Abstract
Background
Historically, smoking cessation was thought to negatively impact substance use outcomes among smokers who use other substances. We sought to synthesize recent reports on this association.
Methods
Google Scholar, PubMed, and Cinahl were searched for studies published from 2006 to March 29, 2016 that reported impact of smoking cessation treatment or quitting smoking on substance use or substance use disorder treatment outcomes in the general population and among those in substance abuse treatment. Studies were grouped by reported impact as follows: “positive” (i.e. improved), “null” (i.e. no change), or “negative” (i.e. worsened).
Results
Twenty-four studies were included. Eighteen reported the impact of quitting smoking and six reported the impact of smoking cessation treatment intervention, independent of quitting, on substance use outcomes. Eleven studies (46%) reported solely positive impact; four (17%) reported solely null impact; eight (33%) reported mixed positive and null impact by analysis (combined and subgroup, n = 1); substance (n = 4); length of follow-up (n = 2); and comparison group (n = 1). One study (4%) reported mixed negative and null impact by ethnic group. No studies reported increased substance use.
Conclusion
Smoking cessation does not appear to have a negative effect, and often has a positive effect on substance use outcomes. Smoking cessation advice should be offered, without hesitation, to smokers who report substance use and those in treatment for substance use disorder.
Keywords: smoking cessation, smoking cessation treatment, substance use, substance use disorder, substance use treatment
1. Introduction
Smoking rates are two to four times higher among adolescents and adults with substance use disorders (SUD) compared to the general population.1–3 Still, smoking cessation treatment is not included in most SUD treatment settings4,5 and there is a dearth of reporting on the impact of quitting smoking on substance use behaviors in non-treatment seeking populations. Smoking has had a steady, long-term relationship with both clinicians and patients in substance use and mental health treatment settings, making these settings less receptive to smoking cessation treatment and less supportive of quitting than providers in general medical facilities or the community.6,7 Historically, smoking was allowed and even encouraged in addiction treatment programs and in mental health units, the pervasive rationale being that tobacco was a lower treatment priority and/or a less harmful alternative to other substance use.5,8,9 Arguments proffered by treatment providers included if their patients quit tobacco they would relapse on other substances of abuse, their depression would recur and/or they would otherwise decompensate.10 Meanwhile, just below the surface, the tobacco industry was marketing cigarettes to persons with mental illness and providing tax-free cigarettes to treatment facilities11 where cigarettes were provided to patients, facilitating smoking initiation, while hospitalized, for some formerly nonsmoking patients.12,13 Finally, many staff and clinicians in the fields of drug abuse treatment and mental health are smokers, which serves to both perpetuate the habit and stem implementation of smoking cessation programs and smoke free policies in these settings.14–17
Many adults and adolescents attend 12-step fellowship meetings such as Alcoholics Anonymous or Narcotics Anonymous to achieve abstinence or as a form of relapse prevention upon completion of formal SUD treatment.18,19 The 12-step philosophy, which teaches that the first and primary responsibility is sobriety from alcohol, illegal drugs, and non-prescription medications,20–22 can further perpetuate continued smoking by recommending members focus and not make too many additional changes (i.e. quitting smoking).21–23 Meetings often allow or encourage smoking as a form of “fellowshipping” to enhance recovery, thereby helping to maintain smoking and nicotine dependence among individuals who report use of other substances.24,25
Evidence is mounting that the harms of tobacco use far outweigh any perceived benefit in the context of substance use or SUD treatment. For example, adolescent substance users who smoke are more likely to continue smoking in adulthood26 and far more deaths among adults reporting alcohol and drug use are due to smoking than to alcohol and all other drugs combined.27 In 2004, a meta-analysis of smoking cessation intervention studies conducted among individuals in SUD treatment or recovery found that cessation interventions offered concurrently with addictions treatment were associated with a 25% increased likelihood of long-term drug and alcohol abstinence.28 Thus, fears associated with smoking cessation among people with SUD may be unwarranted.
Studies have increasingly addressed smoking cessation in the context of SUD treatment over the last decade. Strategies for promoting smoking cessation have included delivering cessation programs to individuals in SUD treatment and implementing and enforcing smoking bans in adult and adolescent treatment facilities.29–31 In 2010, two literature reviews summarized the evidence on the effects of smoking cessation in the context of SUD treatment: one among those in treatment for or in early remission from alcohol dependence32; and one in addiction and mental health treatment settings.10 Both studies found improved rather than worsened substance use treatment outcomes related to smoking cessation intervention. In 2015, a systematic review of randomized controlled trials that included impact of smoking cessation treatment on substance use outcomes among those in early recovery from or in treatment for SUD reported either no impact on or improvement in substance use treatment outcomes.33 With limited extant research, no reviews among adolescent populations were identified. One study (2007) conducted in adolescent residential substance use treatment programs assessed the relationship between program-level policies and client-level smoking, and showed increases in stringency of smoke-free policy were associated with decreases in smoking prevalence.34 These findings suggest addressing tobacco use in the context of addiction treatment and recovery may afford patients multiple health benefits now and in the future.
Here, we provide an updated review and interpretation of the most current knowledge by reviewing reports from the last decade (January 2006 through March 2016) on the impact of formalized smoking cessation treatment or of quitting smoking/former smoker status on substance use outcomes. By synthesizing recent findings and including studies with adolescents, reports from epidemiological studies, and results from pilot studies and secondary analyses, we fill important gaps in the extant literature. Whereas reports from 201032 and 201533 have addressed solely formal smoking cessation treatment interventions among those in treatment for or recovery from substance use (including alcohol) this report includes findings among non-SUD treatment seeking populations including reports published from 2015 through March, 2016 as well. This allows for a broader, more inclusive view of the overarching impact of smoking cessation and quitting smoking on substance use outcomes.
