Abstract
Background:
Shoulder injuries remain one of the most common injuries among collegiate football athletes. Offensive linemen in particular are prone to posterior labral pathology.
Purpose:
To evaluate the efficacy of shoulder bracing in collegiate offensive linemen with respect to injury prevention, severity, and lost playing time.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Offensive linemen at a single collegiate institution wore bilateral shoulder-stabilizing braces for every contact practice and game beginning in the spring of 2013. Between spring of 2007 and fall of 2012, offensive linemen did not wear any shoulder braces. Player injury data were collected for all contact practices and games throughout these time periods to highlight differences with brace use.
Results:
Forty-five offensive linemen (90 shoulders) participated in spring and fall college football seasons between 2007 and 2015. There were 145 complete offensive linemen seasons over the course of the study. Offensive linemen not wearing shoulder braces completed 87 seasons; offensive linemen wearing shoulder braces completed 58 seasons. Posterior labral tear injury rates were calculated for players who wore the shoulder braces (0.71 per 1000 athlete-exposures) compared with shoulders of players who did not wear the braces (1.90 per 1000 athlete-exposures). The risk ratio was 0.46 (95% CI, 0.16-1.30; P = .14). Mean time (contact practices and games) missed due to injury was significant, favoring less time missed by players who used braces (8.7 vs 36.60 contact practices and games missed due to injury; P = .0019). No significant difference in shoulder labral tears requiring surgery was found for brace use compared with no brace use.
Conclusion:
Shoulder-stabilizing braces were shown not to prevent posterior labral tears among collegiate offensive lineman, although they were associated with less time lost to injury. The results of this study have clinical significance, indicating that wearing a shoulder brace provides a protective factor for offensive linemen.
Keywords: collegiate football, shoulder injury, prevention, offensive linemen
High-speed player-to-player collisions put American football players at risk for upper extremity injury. The shoulder is the fourth most common site of injury in football players, accounting for 10% to 20% of the total number of football injuries each year.16 Although concussive head injuries have been given significant attention in the media, shoulder pathology accounted for 3 (acromioclavicular joint, anterior instability, rotator cuff tendinitis) of the top 15 musculoskeletal diagnoses made at the National Football League (NFL) Combine4 between 1987 and 2000. In 2004, 49.7% of the athletes invited to the NFL Combine had previously suffered a shoulder injury, and 34% of those athletes required surgical treatment at the time of injury.16 These injuries recorded throughout the NFL Combine address the high frequency of shoulder injuries among collegiate football athletes.
Kaplan et al16 found that the type of shoulder injury varies depending on the position being played. Defensive players most commonly suffer from anterior shoulder instability, whereas linemen are found to be at greater risk of developing posterior shoulder instability.16 This is significant because posterior labral injuries are 15 times more common in offensive linemen than in the nonactive population.12,14 The proposed mechanism for posterior labral injury in offensive linemen is blocking an opponent with 90° of flexion of the shoulder and elbows locked.17 Contact from an opponent running into an offensive lineman’s outstretched arms directs a posterior force onto the shoulder, thereby transferring a shearing force on the posterior aspect of the glenoid labrum.17 Multiple “microtraumatic” events of forced shoulder retraction over the course of a season are believed to lead to posterior labral detachment and tearing.5,12
Shoulder-stabilizing braces were designed to limit abduction, adduction, external rotation, internal rotation, and retraction of the upper extremity while playing football. Offensive linemen are coached to punch opposing players with both hands. At the moment of contact, most are unable to instinctively protract their shoulders, which would maximize the glenoid surface area to account for the compression force.17 We speculate that the shoulder-stabilizing brace helps maintain anatomic position throughout a collision by limiting retraction of the shoulder, thus directing the collision force to the musculature of the shoulder. The brace resists forced posterior shoulder subluxation by allowing the shoulder musculature to absorb the force rather than the labrum. Offensive linemen can wear the shoulder stabilizer comfortably during practices and games without affecting their playing ability. Most important, these braces limit retraction of the shoulder during collisions.
