Abstract
Aims
The prevalence of heroin use among nonmedical prescription opioid (NMPO) users has increased in recent years. Identifying characteristics associated with heroin use in this population can help inform efforts to prevent heroin initiation and maintenance. The aim of this study was to evaluate differences in perceived risk of heroin among NMPO users with and without histories of heroin use, and to examine temporal trends in perceived risk of heroin among this population.
Methods
Data are from the 2002–2013 National Survey on Drug Use and Health, and included all past-year NMPO users (N=49,045). Participants reported perceived risk of trying heroin once or twice and regular heroin use. Responses were coded dichotomously (great risk vs. other risk) and logistic regression analyses were used to evaluate the association between lifetime heroin use and perceived risk of heroin, and to determine temporal changes in perceived risk.
Results
Results indicated a significant association between lifetime heroin use and lower likelihood of reporting great risk of trying heroin (OR = 0.38, 95% CI: 0.33, 0.44, p < .001), and of regular use of heroin (OR = 0.39, 95% CI: 0.32, 0.48, p < .001). There was a significant, yet modest, trend toward decreasing perception of great risk from 2002–2013.
Conclusions
Findings from this analysis of nationally representative data indicate that NMPO users with a history of heroin use perceive heroin to be less risky. Perception of risk has decreased from 2002–2013 in this population, consistent with increasing rates of heroin initiation.
Keywords: Heroin, Opioid, Nonmedical Prescription Opioid Use, Perceived Risk, National Survey on Drug Use and Health
1. Introduction
An estimated 681,000 individuals in the United States used heroin in 2013, representing an 82.6% increase since 2007 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2014). This increase is largely driven by escalating rates of heroin initiation among nonmedical prescription opioid analgesic (NMPO) users (Compton, Jones, & Baldwin, 2016; Jones, 2013). For example, past-year heroin initiation rates were 19 times higher among individuals reporting lifetime NMPO use relative to those without a history of NMPO use (Muhuri, Gfroerer, & Davies, 2013). These trends are concerning because, among NMPO users, heroin use is associated with intravenous (IV) drug use (Mars, Bourgois, Karandinos, Montero, & Ciccarone, 2014; Mateu-Gelabert, Guarino, Jessell, & Teper, 2015; Meyer, Miller, & Sigmon, 2015; Potter et al., 2013), poor treatment outcomes (i.e., low rates of opioid abstinence and retention) (McCabe et al., 2013; Meyer et al., 2015; Nielsen, Hillhouse, Mooney, Ang, & Ling, 2015; Nielsen, Hillhouse, Thomas, Hasson, & Ling, 2013; Potter et al., 2013), and overdose (Frank et al., 2015; Lake et al., 2015). Understanding differences between NMPO users with and without heroin use is needed to identify potential risk factors for initiating heroin use.
Cross-sectional and prospective studies have identified several sociodemographic and substance-related characteristics associated with heroin use among NMPO users, such as frequent NMPO use (Jones, 2013; Muhuri et al., 2013), prescription opioid dependence (Carlson, Nahhas, Martins, & Daniulaityte, 2016; Jones, 2013; Muhuri et al., 2013), early age of NMPO initiation (Carlson et al., 2016; Rigg & Monnat, 2015), use of prescription opioids to get high (as opposed to self-medicating for pain) (Carlson et al., 2016), IV or intranasal NMPO use (Carlson et al., 2016), and young adult age (i.e., 18–25 years old) (Jones, 2013; Rigg & Monnat, 2015). Although these findings help identify at-risk groups of NMPO users who might benefit from close monitoring and intervention to prevent transition to heroin use, most of these characteristics are not modifiable, and thus cannot be directly targeted with intervention. Dynamic risk factors, or those that can be modified, can be used as therapeutic targets in prevention and treatment efforts to mitigate the risk of heroin initiation and maintenance. The current study aimed to investigate the association between heroin use and a potential dynamic risk factor: perceived risk of using heroin.
Lower perceived risk is associated with use of substances, such as alcohol (Chomynova, Miller, & Beck, 2009; Thornton, Baker, Johnson, & Lewin, 2013), tobacco (Gerking & Khaddaria, 2012; Thornton et al., 2013), marijuana (Apostolidis, Fieulaine, Simonin, & Rolland, 2006; Kilmer, Hunt, Lee, & Neighbors, 2007; Piontek, Kraus, Bjarnason, Demetrovics, & Ramstedt, 2013; Thornton et al., 2013), and MDMA (Leung, Ben Abdallah, Copeland, & Cottler, 2010). Among adolescents, greater perceived risk is associated with disapproval of a substance and lower prevalence of substance use (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2016).
Lower perceived risk of prescription opioids is associated with both initiation and continued use of prescription opioids (Arria, Caldeira, Vincent, O'Grady, & Wish, 2008; Lord, Brevard, & Budman, 2011). Although NMPO users generally perceive prescription opioids as “safer” than illicit drugs (Daniulaityte, Falck, & Carlson, 2012; Mars et al., 2014), limited information is available on perceived risk of heroin among NMPO users. A study of past-year opioid users found that perceived risk of heroin was higher among NMPO-only users relative to heroin-only users, and NMPO users who had also used heroin (Rigg & Monnat, 2015). However, this study did not examine the impact of other variables potentially associated with perceived risk, such as severity of NMPO use (e.g., number of days of use, presence of an opioid use disorder).
