Abstract
Objectives
Sexually transmitted infections (STIs) are significant public health and financial burdens in the United States. This manuscript examines the relationship between substance use and prevalent and incident STIs in HIV-negative adult patients at STI clinics.
Methods
A secondary analysis of Project AWARE was performed based on 5,012 patients from 9 STI clinics. STIs were assessed by laboratory assay and substance use by self-report. Patterns of substance use were assessed using latent class analysis. The relationship of latent class to STI rates was investigated using Poisson regression by population groups at high risk for STIs defined by participant’s and partner’s gender
Results
Drug use patterns differed by risk group and substance use was related to STI rates with the relationships varying by risk behavior group. Substance use treatment participation was associated with increased STI rates
Conclusions
Substance use focused interventions may be useful in STI clinics to reduce morbidity associated with substance use. Conversely, gender-specific sexual health interventions may be useful in substance use treatment.
Keywords: sexually transmitted infections, substance use, substance use treatment, gender differences
1. INTRODUCTION
Despite efforts to promote sexual risk reduction (Centers for Disease Control and Prevention (CDC), 2014; Owusu-Edusei et al., 2013; Satterwhite et al., 2013), sexually transmitted infections (STIs) still remain a significant financial and public health burden in the United States (U.S.). Current estimates indicate that STIs in the U.S. are increasing (Bowen et al., 2015; Patton et al., 2014) with an overall prevalence of 110 million infections and incidence of 20 million new cases per year in the U.S. (CDC, 2013; Satterwhite et al., 2013). Substance users are at increased risk for STIs including HIV (Belani et al., 2012, Des Jarlais, et al., 2011).
Substance using STI clinic patients have demonstrated higher rates of condomless sex, multiple partners and STI diagnoses compared with their counterparts who do not have a history of substance use (Cachay et al., 2004; Cook et al., 2006; Scott-Sheldon et al., 2009). The type of drug used influences the relationship between substance use and sexual behavior, depending on its pharmacological effects and reason for use (Leigh, 2002; Leigh et al., 2008; Rawson et al., 2002, Scott-Sheldon et al., 2009). For example, in one study, only use of amphetamines, but not alcohol, cocaine or marijuana, was associated with decreased condom use (Leigh et al., 2008). Yet in other studies, crack/cocaine use but not heroin use was associated with higher risk behavior scores (Lejuez et al., 2005). Crack cocaine use, in particular, has been found to be associated with increased number of sexual partners (Harzke et al., 2009) and STIs (Ross et al., 2002). Thus evidence points to the importance of type of substance but variability in results point to the potential importance of other factors.
There are gender differences in levels of drug use and drug of choice and the relationships among drug use, sexual risk and STIs. In general, the substance use literature has shown that men are more likely to use substances than women (Cotto et al., 2010, Huang et al., 2006) and men show higher rates of abuse and dependence of alcohol and marijuana, however, women have higher rates of dependence on cocaine and psychotherapeutics (pain relievers, stimulants, tranquilizers and sedatives; Cotto et al., 2010). Crack/Cocaine use and dependence has been found to be particularly elevated for inner-city female substance users relative to males (Lam et al., 2004, Lejuez et al. 2007). Gender power imbalances, such as intimate partner violence, and specific types of drug markets associated with specific sexual networks, such as crack and heroin markets, have shown to be associated with differentially heightened STI risks that are both sexual- and drug-related (Decker et al., 2014; Jennings et al., 2013).
The relationship between substance use and sexual risk is further compounded by evidence that level of drug use and type of drug used, sexual risk behavior, STIs and their interrelationships differ not only by gender but also by partner gender and that STI transmission rates vary by contact type and partnership networks (Adams et al., 2013; Kopetz et al., 2014). Both men who have sex with men (MSM) and women who have sex with women (WSW) have higher rates of substance use than their heterosexual counterparts (Cochran et al., 2004, McCabe et al., 2009) and the relationship between particular substances used and sexual risk varies across gender and partner gender (LaBrie et al., 2005; Leigh et al., 2008; Scott-Sheldon et al., 2009). A 2016 study found that heavy alcohol use is associated with multiple partners for women and men who have sex with men (MSM) only, but not for heterosexual men, demonstrating how partner gender may impact the extent to which specific drugs increase sexual risk behaviors (Carey et al., 2016). A literature review exclusive to MSM showed that binge drinking and methamphetamine use are consistently associated with risky sexual behaviors and concluded that not enough research had been conducted with other substance types (Vosburgh et al., 2012). Therefore, while prior studies have studied the association between substance use and STI incidence within a few particular subgroups defined by type of drug, STI, and/or gender/partner gender, few studies have investigated across multiple types of substances used, gender and partner gender and risk of STIs in a single analysis. It is within this context that the objective of this study was to assess the relationship across subgroups of substance classes and sexuality groups to identify gender-specific and substance-specific risk factors associated with STI prevalence and incidence.
In this secondary analysis, we evaluate the effect of substance use patterns on STI acquisition and hypothesize that 1) substance use patterns will differ by gender and partner gender, 2) more severe substance use patterns will be associated with higher STI prevalence at baseline and 6-month cumulative incidence of STIs and 3) there will be differences in the relationship between patterns of substance use and STIs across gender and partner gender. Compared to other types of substance use, we expect methamphetamine and club drugs to have higher impact for MSM (Pappas and Halkitis, 2011; Senn et al., 2009; Shoptaw, 2006; Shoptaw and Reback, 2007; Theodore et al., 2014; Vosburgh et al., 2012), and marijuana, alcohol and cocaine, particularly crack cocaine, to have higher impact in women and men who have sex with women (MSW; Cavanaugh et al., 2011; Kopetz et al., 2014; Lejuez et al., 2007). We also examine the impact of participation in substance use treatment on STIs.
2. METHODS
2.1 Participants
Project AWARE (Metsch et al., 2013), recruited 5,012 patients seeking services from STI clinics in nine U.S. cities between April and December, 2010. After baseline behavioral assessment and STI testing, patients were randomized to either: (1) HIV testing with brief risk reduction counseling, or (2) a control condition where patients received HIV testing with information only about HIV and HIV testing. Six months later, participants returned for repeated assessment and STI testing. The study was approved by the Institutional Review Boards at each site. All participants provided written informed consent prior to study activities and were compensated up to $90 for study participation. Eligibility criteria included being: (1) 18 years or older, (2) able to communicate in English, (3) HIV-negative or unknown HIV status, (4) able to provide contact information and consent for STI and HIV testing, HIPAA and/or medical record releases, and (5) able to confirm they had no plans to leave the area for 6-months.
2.2 Measures
For the present analysis, participants were classified into four risk behavior groups: MSM, MSW, women who have sex with men only (WSM) and women who have sex with women (WSW). Transgender individuals were grouped with males if they had a penis due to the similarity of possible behaviors. Males who reported episodes of anal or oral sex with another male were classified as MSM. All other males were classified as MSW. Similarly, women who reported sex with women were classified as WSW.
Specimens for STI testing were collected at baseline and 6-months. Urine samples from MSM and MSW, rectal samples from MSM, and cervical/vaginal samples from female participants were collected and tested for Neisseria gonorrhea (GC) and Chlamydia trachomatis (CT) in all participants and Trichomonas vaginalis (TV) in women. Blood serum samples were collected from all participants for testing syphilis and Herpes Simplex-2 (HSV-2, tested by Elisa, confirmed by Western blot). Finger-stick blood was used for HIV rapid testing.
