each model. A manual backward elimination procedure was then employed, in which nonsignificant interaction terms (P > 0.05), beginning with the highest-order effects, were eliminated from each model until a final solution was reached.25
Age at first assessment indexed cross-sectional age differences whereas time since baseline (i.e., years since baseline testing for each administration of the dependent measure) indexed longitudinal age change. The analysis thus revealed whether coffee intake alone accounted for significant variance above and beyond the set of covariates in SBP, DBP, or pulse pressure; and whether the rate of change in coffee intake predicted rate of change in the three hemodynamic measures over time, after adjustment for standard covariates.
Statistical analyses were conducted using SAS versions 8.02 and 9.0 (SAS, Cary, NC). Graphing of estimates produced by individual models was conducted with Stata version 10.0 using parameter estimates of individual mixed-effects regression equations, which included all fixed single-order effects and interactions. Significant interaction effects were presumed to qualify single-order effects, and significant effects of quadratic coffee BMI were presumed to qualify those that involved linear BMI.
RESULTS
Table 2 provides participant characteristics at their initial visit. Participants were 65% male, 89% white, aged 18–97 years (mean = 52.1 years, s.d. = 17.9). Seventy-seven percent of the sample (n = 1,884) reported consuming at least one cup of caffeinated coffee daily (data not shown in Table 2). The frequency distribution of coffee intake at first BLSA visit was as follows: 0 cups/day = 327 men/237 women; 1–3 cups/day = 796 men/510 women; 4–6 cups/day = 355 men/98 women; >6 cups/day = 99 men/20 women. On average, participants had a 0.75 s.d. change over time (range = 0–5.6) in their individual daily coffee intake. The BMI distribution at first visit was: BMI <20 = 45 men/109 women; BMI 20–24.9 = 766 men/469 women; BMI 25–29.9 = 655 men/206 women; BMI ≥30 = 111 men/81 women. The distribution of age was: age <60 = 998 men/553 women; age 60–69 = 236 men/137 women; age 70–79 = 249 men/121 women; age ≥80 = 94 men/54 women.
Table 2.
Characteristics of study sample at first BLSA visit
| Variable | All (n = 2,442) | Men (n = 1,577) | Women (n = 865) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | s.d. | Range | Mean | s.d. | Range | Mean | s.d. | Range | |
| Age (years) | 52.1 | 17.9 | 18–97 | 52.1 | 18.0 | 18–97 | 52.2 | 17.8 | 18–94 |
| Education (years) | 16.5 | 2.8 | 4–25 | 16.8 | 2.9 | 4–25 | 16.1 | 2.5 | 8–24 |
| Gender (% male) | 64.6 | — | — | — | — | — | — | — | — |
| Race (% white) | 89.1 | — | — | 90.8 | — | — | 86.0 | — | — |
| Ever smoker (%) | 66.6 | — | — | 71.7 | — | — | 57.5 | — | — |
| Cardiovascular medication use (%) | 15.2 | — | — | 13.4 | — | — | 18.5 | — | — |
| BMI (kg/m2) | 24.9 | 3.6 | 17–49 | 25.3 | 3.2 | 18–43 | 24.2 | 4.2 | 17–49 |
| Coffee intake (cups/day) | 2.3 | 2.1 | 0–10 | 2.6 | 2.3 | 0–10 | 1.8 | 1.8 | 0–10 |
| DBP (mm Hg) | 79.4 | 10.7 | 40–125 | 80.9 | 10.6 | 45–125 | 76.5 | 10.3 | 40–115 |
| SBP (mm Hg) | 127.4 | 20.1 | 79–210 | 129.7 | 19.2 | 83–210 | 123.2 | 20.9 | 79–210 |
| Pulse pressure (mm Hg) | 48.1 | 15.0 | 18–138 | 48.8 | 14.3 | 20–115 | 46.7 | 16.1 | 18–138 |
BLSA, Baltimore Longitudinal Study of Aging; BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
In men, significant interactions were observed among quadratic coffee intake, age, and time since baseline in predicting SBP (P = 0.02) and pulse pressure (P = 0.03) (Table 3). These interactions are presented graphically in Figure 1a,b, respectively and suggest that both SBP and pulse pressure increase with advancing age, with the rate of increase more pronounced with increasing age. Furthermore, the models predict that beyond 70 years of age, rates of increase in SBP and pulse pressure are affected by coffee intake, such that daily consumption of six or more cups of coffee dramatically increases the rate of increase in SBP and pulse pressure observed with aging. The interaction of coffee intake and the quadratic term of BMI also predicted significantly SBP in men (presented graphically in Figure 1c). The finding indicated that, in overweight and obese men, lower coffee consumption, as assessed at each visit, predicts an attenuation of the BP increases associated with additional weight gain. For example, at a BMI of 40, the model predicted a ~30 mm SBP difference between those abstaining from coffee (SBP = 134) and those consuming nine cups of coffee daily (SBP = 167). It should be noted that the categorical representations of coffee intake and BMI presented in Figure 1a–c are utilized for illustrative purposes only; both variables were analyzed continuously. In women, there were no significant single-order or interactive relations of coffee consumption to BP or pulse pressure.