Buss et al8 found that athletes subjectively report improvement in shoulder stability while wearing a brace. However, no study has measured the effectiveness of wearing a brace in preventing labral tears or recurrent shoulder instability.11 We believe that the institution involved in this study is the only National Collegiate Athletic Association (NCAA) Division I football team that prophylactically braces all of their offensive linemen’s shoulders before every contact practice and game. This study measured the effectiveness of the shoulder-stabilizing braces in preventing posterior shoulder labral injury in collegiate offensive linemen.
Methods
In the spring of 2013, the athletic training department at a single institution mandated that all offensive linemen wear a shoulder-stabilizing brace, the Donjoy Shoulder Stabilizer: Shoulder Pad Attachment (DJO) (Figure 1) during all contact practices and in games. The decision to brace all offensive linemen was influenced by a yearly trend, noted by the football team’s athletic training staff and coaches, of multiple offensive linemen each year undergoing posterior shoulder labrum surgery. The Donjoy Shoulder Stabilizer uses straps attached to the front breastplate of the player’s shoulder pads. The straps are attached with Velcro to a cuff worn on the player’s arm. This positioning serves as an anchor and helps prevent abduction, external rotation, internal rotation, and forced posterior shoulder subluxation. Before 2013, no offensive lineman at this institution had worn the Donjoy Shoulder Stabilizer brace. Each offensive lineman was outfitted with 1 shoulder stabilizer for each arm and was monitored to ensure that he wore it to every practice. Since every offensive lineman was required to wear a shoulder brace, and not only players with a history of shoulder instability, the treatment bias alluded to by Dickens et al11 did not apply in this case.
Figure 1.

Athlete wearing the Donjoy Shoulder Stabilizer: Shoulder Pad Attachment on his right arm/shoulder.
All current and former offensive linemen from 2007 to 2015 at a single collegiate institution were eligible for this study. Only data from when the individuals were active members of the varsity football team were collected. Posterior labral tears were defined and identified by shoulder magnetic resonance imaging radiology reports and clinical correlation. A single, sports fellowship–trained orthopaedic surgeon performed all arthroscopic labral repairs once a trial of conservative management and return to play was initially attempted. Figure 2 demonstrates some of the pathology appreciated in this cohort. Conservative management included rotator cuff strengthening rehabilitation protocol, cessation from contact practice for at least 1 week, and a prescription regimen of anti-inflammatory drugs. Symptoms experienced by athletes included pain, weakness, and instability. One individual who suffered a career-ending injury, without a shoulder brace, and was unable to return to play after treatment was noted, and the games or contact practices missed after his medical retirement were not included in the study. Each missed contact practice and missed game were deemed as equivalent events.
Figure 2.
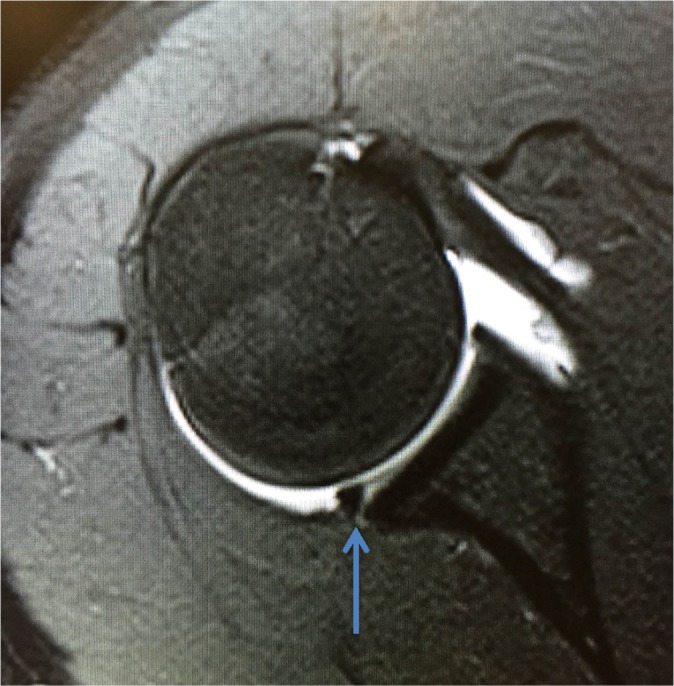
A 22-year-old male collegiate football player with a right posterior labral tear. Axial T2-weighted gradient-echo magnetic resonance arthrographic image shows posterior labral detachment (arrow). This athlete was part of the nonbraced cohort when he suffered this injury.