History of STI in the 6 months before baseline was assessed by self-report. A participant with a positive baseline laboratory STI test was considered to have a prevalent STI. Cumulative 6-month STI incidence was ascertained by laboratory STI tests at follow-up and medical record abstraction for only the STIs listed above. Participants positive for STIs at baseline were considered an incident case only if their positive diagnosis occurred after adequate treatment. Incident HSV-2 and/or HIV required the patient be negative at baseline.
Self-reported sexual risk and substance use behaviors over the prior 6-months were collected at baseline using an Audio Computer-Assisted Self-Interview (ACASI). Sexual behavior was assessed through query about participants’ vaginal and/or anal sexual episodes and partners with and without condoms. Drug use severity was measured by the Drug Abuse Screening Test (DAST-10; Yudko et al., 2007). Moderate and substantial severity were defined by DAST-10 score equal or greater than three but less than six, and equal or greater than six, respectively. Alcohol misuse was categorized as moderate or severe based on the Alcohol Use Disorders Identification Test (AUDIT-C), with scores equal or greater than 3 and less than 6 (in women) or equal or greater than 4 and less than 7 (in men) considered moderate and scores greater than 6 or 7 considered severe. Participants were asked to indicate, from a given list of specific substances, which drugs they had used in the prior six months, then about their frequency of use in the prior six months. Frequency of use was asked as none, less than once a month, 1–3 times a month, once a week, more than once a week but less than daily, and daily. These substances included: amphetamines, cocaine (separately for powder and crack form), MDMA (ecstasy), Ketamine (Special K), GHB and inhalants, heroin and pain pills, hallucinogens, PCP, tranquilizers/barbiturates and marijuana (with or without prescription). Participants were also asked to indicate if they had injected any of these drugs in the prior six months. The higher categories of frequency of use were subsequently combined to weekly or more to create four-ordered categories for the latent-class analysis. Uptake of substance use treatment in the 6-months prior to baseline was asked separately for alcoholics or narcotics anonymous (AA/NA) or professional treatment (including outpatient, inpatient, and detoxification).
2.3 Analyses
Descriptive tables are stratified by risk behavior group (MSM, MSW, WSM and WSW). Substance use was analyzed using latent class analysis (LCA) in Mplus V7.4 (Muthén and Muthén, 2012). In this analysis, MSW, MSM and women were treated as multiple groups. WSW were not treated as a separate group in the latent class due to the smaller number of WSW. WSW status was used as a covariate to predict latent class membership, thus allowing the proportions in each class to differ between WSM and WSW. Analyses with different numbers of classes were compared and the solution with the smallest Adjusted Bayesian Information Criteria (aBIC; Sclove, 1987) was chosen (Dziak et al., 2014). Invariance in thresholds was tested to determine whether the proportions of different drugs within a class varied across risk groups. Individual’s probabilities of class membership were used to take 20 pseudo-class draws (Bandeen-Roche et al., 1997; Wang et al., 2005) from each individual’s multinomial distribution using SAS 9.3. The following analyses were run 20 times, once for each pseudo-class draw, and combined using Rubin’s combining rules for multiple imputation (Li et al., 1991; Rubin, 1987) to account for the uncertainty of class membership and ensure appropriate standard errors. STI rates were directly estimated using Poisson regression with a log link function to examine risk ratios as well as risk levels (Barros and Hirakata, 2003). Unadjusted models were estimated to test for simple risk differences by risk behavior group for prevalent and incident STI as a function of substance use class. Adjusted risk differences controlled for age, race/ethnicity, education, marital status, site of recruitment, randomized treatment, number of unprotected sex acts and unprotected partners. Rates of substance use treatment by substance use class and the relationship of treatment to STI rates are reported using three categories: no treatment, attendance at alcoholics anonymous or narcotics anonymous (AA/NA) meetings or use of professional substance use treatment (with possible concurrent AA/NA attendance). The Benjamini-Hochberg procedure (Benjamini and Hochberg, 1995) is used to control the family-wise error rate to .05 within each hypothesis.
3. RESULTS
3.1 Sample Characteristics
The sample of 5,012 patients were 45.1% black, 31.8% white, and 15.3% Hispanic (Table 1). The majority of the sample (61.5%) had more than a high school education, while approximately one-quarter (25.8%) had a high school education and 12.7% had less than a high school education. Almost three-quarters (74%) were single. Over one-third (36.7%) of the sample was in the lowest income bracket ($0–5,000), and also over one-third (35.0%) was in the second lowest income bracket ($5,001–20,000). The overall sample also included MSW (38.1%), MSM (27.9%), WSM (29.8%) and WSW (4.2%). Table 1 shows all of the sample characteristics for these four groups.
Table 1.
Sample Characteristics by Gender and Partner Gender
| Demographics: | MSW Only | MSM | WSM | WSW | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n=1908 | n=1400 | n=1492 | n=212 | n=5012 | ||||||