Moreover, little is known about temporal trends in perceived risk of heroin use in NMPO users. Despite widespread media and public health attention to the misuse of opioids and opioid overdose risk in recent years (Cicero, Ellis, Surratt, & Kurtz, 2014; McCarty et al., 2015), heroin use has continued to escalate (Jones, 2013; SAMHSA, 2014). It is unclear whether perceived risk of heroin has changed during this period in the context of these trends.
The overarching aim of this study was to examine differences in perceived risk of heroin use among NMPO users with and without histories of heroin use. Participants ages 12 and older from a large, nationally representative survey in the United States who reported past-year NMPO use were included in this study. We hypothesized that NMPO users who had never used heroin would perceive greater risk of heroin use relative to those who had used heroin in their lifetime. In an exploratory analysis, we examined temporal trends from 2002–2013 in perceived risk of heroin among individuals reporting past-year NMPO use.
2. Method
2.1 Data Source
Data were obtained from the National Survey on Drug Use and Health (NSDUH) public use data files for the years 2002 through 2013. The NSDUH is an annual survey designed to produce national estimates on the prevalence and correlates of substance use. Participants were selected through an independent, multistage area probability sample for each of the 50 states and Washington, DC. Survey responses were collected via audio computer-assisted self-interview and computer-assisted personal interview administered by a trained interviewer. To maintain confidentiality, the public use data file was de-identified and consists of a nationally representative subset of the total sample; from 2002 to 2013, an average of 55,435 participants was included in the public use data file. Detailed survey methods are reported elsewhere (SAMHSA, 2014).
2.2 Measures
2.2.1 Sociodemographic Measures
Sociodemographic measures included gender, age, race/ethnicity, education, and annual income. Population density (large urban, small urban, rural) was determined based on 2000 Census data and the June 2003 Core-Based Statistical Area classifications.
2.2.2 Substance Use
Survey respondents endorsing past-year NMPO use from 2002–2013 (N=49,045) were included in this analysis. NMPO use refers to the use of opioid analgesics that are not prescribed to the individual, or taking opioid analgesics exclusively for the experience or feelings they produce (SAMHSA, 2014). To determine NMPO use, participants were shown cards with pictures and names of opioid analgesics (e.g., Percocet®, Vicodin®, Lortab®) and specified which, if any, they had ever used nonmedically. If a participant endorsed nonmedical use of any prescription opioid, they were classified as having lifetime NMPO use. These respondents then identified the length of time since their most recent use and were categorized into groups based on most recent use (i.e., lifetime use, past-year use, past-month use); these variables were included in the NSDUH public use data file. Likewise, participants were asked if they had ever used heroin in their lifetime. For both heroin and NMPO use, participants answered questions about frequency of use in the past year.
Participants answered additional questions about tobacco, alcohol, and other illicit substance use (i.e., marijuana, cocaine, crack cocaine, hallucinogens, inhalants, tranquilizers, stimulants or amphetamines, sedatives). Survey respondents reporting past-year alcohol or drug use answered a standardized set of questions to establish Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 2000) criteria for substance abuse or dependence.
2.2.3 Perceived Risk of Heroin
All survey respondents were asked to answer questions about their perceived risk of several drugs of abuse, including heroin. Participants reported how much they believe people risk harming themselves physically or otherwise when they try heroin once or twice, and when they use heroin regularly (i.e., once or twice a week). Response options included “great risk,” “moderate risk,” “slight risk,” and “no risk.” Responses were then dichotomized into great perceived risk and other (moderate, low, no) perceived risk, consistent with other studies of perceived risk (Pacek, Mauro, & Martins, 2015; Schuermeyer et al., 2014).
2.3 Data Analysis
We examined whether a history of heroin use was associated with the perceived risk of heroin, using logistic regression analyses. Separate regression models were developed for the risk of trying heroin once or twice, and regular use of heroin (i.e., 1–2 times per week). Dichotomized perceived risk (great risk vs. any other risk) was the dependent variable for these analyses, and lifetime heroin use was the focal independent variable. These models included sociodemographic and clinical covariates that have previously been associated with heroin use among NMPO users, or that might be associated with perceived risk (i.e., age, gender, race, family income, population density, education, age of first NMPO use, number of days of NMPO use in the past-year, presence of other illicit drug use in the past-year). These models also controlled for diagnosis of a prescription opioid use disorder (abuse or dependence), and examined the prescription opioid use disorder by heroin use interaction term to determine whether diagnosis moderated the association between heroin use and perceived risk.
Next, we examined whether the year of the study was associated with perceived risk to determine trends in perceived risk of heroin from 2002–2013. For this analysis, study year was added to the logistic regression models. The year by heroin use and year by prescription opioid use disorder interaction terms were added to determine whether temporal trends were moderated by the presence of heroin use or a prescription opioid use disorder diagnosis.
The complex sampling strategy utilized in the NSDUH was accounted for in all analyses to calculate standard errors and point estimates by using analysis weights provided in the NSDUH public access database. Variables for which imputed values were available for missing data were used. Interaction terms were calculated for potential moderators, and all models testing interactions included both the interaction term and the main effects for the moderator and focal independent variable. In models for which interaction terms were not significant, these interactions were removed from the final reported model for ease of interpretation. These analyses were conducted using the Complex Samples procedure in SPSS Version 20.