Athlete-exposures (AEs) were calculated for each player. One AE is defined as participation in 1 contact practice or game. Injury rates (injuries/AE) were calculated. An injury was defined as (1) having occurred during a contact practice or game, (2) requiring medical attention by the team physician or athletic trainer, and (3) resulting in a posterior labral tear diagnosis. The risk ratio with confidence intervals was also calculated.
Institutional research ethics board approval was obtained before study commencement. All individuals were given a unique alpha-numeric identifier to maintain anonymity. Data were analyzed using chi-square and t test statistical formulas to obtain a significance set at P < .05.
Results
From August 2007 to January 2016, a total of 45 offensive linemen participated in the fall and spring college football seasons for this collegiate institution, and all met the inclusion criteria for this study. All offensive linemen at this institution from 2007 to 2016 played under the same coaching staff. Demographic data can be seen in Table 1. There were 145 complete offensive linemen seasons over the course of the study. Offensive linemen not wearing shoulder braces completed 87 seasons; offensive linemen wearing shoulder braces completed 58 seasons. The greatest number of football seasons participated in by 1 individual was 5; the least number of seasons participated in by 1 individual was 1. Players wearing a shoulder brace participated in 4203 AEs. Players not wearing a shoulder brace participated in 8088 AEs (Table 2). The posterior shoulder labrum injury rate for players wearing a shoulder brace was 0.71 per 1000 AEs compared with 1.9 per 1000 AEs for players not wearing a shoulder brace. The relative risk ratio was 0.46 (95% CI, 0.16-1.30; P = .14) (Table 3).
TABLE 1.
Demographic Data for Offensive Linemena
| Shoulder Brace (n = 23) | No Shoulder Brace (n = 22) | |
|---|---|---|
| Age, y | 20 ± 2.8 (18-22) | 20 ± 2.8 (18-22) |
| Height, m | 1.95 ± 0.04 (1.87-2.03) | 1.95 ± 0.04 (1.87-2.03) |
| Weight, kg | 133.9 ± 4.9 (122.5-142.9) | 135.9 ± 4.1 (131.5-142.9) |
| BMI, kg/m2 | 35 ± 1.7 (32-38) | 35 ± 1.4 (32-39) |
aData are presented as mean ± SD (range).
TABLE 2.
Athlete-Exposures
| No. of Athlete-Exposures (Practice and Games) | |
|---|---|
| Shoulder brace | 4203 |
| No shoulder brace | 8088 |
| Total | 12,291 |
| Freshmen | 3077 |
| Sophomores | 3135 |
| Juniors | 3024 |
| Seniors | 3055 |
| Total | 12,291 |
TABLE 3.
Injury Rate and Risk Ratioa
| IRb | RR (95% CI) | P Value | |
|---|---|---|---|
| Shoulder brace | 0.71 | 0.46 (0.16-1.30) | .14 |
| No shoulder brace | 1.9 | ||
| Freshmen | 2.27 | 0.17 (0.02-1.38) | .09 |
| Sophomores | 1.91 | 0.20 (0.02-1.71) | .14 |
| Juniors | 0.99 | 0.50 (0.05-5.51) | .57 |
| Seniors | 0.98 | 0.14 (0.01-2.76) | .19 |
aIR, injury rate; RR, risk ratio.
bInjuries per 1000 athlete-exposures.