| n | % | n | % | n | % | N | % | n | % | |
| Race/Ethnicity | χ2(9) = 757.78 | p < .001 | ||||||||
| Hispanic | 167 | 8.8 | 409 | 29.2 | 156 | 10.5 | 34 | 16.0 | 766 | 15.3 |
| Black | 1076 | 56.4 | 225 | 16.1 | 873 | 58.5 | 85 | 40.1 | 2259 | 45.1 |
| White | 539 | 28.2 | 602 | 43.0 | 368 | 24.6 | 83 | 39.2 | 1592 | 31.7 |
| Other | 126 | 6.6 | 164 | 11.7 | 95 | 6.4 | 10 | 4.7 | 395 | 7.9 |
| Education | χ2(6) = 329.78 | p < .001 | ||||||||
| < High School | 322 | 16.9 | 70 | 5.0 | 216 | 14.5 | 28 | 13.2 | 636 | 12.7 |
| High School | 623 | 32.7 | 204 | 14.6 | 424 | 28.4 | 43 | 20.3 | 1294 | 25.8 |
| > High School | 963 | 50.5 | 1126 | 80.4 | 852 | 57.1 | 141 | 66.5 | 3082 | 61.5 |
| Marital Status1 | χ2(6) = 119.01 | p < .001 | ||||||||
| Married or Partnered | 271 | 14.2 | 221 | 15.8 | 175 | 11.8 | 30 | 14.2 | 697 | 13.9 |
| Divorced/Sep./Wid. | 298 | 15.6 | 60 | 4.3 | 221 | 14.9 | 24 | 11.3 | 603 | 12.1 |
| Single | 1338 | 70.2 | 1117 | 80.0 | 1092 | 73.4 | 158 | 74.5 | 3705 | 74.0 |
| Income Category2 | χ2(4) = 566.49 | p < .001 | ||||||||
| $0–$5,000 | 767 | 41.0 | 271 | 19.7 | 674 | 46.5 | 85 | 40.7 | 1797 | 36.7 |
| $5,001–$20,000 | 661 | 35.3 | 416 | 30.3 | 550 | 37.9 | 88 | 42.1 | 1715 | 35.0 |
| $20.001–40,000 | 286 | 15.3 | 330 | 24.0 | 162 | 11.2 | 26 | 12.4 | 804 | 16.4 |
| $40,001 and up | 157 | 8.4 | 356 | 25.9 | 64 | 4.41 | 10 | 4.78 | 587 | 12.0 |
| Age [Mean | SD]3 | 34.2 | (12.1) | 31.0 | (10.0) | 30.4 | (10.6) | 28.8 | (8.0) | 32.0 | (11.1) |
| Unprotected Partners [Mean I SE]4 | 1.6 | (0.1) | 3.26 | (0.1) | 1.6 | (0.1) | 2.0 | (0.2) | 2.1 | (0.04) |
| Unprotected Sex Acts [Mean I SE]4 | 25.7 | (1.2) | 16.8 | (0.9) | 24.7 | (1.29) | 36.3 | (5.0) | 23.3 | (0.7) |
| Sexually Transmitted Infections5 | Each | p < .001 | ||||||||
| Self-Report prior 6 Months | 354/1908 | 18.6 | 332/1399 | 23.7 | 409/1491 | 27.4 | 45/212 | 21.2 | 1140/5010 | 22.8 |
| Prevalent | 718/1874 | 38.3 | 504/1292 | 39.0 | 829/1455 | 57.0 | 90/210 | 42.9 | 2141/4831 | 44.3 |
| Incident | 93/1518 | 6.1 | 174/1134 | 15.3 | 194/1245 | 15.6 | 15/174 | 8.62 | 476/4071 | 11.7 |
| Substance Use6: | n=1901 | n=1392 | n=1469 | n=211 | n=4973 | |||||
| Any Drug Use | 1137 | 59.8 | 765 | 55.0 | 726 | 49.4 | 153 | 72.5 | 2781 | 55.9 |
| Any Drug excl. Marijuana | 531 | 27.9 | 487 | 35.0 | 349 | 23.7 | 99 | 46.9 | 1466 | 29.4 |
| Heroin | 28 | 1.5 | 15 | 1.1 | 22 | 1.5 | 8 | 3.8 | 73 | 1.5 |
| Crack Cocaine | 156 | 8.2 | 45 | 3.2 | 106 | 7.2 | 26 | 12.3 | 333 | 6.7 |
| Powder Cocaine | 164 | 8.6 | 198 | 14.2 | 101 | 6.9 | 31 | 14.7 | 494 | 9.9 |
| Amphetamines | 39 | 2.1 | 118 | 8.5 | 29 | 2.0 | 10 | 4.7 | 196 | 3.9 |
| Ecstasy | 117 | 6.2 | 179 | 12.9 | 87 | 5.9 | 36 | 17.1 | 419 | 8.4 |
| Hallucinogens | 58 | 3.1 | 78 | 5.6 | 30 | 2.0 | 25 | 11.9 | 191 | 3.8 |
| Ketamine | 13 | 0.7 | 40 | 2.9 | 9 | 0.6 | 8 | 3.8 | 70 | 1.4 |
| GHB | 4 | 0.2 | 91 | 6.5 | 4 | 0.3 | 5 | 2.4 | 104 | 2.1 |
| Inhalants | 7 | 0.4 | 253 | 18.2 | 3 | 0.2 | 4 | 1.9 | 267 | 5.4 |
| Pain Pills | 110 | 5.8 | 100 | 7.2 | 74 | 5.0 | 34 | 16.1 | 318 | 6.4 |
| Tranquilizers | 46 | 2.4 | 65 | 4.7 | 54 | 3.7 | 21 | 10.0 | 186 | 3.7 |
| PCP | 4 | 0.2 | 3 | 0.2 | 2 | 0.1 | 5 | 2.4 | 14 | 0.3 |
| Substance Use Severity: | ||||||||||
| Current Injectors (0–6 mos)7 | 107/1908 | 5.6 | 86/1398 | 6.2 | 87/1491 | 5.8 | 25/212 | 11.8 | 305/5009 | 6.1 |
| Alcohol Problem Severity | χ2(6) = 103.07 | p < .001 | ||||||||
| Moderate | 445/1898 | 23.5 | 358/1391 | 25.7 | 463/1484 | 31.2 | 99/212 | 46.7 | 1396/4985 | 27.4 |
| Substantial | 274/1898 | 14.4 | 160/1391 | 11.5 | 106/1484 | 7.1 | 26/212 | 12.3 | 566/4985 | 11.4 |
| Drug Use Severity | χ2(6) = 67.13 | p < .001 | ||||||||
| Moderate | 340/1884 | 18.1 | 203/1371 | 14.8 | 148/1453 | 10.2 | 32/211 | 15.2 | 723/4919 | 14.7 |
| Substantial | 211/1884 | 11.2 | 113/1371 | 8.2 | 156/1453 | 10.7 | 40/211 | 19 | 520/4919 | 10.6 |
| Substance Use Treatment: | χ2(6) = 69.90 | p < .001 | ||||||||
| AA/NA Only | 103/1907 | 5.4 | 52/1397 | 3.7 | 50/1490 | 3.4 | 7/212 | 3.3 | 212/5006 | 4.2 |
| Professional Treatment8 | 225/1906 | 11.8 | 66/1397 | 4.7 | 176/1490 | 11.8 | 27/212 | 12.7 | 494/5006 | 9.9 |
Sample sizes vary due to missing data: MSW N=1907, MSM N=1398, WSM N=1488, WSW N=212
Sample sizes vary due to missing data: MSW N=1871, MSM N=1373, WSM N=1450, WSW N=209
F(3,5008)=46.65, p<.001
Estimates are from a negative binomial model and the appropriate measure of dispersion is the standard error. Unprotected Sex Acts: χ2(3)=52.42, p<.001, Unprotected Partners χ2(3)=290.68, p<.001
Self-Report: χ2(3) =38.75, Prevalent: χ2(3) = 136.78, Incident: χ2(3) = 80.02, Repeated: χ2(2) = 107.43
All substance use comparisons are significant with p<.001
χ2(3) = 13.01, p<.005
May also participate in AA/NA
STI data showed that 22.8% of the overall sample self-reported an STI in the six months prior to baseline. Furthermore, 44.3% had a confirmed prevalent STI at baseline and 11.7% presented with a cumulative incident STI.
Overall, 55.9% of all participants reported having used at least one drug (not including alcohol), 29.4% reported having used a drug other than marijuana, and 6.1% of the sample reported injecting drugs within the last six months. Use of each drug differed significantly by risk behavior group. Generally, WSM were the least likely to report using drugs, while WSW, followed by MSM, were most likely to report drug use other than marijuana. MSM had much lower crack cocaine use than MSW and WSM; WSW showed the highest level of crack use. Overall attendance at substance use treatment was low in the sample, with 4.2% reporting AA/NA and 9.9% reporting some professional treatment.
