Abstract
PURPOSE
To examine the associations between substance use and antisocial behavior trajectories and seven risky behaviors over time.
METHOD
Data were collected from a high-risk sample of adolescents followed into young adulthood. Five trajectory classes, identified based on dual development of substance use and antisocial behavior symptoms, were used to predict three risky driving and four risky sexual behaviors.
RESULTS
In this high-risk sample, participants reported notably high overall rates of reckless driving (55.5%) and unprotected sex under the influence (44.8%) in the past year. Risky behaviors that are typically of low base rates in population-based studies were also elevated, with 8.8% reporting past-year driving under the influence (DUI) charge, 17.6% reporting lifetime sexually transmitted infection (STI), and 10.4% reporting lifetime injection drug use. The Dual Chronic class had the highest levels of all seven risky behaviors, and were 3–4 times more likely to report risky driving, lifetime STI, and injection drug use than the Relatively Resolved class. Rates of past-year reckless driving and DUI were elevated among classes with persistent antisocial behavior, whereas rates of DUI, DUI charge, and unprotected sex under the influence were elevated among classes with persistent substance use.
CONCLUSIONS
Young adults with persistent co-occurring substance use and antisocial behavior engage in multiple very costly risky behaviors. Differential associations between risky behaviors and trajectory classes highlight the need for targeted interventions.
Keywords: Substance Use, Antisocial Behavior, Risky driving, Sexual Transmitted Infections, Injection Drug Use
1. INTRODUCTION
Substance use and antisocial behaviors are very costly to society. In the U.S. excessive drinking, tobacco and illicit drug use together cost over 700 billion dollars each year due to loss in productivity, health care expenses, and criminal justice costs (Centers for Disease Control and Prevention, 2014; National Drug Intelligence Center, 2011). The estimated cost of a 14-year-old high-risk juvenile progressing into a criminal lifestyle ranges from 2.6 to 5.3 million dollars (Cohen and Piquero, 2008). Substance use and antisocial behaviors are highly correlated and are associated with numerous risky behaviors and negative developmental outcomes (Beauchaine and McNulty, 2013; Compton et al., 2005).
The externalizing spectrum model suggests a common etiological pathway to substance use and antisocial behaviors (Krueger et al., 2002, 2007), but limited research has extended this work to simultaneously examine co-occurrence of other risky behaviors such as risky driving or sexual behaviors. Risky driving can lead to fatal accidents, non-fatal injuries, and damaged vehicles. Motor vehicle crashes in the U.S. attributable to speeding and alcohol involvement have been estimated to cost 50.9 and 40.4 billion dollars, respectively (Blincoe et al., 2002). Sexual risk behaviors, including having multiple partners and unprotected sex, can lead to unplanned pregnancy and sexual transmitted infections (STIs; Capaldi et al., 2002; Valois et al., 1999). Adolescents with STIs were more than twice as likely to have a subsequent HIV infection (Newbern et al., 2013). Injection drug use is a risk factor for HIV infection, with the prevalence of HIV estimated at 15% among injection drug users (Mathers et al., 2008). The total direct estimated medical cost of STIs, including HIV, among adolescents is 6.5 billion dollars (Chesson et al., 2004). In sum, risky driving, sexual risk behaviors, STIs, and injection drug use are all costly risky behaviors that are of significant public health relevance. Less well understood is whether these risky behaviors are developmental outcomes of externalizing psychopathology.
1.1. Substance Use, Antisocial Behavior, and Risky Behaviors
Adolescent substance use is a strong predictor of concurrent and subsequent risky driving behaviors, including driving while impaired by alcohol or drugs (Bingham and Shope, 2004; Li et al., 2013; Vassallo et al., 2008). Of all motor-vehicle-related deaths in 2014, 31% were attributable to alcohol-impaired driving (National Center for Statistics and Analysis, 2015). In a national epidemiological study, cross-sectional data indicated that substance use disorder (SUD) and antisocial personality disorder (ASPD) were independently associated with reckless driving (Vaughn et al., 2011). Individuals convicted of driving under the influence (DUI) showed substantially higher rates of comorbid alcohol and drug use disorders than individuals in the general population (Lapham et al., 2001, 2006).