The mean age of injured offensive linemen was 19 years, whether wearing a shoulder brace or not. It was observed that freshman offensive linemen were injured most commonly; the posterior shoulder labrum injury rate for freshman offensive linemen was 2.27 per 1000 AEs, with a relative risk ratio of 0.17 (95% CI, 0.02-1.38; P = .09). Sophomores were the second most commonly injured age group, with a posterior shoulder labrum injury rate of 1.91 per 1000 AEs and a relative risk ratio of 0.20 (95% CI, 0.02-1.71; P = .14). The posterior shoulder labrum injury rate for juniors was 0.99 per 1000 AEs, with a relative risk ratio of 0.50 (95% CI, 0.05-5.51; P = .57). The posterior shoulder labrum injury rate for seniors was 0.98 per 1000 AEs, with a relative risk ratio of 0.14 (95% CI, 0.01-2.76; P = .19) (Table 3). The mean injury rate for freshmen and sophomores (2.12 posterior labral tears per 1000 AEs) was significantly greater than the mean injury rate for juniors and seniors (0.985 posterior labral tears per 1000 AEs) (P = .001).
The total number of games missed by offensive linemen from 2007 to 2016 due to posterior shoulder labrum injuries was 85. Offensive linemen who were injured while wearing shoulder braces did not miss any games. However, offensive linemen who injured their posterior shoulder labrum while not wearing a shoulder brace missed 5.31 games per injury (Table 4). The total number of contact practices missed by offensive linemen due to posterior shoulder labrum injuries was 527. Offensive linemen who were injured while wearing a shoulder brace missed 8.67 contact practices per injury, while offensive linemen who were injured while not wearing a shoulder brace missed 31.30 contact practices per injury (Table 4). There was 1 athlete included in this study who injured his posterior shoulder labrum while wearing a shoulder brace; the injury required shoulder surgery from which the athlete did not return to his preinjury level of play and was cut from the team. This player was a walk-on, meaning he was not offered a scholarship to play on the team. Many walk-ons get cut in favor of players with scholarships, so his injury may not have been the sole reason for why he was dismissed from the team. The mean time (games and practices) missed due to injury was statistically significant, favoring less time missed with brace use (8.7 vs 36.60 games and practices missed due to shoulder injury; P = .0019).
TABLE 4.
Results Comparing Posterior Shoulder Labral Tears With and Without Brace Use
| Shoulder Brace | No Shoulder Brace | |
|---|---|---|
| Offensive lineman seasons, n (%) | 56 (39) | 87 (61) |
| Games missed per injury, mean | 0 | 5.31 |
| Contact practices missed per injury, mean | 8.67 | 31.30 |
| Time missed (games and practices) per injury, mean | 8.67 | 36.61 |
| Posterior labrum tears requiring surgery, % | 0.66 | 0.75 |
| Posterior labrum tears, % | ||
| Freshman | 0.33 | 0.375 |
| Sophomores | 0.33 | 0.313 |
| Juniors | 0.33 | 0.125 |
| Seniors | 0 | 0.188 |
| Age of injured offensive lineman, y, mean | 19 | 19 |
Of 19 total posterior labral tears, 14 (74%) required surgery. Shoulder surgery was performed on 66% of offensive linemen who were injured while wearing a shoulder brace. Two offensive linemen who were injured while wearing a shoulder brace underwent surgery in the offseason so they did not miss any games during the season in which they were injured. Shoulder surgery was performed on 75% of offensive linemen who were injured while not wearing a shoulder brace. Players diagnosed with a posterior labral tear who had success with nonoperative treatment continued to play football and completed rehabilitation protocols.