3.2 Hypothesis 1—Latent Classes of Substance Use
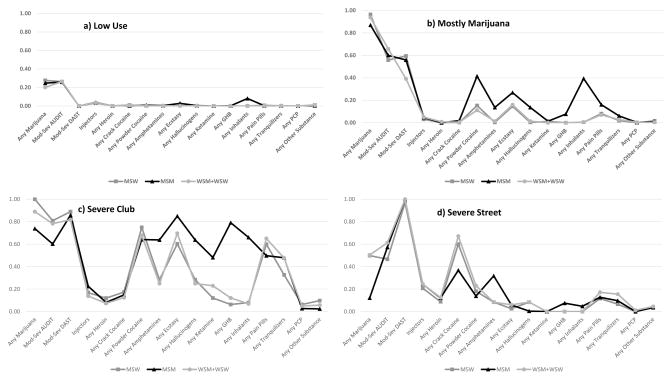
A four class solution had the lowest aBIC score and an entropy score of .91, indicative of good class separation. The class measurement across risk groups (MSW, MSM, WSM and WSW) was significantly different (χ2(320)=1188.26, p < .001); however, there were very common patterns of use across risk groups within classes allowing similar interpretation of the classes across groups. Figure 1 shows the four classes with each risk group plotted within each class plot. Panel a) shows the Low Use substance use class (SUC) with a slightly more than 20% probability of marijuana use and for MSM a small probability of ecstasy or inhalant use. Panel b) shows the Mostly Marijuana SUC in which nearly all members are marijuana users and around 60% show at least moderately severe alcohol and drug use problems. There is also some use of powder cocaine and club drugs in this class. Panel c) is the Severe Club SUC with high levels of powder cocaine, ecstasy, GHB, and hallucinogens (all frequently used when attending dance clubs) as well as pain pills and tranquilizers/sedatives. The final panel, d) shows the Severe Street SUC in which injection, heroin and crack cocaine are at their highest of all the classes. Nearly all in this final class show at least moderate drug use severity. Across these classes, patterns of use for MSW and all women (WSM and WSW) are quite similar. MSM, in contrast, show elevated levels of use of many of the substances within each class. There are also quantitative differences in the proportions of each risk group in each class in addition to these qualitative differences among classes. Table 2 shows the proportion of each risk group in each of the classes which differed significantly overall and between all pairwise comparisons of risk group (p < .001, all significant after multiple testing correction). WSW have the lowest proportion in the Low Use SUC and the highest proportion in each of the other SUCs. MSW, WSM and WSW have higher proportions in the Severe Street SUC than do MSM.
Figure 1. Profiles of Substance Use within Classes.
Lines plot the probability any use of the particular substance (or type of use for Injectors and Mod-Sev Dast)within each of the four plots. MSM are represented by the darkest line and WSM+WSW are represented by the lightest line.
Table 2.
Substance Use Class Membership by Risk Groups1
| MSW | MSM | WSM | WSW | Totals | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Substance Use Class (SUC) | Count | % | Count | % | Count | % | Count | % | Count | % |
| Low Use | 1144.7 | 60.0 | 927.3 | 66.3 | 1001 | 67.1 | 80.2 | 37.8 | 3153.2 | 62.9 |
| Mostly Marijuana | 476.8 | 25.0 | 322.9 | 23.1 | 297.5 | 19.9 | 75.4 | 35.6 | 1172.6 | 23.4 |
| Severe Club Use | 63.6 | 3.3 | 74.6 | 5.3 | 42.98 | 2.9 | 32.0 | 15.1 | 213.1 | 4.3 |
| Severe Street Use | 222.9 | 11.7 | 74.3 | 5.3 | 150.5 | 10.1 | 24.4 | 11.5 | 472.1 | 9.4 |
| Totals | 1908 | 1399 | 1492 | 212 | 5011 | |||||
Counts are based on the sum of posterior probabilities of class membership across the sample.
3.3 STIs
Table 3 shows the rates of prevalent and incident STIs by substance use class and risk group in both unadjusted and adjusted models (See Supplemental Table 11 for statistical significance of model terms). In general, adjusting for demographics and sexual risk decreases predicted STI rates at least slightly for all groups other than MSM where adjustment increases rates in nearly all STI/SUC combinations. To address hypotheses 2 and 3 we examined both contrasts of different SUCs across and within risk group.
Table 3.
Rates of Sexually Transmitted Infections by Substance Use Class Membership and Risk Groups
| MSW | MSM | WSM | WSW | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STI Rates | Unadjusted | Adjusted | UnAdjusted | Adjusted | UnAdjusted | Adjusted | UnAdjusted | Adjusted | ||||||||
| SUC | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) |
| Baseline Prevalence | ||||||||||||||||
| Low Use | 39.7 | (36.9, 42.7) | 28.3 | (25.7, 31.2) | 35.8 | (32.7, 39.3) | 45.9 | (41.2, 51.2) | 55.4 | (52.2, 58.7) | 42.8 | (39.3, 46.7) | 34.0 | (24.5, 47.1) | 30.2 | (22.0, 41.6) |
| Marijuana | 31.4 | (27.1, 36.4) | 25.3 | (21.7, 29.6) | 41.5 | (36.0, 47.9) | 57.1 | (48.6, 66.9) | 53.0 | (46.7, 60.2) | 46.7 | (41.0, 53.1) | 37.9 | (27.3, 52.6) | 41.6 | (29.9, 57.9) |
| Severe Club | 23.1 | (14.2, 37.4) | 25.9 | (15.1, 44.3) | 51.3 | (40.5, 65.1) | 74.0 | (55.4, 98.7) | 43.4 | (28.7, 65.5) | 49.8 | (33.1, 74.9) | 40.2 | (25.5, 63.4) | 46.9 | (26.8, 82.3) |
| Severe Street | 49.3 | (42.4, 57.2) | 28.9 | (24.3, 34.4) | 52.2 | (40.7, 66.8) | 49.4 | (39.1, 62.4) | 81.3 | (74.2, 89.1) | 54.6 | (48.5, 61.4) | 90.2 | (77.6, 100.0) | 61.7 | (50.8, 74.9) |
| 6-Month Cumulative Incidence | ||||||||||||||||
| Low Use | 6.1 | (4.6, 8.) | 4.2 | (3.0, 5.9) | 13.7 | (11.4, 16.4) | 14.8 | (11.3, 19.3) | 13.9 | (11.7, 16.6) | 9.2 | (7.0, 12.1) | 4.9 | (1.3, 18.9) | 4.2 | (1.1, 16.2) |
| Marijuana | 7.7 | (5.1, 11.7) | 4.9 | (3.0, 8.1) | 16.6 | (12.3, 22.4) | 20.0 | (13.9, 28.9) | 8.8 | (2.1, 37.2) | 5.8 | (1.0, 35.2) | 9.2 | (2.5, 33.9) | 11.0 | (2.8, 42.5) |
| Severe Club | 4.5 | (1.0, 20.6) | 5.5 | (1.2, 24.3) | 28.7 | (18.9, 43.6) | 35.5 | (22.0, 57.2) | 17.4 | (13.0, 23.2) | 12.8 | (9.0, 18.1) | 8.9 | (3.7, 21.4) | 8.2 | (3.4, 20.0) |
| Severe Street | 3.4 | (1.3, 8.7) | 2.3 | (0.8, 7.0) | 17.0 | (8.7, 33.3) | 16.6 | (7.3, 37.5) | 23.0 | (16.3, 32.4) | 19.6 | (13.1, 29.3) | 17.1 | (5.9, 50.1) | 7.6 | (1.3, 46.) |
3.3.1 Hypothesis 2—Severity of Substance Use and STI Rates across Risk Groups
All comparisons with p<.0083 were statistically significant after multiple testing correction. The Severe Street SUC was associated with significantly higher rates of prevalent STIs (RR=1.63, (1.44, 1.84); aRR=1.30, (1.15, 1.47)) relative to the Low Use SUC controlling for risk group. In the unadjusted model for prevalent STIs, Severe Street SUC had significantly higher rates of STI relative to both the Severe Club SUC (RR=174, (1.39, 2.18))) and the Mostly Marijuana SUC (RR=1.64, (1.42, 1.99)) controlling for risk group.