Adolescent substance use is also a significant predictor of young adulthood sexual risk behaviors (Bryan et al., 2012; Guo et al., 2002; Khan et al., 2012; Tapert et al., 2001). A recent meta-analysis indicated that adolescent substance use is associated with unprotected sex, more sexual partners, and sex with an intravenous drug user (Ritchwood et al., 2015). Antisocial behaviors in adolescence predicted sexual risk behaviors in young adulthood (Adalbjarnardottir and Rafnsson, 2002; Mason et al., 2010). Adolescents with a history of conduct disorder (CD) reported a greater number of lifetime sexual partners, and ASPD symptoms were positively associated with sexual risk behaviors (Lavan and Johnson, 2002). Taken together, both substance use and antisocial behaviors are likely important developmental precursors of risky driving and sexual risk behaviors.
1.2. The Current Study
No prior study has examined whether both the co-occurrence and persistence over time in substance use and antisocial behavior are associated with risky behaviors. In a highly affected sample of adolescents with early onset of problematic substance use and antisocial behavior, five latent classes with distinct “dual trajectories” of substance use and antisocial behaviors during young adulthood were previously identified (Trim et al., 2015). In the current study, we used this sample to examine whether risky driving and sexual risk behaviors were elevated in trajectory classes characterized by persistent substance use, persistent antisocial behavior, or the persistent co-occurrence of both behaviors. We hypothesized that the Dual Chronic class (characterized by persistent high levels of substance use and antisocial behavior) would have the highest rates of risky driving and sexual risk behaviors, whereas the Relatively Resolved class (characterized by relatively resolved substance use and antisocial behavior) would have the lowest rates of risky behaviors. While recognizing that alternative hypotheses could be supported by existing literature, our a priori hypotheses were theorized based on whether the risky behaviors of interest were related to substance use or not. Because DUI of alcohol or drugs, DUI charges, unprotected sex under the influence, and injection drug use are conceptually substance use related, we hypothesized that they would be more prevalent in the trajectory classes characterized by persistent substance use and relatively lower antisocial behavior. Because reckless driving, number of sexual partners, and STIs are not by definition related to substance use, we hypothesized that they would be more prevalent in the trajectory classes characterized by persistent antisocial behaviors and relatively lower substance use.
2. METHOD
2.1. Participants
Data were drawn from a high-risk sample of youth originally recruited for a study on familial transmission and genetic linkage of SUD and CD (Derringer et al., 2015; Melroy et al., 2014). The original sample included 799 youth (M age = 16.1 years, range 13–19 years) recruited from facilities in Denver, CO (substance use treatment programs and the juvenile criminal justice system) and San Diego, CA (treatment programs and alternative schools). At the baseline assessment (age range 13–19 years), each youth was asked to report on substance use and antisocial behavior for the past year. Follow-up interviews occurred on average 6.5 years (range from 3–12 years) after the original assessment. At the follow-up assessment (age range 19–30 years), in addition to providing ratings for the past year, participants also provided retrospective reports on these behaviors at age 18 years and at age 21 years when applicable. For participants who were older than 21 years old at follow-up, data from up to four time points were included (past year at baseline, past year at follow-up, and retrospective reports of behaviors at age 18 years and age 21 years collected at follow-up). For participants who were 19–21 years old at follow-up, data from up to three time points were included (past year at baseline, past year at follow-up, and retrospective report of behaviors at age 18 years collected at follow-up). In total, a majority of participants provided reports of substance use at three or four time points (69%) and most provided reports of antisocial behavior at three or four time points (90%).
Participants who completed a young adult follow-up interview were included as part of the trajectory class analyses based on substance use and antisocial behavior symptoms (n = 536; Trim et al., 2015), 6 of the participants had no follow-up data on risky behavior outcomes and were therefore excluded from the current study. The current sample (n = 530) had an average of 6.5 CD symptoms and 10.4 symptoms of non-tobacco substance abuse or dependence (summed for alcohol, marijuana, and other drugs) at initial assessment, and was similar to the full trajectory class sample in demographics, substance use, and antisocial behavior at baseline and follow-up. At follow-up, 27% (n = 142) of the sample were still in school and 59% (n = 312) were currently employed. Because of a skip pattern in our questionnaire, where only individuals who endorsed having sex with two or more different sexual partners in the past five years were asked all the sexual risk behavior questions, approximately 20% of the sample had missing responses to two questions on sexual risk behaviors (unprotected sex under the influence and STIs). Compared to participants with data on these two sexual risk behaviors, those with missing these data were significantly older (M age 23.1 vs. 22.5 years, t = 2.78, p < 0.01), but there were no significant differences across sex, race/ethnicity, or trajectory class. Age was controlled for in the primary analyses of all risky behavior outcomes.