3. Results
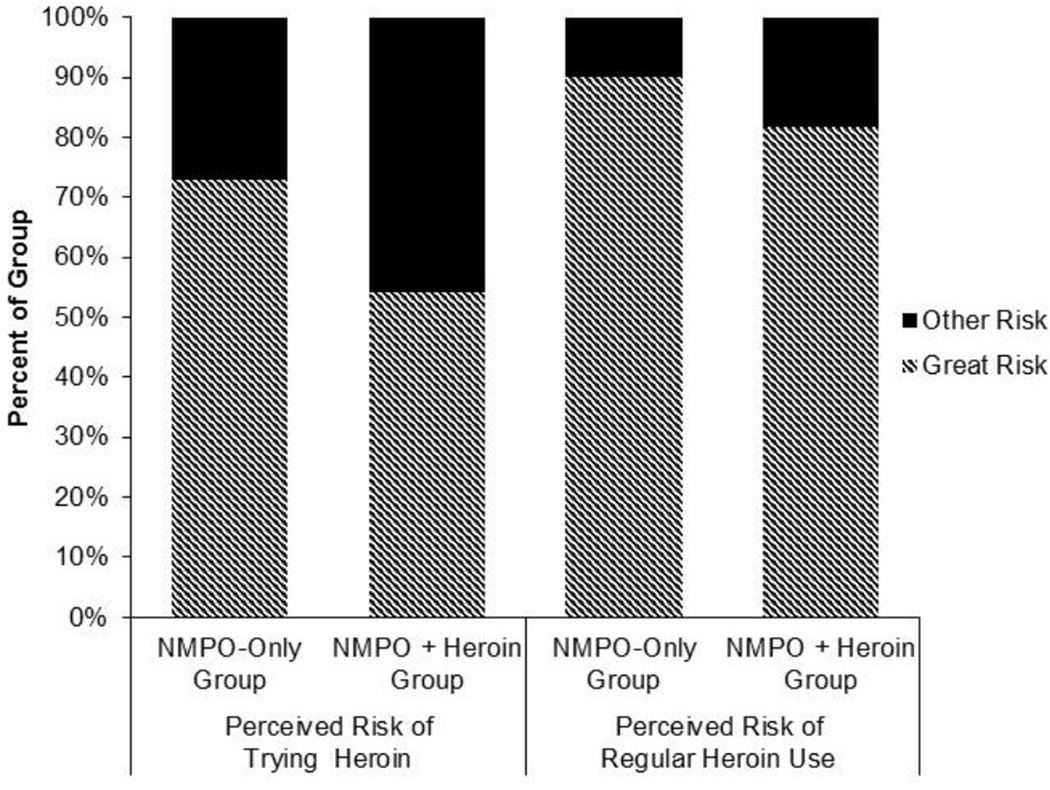
Perceived risk of trying heroin and regular use of heroin by those with and without a history of heroin use is depicted in Figure 1. Results indicated a significant association between heroin use and lower likelihood of reporting great risk of trying heroin once or twice (OR = 0.38, 95% CI = 0.33, 0.44, p < .001), and of regular use of heroin (OR = 0.39, 95% CI = 0.32, 0.48, p < .001). Table 1 presents the results of the logistic regression analyses testing the association between lifetime heroin use and perceived risk of trying heroin, and the results of the model examining perceived risk of regular heroin use.
Figure 1.
Perceived Risk of Heroin Use among Past-Year NMPO Users
Table 1.
Adjusted Logistic Regression Predicting Great Perceived Risk of Heroin
| Great Perceived Risk of Trying Heroin |
Great Perceived Risk of Regular Heroin Use |
|||
|---|---|---|---|---|
| Variable | OR (95% CI) | p | OR (95% CI) | p |
| Heroin Use | <0.001 | <0.001 | ||
| No Lifetime heroin use | Ref | Ref | ||
| Lifetime heroin use | 0.38 (0.33– 0.44) |
0.39 (0.32– 0.48) |
||
| Age | 0.007 | 0.430 | ||
| 26 years or older | Ref | Ref | ||
| 18–25 years | 0.88 (0.80– 0.97) |
1.07 (0.91– 1.26) |
||
| 12–17 years | 0.84 (0.73– 0.96) |
0.33 (0.26– 0.44) |
||
| Gender | <0.001 | 0.001 | ||
| Female | Ref | Ref | ||
| Male | 0.71 (0.65– 0.77) |
0.82 (0.74– 0.92) |
||
| Race | 0.032 | <0.001 | ||
| Non-Hispanic White | Ref | Ref | ||
| African American | 1.11 (0.96– 1.29) |
0.54 (0.45– 0.66) |
||
| Hispanic | 1.18 (1.05– 1.33) |
0.61 (0.51– 0.73) |
||
| Other | 1.03 (0.85– 1.26) |
0.52 (0.38– 0.71) |
||
| Education | <0.001 | <0.001 | ||
| Less than high school | Ref | Ref | ||
| Age 12–17 | 0.53 (0.45– 0.63) |
1.55 (1.14– 2.11) |
||
| High school graduate | 0.92 (0.80– 1.06) |
1.23 (1.01– 1.49) |
||
| Some college | 0.79 (0.68– 0.92) |
1.63 (1.30– 2.05) |
||
| College graduate | 0.53 (0.45– 0.63) |
1.55 (1.14– 2.11) |
||
| Income | 0.072 | <0.001 | ||
| >$75,000/year | Ref | Ref | ||
| $50,000–$74,999/year | 1.01 (0.88– 1.15) |
1.02 (0.80– 1.29) |
||
| $20,000–$49,999/year | 1.03 (0.92– 1.15) |
0.86 (0.70– 1.06) |
||
| <$20,000/year | 0.92 (0.83– 1.03) |
0.70 (0.57– 0.88) |
||
| Population Density | 0.239 | 0.111 | ||
| Large urban | Ref | Ref | ||
| Small urban | 1.03 (0.95– 1.11) |
0.95 (0.84– 1.08) |
||
| Rural | 0.90 (0.78– 1.04) |
0.77 (0.60– 0.98) |
||
| Prescription Opioid Use Disorder | 0.910 | 0.137 | ||