2. Methods
Articles published in print or online between January 1, 2006 and March 29, 2016 were identified through electronic searches of Google Scholar, PubMed, and Cinahl. Google Scholar was chosen for breadth and as a more novel search tool; PubMed as a standard search engine; and Cinahl for its inclusion of peer-reviewed nursing and nursing practice journals not easily identified elsewhere. Search criteria combined the terms “smoking” “cessation” “substance” “drug,” and “alcohol.” Study title, abstracts, and bodies were reviewed by KM and JT to determine study inclusion. Selection was restricted to English language studies that: (a) established temporality (i.e. cross sectional studies were excluded), (b) listed at least one outcome related to substance use, SUD, or SUD treatment, and (c) identified quitting smoking (“former smoker status”) or a smoking cessation treatment intervention as an independent variable. To avoid duplicative reporting and in light of the similarity in conclusions drawn by the three reviews conducted over the past decade10,32,33 the reviews and the studies included within were omitted.
Titles of the first 100 citations in Google Scholar were scanned and 35 unique and potentially relevant citations were identified. Google Scholar has been found to have recall and precision comparable or superior to more traditional databases when the first 100 citations are considered (over 84,000 citations were identified in the instant search).35 PubMed and Cinahl were then searched using the same search terms and resulted in 50 unique citations (35 and 15, respectively). No additional studies were identified through bibliographic searches. The 85 articles identified were read by JT and KM to ascertain if they met inclusion criteria and 24 studies were included in the review.
As the 24 selected studies showed considerable heterogeneity in terms of measurement of smoking cessation intervention or quit status, outcome variables, and analyses, it was not feasible to conduct a meta-analysis focused on effect size.36 In accordance with the “principle of best evidence,”37 we did not discard studies without the information necessary for formal quantification since they still provide valuable and relevant evidence. We then appraised each study for overall impact on substance use outcomes as positive, null, mixed, or negative. Within each study, impact was assessed for each reported substance use outcome. Overall impact was deemed “positive” if only improvements were reported on all substance-related outcomes assessed (e.g. increased length of time to relapse, decreased number of days using drugs). “Null” impact was assigned if no change in any substance use outcomes was reported. A “negative” impact was assigned if worse substance use outcomes were found (e.g. shorter term of abstinence). A “mixed” impact was assigned if there were differences in the direction of individual outcomes within a study.
3. Results
Twenty-four studies (25 study populations as one study [Lisha, et al., 2014] included two samples) reported the impact of quitting smoking (n = 18) or of smoking cessation treatment intervention, independent of quitting smoking, (n = 6) on substance use outcomes (Table 1). Fourteen studies were among SUD treatment samples (five among adolescents); two in household survey samples, one in a school-based survey sample (among adolescents); four among samples seeking smoking cessation treatment; and one each of high-needs population samples: HIV positive patients, homeless smokers, and smokers in mental health outpatient and inpatient (adolescent) treatment (Figure 1).
Table 1.
Studies examining the effect of tobacco cessation or quitting smoking on substance use outcomes (N=24)
| Authors (Year) | Study Design | Sample Description* | Smoking Variable Assessed | SU Outcome of Interest | Cessation/Treatment | Synopsis of Findings | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Positive Impact | ||||||||||
| 1. | Berg, Piper, Smith, Fiore, Jorenby (2015) | Secondary analysis of RCT, bupropion, NRT, counseling | N=1,301, mean age 45, 59% female, 84% white, 48% history alcohol abuse, 10% history of alcohol dependence, smokers | N/A, investigated changes pre and post target quit date | Mean number of drinks per day 2 weeks pre and post target quit date | Smoking Cessation |
Positive Generally, alcohol use decreased post-target quit date. Smokers who reported less pre-quit alcohol use, as well as smokers who were female, non-white, and had a history of alcohol dependence tended to use less alcohol post-quit |
|||
| 2. | Magee, Winhusen (2015) | Secondary analysis of multisite RCT, SUD treatment with or without smoking cessation treatment, counseling, bupropion, contingency management | N=538, mean age 36, 48% female, adults with cocaine or methamphetamine SUD | N/A, investigated impact of smoking cessation intervention | Stimulant craving | Smoking Cessation |
Positive Smoking cessation eliminated coupling between nicotine craving and stimulant craving, γ = −.07, p = .39. Conclusions: Contrary to concerns about nicotine abstinence during substance dependence treatment, increases in nicotine craving may be associated with later reductions in stimulant craving and use |
|||
| 3. | Cavazos-Rehg, Breslau, Hatsukami, Krauss, Spitznagel, Grucza, Salyer, Hartz, Bierut (2014) | Prospective cohort, NESARC | N=4,853, adults, 48% female, 77% white | Usual number of cigarettes per day, self-report | Past year diagnosis DSM-IV alcohol use disorder or drug use disorder | Smoking Cessation |
Positive Among daily smokers who had current or lifetime history diagnosis of the outcome of interest at Wave 1, quitting by Wave 2 predicted a decreased risk of mood/anxiety disorder (aOR 0.6, 95% CI 0.4, 0.9) and alcohol disorder (aOR 0.7, 95% CI 0.5, 0.99) at Wave 2. Among daily smokers with no lifetime history diagnosis of the outcome of interest at Wave 1, quitting smoking by Wave 2 predicted a decreased risk of drug use disorder at Wave 2 aOR 0.3, 95% CI 0.1, 0.9). |
|||