Discussion
Prophylactic shoulder bracing has been used in football players at the high school, collegiate, and professional levels.2,8,22 Unlike prophylactic knee bracing, where it has been established that there is a lack of evidence to support routine use of braces in uninjured knees,10,23,24,27,30 the evidence supporting prophylactic shoulder bracing is unclear.3,7,20 Reuss et al25 provided circumstantial recommendations of shoulder braces to help manage anterior shoulder instability after an injury, but we were unable to find clear recommendations for shoulder brace use in athletes susceptible to posterior shoulder labrum injury. Weise et al33 measured the effectiveness of shoulder braces in limiting active and passive shoulder range of motion in collegiate football players. They found that shoulder braces effectively provide protection against the vulnerable position of abduction and external rotation in collegiate football players,33 but no previous study has measured the effectiveness of prophylactic shoulder bracing in preventing recurrent shoulder instability.7,8,11,15 A contributing factor to the lack of evidence-based recommendations for shoulder bracing is that most football players only prophylactically brace their shoulders after having previously suffered a shoulder injury.22 This trend may be attributed to the fact that previous shoulder braces were considered cumbersome,7,21 and many feared a potential limitation in an athlete’s function and level of play.7,22 The offensive line, however, is one position in football where having limited abduction, external rotation, and retraction of the shoulder joint does not significantly affect a player’s level of play on the field.25,33 Since offensive linemen were found to be 15 times more likely to suffer a posterior labral injury when compared with nonfootball players, the use of a stabilizing brace may have a significant impact on injury prevention.12,14,32
An important finding of this retrospective cohort study is the measured injury rate for players wearing a shoulder brace (0.71 posterior shoulder labrum tears per 1000 AEs) was lower than the measured injury rate (1.9 posterior shoulder labrum tears per 1000 AEs) for players not wearing a shoulder brace; however, this difference was not significant given the numbers available. Shoulder injuries are the fourth most common musculoskeletal football injury.1,4,8,12,14,16,21 Kaplan et al16 found that of the 336 collegiate football players invited to the 2004 NFL Combine, 50% had a history of shoulder injury and 33% of shoulder surgery. More specifically, it was found that shoulder injuries resulting in surgery are more common among football linemen.5,6 This is not surprising as linemen often find their shoulders in a compromised position as a result of blocking an opponent.1,4,6,12,14 More important, Brophy et al4–6 concluded that a history of any shoulder instability negatively affects a collegiate football player’s chances of playing in the NFL and significantly reduces career length for defensive linemen. Because our results showed less time loss in the intervention group, it may be argued that prophylactic use of a shoulder-stabilizing brace may improve the future career prospects of collegiate offensive linemen.
In this study, players who wore a shoulder brace had a 54% reduction in risk of posterior shoulder labral tears compared with those who did not wear a shoulder brace. Due to a large 95% CI (0.16-1.30) and a P value of 0.14, these results are not statistically significant. However, the large CI is likely due to the outcome of interest having a low probability and the small number of subjects in the study. A number of publications have shown risk ratios to be an effective method of analyzing the clinical significance of binary outcomes with low probability.9,26,29 Thus, it is our belief that these findings hold clinical significance and warrant further investigation with a larger sample size.
Another noteworthy finding is that shoulder bracing significantly reduces mean time missed (games and contact practices) due to injury (8.7 vs 36.60; P = .0019). Lost time to injury can have significant economic, financial, and psychological consequences for players.13,19,28 Gabbett13 found that lost time to injury results in a loss of training, playing time, and potential employment opportunities. Thus, reducing lost time to injury can have a significant positive effect on players’ careers.
Albright et al1 found that the number of contact practices and games missed by football players depends on the time of the year a player is injured and the severity of the injury. More specifically, players injured early in the fall, which is during the football season, miss significantly more practices and games than players injured late during the fall season.1,21 If a player is injured during the spring season and receives surgery during the spring, they will routinely miss a significant portion of the upcoming fall season.1 For example, the 2 players in this study who underwent surgery for suffering a shoulder injury while wearing a shoulder brace did not have surgery until after the football season was done. In this case, the 2 players did not miss any games, and it can be concluded that the time lost from an injury plays a significant role in the number of games played and practices missed. Thus, it also can be concluded that the timing of an injury can skew the results of the mean time missed per injury statistic.