| No past-year diagnosis | Ref | Ref | ||
| Past-year diagnosis | 1.01 (0.90– 1.12) |
0.89 (0.76– 1.04) |
||
| Total Weeks of NMPO Use in Past Year* |
1.00 (0.99– 1.00) |
0.119 | 0.98 (0.98– 0.99) |
<0.001 |
| Age of First NMPO Use | 1.02 (1.01– 1.02) |
<0.001 | 1.02 (1.00– 1.03) |
0.014 |
| Any IV Drug Use | 0.272 | 0.936 | ||
| No IV drug use | Ref | Ref | ||
| History of IV drug use | 1.13 (0.91– 1.39) |
1.01 (0.79– 1.29) |
||
| Past-Year Substance Use | ||||
| No past-year use** | Ref | Ref | ||
| Marijuana | 1.12 (1.02– 1.23) |
0.017 | 1.61 (1.40– 1.83) |
<0.001 |
| Cocaine | 0.80 (0.72– 0.90) |
<0.001 | 1.00 (0.83– 1.20) |
0.997 |
| Crack Cocaine | 0.99 (0.83– 1.17) |
0.885 | 0.58 (0.44– 0.77) |
<0.001 |
| Hallucinogens | 0.86 (0.79– 0.95) |
0.003 | 0.92 (0.79– 1.07) |
0.271 |
| Tranquilizers | 1.06 (0.97– 1.16) |
0.220 | 1.20 (1.02– 1.41) |
0.026 |
| Stimulants | 0.89 (0.79– 1.01) |
0.071 | 0.86 (0.71– 1.05) |
0.135 |
| Sedatives | 0.82 (0.67– 1.00) |
0.053 | 0.80 (0.63– 1.02) |
0.076 |
Weeks were calculated using reported number of days of NMPO use in the past year.
Reference is no past-year use of each specific substance (e.g., reference for marijuana is no past-year marijuana use).
There was not a significant main effect of prescription opioid use disorder on perceived risk of trying heroin (OR = 1.01, 95% CI = 0.90, 1.12, p = .91) or regular heroin use (OR = 0.89, 95% CI = 0.76, 1.04, p = .14). Prescription opioid use disorder diagnosis did not moderate the association between heroin use and perceived risk of trying heroin (Wald F= 0.19, p = .67) or regular heroin use (Wald F= 0.61, p = .44); this interaction term was excluded from the final models.
Other significant predictors varied slightly between the two models (see Table 1). Specifically, female gender, later age of NMPO onset, and past-year marijuana use were associated with greater perceived risk of both trying heroin, and of regular heroin use. Older age, self-reported Hispanic ethnicity, and less education were associated with greater perceived risk of trying heroin, whereas cocaine and hallucinogen use were associated with lower perceived risk. Income of less than $20,000, race other than White, and crack cocaine use were all associated with lower perceived risk of regular heroin use; more education, fewer weeks of prescription opioid use, and tranquilizer use were associated with higher perceived risk of regular heroin use.