| 4. | Dawson, Goldstein, Grant (2013) | Prospective cohort | N=14,885, adult past-year ≥ monthly drinkers | Smokers at baseline but not during year preceding follow-up, self-report | One year alcohol abstinence | Smoking Cessation |
Positive Smoking cessation associated with drinking cessation over follow-up, OR=2.82 (95% CI=1.62–4.92) to 3.45 (2.20–5.39) |
|||
| 5. | Piper, Rodock, Cook, Schlam, Fiore, Baker (2013). | RCT, bupropion, NRT, counseling | N=1,470, mean age 45, 58% female, 84% white, smokers | 7-day point prevalence abstinence, biochemically verified (breath CO) | Past year SUD diagnosis | Smoking Cessation |
Positive Participants who were smoking at the Year 3 follow-up were more likely to have developed and maintained a substance use or major depressive disorder by that time than were individuals who were abstinent at Year 3 |
|||
| 6. | Metrik, Spillane, Leventhal, Kahler (2011) | RCT, counseling, NRT, brief alcohol intervention | N=216, mean age 42, 45% female, 91% white, heavy drinkers seeking smoking cessation treatment | N/A, investigated impact of smoking cessation intervention | Number of drinks/week, percent of marijuana use days | Smoking Cessation Treatment Intervention |
Positive All participants made large reductions in weekly alcohol consumption during the trial, with weekly marijuana users also reducing their marijuana use. Frequent marijuana smokers may benefit from smoking cessation even when not explicitly discussed |
|||
| 7. | Tsoh, Chi, Mertens, Weisner (2011) | Retrospective cohort/chart review | N=1,951, adults, 39% female, 75% white, Kaiser patients from 1994–98 | Current cigarette smoking, self-report | 1 year alcohol or drug abstinence at 5, 7, and 9 years; past-year remission SUD | Smoking Cessation |
Positive Stopping smoking during the first year after substance use treatment intake predicted better long-term substance use outcomes through 9 years after intake |
|||
| 8. | Brown, Strong, Abrantes, Myers, Ramsey, Kahler (2009) | RCT, motivational interviewing, brief advice | N=191, adolescents mean age 15, 62% female, 95% white, mental hospital inpatients | N/A, investigated impact of smoking cessation intervention | Percentage of days with substance use (alcohol and illicit drugs) | Smoking Cessation Treatment Intervention |
Positive The results of this study suggest that MI for smoking cessation had a significant effect in preventing an increase in substance use during the first 6 months following hospitalization |
|||
| 9. | de Dios, Vaughan, Stanton, Niaura (2009) | Multi-site prospective cohort | N=1,779, adolescents mean age 16, 30% female, 57% white, in SUD treatment | Current cigarette smoking, self-report | Relapse to alcohol and marijuana; time to relapse to alcohol and marijuana | Smoking Cessation |
Positive Persistent smokers and smoking initiators had significantly greater odds of alcohol and marijuana relapse and shorter periods to marijuana relapse at follow-up compared with quitters |
|||
| 10. | Myers, Doran, Brown (2007) | Prospective cohort, secondary analysis | N=123, adolescents, mean age 16, 41% female, 81% white, in SUD treatment | Smoking abstinence for > 1 year, self-report | Alcohol use trajectory (abstainers, infrequent drinkers, worse over time, frequent drinkers) | Smoking Cessation |
Positive Larger proportion of quitters (v. persistent smokers) were alcohol abstainers compared to frequent drinkers |
|||
| 11. | Satre, Kohn, Weisner (2007) | Prospective cohort | N=598, smokers: n=315, mean age 36, 44% female, 76% white, non-smokers: n=283, mean age 40, 42% female, 71% white, Kaiser, CA, admitted 1997–1998, health plan members | Current cigarette smoking, self-report | Addiction Severity Index scores, 30 day abstinence from alcohol and drugs | Smoking Cessation |
Positive Smokers were less likely to be abstinent from alcohol and drugs in the prior 30 days (48.3% vs. 64.0%), and had higher Addiction Severity Index scores |
|||
| Null Impact | ||||||||||
| 12. | Alessi and Petry (2014) | RCT, frequent monitoring and behavioral support or that plus contingency management | N=45 – behavioral support: N=21, 100% male, mean age 37, 43% Black, 48% European American; contingency management: N=24, 100% male, mean age 38, 17% Black, 79% European American | Percent of days CO-negative (biochemically validated) | Study attendance, study adherence, days of self-reported drug use (biochemically validated) | Smoking Cessation Treatment Intervention |
Null No study withdrawals, no difference by treatment arm for adherence, days of self-reported substance use, or drug-positive urine tests. |
|||
| 13. | Kahler, Borland, Hyland, McKee, O’Connor, Fong, Cummings (2010) | Prospective cohort | N=3,614, mean age 42, 47% female, 95.8%, adult daily smokers from AU, CA, UK, US | Smoking abstinence for > 6 months, self-report | Drinking frequency, number of drinks per day and heavy or “binge” drinking frequency | Smoking Cessation |
Null No difference in reduction in drinking by quitters compared to non-quitters |
|||
| 14. | Callaghan, Brewster, Johnson, Taylor, Beach, Lentz (2007) | Retrospective cohort, NRT available on request | N=520, adolescents mean age 17, 57% female, 39% Aboriginal ancestry, in SUD treatment | N/A, investigated impact of smoking ban at SUD treatment facility | SUD treatment enrollment and treatment completion | Smoking Cessation |
Null The total smoking ban was not associated with a lower proportion of adolescent smokers seeking treatment or a lower treatment completion rate among smokers compared to nonsmokers |
|||
| 15. | Rohsenow, Tidey, Martin, Colby, Sirota, Swift, Monti (2015) | RCT, contingent vouchers, motivational interviewing, brief advice | N=184, mean age 35, 55% female, 83% white, smokers in SUD treatment | N/A, investigated impact of smoking cessation intervention | Number of heavy drinking days and biochemically verified number of drug use days at each follow up and relapse at 1 year | Smoking Cessation Treatment Intervention |
Null No differential effects on drug use |
|||
| Mixed Impact (positive and null) | ||||||||||