3.3.2 Hypothesis 3—SUC Differences within Risk Group
All contrasts with p < .015 were statistically significant after multiple testing correction. MSM within the Severe Club SUC relative to the Low Use SUC were at elevated risk for prevalent (RR=1.43, (1.11, 1.85), aRR=1.61, (1.20, 2.17)) and incident STIs ((RR=2.10, (1.34, 3.31.85), aRR=2.41, (1.49, 3.88)). WSM within the Severe Street SUC relative to WSM in the Low Use SUC were also at elevated risk for prevalent (RR=1.47, (1.32, 1.63), aRR=1.27, (1.14, 1.43)) and incident STIs (RR=1.65, (1.12, 2.43), aRR=2.12, (1.36, 3.31)). WSW in the Severe Street SUC relative to WSW in the Low Use SUC had elevated prevalent (RR=2.66, (1.84, 3.83), aRR=2.04, (1.42, 2.93)). MSW in the Severe Street SUC had significantly higher risk of prevalent STIs in unadjusted analyses relative to MSW in Severe Club SUC (RR=2.14, (1.29, 3.55), the Mostly Marijuana SUC (RR=1.57 (1.26, 1.96)) and the Low Use SUC (RR=1.24, (1.05, 1.47)). There were no significant differences in incident STIs across SUCs for MSW. This same pattern of unadjusted prevalent STI rates held for both WSM and WSW (Supplemental Table 22). Supplemental Table 33 shows risk ratios among risk groups within SUCs. Within the Severe Street SUC both MSM and MSW have lower rates of STIs than do WSW and WSM.
3.4 Substance Use Treatment
The proportion of participants reporting substance use treatment increased with the increasing severity of the SUC (Supplemental Table 44). Rates of professional treatment were high within the Severe Street SUC for WSM (58.3%) and WSW (70.8%). Rates of substance use treatment in the Severe Club SUC were lower (12.1% across gender and partner gender). MSM had the lowest rates of professional substance abuse treatment within the Severe Club (10.0%) and Severe Street (30.7%) SUCs. Adding substance use treatment as a predictor of STI rates (Table 4) showed that the No Treatment group had significantly lower rates of prevalent STIs than either the AA/NA only group (RR=0.79, (0.69, 0.90)) or the professional treatment group (RR=0.85, (0.77, 0.94)).
Table 4.
Rates of Sexually Transmitted Infections by Substance Use Treatment
| Prevalent | Incident | |||||||
|---|---|---|---|---|---|---|---|---|
| Substance Use Treatment | Unadjusted1 | Adjusted | Unadjusted1 | Adjusted | ||||
| Category | % | (95%CI) | % | (95%CI) | % | (95%CI) | % | (95%CI) |
| No Treatment | 42.7 | (40.0, 45.7) | 41.7 | (38.2, 45.6) | 10.2 | (8.2, 12.7) | 8.2 | (6.1, 11.0) |
| AA/NA | 54.2 | (47.6, 61.7) | 44.4 | (38.2, 51.7) | 11.8 | (8.1, 17.4) | 12.9 | (8.5, 19.6) |
| Professional Treatment | 50.4 | (45.6, 55.7) | 43.5 | (38.7, 48.8) | 11.8 | (8.8, 16.0) | 10.3 | (7.1, 14.9) |
4. DISCUSSION
Substance use was high in this sample of STI patients from 9 STD clinics throughout the U.S. Over half of the sample reported use of any drugs and 29.4% reported using drugs other than marijuana. Over one quarter showed moderate to severe levels of substance use severity. These rates are considerably higher than the general population; namely the 2013 National Survey on Drug Use and Health (Substance Abuse Mental Health Services Administration, 2014) reported that 16% of the U.S. population over 12 years of age reported any illicit drug use in the last year (8.2% illicit drugs other than marijuana). Substance use treatment in the sample was low as is true nationally (Compton et al., 2007). Among individuals in the Severe Street class, substance use treatment was higher but still only around 50%. MSM had particularly low rates of treatment.
Our latent class analysis confirmed our hypothesis that across different risk groups, based on gender and partner-gender, there are different patterns of substance use: WSW had the highest proportions of all risk groups in both the Severe Club SUCs. MSM had the lowest proportion of all risk groups in the Severe Street and the highest in the Severe Club SUCs. There was little difference in proportion of MSW, WSM, and WSW 10.1% to 11.7 % in the Severe Street SUC (10.1%–11.7%).
Hypothesis 2, predicting an association between more severe substance use patterns and higher STI rates, was confirmed with Severe Street SUC having significantly higher prevalent STIs controlling for risk group; however, Hypotheses 3 showed that this pattern differed across risk group with MSM in the Severe Club SUC showing elevations in both STI measures relative to MSM in the Low Use SUC. Higher levels of STIs were seen in Severe Street SUC relative to the Low Use SUC for both WSM (prevalent and incident) and WSW (prevalent). MSW showed the least relationship between substance use and STIs with only unadjusted prevalent STIs being different in the Severe Street SUC than in all other SUCs. STIs were also lowest in MSW.
Much research has pointed to how use of a particular substance within a particular risk group is related to sexual risk behavior or STIs (Logan et al., 1998; Nuttbrock et al., 2000; Pappas and Halkitis, 2011; Shoptaw, 2006; Shoptaw and Reback, 2007; Stahlman et al., 2013; Theodore et al., 2014; Vosburgh et al., 2012; Wechsberg et al., 2015). The current investigation was able to compare and statistically test differences among four risk-groups—MSM, MSW, WSM and WSW—across empirically determined SUCs in their risk for a uniformly tested battery of STIs. Overall, substance use was related to STIs, but this differed by risk behavior groups suggesting that interventions might differentially target these groups, delineated by gender and partner gender, depending on their substance use patterns. For WSM and WSW, and a lesser extent MSW, the Severe Street SUC typified by high levels of crack cocaine use was the primary risk for STIs, whereas for MSM the Severe Club SUC typified by powder cocaine, methamphetamine, ecstasy, hallucinogens as well as pain pill use showed elevated risk. These relationships were apparent even after controlling for the level of sexual risk, suggesting that the increased risk may work through drug users’ sexual networks rather than changes in risky behaviors (Schneider et al., 2013; Tobin et al., 2011). Use of club drugs and methamphetamines is particularly high in MSM, and has been associated with heightened disease transmission (Cheng et al., 2010; Colfax and Guzman, 2006; Green and Halkitis, 2006; Mansergh et al., 2006; Purcell et al., 2005; Semple et al., 2011; Thiede et al., 2009; Wohl et al., 2008; Zuckerman and Boyer, 2012). Furthermore, previous studies have documented high crack cocaine and other cocaine use and dependence among women compared to men, and associated this with high levels of STIs/HIV due to factors like trading sex tfor money or drugs with anonymous or recently incarcerated partners (Absalon et al., 2006; Cavanaugh et al., 2011; Kopetz et al., 2014; Lejuez et al., 2007; Logan et al., 1998; Nuttbrock et al., 2000; Stahlman et al., 2013). Tailored interventions can specifically target women who use drugs by addressing the proximal and distal factors that contribute to women’s drug use, engagement in sex trade, and HIV risk, including childhood abuse, homelessness and unemployment (Edwards et al., 2006; El-Bassel and Strathdee, 2015; Wechsberg et al., 2015).