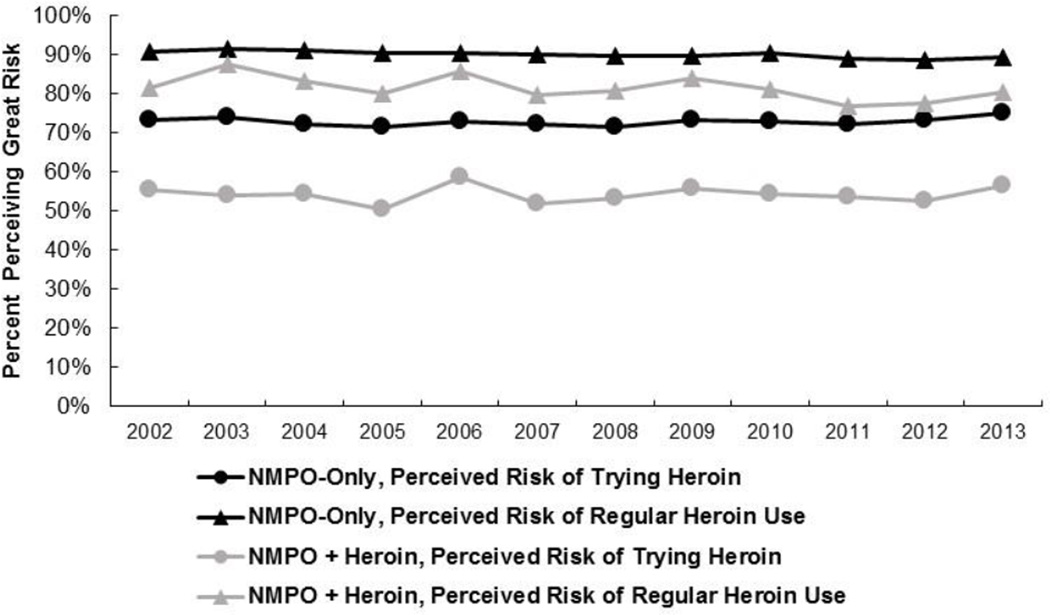
When year was added to the model, there was a modest main effect of year on perceived risk for both trying heroin (OR = 0.99, 95% CI = 0.98, 1.00, p = .006) and regular heroin use (OR = 0.97, 95% CI = 0.95, 0.99, p = .002), indicating that perceived risk of heroin use has modestly decreased from 2002–2013 among NMPO users. Although there was some minor fluctuation from year to year, and a modest downward trend overall, perceived great risk of heroin use from 2002–2013 remained relatively stable (see Figure 2). There were no significant interactions between year and heroin use, or year and diagnosis of a prescription opioid use disorder; these interaction terms were excluded from the final model.
Figure 2.
Trends in Great Perceived Risk of Heroin Use among NMPO Users
4. Discussion
This analysis of a large, nationally representative sample found that those who had never used heroin had more than 2.6 times greater odds of reporting great risk of trying heroin, and more than 3 times greater odds of reporting great risk of regular heroin use. These findings were not moderated by a prescription opioid use disorder diagnosis, suggesting that heroin use was associated with lower perceived risk, even for individuals with a prescription opioid use disorder. The modest downward trend in perceived risk of heroin from 2002–2013 is consistent with increasing rates of heroin initiation during the same period (Jones, 2013; SAMHSA, 2014). Nonetheless, this effect of time was modest, which might reflect the competing influence of increased public health awareness to the harms of opioid use.
This analysis consisted of cross-sectional analyses, and thus no conclusions can be drawn with respect to whether perceived risk impacts future heroin use among NMPO users. Prospective studies are necessary to determine if perceived risk predicts heroin initiation and maintenance. Nonetheless, lower perceived risk is cross-sectionally and prospectively associated with use of numerous substances (Apostolidis et al., 2006; Chomynova et al., 2009; Gerking & Khaddaria, 2012; Kilmer et al., 2007; Piontek et al., 2013; Leung et al., 2010; Thornton et al., 2013). Moreover, perceived risk appears to be important to both treatment engagement (Romer & Jamieson, 2001; Savoy et al., 2014) and reduction of substance use and substance-related behaviors (Bailey et al., 2007; Leung et al., 2010). The association between lifetime heroin use and perceived risk of heroin was not moderated by prescription opioid use disorder, suggesting that perceived risk might be a viable target for intervention, even among those with a prescription opioid use disorder.
In qualitative studies examining opioid use trajectories (i.e., transitions from NMPO use to heroin and injection drug use), participants often cite the risks associated with these behaviors as delaying or hindering drug use escalation (Daniulaityte et al., 2012; Mateu-Gelabert et al., 2015; Witteveen, Van Ameijden, & Schippers, 2006). Taken together, our findings and these qualitative studies suggest that perception of heroin risk is a promising candidate risk factor for the initiation of heroin use and related behaviors among NMPO users. We cannot, however, rule out the possibility that perceived risk of heroin decreases following heroin initiation, an effect that has been observed for marijuana use, but not alcohol or tobacco use (Grevenstein, Nagy, & Kroeninger-Jungaberle, 2015).
More than 50% of individuals reporting lifetime heroin use perceived great risk of trying heroin, and more than 80% perceived great risk of regular heroin use. Although these rates were significantly lower than NMPO users without histories of heroin use (more than 70% and 90% for trying and regular use, respectively), they still represent a substantial portion of those with lifetime heroin use. This finding begs a deeper understanding of what factors motivate an individual to use a drug, despite perceiving it to be highly risky. Impulsivity appears to be uniquely and additively associated with the initiation of substance use (Arria et al., 2008; Ryb, Dischinger, Kufera, & Read, 2006), and thus higher levels of impulsivity might contribute to the initiation of substance use, even among those with high perceived risk. Among adolescents, the protective effect of perceived risk is attenuated by living in a neighborhood with more opportunities for substance use (Zimmerman & Farrell, 2016), and peer influences have been shown to increase risk-taking more generally (Arnaud, Broning, Drechsel, Thomasius, & Baldus, 2012; Foxcroft, Ireland, Lister-Sharp, Lowe, & Breen, 2002). Future research examining additional moderators of perceived risk could clarify this discrepancy between perceived risk of heroin and its use.