2.2. Measures
2.2.1. Substance Use and Antisocial Behavior Trajectories
Past-year substance use and SUD criteria were assessed at baseline and follow-up using the Composite International Diagnostic Interview Substance Abuse Module (CIDI-SAM; Crowley et al., 2001), a structured diagnostic interview covering all major substances using the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R and DSM-IV) criteria. A supplement to the CIDI-SAM assessed frequency of substance use, which was the primary substance use variable in trajectory analyses. Baseline CD symptoms were assessed using Diagnostic Interview Schedule for Children (DISC; Shaffer et al., 1993), whereas ASPD symptoms at age 18 years, age 21 years, and in the past year were assessed using the Diagnostic Interview Schedule – Version IV (DIS-IV; Helzer, 1987). Substance use and antisocial behavior were also retrospectively reported for ages 18 years and 21 years for individuals above these ages at follow-up. An Alcohol and Other Drug index (AOD index) was created for past-year alcohol, marijuana, and other drug use, with frequency reported from 0 “never” to 7 “daily” (range of 0–21). An Antisocial Behavior index (ASB index) was created which summed past-year antisocial behaviors in five domains (law/rule-breaking, truancy/irresponsibility, stealing/deceitfulness, property destruction, and fighting/aggression), with a possible range of 0–10 (score of 0–2 for each domain). All repeated measures of AOD and ASB were entered into a latent class growth model, a person-centered analytic approach used to identify latent groups defined by similar patterns of change. Five trajectory classes were identified:
Class 1: Individuals classified as Dual Chronic (9.5%) had the highest initial levels of AOD which remained elevated over time, and high initial levels of ASB which increased over time, particularly from baseline to age 18 years.
Class 2: Individuals classified as Increasing AOD/Persistent ASB (18.1%) had significant increases in AOD over time, and had high initial levels of ASB, which followed a non-significant declining trend over time.
Class 3: Individuals classified as Persistent AOD/Adolescent ASB (29.0%) had stable high levels of AOD over time, and had a rapid decline in ASB by age 18 years, indicating adolescent-limited antisocial behaviors.
Class 4: Individuals classified as Decreasing Drugs/Persistent ASB (11.8%) had decreasing levels of drug use over time, whereas alcohol use declined from baseline to age 21 years but then increased to near-baseline levels at older ages. This class is also characterized by the highest initial levels of ASB which only declined slightly over time, and their ASB levels were second to those in the Dual Chronic group at older ages.
Class 5: Individuals classified as Relatively Resolved (31.5%) had elevated levels of AOD and lowest levels of ASB at baseline, with both AOD and ASB decreasing over time.
Demographic differences between latent trajectory classes were previously reported in Trim et al. (2015). Latent trajectory classes differed by sex but not by race/ethnicity. Relative to the Decreasing Drugs/Persistent ASB and Relatively Resolved classes, more males were found in the Dual Chronic, Increasing AOD/Persistent ASB, and Persistent AOD/Adolescent ASB classes. The omnibus effect of age on trajectory class was significant at p < 0.05, although the post-hoc corrected pairwise comparisons were not significant.
2.2.2. Risky Behaviors
Risky behavior measures were part of a self-report survey administered at follow-up. Past-year reckless driving and DUI of alcohol or drugs were measured using two single self-report items (0 “never” to 4 “very often”). Reckless driving was conceptualized as risky driving unrelated to alcohol/drug use and was defined as “taking chances when driving a car, motorcycle, or other vehicle—like speeding through city street or driving recklessly.” Number of past-year DUI charges was measured using a self-report item (0 “never” to 3 “more than two times”). Two self-report items assessed number of sexual partners in the past five years and frequency of past-year unprotected sex under the influence, with response options for both items ranging from “none” (0) to “20+” (6). For lifetime STI, a dichotomous measure assessed if participants had ever been told by a health professional that they had: hepatitis B, hepatitis C, gonorrhea, syphilis, genital warts (HPV), chlamydia (or NGU), and HIV/AIDS. For lifetime injection drug use, a dichotomous measure assessed if participants have ever injected drugs (not prescribed by a doctor) with a needle.