| 16. | Lisha, Carmody, Humfleet, Delucchi (2014) | Secondary analysis of 2 RCTs, smoking cessation interventions, NRT, counseling, estimated both synchronous (within day) and lagged (across day) forecasts between smoking and alcohol use | N=302, mean age 48, 9% female, 50% white, adults with HIV & adults in alcohol use disorder treatment | Number of cigarettes, timeline follow-back, 7-day point prevalence abstinence, biochemically verified (breath CO) | Alcohol use number of drinks | Smoking Cessation |
Positive & null by subgroup/Null overall In the overall sample, there was no difference in alcohol use between those who stopped smoking (even for one day) and those who never stopped (t(300) = 0.08, p = .93). When broken up by study there was a significant reduction in the alcohol dependent sample: t(137) = 2.88, p < .0001. The mean number of drinks was 29.76 (SD = 90.9) for those who stopped v. 131.7 (SD = 324.5) for those who did not. |
|||
| 17. | Reitzel, Nguyen, Eischen, Thomas, Okuyemi (2014) | Secondary analysis of RCT, NRT, self-help guide, counseling | N=427, mean age 44, 25% female, 35% white, homeless adult daily smokers interested in quitting smoking | 7-day point prevalence abstinence, biochemically verified (breath CO) | Number of drinking days of 30; drinks per drinking day; number of heavy drinking days; number of days cocaine or mj/hash or heroin and any drug | Smoking Cessation |
Positive (alcohol)/Null (drugs) Smoking abstinence (CO-verified) was associated with fewer drinking days (P = 0.03), fewer drinks consumed on drinking days (P = 0.01), and lower odds of heavy drinking (P = 0.05), but not with differences in the number of days of cocaine, marijuana/hashish, heroin or any drug use |
|||
| 18. | Winhusen, Kropp, Theobald, Lewis (2014) | Secondary analysis of multisite RCT, SUD treatment with or without smoking cessation treatment, counseling, bupropion, contingency management | N=249, baseline demographics reported by follow-up smoking status, continued smoking: N=174, mean age 38, 49% female, 61% white, smoking abstinent: N=75, mean age 36, 37% female, 55% white, adults with cocaine or methamphetamine SUD | 7-day point prevalence abstinence, biochemically verified (breath CO) | Stimulant abstinence (biochemically verified) | Smoking Cessation |
Positive (cocaine)/Null (methamphetamines) A significant effect was found for the cocaine-dependent subsample (N=147) in which participants who stopped smoking were abstinent for illicit stimulants an average of 78.2% of the post-smoking-quit weeks (weeks 4–10) relative to 63.6% in participants who continued smoking (χ2(1)=8.55, p<.01, d=0.36). No significant effects were found for the sample as a whole (N=249) or for the methamphetamine-dependent subsample (N=102). |
|||
| 19. | Stahre, Toomey, Erickson, Forster, Okuyemi, Ahluwalia (2013) | RCT, counseling | N=755, mean age 45, 67% female, African American adults | 7-day point prevalence abstinence, self-report | Prevalence and frequency of past 30-day binge drinking and average daily alcohol consumption | Smoking Cessation |
Positive (short term)/Null (long term) Individuals who quit smoking within the first 8 weeks of the study reported lower past 30-day binge drinking prevalence at week 8 than those who did not quit during the first 8 weeks (P = .035), but the effect was not sustained at the end of the study (week 26) |
|||
| 20. | Campbell, Chi, Sterling, Kohn, Weisner (2009) | Prospective cohort | N=419, adolescents mean age 16, 34% female, 49% white, recruited when entering SUD treatment | Abstinence for previous 6 or 12 months, self-report | SU self-report follow-up data validated on subsample at 12 months w/urinalysis, abstinence from drugs and alcohol | Smoking Cessation |
Positive (drugs)/Null (alcohol) Self-initiated tobacco cessation at 6 months, and at both 6 and 12 months, were related to higher odds of drug abstinence but not alcohol abstinence |
|||
| 21. | Myers, Prochaska (2008) | RCT, group counseling | N=54, adolescents mean age 16, 22% female, 69% white, outpatient SUD treatment in Southern California | N/A, investigated impact of smoking cessation intervention | Total days of substance use at the 3-and 6-month follow up time points | Smoking Cessation Treatment Intervention |
Positive (short term)/Null (long term) Participants who received smoking cessation intervention had significantly fewer days of substance use than controls at the 3-months, but not at 6-months follow-up |
|||
| 22. | Prochaska, Hall, Tsoh, Eisendrath, Rossi, Redding, Rosen, Meisner, Humfleet, Gorecki (2008) | RCT, smoking cessation intervention, computer-based intervention, counseling | N=322, depressed smokers in mental health outpatient treatment | 7-day point prevalence abstinence, biochemically verified (breath CO) | Alcohol, mj, stimulant, opiate use (y/n) between follow-ups |
Positive (alcohol)/Null (drugs) Participants who successfully stopped smoking reported less alcohol use than did participants who continued smoking. No difference in drug use |
||||
| 23. | Brook, Balka, Ning, Brook (2007) | Prospective cohort | N=473, adolescents mean age 14, 51% female, 51% black, 49% Puerto Rican | Current cigarette smoking, self-report | Alcohol dependence, illicit drug dependence, alcohol and illicit drug dependence | Smoking Cessation |
Positive (quitters v. early starters & continuous) Null (quitters v. late starters) Early starting continuous smokers more likely than quitters report alcohol dependence (OR 3.72) and illicit drug dependence (3.21). There was no difference between late-starting smokers and quitters |
|||
| Mixed Impact (negative and null) | ||||||||||
| 24. | Fu, Kodl, Willenbring, Nelson, Nugent, Gravely, Joseph (2008) | Secondary analysis of RCT, smoking cessation intervention, NRT, counseling (concurrent or delayed smoking cessation treatment) | N=459, mean age 40, 30% female, 83% white, adults in alcohol use disorder treatment | 7-day point prevalence abstinence, self-report (25% subsample biochemically verified) | 6-months alcohol abstinence @ 6, 12, 18 months; time to first alcohol use; black/white differences | Smoking Cessation Treatment Intervention | For whites: alcohol abstinence outcomes were consistently worse in concurrent group than delayed group, but not for blacks | |||
Figure 1.