We also observed that the mean injury rate for freshmen and sophomores was significantly greater than the mean injury rate for juniors and seniors. Freshman football players are required to complete an entrance physical before practicing at the institution in this study. Any existing or suspected injuries suffered during high school are identified and recorded. Thus, it is unlikely that any of the injuries suffered by the freshmen in this study happened during high school. Practices and games missed by players receiving treatment for injuries that originally occurred during high school were not included in this study. Spring practice is an important developmental time for young players.31 It is often the first time these athletes are given the same amount of playing time as their older counterparts.31 For these individuals, it is very important to participate in spring football to enhance their opportunity to play.31 Albright et al1 found a 3-fold increase in injury rate in spring practice when compared with fall practice. Thus, not only are players at a much greater risk of getting injured during spring football practice, the implications of a spring injury on a player’s career as a freshman or sophomore can be devastating.1
This study also found that shoulder bracing does not significantly reduce the number of tears requiring surgery, where 66% of injured and braced shoulders required surgery and 75% of injured and nonbraced shoulders also required surgery. Kaplan et al16 found that the majority of shoulder injuries suffered by football players do not undergo operative treatment, yet offensive linemen are more likely than any other position to suffer a shoulder injury requiring operation. Furthermore, there are no clear guidelines for nonoperative management of in-season shoulder injuries.2,6–8,15 This finding has less meaningful application since offensive linemen are rarely able to adequately function with posterior labral tears that are not repaired.4–8,11
There are some limitations to this study. Only 1 collegiate institution with a single player position was investigated. This limits results and perhaps applicability to the college-level offensive lineman. Treatment bias may also be considered, as only 1 academic surgeon was involved in surgical decision making. The retrospective nature of this study is uncontrollably confounded by factors such as nonrandomization and design. The decision to mandate brace wear may have been because of a spike in posterior labral injuries in offensive linemen. Injury prevention level may also have been variable depending on each athlete’s different blocking techniques, proper or improper brace wear, and skill level. Player misreporting may also have limited the true number of severe shoulder injuries. McCrea et al18 found that football players often underreport injuries to athletic training staff. Further investigation must be performed at various levels of competition and more than 1 institution using a randomized control design to understand whether prophylactic shoulder bracing can prevent posterior labral tears and reduce missed time secondary to injury.
Conclusion
Shoulder injuries are common among college football players. The use of a shoulder-stabilizing brace may reduce the posterior labral tear injury rate in collegiate offensive linemen and decreases amount of contact practices and games missed by injured players. Prophylactically bracing offensive lineman may positively influence the outcome of a football player’s athletic career and risk of injury.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from Northwestern University.
References
- 1. Albright JP, Powell JW, Martindale A, et al. Injury patterns in Big Ten conference football. Am J Sports Med. 2004;32:1394–1404. [DOI] [PubMed] [Google Scholar]
- 2. Aronen JG, Regan K. Decreasing the incidence of recurrence of first time anterior shoulder dislocations with rehabilitation. Am J Sports Med. 1984;12:283–291. [DOI] [PubMed] [Google Scholar]
- 3. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576–580. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine—trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39:22–27. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Chehab EL, Barnes RP, Lyman S, Rodeo SA, Warren RF. Predictive value of orthopedic evaluation and injury history at the NFL combine. Med Sci Sports Exerc. 2008;40:1368–1372. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37:768–775. [DOI] [PubMed] [Google Scholar]
- 7. Burns TC, Owens BD. Management of shoulder instability in in-season athletes. Phys Sportsmed. 2010;38(3):55–60. [DOI] [PubMed] [Google Scholar]