Table 3.
Results of mixed-effects regression models in men: significant predictors
| Blood pressure parameter | Predictor | β | s.e. | P |
|---|---|---|---|---|
| DBP | Medication status | −0.95 | 0.31 | 0.00 |
| Time since baseline | 2.03 | 0.72 | 0.01 | |
| BMI | 3.54 | 1.52 | 0.02 | |
| Baseline age × time since baseline | −0.01 | 0.002 | <0.01 | |
| Time since baseline × BMI | −0.12 | 0.05 | 0.02 | |
| Time since baseline × BMI × BMI | 0.002 | 0.001 | 0.03 | |
| SBP | Smoking status | 1.63 | 0.81 | 0.04 |
| Education | −0.27 | 0.12 | 0.03 | |
| Cups coffee/day × BMI × BMI | −0.01 | 0.01 | 0.04 | |
| Baseline age × time since baseline | 0.01 | 0.003 | 0.01 | |
| Cups coffee/day × cups coffee/day × baseline age × Time since baseline | 0.001 | 0.0003 | 0.02 | |
| Pulse pressure | Medication status | 1.26 | 0.43 | <0.01 |
| Education | −0.25 | 0.09 | <0.01 | |
| Baseline age × time since baseline | 0.02 | 0.003 | <0.01 | |
| Cups coffee/day × cups coffee/day × baseline age × time since baseline | 0.001 | 0.0003 | 0.03 |
Due to space limitations, only significant findings are presented. Please see Supplementary Table S1 in online for full results. Medication status: “1” = taking antihypertensive or antihyperlipidemic medication, “0” = not taking these medications; Smoking status: “1” = ever smoked, “0” = has never smoked.
BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Figure 1.
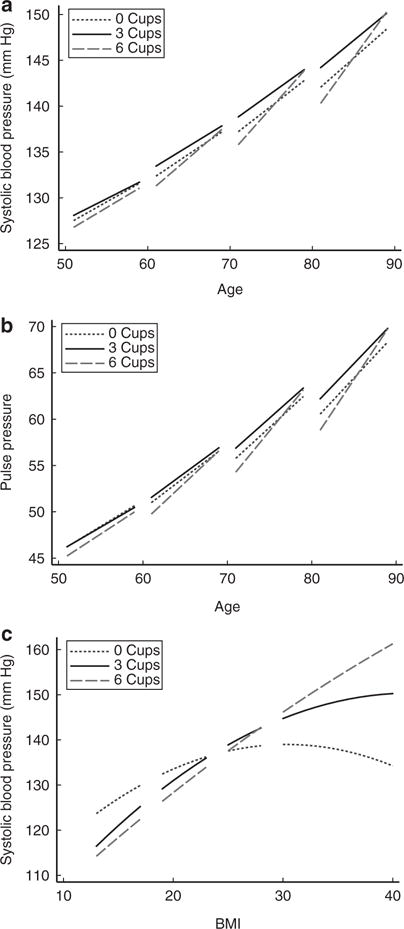
(a) Predicted systolic blood pressure in men by coffee intake, baseline age, time since baseline, and covariates (age, education, smoking, cardiovascular medication use); (b) predicted pulse pressure in men by coffee intake, baseline age, time since baseline, and covariates (age, education, smoking, cardiovascular medication use); (c) predicted systolic blood pressure in men by coffee intake, body mass index (BMI), and covariates (age, education, smoking, cardiovascular medication use).