2.3. Statistical Analyses
Distributions of the continuous risky behavior measures exhibited significant deviation from normality. Preliminary analyses compared alternative regression models (e.g., linear, Poisson, negative binomial) to determine the optimal model for each outcome. Final models were analysis of covariance (ANCOVA) for sexual partners, Poisson regression for reckless driving and DUI, and negative binomial regression for DUI charges and unprotected sex under the influence. Logistic regression was used for the dichotomous outcomes of lifetime STI and injection drug use. Age, sex, and race/ethnicity (non-Hispanic White vs. all other racial/ethnic groups combined) were included as covariates. The alpha level was set to p < 0.05 for all primary analyses where the Relatively Resolved trajectory class was set as the referent group. To control for multiple comparisons, the alpha level was set to p < 0.01 for all follow-up pairwise comparisons. All statistical tests were two-tailed. All analyses were conducted in STATA 13.0.
3. RESULTS
3.1. Descriptive Statistics
At follow-up, participants had a mean age of 22.6 years (SD = 2.0). The sample was 73.4% male, with 50.9% non-Hispanic White, 7.9% African-American, 28.5% Hispanic, and 12.7% other race/ethnicity. Frequencies of risky behaviors are presented in Table 1 and are broadly summarized here. Over half of the participants (55.5%) had driven recklessly in the past year, and 47.7% reported DUI of alcohol or drugs in the past year. Almost 9% of the participants reported being charged with a DUI once or more in the past year. Almost half of the participants (49.4%) endorsed having six or more different sexual partners in the past five years. About 45% of participants reported having unprotected sex under the influence once or more in the past year. Lifetime rates of any STI and injection drug use were 17.6% and 10.4%, respectively.
Table 1.
Frequencies of risky driving and sexual risk behaviors for the overall sample and by trajectory class membership
| Overall | Trajectory Class 1: Dual Chronic | Trajectory Class 2: Increasing AOD/Persistent ASB | Trajectory Class 3: Persistent AOD/Adoles cent ASB | Trajectory Class 4: Decreasing Drugs/Persistent ASB | Trajectory Class 5: Relatively Resolved | |
|---|---|---|---|---|---|---|
| Risky Driving Behaviors | ||||||
| Past-Year Any Reckless Driving | 55.5% | 76.0% | 56.4% | 46.1% | 71.0% | 35.9% |
| Past-Year Any Driven Under Influence | 47.7% | 72.0% | 67.8% | 46.7% | 58.1% | 26.5% |
| Past-Year Any DUI/Driving Offense | 8.8% | 18.4% | 9.8% | 10.5% | 6.5% | 4.8% |
| Sexual Risk Behaviors | ||||||
| Past-5-Year ≥ 6 Sexual Partners | 49.4% | 85.7% | 56.0% | 43.6% | 50.8% | 39.2% |
| Past-Year Any Unprotected Sex Under Influence | 44.8% | 65.2% | 45.0% | 52.8% | 43.1% | 30.2% |
| Lifetime Any STIs | 17.6% | 22.0% | 13.8% | 8.4% | 6.5% | 8.3% |
| Lifetime Any Injection Drug Use | 10.4% | 25.5% | 17.1% | 12.2% | 29.4% | 15.5% |
3.2. Covariate Effects
Older age was associated with fewer sexual partners in the past five years (b = −0.12, SE = 0.04, p < 0.001). Males were more likely than females to report more sexual partners in the past five years (b = 0.40, SE = 0.17, p = 0.017) and more frequent unprotected sex under the influence (Incidence Rate Ratio [IRR] = 1.80, p = 0.003). Males were less likely than females to report any lifetime STI (Odds Ratio [OR] = 0.27, p < 0.001). Compared to non-Hispanic Whites, participants who belong to other racial/ethnic groups were less likely to have driven recklessly in the past year (IRR = 0.73, p = 0.001), less likely to report having more sexual partners in the past five years (b = −0.37, SE = 0.14, p = 0.009), and were less likely to report lifetime injection drug use (OR = 0.54, p = 0.043). Age, sex, and race/ethnicity were controlled for in all subsequent analyses.