- 8. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32:1430–1433. [DOI] [PubMed] [Google Scholar]
- 9. Deeks J. When can odds ratios mislead? Odds ratios should be used only in case-control studies and logistic regression analyses. BMJ. 1998;317:1155–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Deppen RJ, Landfried MJ. Efficacy of prophylactic knee bracing in high school football players. J Orthop Sports Phys Ther. 1994;20:243–246. [DOI] [PubMed] [Google Scholar]
- 11. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42:2842–2850. [DOI] [PubMed] [Google Scholar]
- 12. Escobedo EM, Richardson ML, Schulz YB, Hunter JC, Green JR, 3rd, Messick KJ. Increased risk of posterior glenoid labrum tears in football players. AJR Am J Roentgenol. 2007;188:193–197. [DOI] [PubMed] [Google Scholar]
- 13. Gabbett TJ. Severity and cost of injuries in amateur rugby league: a case study. J Sports Sci. 2001;19:341–347. [DOI] [PubMed] [Google Scholar]
- 14. Gibbs DB, Lynch TS, Nuber ED, Nuber GW. Common shoulder injuries in American football athletes. Curr Sports Med Rep. 2015;14:413–419. [DOI] [PubMed] [Google Scholar]
- 15. Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90:945–952. [DOI] [PubMed] [Google Scholar]
- 16. Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33:1142–1146. [DOI] [PubMed] [Google Scholar]
- 17. Mair SD, Zarzour RH, Speer KP. Posterior labral injury in contact athletes. Am J Sports Med. 1998;26:753–758. [DOI] [PubMed] [Google Scholar]
- 18. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14:13–17. [DOI] [PubMed] [Google Scholar]
- 19. Meir RA, McDonald KN, Russell R. Injury consequences from participation in professional rugby league: a preliminary investigation. Br J Sports Med. 1997;31:132–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Monk AP, Garfjeld Roberts P, Logishetty K, et al. Evidence in managing traumatic anterior shoulder instability: a scoping review. Br J Sports Med. 2015;49:307–311. [DOI] [PubMed] [Google Scholar]
- 21. Olson DE, Sikka RS, Hamilton A, Krohn A. Football injuries: current concepts. Curr Sports Med Rep. 2011;10:290–298. [DOI] [PubMed] [Google Scholar]
- 22. Owens BD, Dickens JF, Kilcoyne KG, Rue JP. Management of mid-season traumatic anterior shoulder instability in athletes. J Am Acad Orthop Surg. 2012;20:518–526. [DOI] [PubMed] [Google Scholar]
- 23. Pietrosimone BG, Grindstaff TL, Linens SW, Uczekaj E, Hertel J. A systematic review of prophylactic braces in the prevention of knee ligament injuries in collegiate football players. J Athl Train. 2008;43:409–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Requa RK, Garrick JG. A review of the use of prophylactic knee braces in football. Pediatr Clin North Am. 1990;37:1165–1173. [DOI] [PubMed] [Google Scholar]
- 25. Reuss BL, Harding WG, 3rd, Nowicki KD. Managing anterior shoulder instability with bracing: an expanded update. Orthopedics. 2004;27:614–618. [DOI] [PubMed] [Google Scholar]
- 26. Sackett DL. Why randomized controlled trials fail but needn’t: 2. Failure to employ physiological statistics, or the only formula a clinician-trialist is ever likely to need (or understand!). CMAJ. 2001;165:1226–1237. [PMC free article] [PubMed] [Google Scholar]
- 27. Salata MJ, Gibbs AE, Sekiya JK. The effectiveness of prophylactic knee bracing in american football: a systematic review. Sports Health. 2010;2:375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shuer ML, Dietrich MS. Psychological effects of chronic injury in elite athletes. West J Med. 1997;166:104–109. [PMC free article] [PubMed] [Google Scholar]
- 29. Sistrom CL, Garvan CW. Proportions, odds, and risk. Radiology. 2004;230:12–19. [DOI] [PubMed] [Google Scholar]
- 30. Sitler M, Ryan J, Hopkinson W, et al. The efficacy of a prophylactic knee brace to reduce knee injuries in football. A prospective, randomized study at West Point. Am J Sports Med. 1990;18:310–315. [DOI] [PubMed] [Google Scholar]
- 31. Stodden DF, Galitski HM. Longitudinal effects of a collegiate strength and conditioning program in American football. J Strength Cond Res. 2010;24:2300–2308. [DOI] [PubMed] [Google Scholar]
- 32. Tannenbaum E, Sekiya JK. Evaluation and management of posterior shoulder instability. Sports Health. 2011;3:253–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weise K, Sitler MR, Tierney R, Swanik KA. Effectiveness of glenohumeral-joint stability braces in limiting active and passive shoulder range of motion in collegiate football players. J Athl Train. 2004;39:151–155. [PMC free article] [PubMed] [Google Scholar]