DISCUSSION
Few epidemiological investigations have examined the relations of habitual coffee consumption to longitudinal change in BP, and none have examined pulse pressure. Also examined were potential differential associations as a function of sex, age, and BMI. Here, we found that, in men, there were significant interactions of nonlinear coffee intake, age, and length of follow-up in predicting SBP and pulse pressure such that the rate of age-related increase in SBP and pulse pressure beyond age 70 may be increased at high levels of coffee consumption. The interaction of coffee intake and nonlinear BMI also significantly predicted SBP in men. The finding indicated that, in overweight and obese men, higher levels of coffee consumption were associated with greater increases in SBP. Thus, in both older men and men with a BMI above 25 (particularly obese men), reducing coffee consumption may reduce observed SBP.
In one prior longitudinal investigation in men, significant SBP and DBP reductions were found among those who reduced their coffee intake over the follow-up period.13 However, only two time points were available for analysis among 340 participants, whereas in the current investigation over 700 men had at least five visits, with an average follow-up of 15 years. In another prior investigation among men, BP levels were self-reported.12
In the present study, coffee intake was not significantly associated with longitudinal changes in any BP parameter in women. These results stand in contrast to the results of the Nurses’ Health Study14 and the Doetinchem Cohort Study,15 which both suggested an inverted U-shaped association between caffeine or coffee consumption and incident hypertension among women. Several issues could account for the contrasting results; both studies had significantly larger female sample sizes (n = 155,594 and n = 3,383, respectively) than the present study, utilized a different endpoint (dichotomous hypertension vs. continuous BP parameters), and were comprised of much larger percentages of moderate and heavy coffee drinkers.
The similarity of results observed for SBP and pulse pressure in men suggests that increases in arterial stiffness should be considered a potential mechanism by which high levels of regular coffee intake may influence BP and possibly the development of hypertension.26 However, identifying potential mechanisms by which coffee intake may ultimately impact arterial compliance may be confounded by the complex mix of bioactive compounds contained in coffee. Coffee contains a significant number of biologically active components, both deleterious and beneficial. Furthermore, the length of coffee bean roasting, as well as the method of coffee preparation (e.g., boiled vs. paper filtered coffee) can alter the ratio of chemical compounds within coffee.27
Of the potentially deleterious compounds in coffee, resultant actions of caffeine are the most likely mechanism explaining observed results of the present investigation. Caffeine acts as an antagonist at adenosine A3 receptors that are expressed in the liver, lung, placenta, and extensively throughout the brain28 and have been indicated as having possible cardioprotective functions.29 Additionally, caffeine has demonstrated vasoconstrictive effects by acting directly on vessel wall adenosine receptors.20 In contrast, antioxidant compounds found in coffee, such as chlorogenic acid, may counteract the effects of caffeine on BP30 or affect cardiovascular risk associated with insulin resistance,31 reducing the net effect of caffeine on basal BPs. Therefore, the results of the present investigation, which suggest that coffee intake may accelerate age-related decreases in arterial compliance, may be explained by a tempering of the action of caffeine by a number of newly identified antioxidant compounds contained in coffee. Furthermore, greater understanding of the interplay among deleterious and beneficial cardiovascular effects of coffee may result from examination of the pharmacological action of these compounds on blood vessel endothelial tissue. Other potential mechanisms whereby coffee intake may increase hypertension risk include elevation of homocysteine levels,32 and potentiation of acute BP responses during mental stress.33
Strengths of the present investigation include the largest number of longitudinal data points available for coffee intake and BP, examination of differential patterning of results in men and women, examination of linear and nonlinear relations among coffee intake and hemodynamic measures, and incorporation of an index of arterial compliance in addition to BP.