Substance use treatment, particularly AA/NA, was associated with higher level of STIs controlling for class of substance use indicating sustained risk of STIs after entering treatment or lack of attention to STIs in treatment settings. In light of these findings, it may be useful to improve sexual behavioral interventions and modify the way in which sexual health is addressed within the context of substance use treatment, certainly for women and MSM who had higher STI rates than MSW. This may likely include the integration of targeted repeated HIV and STI testing services and gender-specific interventions that address sexual risk reduction and sexual health in substance use treatment given the association between risk behaviors and substance use (Calsyn et al., 2009; Tross et al., 2008; Wechsberg et al., 2015).
4.1 Limitations
These results should be interpreted in light of several limitations. First, clinics were not randomly selected and findings may not be generalizable to all STI clinics in or outside the U.S. Second, we did not assess any pharyngeal STIs nor rectal infections in female participants. Third, risk remained after controlling for level of sexual risk indicating that at least part of the increased risk of STIs is due to elevated risk of substance users’ sexual networks; data are not available to explore this further. Fourth, we had relatively few WSW in the sample and confidence intervals for their risk levels are quite wide. Fifth, these are observational relationships as participants were not randomly assigned to substance use treatment. Finally, other studies have analyzed sexual orientation by three dimensions – identity, attraction, and behavior – and shown that risk for substance misuse is not uniform across all sexual minorities but instead varies based upon how sexual orientation is defined (McCabe et al., 2009; McCabe et al., 2013); we only have data on behavior.
4.2 Public Health Implications
Studies have shown that efforts to facilitate behavior change in STI clinics through risk reduction counseling, such as promoting use of protection and monogamy, are often limited and ineffective (Anderson et al., 2013; Erbelding et al., 2004; Lin et al., 2008; Proude et al., 2004). Many patients are returning with reoccurring STIs, indicating that there are likely underlying, unmet needs and comorbidities, often related to their gender, partner gender, and substance type, which must also be addressed through targeted screening and interventions to promote behavior change and limit STI incidence and reoccurrence (Erbelding et al., 2004; Newman et al., 2006; Senn et al., 2010). STI clinics are potentially important settings for identifying and treating patients with substance use issues when the context of each patient’s environment is considered (Scott-Sheldon et al., 2009). However, our data also indicate that specific attention to sexual health may be necessary to reduce STI risk during the substance use treatment course.
Substance use screening, referral and linkage for substance use treatment (Madras et al., 2009) may be useful in this setting in light of our finding that only 9.9% of our sample reported current or recent professional substance use treatment, despite high reported substance use. The data presented herein would be of use in planning this type of research and tailoring screening instruments to the client’s context. Of note, however, the ASPIRE randomized controlled trial showed that brief negotiated interviewing and motivational interviewing were not effective in reducing drug use among primary care patients identified by SBIRT programs (Saitz et al., 2014, see also Saitz, 2014 ). Therefore, further research is needed to evaluate more targeted SBIRT and targeted intervention approaches specific to this STI setting and these particularly vulnerable subpopulations where incidence of substance use and risk for STI acquisition is high (Gunn et al., 2000; Newman et al., 2006; Richert et al., 1993). Specifically, the beneficial impact of such prevention and treatment services on STI incidence rates and repeated STI diagnoses need to be assessed, in light of feasibility, cost-effectiveness, and lack of evidence supporting its effectiveness specific to this potentially resource-limited venue.
Supplementary Material
HIGHLIGHT.
We studied relationships between drug use and prevalent and incident sexually transmitted infections (STIs).
Substance use was related to STI rates and varied by gender and partner gender.
Participation in substance use treatment was associated with increased STI rates.
Focused interventions may be useful in STD clinics to reduce drug-related morbidity.
Gender-specific sexual health interventions may be useful in substance use treatment.
Acknowledgments
Role of Funding: This work was supported by the Office of the Director, National Institutes of Health (OD) (RC2DA028973), and the National Institute on Drug Abuse (R21DA038641 and R01DA027379). The infrastructure of the National Drug Abuse Treatment Clinical Trials Network was used as a platform in conducting the Project AWARE trial (U10DA13720). Support from the University of Miami Center for AIDS Research (CFAR) is also acknowledged (P30 AI073961). The NIH had no further role in study design, in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
None to report.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Conflict of Interest: None of the authors have declared any conflict of interest.
Contributors: Dr. Feaster conceptualized the study, analyzed the data and contributed to the overall writing and editing of the manuscript. He had full access to all data and participated in the design, execution, and analysis of the article. Dr. Parish contributed to the overall writing, editing and submission of the manuscript. Dr. Gooden, Dr. Matheson, Mr. Castellon, Mr. Duan, Mr. Pan, Ms. Haynes, Dr. Schackman, Dr. Malotte, Dr. Mandler, and Dr. Colfax all contributed to the editing of the manuscript. Dr. Metsch was a principal investigator for Project Aware (with Drs. Colfax and Feaster), conceptualized the study and contributed to the writing of the manuscript. All authors have reviewed and approved of the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Absalon J, Fuller CM, Ompad DC, Blaney S, Koblin B, Galea S, Vlahov D. Gender differences in sexual behaviors, sexual partnerships, and HIV among drug users in New York City. AIDS Behav. 2006;10:707–715. doi: 10.1007/s10461-006-9082-x. [DOI] [PubMed] [Google Scholar]
- Adams J, Moody J, Morris M. Sex, drugs, and race: how behaviors differentially contribute to the sexually transmitted infection risk network structure. Am J Public Health. 2013;103:322–329. doi: 10.2105/AJPH.2012.300908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C, Gallo MF, Hylton-Kong T, Steiner MJ, Hobbs MM, Macaluso M, Figueroa JP, Jamieson DJ, Legardy-Williams J, Wiener J, Warner L. Randomized controlled trial on the effectiveness of counseling messages for avoiding unprotected sexual intercourse during sexually transmitted infection and reproductive tract infection treatment among female sexually transmitted infection clinic patients. Sex Transm Dis. 2013;40:105–110. doi: 10.1097/OLQ.0b013e31827938a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandeen-Roche K, Miglioretti DL, Zeger SL, Rathouz PJ. Latent variable regression for multiple discrete outcomes. J Am Stat Assoc. 1997;92:1375–1386. [Google Scholar]
- Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belani H, Chorba T, Fletcher F, Hennessey K, Kroeger K, Lansky A, Leichter J, Mital S, Needle R, O'Connor K, Oeltmann J, Pevzner E, Purcell D, Sabin M, Semaan S, Sharapov U, Smith B, Vogt T, Wynn BA. Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. MMWR. 2012;61:1–43. [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Statist Soc Ser B. 1995:289–300. [Google Scholar]
- Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis - United States, 2012–2014. MMWR. 2015;64:1241–1245. doi: 10.15585/mmwr.mm6444a3. [DOI] [PubMed] [Google Scholar]
- Cachay E, Mar-Tang M, Mathews WC. Screening for potentially transmitting sexual risk behaviors, urethral sexually transmitted infection, and sildenafil use among males entering care for HIV infection. AIDS Patient Care STDS. 2004;18:349–354. doi: 10.1089/1087291041444050. [DOI] [PubMed] [Google Scholar]
- Calsyn DA, Hatch-Maillette M, Tross S, Doyle SR, Crits-Christoph P, Song YS, Harrer JM, Lalos G, Berns SB. Motivational and skills training HIV/sexually transmitted infection sexual risk reduction groups for men. J Subst Abuse Treat. 2009;37:138–150. doi: 10.1016/j.jsat.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Senn TE, Walsh JL, Scott-Sheldon LA, Carey MP. Alcohol use predicts number of sexual partners for female but not male STI clinic patients. AIDS Behav. 2016;20(Suppl 1):S52–59. doi: 10.1007/s10461-015-1177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh CE, Floyd LJ, Penniman TV, Hulbert A, Gaydos C, Latimer WW. Examining racial/ethnic disparities in sexually transmitted diseases among recent heroin-using and cocaine-using women. J Womens Health. 2011;20:197–205. doi: 10.1089/jwh.2010.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC Fact Sheet: Incidence, Prevalence and Cost of Sexually Transmitted Infections in the United States. CDC; Atlanta: 2013. [accessed on June 4, 2014]. http://www.cdc.gov/std/stats/STI-Estimates-Fact-Sheet-Feb-2013.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2012. CDC; Atlanta: 2014. [accessed on July 1, 2014]. http://www.cdc.gov/std/stats12/Surv2012.pdf. [Google Scholar]
- Cheng WS, Garfein RS, Semple SJ, Strathdee SA, Zians JK, Patterson TL. Increased drug use and STI risk with injection drug use among HIV-seronegative heterosexual methamphetamine users. J Psychoactive Drugs. 2010;42:11–18. doi: 10.1080/02791072.2010.10399781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction (Abingdon, England) 2004;99:989–998. doi: 10.1111/j.1360-0443.2004.00759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Guzman R. Club drugs and HIV infection: a review. Clin Infect Dis. 2006;42:1463–1469. doi: 10.1086/503259. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cook RL, Comer DM, Wiesenfeld HC, Chang CC, Tarter R, Lave JR, Clark DB. Alcohol and drug use and related disorders: An underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33:565–570. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- Decker MR, Miller E, McCauley HL, Tancredi DJ, Anderson H, Levenson RR, Silverman JG. Recent partner violence and sexual and drug-related STI/HIV risk among adolescent and young adult women attending family planning clinics. Sex Transm Infect. 2014;90:145–149. doi: 10.1136/sextrans-2013-051288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Arasteh K, McKnight C, Hagan H, Perlman DC, Semaan S. Associations between herpes simplex virus Type 2 and HCV With HIV among injecting drug users in New York City: the current importance of sexual transmission of HIV. Am J Public Health. 2011;101:1277–1283. doi: 10.2105/AJPH.2011.300130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziak JJ, Lanza ST, Tan X. Effect size, statistical power and sample size requirements for the bootstrap likelihood ratio test in latent class analysis. Struct Equ Modeling. 2014;21:534–552. doi: 10.1080/10705511.2014.919819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JM, Halpern CT, Wechsberg WM. Correlates of exchanging sex for drugs or money among women who use crack cocaine. AIDS Educ Prev. 2006;18:420–429. doi: 10.1521/aeap.2006.18.5.420. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Strathdee SA. Women who use or inject drugs: an action agenda for women-specific, multilevel, and combination hiv prevention and research. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S182–190. doi: 10.1097/QAI.0000000000000628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbelding EJ, Hutton HE, Zenilman JM, Hunt WP, Lyketsos CG. The prevalence of psychiatric disorders in sexually transmitted disease clinic patients and their association with sexually transmitted disease risk. Sex Transm Dis. 2004;31:8–12. doi: 10.1097/01.OLQ.0000105326.57324.6F. [DOI] [PubMed] [Google Scholar]
- Green AI, Halkitis PN. Crystal methamphetamine and sexual sociality in an urban gay subculture: an elective affinity. Cult Health Sex. 2006;8:317–333. doi: 10.1080/13691050600783320. [DOI] [PubMed] [Google Scholar]
- Gunn RA, Fitzgerald S, Aral SO. Sexually transmitted disease clinic clients at risk for subsequent gonorrhea and chlamydia infections: possible 'core' transmitters. Sex Transm Dis. 2000;27:343–349. doi: 10.1097/00007435-200007000-00008. [DOI] [PubMed] [Google Scholar]
- Harzke AJ, Williams ML, Bowen AM. Binge use of crack cocaine and sexual risk behaviors among African-American, HIV-positive users. AIDS Behav. 2009;13:1106–1118. doi: 10.1007/s10461-008-9450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings JM, Woods SE, Curriero FC. The spatial and temporal association of neighborhood drug markets and rates of sexually transmitted infections in an urban setting. Health Place. 2013;23:128–137. doi: 10.1016/j.healthplace.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopetz C, Pickover A, Magidson JF, Richards JM, Iwamoto D, Lejuez CW. Gender and social rejection as risk factors for engaging in risky sexual behavior among crack/cocaine users. Prev Sci. 2014;15:376–384. doi: 10.1007/s11121-013-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42:259–266. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis. 2002;29:476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Ames SL, Stacy AW. Alcohol, drugs, and condom use among drug offenders: an event-based analysis. Drug Alcohol Depend. 2008;93:38–42. doi: 10.1016/j.drugalcdep.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez C, Bornovalova MA, Daughters SB, Curtin JJ. Differences in impulsivity and sexual risk behavior among inner-city crack/cocaine users and heroin users. Drug Alcohol Depend. 2005;77:169–175. doi: 10.1016/j.drugalcdep.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Reynolds EK, Daughters SB, Curtin JJ. Risk factors in the relationship between gender and crack/cocaine. Exp Clin Psychopharmacol. 2007;15:165–175. doi: 10.1037/1064-1297.15.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li KH, Meng XL, Raghunathan TE, Rubin DB. Significance levels from repeated p-values with multiply-imputed data. Stat Sin. 1991;1:65–92. [Google Scholar]
- Lin JS, Whitlock E, O'Connor E, Bauer V. Behavioral counseling to prevent sexually transmitted infections: a systematic review for the U.S. Preventive Services Task Force. Ann Int Med. 2008;149:497–508. W496–499. doi: 10.7326/0003-4819-149-7-200810070-00011. [DOI] [PubMed] [Google Scholar]
- Logan TK, Leukefeld C, Farabee D. Sexual and drug use behaviors among women crack users: implications for prevention. AIDS Educ Prev. 1998;10:327–340. [PubMed] [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansergh G, Purcell DW, Stall R, McFarlane M, Semaan S, Valentine J, Valdiserri R. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121:127–132. doi: 10.1177/003335490612100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction. 2009;104:1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Hughes TL, Boyd CJ. Sexual orientation and substance abuse treatment utilization in the United States: results from a national survey. J Subst Abuse Treat. 2013;44:4–12. doi: 10.1016/j.jsat.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metsch LR, Feaster DJ, Gooden L, Schackman BR, Matheson T, Das M, Golden MR, Huffaker S, Haynes LF, Tross S, Malotte CK, Douaihy A, Korthuis PT, Duffus WA, Henn S, Bolan R, Philip SS, Castro JG, Castellon PC, McLaughlin G, Mandler RN, Branson B, Colfax GN. Effect of risk-reduction counseling with rapid HIV testing on risk of acquiring sexually transmitted infections: the AWARE randomized clinical trial. JAMA. 2013;310:1701–1710. doi: 10.1001/jama.2013.280034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Muthén & Muthén; Los Angeles, CA: 1998–2012. [Google Scholar]