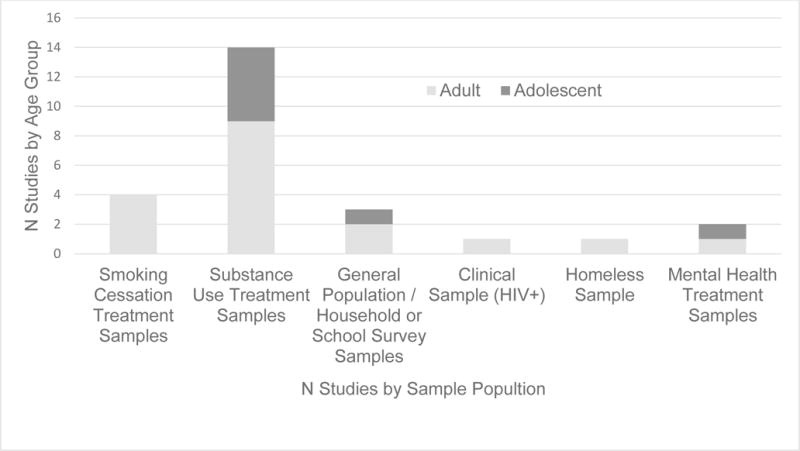
Overview of included studies by sample populations and age group (N=24*)
*Chart adds to 25 study sample populations as one study included two samples (Lisha et al., 2014)
3.1 Positive Findings
Eleven of 24 studies (46%) reported positive findings regarding the impact of quitting smoking (n=9)38–46 and of smoking cessation treatment interventions (n=2)29,47 on substance use outcomes. Of these, five were among patients in SUD treatment-42–46 of which two targeted adolescents,43,44 four were among participants delivered smoking cessation interventions,29,38,41,47 of which one study targeted adolescents during psychiatric hospitalization,29 and two were among adult general population samples.39,40 (Figure 2)
Figure 2.
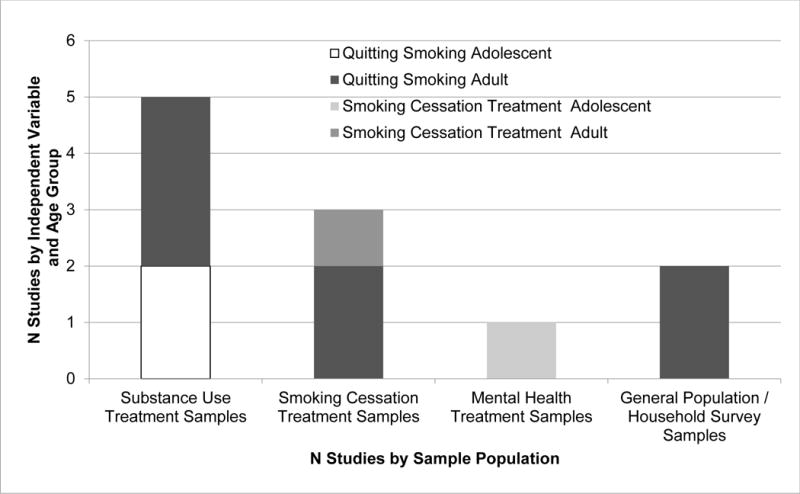
Positive findings by sample population, independent variable (Quitting smoking or Smoking cessation treatment intervention), and age group (n=11)
Of the 11 studies with positive findings, eight (73%) found improved alcohol-specific outcomes of fewer drinks per day,38 fewer drinks per week,47 decreased likelihood of relapse,43 increased abstinence for 12 months40,42 and for 30 days,45 increased likelihood of “alcohol-abstainer” trajectory membership,44 and decreased likelihood of being diagnosed with alcohol use disorder.39 Five studies (45%) reported drug-specific outcomes or general “drug” outcomes that excluded alcohol; one found increased likelihood of past year abstinence from drugs,42 one found decreased likelihood of being diagnosed with a drug use disorder,39 two found improved marijuana-specific outcomes of reduced percent of using days47 and decreased likelihood of relapse and longer time to relapse43 and one found reduced stimulant craving.46 Finally, among studies that reported improved combined (e.g. alcohol and other drugs) substance use outcomes (n = 4; 36%), findings of decreased likelihood of SUD diagnosis,41 past-year remission,42 decreased escalation of use post-treatment,29 and increased likelihood of past 30-day abstinence and lower addiction severity index (ASI) scores45 were found.
3.2 Null Findings
Four studies (17%) reported an overall null impact on substance use outcomes. Study designs varied (pro- and retrospective cohort studies and RCT) as did outcomes: drinking and drug use behavior, treatment enrollment and completion, study attendance and adherence. Sample populations also varied widely: general population adults, and adolescents, adults in SUD treatment, adolescents in SUD treatment., and adults seeking smoking cessation treatment. The studies investigated quitting smoking as well as effects of different smoking cessation interventions (implementation of a smoking ban, contingent vs. non-contingent vouchers crossed with motivational interviewing or brief advice, contingency management vs. behavioral support).
One study reported no change in the alcohol-specific outcomes of binge- and overall drinking frequency.48 Another found no difference in SUD treatment enrollment or completion.30 The third study showed no difference in reported number of heavy drinking days, number of drug use days, and instances of reported relapse.49 The fourth study found no differences in study attendance and adherence and no difference in reported and verified substance use abstinence.50 Given the sample sizes of 45 (Alessi & Petry, 2014), 54 (Myers & Prochaska, 2004), and 184 (Rohsenow, et al., 2015), it is possible (but not likely) that the null findings were due to small sample sizes and thus low power to detect an effect.