Limitations of the present investigation include its use of a sample of convenience and the potential lack of generalizability to non-Caucasians. From 1958 to 1978, BLSA participation was restricted to white men. In 1979, recruitment of a similar convenience sample of women was initiated. However, this difference in recruitment may have introduced a number of cohort effects, including shorter follow-up times among women and the awareness of coffee intake as a potential health threat. Popularized findings suggesting a link between coffee intake and myocardial infarction were initially published in 1973, and the number of published articles relating coffee intake to health numbered 27 references in 1979, 47 in 1981, 68 in 1990, and 88 in 2000. Therefore, female BLSA participants have been exposed to significantly more information about potential health risks of coffee during their participation in BLSA than men. In addition, the discrepancy in sample size and thus statistical power between men (n = 1,577) and women (n = 865) may indicate that significant effect(s) in women were overlooked in the present analyses. However, results of a priori power analyses (see Methods section) reduce the likelihood of this possibility. Measurement of coffee intake represents another study limitation because the size of the coffee cup was not assessed. The typical size of a cup of coffee has increased over time as has the caffeine content of coffee served. Other sources of caffeine intake (e.g., tea, caffeine, soda) were also not assessed. In addition, available data precluded analysis of coffee intake as truly “current” intake (rather than as average intake between last and current visit), a distinction that would have eased interpretation of mixed-effects analyses. Due to the way in which antihypertensive medication use data were collected in the BLSA, we were unable to adjust for or investigate the effects of specific types of antihypertensive medications in the present analyses. Family history of hypertension, dietary nutrient intake, oral contraceptive use, and time-dependent smoking status represent additional covariates that could not be included in the present analyses due to similar challenges, though future researchers may consider their inclusion.
The present findings largely indicate significant relations of coffee intake to SBP and pulse pressure in men, with the pattern of results being remarkably similar for both hemodynamic measures. Greater coffee intake in men was associated with steeper age-related increases in SBP and pulse pressure, particularly beyond 70 years of age and in overweight to obese men. These findings indicate that studies of coffee intake and cardiovascular health should routinely examine nonlinear trends. These results further suggest examination of current recommendations regarding coffee intake in overweight and obese individuals relative to BP.
Supplementary Material
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, National Institute on Aging.
Footnotes
Supplementary material is linked to the online version of the paper at http://www.nature.com/ajh
Disclosure: The authors declared no conflict of interest.
References
- 1.Frary CD, Johnson RK, Wang MQ. Food sources and intakes of caffeine in the diets of persons in the United States. J Am Diet Assoc. 2005;105:110–113. doi: 10.1016/j.jada.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 2.Chou TM, Benowitz NL. Caffeine and coffee: effects on health and cardiovascular disease. Comp Biochem Physiol C, Pharmacol Toxicol Endocrinol. 1994;109:173–189. [PubMed] [Google Scholar]