Perceived risk of heroin among NMPO users has remained relatively stable from 2002–2013, with a modest downward trend. This is somewhat surprising considering the attention that opioid use has received in recent years (Cicero et al., 2014). For other substances, temporal changes in perceived risk appear to be affected through political and cultural mechanisms (e.g., medical marijuana policies, increased media attention to the risks associated with cocaine) (Bachman, Johnston, & O’Malley, 1990; Schuermeyer et al., 2014). Despite widespread media attention and policies surrounding heroin (Cicero et al., 2014; McCarty et al., 2015), perceived risk of heroin has remained relatively consistent among the general population (Lipari & Hughes, 2015), and has trended slightly downward among NMPO users. This might reflect the timing of current study, which includes data through 2013; it is possible that these trends will reverse as attention to the risks of opioid use continues to grow. Alternatively, the absence of substantial temporal changes in perceived risk of heroin might be attributable—at least in part—to a ceiling effect that precludes the ability to detect more subtle changes. Continued attention to this association, and to the ability of public health interventions to modify perceptions of risk on the population-level, are needed to enhance public health efforts preventing opioid initiation and maintenance.
Findings from this study contribute to the growing body of literature ascertaining factors associated with heroin use among NMPO users. A number of the risk factors for heroin use previously identified among NMPO users were also associated with lower perceived risk of heroin use in this study (e.g., younger age, early opioid initiation). Thus, perceived risk might reflect a mechanism linking these variables to likelihood of use, and accordingly might be a promising target in high-risk subgroups. Although young adult NMPO users (18–25 year olds) are at the highest risk for heroin initiation (Jones, 2013; Rigg & Monnat, 2015), adolescent age (12–17 years of age) was associated with lower perceived risk of heroin use, indicating that perceived risk might be a particularly important target among youth.
Cocaine and crack cocaine use were also associated with lower perceived risk of heroin, consistent with previous findings that cocaine use is robustly associated with heroin use (Jones, Logan, Gladden, & Bohm, 2015). Targeting perceived risk of heroin among those with concomitant cocaine and NMPO use might be worthwhile; treatment episodes for cocaine or opioid use disorder might be an effective point of intervention for this population. Past-year use of most other substances was not associated with lower perceived risk of heroin use, which echoes previous findings that use of other substances does not uniquely predict heroin initiation among NMPO users (Carlson et al., 2016). Nevertheless, heroin use is associated with more polysubstance use among NMPO users (Rigg & Monnat, 2015). Prospective studies are needed to examine the temporal relationship between polysubstance use and heroin use among NMPO users, including the potential impact of heroin use on perceived risk and initiation of other substances.
Data from other substances suggest that prevention and treatment interventions targeting consequences of substance use can be of benefit for increasing perceived risk and decreasing substance use. For example, primary prevention programs (e.g., school-based programs) providing normative feedback and educational information about consequences of substance use have produced significant change in perceived negative consequences of substance use (Giannotta, Vigna-Taglianti, Galanti, Scatigna, & Faggiano, 2014; Longshore, Ellickson, McCaffrey & St Clair, 2007). Motivational interviewing has shown promising effects in changing the perception of drug-related risk, in addition to reducing drug consumption (McCambridge & Strang, 2004).
We acknowledge several limitations of the present study. First, the NSDUH relies on self-report. Therefore, there is the risk of recall bias, as well as underreporting of substance use and other sensitive behaviors. Because this was a cross-sectional study, it cannot be determined if low perceived risk precedes heroin use, heroin contributes to a reduction in perceived risk, or a bi-directional relationship exists between heroin use and perceived risk. The NSDUH includes only non-institutionalized, civilian citizens, and therefore a portion of the population is not included, which might obscure population estimates of substance use (Wright, Gfroerer, & Epstein, 1997).
In conclusion, findings from this cross-sectional analysis indicate that NMPO users with lifetime heroin use perceive heroin to be less risky. Prospective studies are needed to determine whether this difference in perceived risk precedes heroin use, thus serving as a risk factor for heroin initiation and maintenance. Perceived risk of heroin appears to be modestly decreasing despite widespread media and public health attention to the harms associated with heroin use. Efforts at the public health and health services levels to increase the perceived risk of heroin use among NMPO users might be a fruitful target for decreasing this potential vulnerability for heroin use.
Highlights.
NMPO users with lifetime heroin use had lower perceived risk of heroin use.
Prescription opioid use disorder did not moderate this association.
Known risk factors for heroin use were associated with lower perceived heroin risk.
Among NMPO users, perceived risk of heroin decreased modestly from 2002–2013.
Acknowledgments
Role of Funding Sources
Effort on this manuscript was supported by NIDA grants K23 DA035297 (Dr. McHugh) and K24 DA022288 (Dr. Weiss). NIDA had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Dr. Weiss has consulted for Indivor, GW Pharmaceuticals, and US WorldMeds. Dr. Wittenauer has consulted for GW Pharmaceuticals.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosures
Conflict of Interest
All other authors declare they have no conflicts of interest.