3.3 Mixed Findings
Nine studies (38%) reported mixed findings: eight studies (89%) reported mixed positive and null impact by analysis (combined and subgroup, n = 1)51; type of substance (n = 4)11,52–54; length of follow-up (n = 2)55,56; and comparison group (n = 1).57 Six studies11,51–54,57 addressed quitting smoking and three were smoking cessation treatment interventions.55,56,58 Five were among SUD treatment seeking samples,51,53,54,56,58 three were among adolescents,54,56,57 two in general population samples,55,57 one among a smoking-cessation treatment-seeking (but not SUD treatment seeking) sample, and three among high-needs populations (an HIV clinic sample (of HIV+ patients), a homeless smokers sample, and a sample of smokers in mental health outpatient treatment). While all nine reported at least one substance use outcome that was not impacted, eight reported at least one substance use outcome that was positively impacted11,51–57 and only one reported a negatively impacted substance use outcome.58
Considering substance use outcomes, six reported alcohol-specific outcomes (either alone or in combination with other substance use outcomes), three of which had findings both positive and null for the same alcohol-specific outcomes, two had findings of positive impact, and one reported no impact. Both positive and no impact was reported regarding number of drinks,51 prevalence of binge drinking,55 and odds of reporting alcohol (or illicit drug) dependence.57 The direction of these findings depended on the group analyzed, length of follow-up, and comparison group, in that order. Two studies reported impacts resulting solely in positive alcohol-related outcomes of decreased use11 and decreased number of drinks and drinking days as well as lower odds of heavy drinking.52 These same studies, however, found no impact on drug use or number of days using drugs, respectively. One study reported no impact on odds of reporting alcohol abstinence and positive impact/increased odds of reporting abstinence from drugs.54
Only one study did not separate alcohol from other drug outcomes and instead reported on “substance use” outcomes.56 Here, the positive impact of decreased number of substance use days at 3 months follow-up was not found at 6 months (no impact). There was also a single study that reported higher average percent of abstinent weeks among cocaine dependent (positive impact), but not methamphetamine dependent (no impact), individuals.53 Finally, one study reported decreased alcohol abstinence (negative impact) for Caucasian participants who received smoking cessation treatment concurrent with alcohol use treatment compared to those who received smoking cessation treatment 6 months after alcohol use treatment, the same was not true for African American participants (no impact).58
4. Discussion
We reviewed the published evidence from the last decade reporting the impact of quitting smoking and/or smoking cessation treatment intervention on substance use outcomes. Across 24 studies, both quitting smoking and smoking cessation treatment intervention had either a positive impact or no impact on substance use outcomes. Positive impact was reported for a range of alcohol use outcomes (e.g., number of drinks, alcohol abstinence, and alcohol use disorder diagnosis) as well as drug use outcomes (e.g., using days, relapse, remission, SUD diagnosis). Importantly, for those in SUD treatment, neither forced quit attempt (smoke-free policy) nor smoking cessation treatment intervention type (e.g. brief advice to quit, motivational interviewing, and offering vs. not offering nicotine replacement) affected treatment outcomes. Results support the broad delivery of smoking cessation intervention in accordance with clinical practice guidelines59 (offering advice to quit, using medications, and enrollment in smoking cessation counseling) to any individual that reports alcohol or other drug use (whether recreational, disordered, or otherwise). Further, if patients are able to quit smoking, it may make it easier for them to change other substance use for a variety of reasons.
Only one study reported a negative impact of smoking cessation on a substance use outcome.58 A secondary analysis of data from a 2004 study by Joseph and colleagues60 found smoking cessation treatment delayed by 6 months was associated with longer alcohol abstinence than smoking cessation treatment implemented concurrently with alcohol treatment, but only for Caucasian (not African-American) participants.58 Results cannot be generalized to the general population of smokers with alcohol use disorders.
It is evident that neither quitting smoking nor smoking cessation treatment-intervention results in worsening substance use outcomes (e.g. increased rates of relapse to alcohol or other drugs), even absent direct comparisons. For example, one study found participants who quit smoking reported less craving for stimulants (elimination of craving coupling)46 while two others (an RCT and analysis of a large prospective cohort) found those who quit smoking were less likely to have incident SUD diagnoses.33, 35 Further, if patients are able to quit smoking, it may make it easier for them to change other substance use.
Some limitations of this review bear noting. First, review was restricted to studies published in English. Second, findings in reviewed studies were limited to those the authors chose to publish. Third, meta-analysis was not conducted due to heterogeneity of outcomes, measurements, and sample characteristics. Fourth, studies reporting the impact of quitting smoking, or of “former smoker” status did not differentiate between former smokers who quit on their own and those who may have participated in a formal smoking cessation treatment intervention.
5. Conclusions
When considered in conjunction with the known, undisputed harms of smoking,61 this review provides support for policies encouraging quitting among smokers in SUD treatment settings and the offering of formal smoking cessation treatment or advice to quit, including cessation aids, to smokers who report use of other substances, whether or not they are seeking SUD treatment. Additionally, since provider barriers to offering smoking cessation treatment options and strategies to patients is often cited,62,63 this review also provides support for broad delivery of clinician training in smoking cessation treatment and support. The integration of such practices and policies will improve the health and wellbeing not only of substance using populations, but also of their families and friends- now and for future generations. Failing to do so is tantamount to increased harm.
Highlights.
Quitting smoking/smoking cessation has a positive effect on substance use outcomes
Improvement in a range of alcohol and drug use outcomes was reported
Smoke-free policy nor cessation intervention worsened SUD treatment outcomes
Smoking cessation aid should be offered to any individual who reports substance use
Not offering smoking cessation in SUD treatment is tantamount to increased harm
Acknowledgments
Funding: This work was supported by the National Institute on Drug Abuse (NIDA) [grant number K23 DA032578] and National Cancer Institute (NCI) [grant R25 CA113710]. NIDA and NCI had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
KM and DR designed the review. KM conducted the literature review. KM and JT selected and summarized articles for the review. KM wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
All three authors declare they have no conflicts of interest.
References
- 1.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psych. 2007 doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 2.Guydish J, Passalacqua E, Pagano A, et al. An international systematic review of smoking prevalence in addiction treatment. Addiction. 2015 doi: 10.1111/add.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalman D, Morissette SB, George TP. Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict. 2005 doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedmann PD, Jiang L, Richter KP. Cigarette smoking cessation services in outpatient substance abuse treatment programs in the United States. J Subst Abuse Treat. 2008 doi: 10.1016/j.jsat.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuller BE, Guydish J, Tsoh J, et al. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. J Subst Abuse Treat. 2007 doi: 10.1016/j.jsat.2006.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knudsen HK, Studts JL, Boyd S, Roman PM. Structural and cultural barriers to the adoption of smoking cessation services in addiction treatment organizations. J Addictive Dis. 2010 doi: 10.1080/10550887.2010.489446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stubbs J, Haw C, Garner L. Survey of staff attitudes to smoking in a large psychiatric hospital. The Psychiatrist. 2004 [Google Scholar]
- 8.Prochaska JJ, Fromont SC, Louie AK, Jacobs MH, Hall SM. Training in tobacco treatments in psychiatry: A national survey of psychiatry residency training directors. Academ Psych. 2006 doi: 10.1176/appi.ap.30.5.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richter KP, McCool RM, Okuyemi KS, Mayo MS, Ahluwalia JS. Patients’ views on smoking cessation and tobacco harm reduction during drug treatment. Nicotine Tob Res. 2002 doi: 10.1080/1462220021000032735. [DOI] [PubMed] [Google Scholar]
- 10.Prochaska JJ. Failure to treat tobacco use in mental health and addiction treatment settings: A form of harm reduction? Drug Alcohol Depend. 2010 doi: 10.1016/j.drugalcdep.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prochaska JJ, Hall SM, Tsoh JY, et al. Treating tobacco dependence in clinically depressed smokers: Effect of smoking cessation on mental health functioning. Am J Public Health. 2008 doi: 10.2105/AJPH.2006.101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayworth P. My name is Peg Hayworth and I am a caseworker at step forward, which is a rehabilitative psychosocial club for the chronically mentally ill in Waco, Texas. :524108319–524108322. https://industrydocuments.library.ucsf.edu/tobacco/docs/#id=kgnp0096. Accessed January 27, 2016.