- Newman LM, Warner L, Weinstock HS. Predicting subsequent infection in patients attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33:737–742. doi: 10.1097/01.olq.0000218865.37084.f6. [DOI] [PubMed] [Google Scholar]
- Nuttbrock L, Rosenblum A, Magura S, McQuistion HL, Joseph H. The association between cocaine use and HIV/STDs among soup kitchen attendees in New York City. J Acquir Immune Defic Syndr. 2000;25:86–91. doi: 10.1097/00042560-200009010-00012. [DOI] [PubMed] [Google Scholar]
- Owusu-Edusei K, Jr, Chesson HW, Gift TL, Tao G, Mahajan R, Ocfemia MC, Kent CK. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex Transm Dis. 2013;40:197–201. doi: 10.1097/OLQ.0b013e318285c6d2. [DOI] [PubMed] [Google Scholar]
- Pappas MK, Halkitis PN. Sexual risk taking and club drug use across three age cohorts of HIV-positive gay and bisexual men in New York City. AIDS Care. 2011;23:1410–1416. doi: 10.1080/09540121.2011.565027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton ME, Su JR, Nelson R, Weinstock H CDC. Primary and secondary syphilis--United States, 2005–2013. MMWR. 2014;63:402–406. [PMC free article] [PubMed] [Google Scholar]
- Proude EM, D'Este C, Ward JE. Randomized trial in family practice of a brief intervention to reduce STI risk in young adults. Fam Pract. 2004;21:537–544. doi: 10.1093/fampra/cmh510. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Moss S, Remien RH, Woods WJ, Parsons JT. Illicit substance use, sexual risk, and HIV-positive gay and bisexual men: differences by serostatus of casual partners. AIDS. 2005;19(Suppl 1):S37–47. doi: 10.1097/01.aids.0000167350.00503.db. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Washton A, Domier CP, Reiber C. Drugs and sexual effects: role of drug type and gender. J Subst Abuse Treat. 2002;22:103–108. doi: 10.1016/s0740-5472(01)00215-x. [DOI] [PubMed] [Google Scholar]
- Richert CA, Peterman TA, Zaidi AA, Ransom RL, Wroten JE, Witte JJ. A method for identifying persons at high risk for sexually transmitted infections: opportunity for targeting intervention. Am J Public Health. 1993;83:520–524. doi: 10.2105/ajph.83.4.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross MW, Hwang L, Zack C, Bull L, Williams ML. Sexual risk behaviours and STIs in drug abuse treatment populations whose drug of choice is crack cocaine. Int J STD AIDS. 2002;13:769–774. doi: 10.1258/095646202320753736. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons; New York: 1987. [Google Scholar]
- Saitz R. Screening and brief intervention for unhealth drug use: little or no efficacy. Front Psychiatry. 2014;5:121. doi: 10.3389/fpsyt.2014.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Meli SM, Chaisson CE, Samet JH. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312:502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, Su J, Xu F, Weinstock H. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40:187–193. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, Friedman S. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. Am J Public Health. 2013;103:e28–e36. doi: 10.2105/AJPH.2012.301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Scott-Sheldon LA, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Alcohol consumption, drug use, and condom use among STD clinic patients. J Stud Alcohol Drugs. 2009;70:762–770. doi: 10.15288/jsad.2009.70.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Strathdee SA, Zians J, Patterson TL. Correlates of trading sex for methamphetamine in a sample of HIV-negative heterosexual methamphetamine users. J Psychoactive Drugs. 2011;43:79–88. doi: 10.1080/02791072.2011.587390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. The intersection of violence, substance use, depression, and STDs: testing of a syndemic pattern among patients attending an urban STD clinic. J Natl Med Assoc. 2010;102:614–620. doi: 10.1016/s0027-9684(15)30639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban M. Sexual partner concurrency among STI clinic patients with a steady partner: correlates and associations with condom use. Sex Transm Infect. 2009;85:343–347. doi: 10.1136/sti.2009.035758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Top HIV Med. 2006;14:84–87. [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ. Methamphetamine use and infectious disease-related behaviors in men who have sex with men: implications for interventions. Addiction. 2007;102(Suppl 1):130–135. doi: 10.1111/j.1360-0443.2006.01775.x. [DOI] [PubMed] [Google Scholar]
- Stahlman S, Javanbakht M, Stirland A, Guerry S, Gorbach PM. Methamphetamine use among women attending sexually transmitted disease clinics in Los Angeles County. Sex Transm Dis. 2013;40:632–638. doi: 10.1097/01.OLQ.0000430801.14841.75. [DOI] [PubMed] [Google Scholar]
- Substance Abuse Mental Health Services Administration. [accessed on June 20, 2015];Results from the 2013 National Survey on Drug Use and Health: Detailed Tables. 2014 http://www.samhsa.gov/data/population-data-nsduh/reports.
- Theodore PS, Duran RE, Antoni MH. Drug use and sexual risk among gay and bisexual men who frequent party venues. AIDS Behav. 2014;18:2178–2186. doi: 10.1007/s10461-014-0779-y. [DOI] [PubMed] [Google Scholar]
- Thiede H, Jenkins RA, Carey JW, Hutcheson R, Thomas KK, Stall RD, White E, Allen I, Mejia R, Golden MR. Determinants of recent HIV infection among Seattle-area men who have sex with men. Am J Public Health. 2009;99(Suppl 1):S157–164. doi: 10.2105/AJPH.2006.098582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, German D, Spikes P, Patterson J, Latkin C. A comparison of the social and sexual networks of crack-using and non-crack using African American men who have sex with men. J Urban Health. 2011;88:1052–1062. doi: 10.1007/s11524-011-9611-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tross S, Campbell AN, Cohen LR, Calsyn D, Pavlicova M, Miele GM, Hu MC, Haynes L, Nugent N, Gan W, Hatch-Maillette M, Mandler R, McLaughlin P, El-Bassel N, Crits-Christoph P, Nunes EV. Effectiveness of HIV/STD sexual risk reduction groups for women in substance abuse treatment programs: results of NIDA Clinical Trials Network Trial. J Acquir Immune Defic Syndr. 2008;48:581–589. doi: 10.1097/QAI.0b013e31817efb6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Wang C, Brown CH, Bandeen-Roche K. Residual diagnostics for growth mixture models: Examining the impact of a preventive intervention on multiple trajectories of aggressive behavior. J Am Stat Assoc. 2005;100:1054–1076. [Google Scholar]
- Wechsberg WM, Deren S, Myers B, Kirtadze I, Zule WA, Howard B, El-Bassel N. Gender-specific HIV prevention interventions for women who use alcohol and other drugs: the evolution of the science and future directions. J Acquir Immune Defic Syndr. 2015;69:S128–139. doi: 10.1097/QAI.0000000000000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohl AR, Frye DM, Johnson DF. Demographic characteristics and sexual behaviors associated with methamphetamine use among MSM and non-MSM diagnosed with AIDS in Los Angeles County. AIDS Behav. 2008;12:705–712. doi: 10.1007/s10461-007-9315-7. [DOI] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. J Subst Abuse Treat. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Zuckerman MD, Boyer EW. HIV and club drugs in emerging adulthood. Curr Opin Pediatr. 2012;24:219–224. doi: 10.1097/MOP.0b013e32834faa9b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.