- 3.Jee SH, He J, Whelton PK, Suh I, Klag MJ. The effect of chronic coffee drinking on blood pressure: a meta-analysis of controlled clinical trials. Hypertension. 1999;33:647–652. doi: 10.1161/01.hyp.33.2.647. [DOI] [PubMed] [Google Scholar]
- 4.Lane JD, Adcock RA, Williams RB, Kuhn CM. Caffeine effects on cardiovascular and neuroendocrine responses to acute psychosocial stress and their relationship to level of habitual caffeine consumption. Psychosom Med. 1990;52:320–336. doi: 10.1097/00006842-199005000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Bellet S, Roman L, Barham F. Effect of physical exercise on adrenocortical excretion. Metab Clin Exp. 1969;18:484–487. doi: 10.1016/0026-0495(69)90141-3. [DOI] [PubMed] [Google Scholar]
- 6.Lane JD, Phillips-Bute BG, Pieper CF. Caffeine raises blood pressure at work. Psychosom Med. 1998;60:327–330. doi: 10.1097/00006842-199805000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Casiglia E, Bongiovì S, Paleari CD, Petucco S, Boni M, Colangeli G, Penzo M, Pessina AC. Haemodynamic effects of coffee and caffeine in normal volunteers: a placebo-controlled clinical study. J Intern Med. 1991;229:501–504. doi: 10.1111/j.1365-2796.1991.tb00385.x. [DOI] [PubMed] [Google Scholar]
- 8.Lang T, Bureau JF, Degoulet P, Salah H, Benattar C. Blood pressure, coffee, tea and tobacco consumption: an epidemiological study in Algiers. Eur Heart J. 1983;4:602–607. doi: 10.1093/oxfordjournals.eurheartj.a061531. [DOI] [PubMed] [Google Scholar]
- 9.Lang T, Degoulet P, Aime F, Fouriaud C, Jacquinet-Salord MC, Laprugne J, Main J, Oeconomos J, Phalente J, Prades A. Relation between coffee drinking and blood pressure: analysis of 6,321 subjects in the Paris region. Am J Cardiol. 1983;52:1238–1242. doi: 10.1016/0002-9149(83)90580-5. [DOI] [PubMed] [Google Scholar]
- 10.Nurminen ML, Niittynen L, Korpela R, Vapaatalo H. Coffee, caffeine and blood pressure: a critical review. Eur J Clin Nutr. 1999;53:831–839. doi: 10.1038/sj.ejcn.1600899. [DOI] [PubMed] [Google Scholar]
- 11.Noordzij M, Uiterwaal CS, Arends LR, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens. 2005;23:921–928. doi: 10.1097/01.hjh.0000166828.94699.1d. [DOI] [PubMed] [Google Scholar]
- 12.Klag MJ, Wang NY, Meoni LA, Brancati FL, Cooper LA, Liang KY, Young JH, Ford DE. Coffee intake and risk of hypertension: the Johns Hopkins precursors study. Arch Intern Med. 2002;162:657–662. doi: 10.1001/archinte.162.6.657. [DOI] [PubMed] [Google Scholar]
- 13.Jenner DA, Puddey IB, Beilin LJ, Vandongen R. Lifestyle- and occupation-related changes in blood pressure over a six-year period in a cohort of working men. J Hypertens Suppl. 1988;6:S605–S607. doi: 10.1097/00004872-198812040-00189. [DOI] [PubMed] [Google Scholar]
- 14.Winkelmayer WC, Stampfer MJ, Willett WC, Curhan GC. Habitual caffeine intake and the risk of hypertension in women. JAMA. 2005;294:2330–2335. doi: 10.1001/jama.294.18.2330. [DOI] [PubMed] [Google Scholar]
- 15.Uiterwaal CS, Verschuren WM, Bueno-de-Mesquita HB, Ocké M, Geleijnse JM, Boshuizen HC, Peeters PH, Feskens EJ, Grobbee DE. Coffee intake and incidence of hypertension. Am J Clin Nutr. 2007;85:718–723. doi: 10.1093/ajcn/85.3.718. [DOI] [PubMed] [Google Scholar]
- 16.Nygård O, Refsum H, Ueland PM, Stensvold I, Nordrehaug JE, Kvåle G, Vollset SE. Coffee consumption and plasma total homocysteine: The Hordaland Homocysteine Study. Am J Clin Nutr. 1997;65:136–143. doi: 10.1093/ajcn/65.1.136. [DOI] [PubMed] [Google Scholar]
- 17.Abernethy DR, Todd EL. Impairment of caffeine clearance by chronic use of low-dose oestrogen-containing oral contraceptives. Eur J Clin Pharmacol. 1985;28:425–428. doi: 10.1007/BF00544361. [DOI] [PubMed] [Google Scholar]