- 13.Robertson ER. I am a psychiatrist at the Hawaii state hospital. :522700931–522700932. https://industrydocuments.library.ucsf.edu/tobacco/docs/#id=jzfv0097. Accessed January 27, 2016.
- 14.Williams JM, Foulds J, Dwyer M, et al. The integration of tobacco dependence treatment and tobacco-free standards into residential addictions treatment in New Jersey. J Subst Abuse Treat. 2005 doi: 10.1016/j.jsat.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Guydish J, Passalacqua E, Tajima B, Manser ST. Staff smoking and other barriers to nicotine dependence intervention in addiction treatment settings: A review. J Psychoactive Drugs. 2007 doi: 10.1080/02791072.2007.10399881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziedonis DM, Guydish J, Williams JM, Steinberg M, Foulds J. Barriers and solutions to addressing tobacco dependence in addiction treatment programs. Alc Res Health. 2007 [PMC free article] [PubMed] [Google Scholar]
- 17.Cookson C, Strang J, Ratschen E, Sutherland G, Finch E, McNeill A. Smoking and its treatment in addiction services: Clients’ and staff behaviour and attitudes. BMC Health Serv Res. 2014 doi: 10.1186/1472-6963-14-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiorentine R, Hillhouse MP. Drug treatment and 12-step program participation: The additive effects of integrated recovery activities. J Subst Abuse Treat. 2000 doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- 19.White WL, Boyle M, Loveland D. Alcoholism/addiction as a chronic disease: From rhetoric to clinical reality. Alcoholism Treatment Quarterly. 2002 [Google Scholar]
- 20.White WL. Slaying the dragon: The history of addiction treatment and recovery in America. Chestnut Health Systems/Lighthouse Institute; Bloomington, IL: 1998. [Google Scholar]
- 21.Laudet AB, White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. J Subst Abuse Treat. 2010 doi: 10.1016/j.jsat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bobo JK, Husten C. Sociocultural influences on smoking and drinking. Alc Res Health. 2000 [PMC free article] [PubMed] [Google Scholar]
- 23.Kotz MM. A smoke-free chemical dependency unit: The cleveland clinic experience. J Subst Abuse Treat. 1993 doi: 10.1016/0740-5472(93)90036-2. [DOI] [PubMed] [Google Scholar]
- 24.Caldwell PE, Cutter HS. Alcoholics Anonymous affiliation during early recovery. J Subst Abuse Treat. 1998 doi: 10.1016/s0740-5472(97)00191-8. [DOI] [PubMed] [Google Scholar]
- 25.Laudet AB, Morgen K, White WL. The role of social supports, spirituality, religiousness, life meaning and affiliation with 12-step fellowships in quality of life satisfaction among individuals in recovery from alcohol and drug problems. Alcoholism Treatment Quarterly. 2006 doi: 10.1300/J020v24n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Orlando M, Tucker JS, Ellickson PL, Klein DJ. Concurrent use of alcohol and cigarettes from adolescence to young adulthood: An examination of developmental trajectories and outcomes. Subst Use Misuse. 2005 doi: 10.1081/JA-200030789. [DOI] [PubMed] [Google Scholar]
- 27.Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. J Subst Abuse Treat. 2009 doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 28.Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004 doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- 29.Brown RA, Strong DR, Abrantes AM, Myers MG, Ramsey SE, Kahler CW. Effects on substance use outcomes in adolescents receiving motivational interviewing for smoking cessation during psychiatric hospitalization. Addict Behav. 2009 doi: 10.1016/j.addbeh.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Callaghan RC, Brewster JM, Johnson J, Taylor L, Beach G, Lentz T. Do total smoking bans affect the recruitment and retention of adolescents in inpatient substance abuse treatment programs? A 5-year medical chart review, 2001–2005. J Subst Abuse Treat. 2007 doi: 10.1016/j.jsat.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Lawn S, Campion J. Achieving smoke-free mental health services: Lessons from the past decade of implementation research. Int J Environ Res Public Health. 2013 doi: 10.3390/ijerph10094224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalman D, Kim S, DiGirolamo G, Smelson D, Ziedonis D. Addressing tobacco use disorder in smokers in early remission from alcohol dependence: The case for integrating smoking cessation services in substance use disorder treatment programs. Clin Psychol Rev. 2010 doi: 10.1016/j.cpr.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thurgood SL, McNeill A, Clark-Carter D, Brose LS. A systematic review of smoking cessation interventions for adults in substance abuse treatment or recovery. Nicotine Tob Res. 2015 doi: 10.1093/ntr/ntv127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chun J, Guydish J, Chan Y. Smoking among adolescents in substance abuse treatment: A study of programs, policy, and prevalence. J Psychoactive Drugs. 2007 doi: 10.1080/02791072.2007.10399883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walters WH. Google scholar search performance: Comparative recall and precision. Portal: Libraries and the Academy. 2009 [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009 [PMC free article] [PubMed] [Google Scholar]
- 37.Slavin RE. Best evidence synthesis: An intelligent alternative to meta-analysis. J Clin Epidemiol. 1995 doi: 10.1016/0895-4356(94)00097-a. [DOI] [PubMed] [Google Scholar]