Contributors
Ms. Votaw and Dr. McHugh designed this present analysis. Dr. McHugh undertook the statistical analysis. Ms. Votaw wrote the first draft of the manuscript. Drs. Wittenauer, Connery, and Weiss contributed to the interpretation and presentation of study findings. All authors contributed to and have approved the final manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Apostolidis T, Fieulaine N, Simonin L, Rolland G. Cannabis use, time perspective and risk perception: Evidence of a moderating effect. Psychology and Health. 2006;21(5):571–592. [Google Scholar]
- Arnaud N, Broning S, Drechsel M, Thomasius R, Baldus C. Web-based screening and brief intervention for poly-drug use among teenagers: study protocol of a multicentre two-arm randomized controlled trial. BMC Public Health. 2012;12:826. doi: 10.1186/1471-2458-12-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, O'Grady KE, Wish ED. Perceived harmfulness predicts nonmedical use of prescription drugs among college students: interactions with sensation-seeking. Prevention Science. 2008;9(3):191–201. doi: 10.1007/s11121-008-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachman JG, Johnston LD, O'Malley PM. Explaining the recent decline in cocaine use among young adults: further evidence that perceived risks and disapproval lead to reduced drug use. Journal of Health and Social Behavior. 1990;13(2):173–184. [PubMed] [Google Scholar]
- Bailey SL, Ouellet LJ, Mackesy-Amiti ME, Golub ET, Hagan H, Hudson SM, Garfein RS. Perceived risk, peer influences, and injection partner type predict receptive syringe sharing among young adult injection drug users in five U.S. cities. Drug and Alcohol Dependence. 2007;91S:S18–S29. doi: 10.1016/j.drugalcdep.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Hayes RB, Dunsiger S, Fava JL. Risk perception and smoking behavior in medically ill smokers: a prospective study. Addiction. 2010;105(6):1100–1108. doi: 10.1111/j.1360-0443.2010.02900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson RG, Nahhas RW, Martins SS, Daniulaityte R. Predictors of transition to heroin use among initially non-opioid dependent illicit pharmaceutical opioid users: A natural history study. Drug and Alcohol Dependence. 2016;160:127–134. doi: 10.1016/j.drugalcdep.2015.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomynova P, Miller P, Beck F. Perceived risks of alcohol and illicit drugs: relation to prevalence of use on individual and country level. Journal of Substance Use. 2009;14(3–4):250–264. [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. New England Journal of Medicine. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Falck R, Carlson RG. “I’m not afraid of those ones just ‘cause they’ve been prescribed”: Perceptions of risk among illicit users of pharmaceutical opioids. International Journal of Drug Policy. 2012;23(5):374–384. doi: 10.1016/j.drugpo.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxcroft DR, Ireland D, Lister-Sharp DJ, Lowe G, Breen R. Primary prevention for alcohol misuse in young people. Cochrane Database Syst Rev. 2002;3:CD003024. doi: 10.1002/14651858.CD003024. [DOI] [PubMed] [Google Scholar]
- Frank D, Mateu-Gelabert P, Guarino H, Bennett A, Wendel T, Jessell L, Teper A. High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. International Journal of Drug Policy. 2015;26(1):84–91. doi: 10.1016/j.drugpo.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerking S, Khaddaria R. Perceptions of health risk and smoking decisions of young people. Health economics. 2012;21(7):865–877. doi: 10.1002/hec.1760. [DOI] [PubMed] [Google Scholar]
- Giannotta F, Vigna-Taglianti F, Galanti MR, Scatigna M, Faggiano F. Short-term mediating factors of a school-based intervention to prevent youth substance use in Europe. Journal of Adolescent Health. 2014;54(5):565–573. doi: 10.1016/j.jadohealth.2013.10.009. [DOI] [PubMed] [Google Scholar]
- Grevenstein D, Nagy E, Kroeninger-Jungaberle H. Development of risk perception and substance use of tobacco, alcohol and cannabis among adolescents and emerging adults: evidence of directional influences. Substance Use & Misuse. 2015;50(3):376–386. doi: 10.3109/10826084.2014.984847. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers–United States, 2002–2004 and 2008–2010. Drug and Alcohol Dependence. 2013;132(1):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital Signs: Demographic and Substance Use Trends Among Heroin Users - United States, 2002–2013. MMWR Morbidity and Mortality Weekly Report. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- Kilmer JR, Hunt SB, Lee CM, Neighbors C. Marijuana use, risk perception, and consequences: is perceived risk congruent with reality? Addictive Behaviors. 2007;32(12):3026–3033. doi: 10.1016/j.addbeh.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Lake S, Hayashi K, Buxton J, Milloy MJ, Dong H, Wood E, Kerr T. The effect of prescription opioid injection on the risk of non-fatal overdose among people who inject drugs. Drug and Alcohol Dependence. 2015;156:297–303. doi: 10.1016/j.drugalcdep.2015.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung KS, Ben Abdallah A, Copeland J, Cottler LB. Modifiable risk factors of ecstasy use: risk perception, current dependence, perceived control, and depression. Addictive Behaviors. 2010;35(3):201–208. doi: 10.1016/j.addbeh.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari RN, Hughes A. NSDUH Report. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2015. Trends in Heroin Use in the United States: 2002 to 2013. [PubMed] [Google Scholar]