- 18.Puccio EM, McPhillips JB, Barrett-Connor E, Ganiats TG. Clustering of atherogenic behaviors in coffee drinkers. Am J Public Health. 1990;80:1310–1313. doi: 10.2105/ajph.80.11.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arciero PJ, Gardner AW, Benowitz NL, Poehlman ET. Relationship of blood pressure, heart rate and behavioral mood state to norepinephrine kinetics in younger and older men following caffeine ingestion. Eur J Clin Nutr. 1998;52:805–812. doi: 10.1038/sj.ejcn.1600651. [DOI] [PubMed] [Google Scholar]
- 20.Riksen NP, Rongen GA, Smits P. Acute and long-term cardiovascular effects of coffee: implications for coronary heart disease. Pharmacol Ther. 2009;121:185–191. doi: 10.1016/j.pharmthera.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 22.James JE, Bruce MS, Lader MH, Scott NR. Self-report reliability and symptomatology of habitual caffeine consumption. Br J Clin Pharmacol. 1989;27:507–514. doi: 10.1111/j.1365-2125.1989.tb05400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.James JE. Critical review of dietary caffeine and blood pressure: a relationship that should be taken more seriously. Psychosom Med. 2004;66:63–71. doi: 10.1097/10.psy.0000107884.78247.f9. [DOI] [PubMed] [Google Scholar]
- 24.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;24:323–355. [Google Scholar]
- 25.Morrell CH, Pearson JD, Brant LJ. Linear transformations of linear mixed-effects models. American Statistician. 1997;51:338–343. [Google Scholar]
- 26.Mahmud A, Feely J. Acute effect of caffeine on arterial stiffness and aortic pressure waveform. Hypertension. 2001;38:227–231. doi: 10.1161/01.hyp.38.2.227. [DOI] [PubMed] [Google Scholar]
- 27.Cornelis MC, El-Sohemy A. Coffee, caffeine, and coronary heart disease. Curr Opin Clin Nutr Metab Care. 2007;10:745–751. doi: 10.1097/MCO.0b013e3282f05d81. [DOI] [PubMed] [Google Scholar]
- 28.Murrison EM, Goodson SJ, Edbrooke MR, Harris CA. Cloning and characterisation of the human adenosine A3 receptor gene. FEBS Lett. 1996;384:243–246. doi: 10.1016/0014-5793(96)00324-9. [DOI] [PubMed] [Google Scholar]
- 29.Stambaugh K, Jacobson KA, Jiang JL, Liang BT. A novel cardioprotective function of adenosine A1 and A3 receptors during prolonged simulated ischemia. Am J Physiol. 1997;273:H501–H505. doi: 10.1152/ajpheart.1997.273.1.H501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suzuki A, Fujii A, Yamamoto N, Yamamoto M, Ohminami H, Kameyama A, Shibuya Y, Nishizawa Y, Tokimitsu I, Saito I. Improvement of hypertension and vascular dysfunction by hydroxyhydroquinone-free coffee in a genetic model of hypertension. FEBS Lett. 2006;580:2317–2322. doi: 10.1016/j.febslet.2006.03.047. [DOI] [PubMed] [Google Scholar]
- 31.Johnston KL, Clifford MN, Morgan LM. Coffee acutely modifies gastrointestinal hormone secretion and glucose tolerance in humans: glycemic effects of chlorogenic acid and caffeine. Am J Clin Nutr. 2003;78:728–733. doi: 10.1093/ajcn/78.4.728. [DOI] [PubMed] [Google Scholar]
- 32.Panagiotakos DB, Pitsavos C, Zeimbekis A, Chrysohoou C, Stefanadis C. The association between lifestyle-related factors and plasma homocysteine levels in healthy individuals from the “ATTICA” Study. Int J Cardiol. 2005;98:471–477. doi: 10.1016/j.ijcard.2003.12.036. [DOI] [PubMed] [Google Scholar]
- 33.Lovallo WR, Pincomb GA, Sung BH, Everson SA, Passey RB, Wilson MF. Hypertension risk and caffeine’s effect on cardiovascular activity during mental stress in young men. Health Psychol. 1991;10:236–243. doi: 10.1037//0278-6133.10.4.236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