- 38.Berg KM, Piper ME, Smith SS, Fiore MC, Jorenby DE. Defining and predicting short-term alcohol use changes during a smoking cessation attempt. Addict Behav. 2015 doi: 10.1016/j.addbeh.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cavazos-Rehg PA, Breslau N, Hatsukami D, et al. Smoking cessation is associated with lower rates of mood/anxiety and alcohol use disorders. Psychol Med. 2014 doi: 10.1017/S0033291713003206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dawson DA, Goldstein RB, Grant BF. Prospective correlates of drinking cessation: Variation across the life-course. Addiction. 2013 doi: 10.1111/add.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Piper ME, Rodock M, Cook JW, Schlam TR, Fiore MC, Baker TB. Psychiatric diagnoses among quitters versus continuing smokers 3 years after their quit day. Drug Alcohol Depend. 2013 doi: 10.1016/j.drugalcdep.2012.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsoh JY, Chi FW, Mertens JR, Weisner CM. Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Dios MA, Vaughan EL, Stanton CA, Niaura R. Adolescent tobacco use and substance abuse treatment outcomes. J Subst Abuse Treat. 2009 doi: 10.1016/j.jsat.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Myers MG, Doran NM, Brown SA. Is cigarette smoking related to alcohol use during the 8 years following treatment for adolescent alcohol and other drug abuse? Alcohol Alcohol. 2007 doi: 10.1093/alcalc/agm025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Satre DD, Kohn CS, Weisner C. Cigarette smoking and long-term alcohol and drug treatment outcomes: A telephone follow-up at five years. Am J Addict. 2007 doi: 10.1080/10550490601077825. [DOI] [PubMed] [Google Scholar]
- 46.Magee JC, Winhusen T. The coupling of nicotine and stimulant craving during treatment for stimulant dependence. 2015 doi: 10.1037/ccp0000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Metrik J, Spillane NS, Leventhal AM, Kahler CW. Marijuana use and tobacco smoking cessation among heavy alcohol drinkers. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2011.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kahler CW, Borland R, Hyland A, et al. Quitting smoking and change in alcohol consumption in the international tobacco control (ITC) four country survey. Drug Alcohol Depend. 2010 doi: 10.1016/j.drugalcdep.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rohsenow DJ, Tidey JW, Martin RA, et al. Contingent vouchers and motivational interviewing for cigarette smokers in residential substance abuse treatment. J Subst Abuse Treat. 2015 doi: 10.1016/j.jsat.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alessi SM, Petry NM. Smoking reductions and increased self-efficacy in a randomized controlled trial of smoking abstinence-contingent incentives in residential substance abuse treatment patients. Nicotine Tob Res. 2014 doi: 10.1093/ntr/ntu095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lisha NE, Carmody TP, Humfleet GL, Delucchi KL. Reciprocal effects of alcohol and nicotine in smoking cessation treatment studies. Addict Behav. 2014 doi: 10.1016/j.addbeh.2013.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reitzel LR, Nguyen N, Eischen S, Thomas J, Okuyemi KS. Is smoking cessation associated with worse comorbid substance use outcomes among homeless adults? Addiction. 2014 doi: 10.1111/add.12688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Winhusen TM, Kropp F, Theobald J, Lewis DF. Achieving smoking abstinence is associated with decreased cocaine use in cocaine-dependent patients receiving smoking-cessation treatment. Drug Alcohol Depend. 2014 doi: 10.1016/j.drugalcdep.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campbell CI, Chi F, Sterling S, Kohn C, Weisner C. Self-initiated tobacco cessation and substance use outcomes among adolescents entering substance use treatment in a managed care organization. Addict Behav. 2009 doi: 10.1016/j.addbeh.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stahre MA, Toomey TL, Erickson DJ, Forster JL, Okuyemi KS, Ahluwalia JS. The effects of a tobacco intervention on binge drinking among African American light smokers. J Addict Dis. 2013 doi: 10.1080/10550887.2013.849972. [DOI] [PubMed] [Google Scholar]
- 56.Myers MG, Prochaska JJ. Does smoking intervention influence adolescent substance use disorder treatment outcomes? Substance Abuse. 2008 doi: 10.1080/08897070802093361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brook JS, Balka EB, Ning Y, Brook DW. Trajectories of cigarette smoking among African Americans and puerto ricans from adolescence to young adulthood: Associations with dependence on alcohol and illegal drugs. Am J Addict. 2007 doi: 10.1080/10550490701375244. [DOI] [PubMed] [Google Scholar]
- 58.Fu SS, Kodl M, Willenbring M, et al. Ethnic differences in alcohol treatment outcomes and the effect of concurrent smoking cessation treatment. Drug Alcohol Depend. 2008 doi: 10.1016/j.drugalcdep.2007.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fiore M, Jaen CR, Baker T, et al. Treating tobacco use and dependence: 2008 update. Evidence Based Practices for Substance Use Disorders. 2008 http://lib.adai.washington.edu/dbtw-wpd/exec/dbtwpub.dll?BU=http%3A//lib.adai.washington.edu/ebpsearch.htm&TN=EBP&QY=Find+AccessNo=50&RF=Full+Display&DF=Full+Display&NP=3&RL=1&DL=0&XC=/dbtw-wpd/exec/dbtwpub.dll&AC=QBE_QUERY&CS=0. Accessed September 22, 2016.
- 60.Joseph AM, Willenbring ML, Nugent SM, Nelson DB. A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. J Stud Alcohol. 2004 doi: 10.15288/jsa.2004.65.681. [DOI] [PubMed] [Google Scholar]
- 61.US Department of Health and Human Services. The health consequences of smoking: 50 years of progress: A report of the surgeon general. 2014 [Google Scholar]
- 62.Blumenthal DS. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med. 2007 doi: 10.3122/jabfm.2007.03.060115. [DOI] [PubMed] [Google Scholar]
- 63.Bowman J, Walsh R. Smoking intervention within alcohol and other drug treatment services: A selective review with suggestions for practical management. Drug Alcohol Rev. 2003 doi: 10.1080/0959523021000059857. [DOI] [PubMed] [Google Scholar]