- Longshore D, Ellickson PL, McCaffrey DF, Clair PAS. School-based drug prevention among at-risk adolescents: Effects of ALERT plus. Health Education & Behavior. 2007;34(4):651–668. doi: 10.1177/1090198106294895. [DOI] [PubMed] [Google Scholar]
- Lord S, Brevard J, Budman S. Connecting to young adults: an online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Substance Use & Misuse. 2011;46(1):66–76. doi: 10.3109/10826084.2011.521371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’I ever said came true”: transitions from opioid pills to heroin injecting. International Journal of Drug Policy. 2014;25(2):257–266. doi: 10.1016/j.drugpo.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateu-Gelabert P, Guarino H, Jessell L, Teper A. Injection and sexual HIV/HCV risk behaviors associated with nonmedical use of prescription opioids among young adults in New York City. Journal of Substance Abuse Treatmeant. 2015;48(1):13–20. doi: 10.1016/j.jsat.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe BE, Santisteban DA, Mena MP, Duchene DM, McLean C, Monroe M. Engagement, retention, and abstinence for three types of opioid users in Florida. Substance Use & Misuse. 2013;48(8):623–634. doi: 10.3109/10826084.2013.800112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- McCarty D, Bovett R, Burns T, Cushing J, Glynn ME, Kruse J, Shames J. Oregon's strategy to confront prescription opioid misuse: a case study. Journal of Substance Abuse Treatmeant. 2015;48(1):91–95. doi: 10.1016/j.jsat.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer AC, Miller ME, Sigmon SC. Lifetime history of heroin use is associated with greater drug severity among prescription opioid abusers. Addictive Behaviors. 2015;42:189–193. doi: 10.1016/j.addbeh.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. The CBHSQ Data Review. 2013:1–17. [Google Scholar]
- Nielsen S, Hillhouse M, Mooney L, Ang A, Ling W. Buprenorphine pharmacotherapy and behavioral treatment: comparison of outcomes among prescription opioid users, heroin users and combination users. Journal of Substance Abuse Treatmeant. 2015;48(1):70–76. doi: 10.1016/j.jsat.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen S, Hillhouse M, Thomas C, Hasson A, Ling W. A comparison of buprenorphine taper outcomes between prescription opioid and heroin users. Journal of Addiction Medicine. 2013;7(1):33–38. doi: 10.1097/ADM.0b013e318277e92e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug and Alcohol Dependence. 2015;149:232–244. doi: 10.1016/j.drugalcdep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piontek D, Kraus L, Bjarnason T, Demetrovics Z, Ramstedt M. Individual and country-level effects of cannabis-related perceptions on cannabis use. A multilevel study among adolescents in 32 European countries. Journal of Adolescent Health. 2013;52(4):473–479. doi: 10.1016/j.jadohealth.2012.07.010. [DOI] [PubMed] [Google Scholar]
- Potter JS, Marino EN, Hillhouse MP, Nielsen S, Wiest K, Canamar CP, Ling W. Buprenorphine/naloxone and methadone maintenance treatment outcomes for opioid analgesic, heroin, and combined users: findings from starting treatment with agonist replacement therapies (START) Journal of Studies on Alcohol and Drugs. 2013;74(4):605–613. doi: 10.15288/jsad.2013.74.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg KK, Monnat SM. Comparing characteristics of prescription painkiller misusers and heroin users in the United States. Addictive Behaviors. 2015;51:106–112. doi: 10.1016/j.addbeh.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D, Jamieson P. The role of perceived risk in starting and stopping smoking. In: Slovic P, editor. Smoking: Risk, Perception, and Policy. Sage Publications; 2001. [Google Scholar]
- Ryb GE, Dischinger PC, Kufera JA, Read KM. Risk perception and impulsivity: association with risky behaviors and substance abuse disorders. Accident Analysis & Prevention. 2006;38(3):567–573. doi: 10.1016/j.aap.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Savoy E, Reitzel LR, Scheuermann TS, Agarwal M, Mathur C, Choi WS, Ahluwalia JS. Risk perception and intention to quit among a tri-ethnic sample of nondaily, light daily, and moderate/heavy daily smokers. Addictive Behaviors. 2014;39(10):1398–1403. doi: 10.1016/j.addbeh.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, Min SJ, Sakai JT. Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–11. Drug and Alcohol Dependence. 2014;140:145–155. doi: 10.1016/j.drugalcdep.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- Thornton LK, Baker AL, Johnson MP, Lewin T. Perceived risk associated with tobacco, alcohol and cannabis use among people with and without psychotic disorders. Addictive Behaviors. 2013;38(6):2246–2251. doi: 10.1016/j.addbeh.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Witteveen E, Van Ameijden EJ, Schippers GM. Motives for and against injecting drug use among young adults in Amsterdam: qualitative findings and considerations for disease prevention. Substance Use & Misuse. 2006;41(6–7):1001–1016. doi: 10.1080/10826080600669561. [DOI] [PubMed] [Google Scholar]
- Wright D, Gfroerer J, Epstein J. Ratio estimation of hardcore drug use. Journal of Official Statistics. 1997;13:401–416. [Google Scholar]
- Zimmerman GM, Farrell C. Parents, Peers, Perceived Risk of Harm, and the Neighborhood: Contextualizing Key Influences on Adolescent Substance Use. Journal of Youth and Adolescence. 2016:1–20. doi: 10.1007/s10964-016-0475-5. [DOI] [PubMed] [Google Scholar]