3.3. Prediction of Risky Behavior from Trajectory Classes
3.3.1. Risky Driving Behaviors
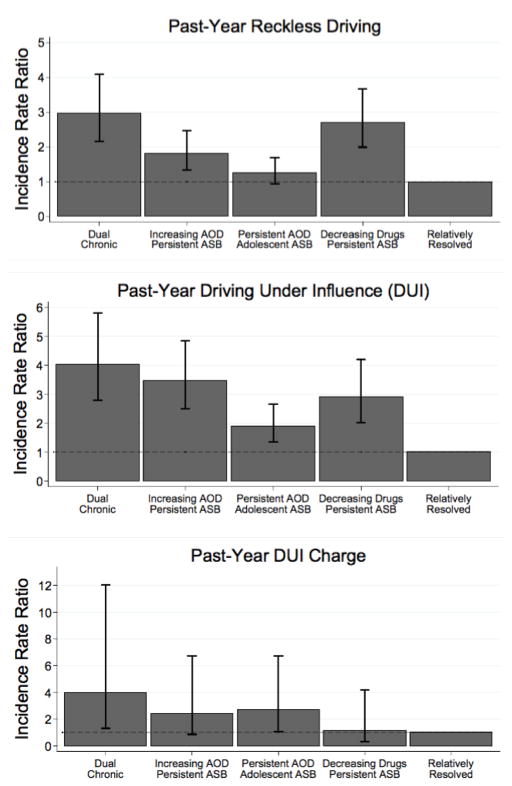
As shown in Figure 1, the Dual Chronic class was three times more likely than the Relatively Resolved class to have driven recklessly (IRR = 3.00, p < 0.001), and four times more likely to have DUI of alcohol or drugs (IRR = 4.03, p < 0.001) and to be charged with DUI (IRR = 3.99, p = 0.014) in the past year. The Increasing AOD/Persistent ASB and Decreasing Drugs/Persistent ASB classes were both more likely than the Relatively Resolved class to have driven recklessly (IRRs = 1.82 and 2.70, ps < 0.001) and have DUI of alcohol or drugs (IRRs = 3.47 and 2.91, ps < 0.001) in the past year. The Persistent AOD/Adolescent ASB class was more likely than the Relatively Resolved class to have DUI of alcohol or drugs (IRR = 1.90, p < 0.001) and be charged with DUI (IRR = 2.69, p = 0.035) in the past year. Pairwise comparisons indicated that the Dual Chronic class had higher levels of past-year reckless driving and DUI of alcohol or drugs than the Persistent AOD/Adolescent ASB class (ps < 0.001). The Decreasing Drugs/Persistent ASB class had higher levels of past-year reckless driving than the Persistent AOD/Adolescent ASB class (p < 0.001). The Increasing AOD/Persistent ASB class had higher levels of past-year DUI of alcohol or drugs than the Persistent AOD/Adolescent ASB class (p < 0.001).
Figure 1.
Incidence rate ratios of past-year risky driving behaviors by trajectory class membership
Note. Analyses were adjusted for age, sex, and race/ethnicity. The relatively resolved trajectory class was set as the referent class. The error bars indicate the 95% confidence intervals for comparisons between trajectory classes 1–4 with the referent class. Additional pairwise comparisons are not illustrated in these figures.
3.3.2. Sexual Risk Behaviors, STI, and Injection Drug Use
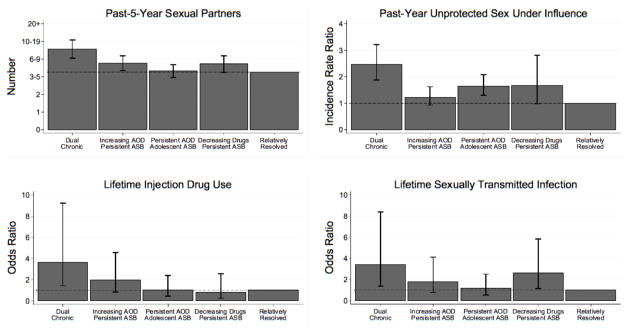
As shown in Figure 2, both the Dual Chronic and the Increasing AOD/Persistent ASB classes were more likely than the Relatively Resolved class to report more sexual partners in the past five years. The Dual Chronic and the Persistent AOD/Adolescent ASB classes were more likely than the Relatively Resolved class to report unprotected sex under the influence (IRRs = 2.41 and 1.63, ps < 0.001). Compared to the Relatively Resolved class, the Dual Chronic class was over three times more likely to have had a lifetime STI (OR = 3.40, p = 0.008) and lifetime injection drug use (OR = 3.62, p = 0.007). The Decreasing Drugs/Persistent ASB class was also more likely than the Relatively Resolved class to report any lifetime STI (OR = 2.60, p = 0.02). Pairwise comparisons indicated that the Dual Chronic class had significantly more sexual partners in the past five years than all other trajectory classes (p < 0.001). With the adjusted alpha level for pairwise comparisons, the difference between the Dual Chronic and the Increasing AOD/Persistent ASB classes in unprotected sex under the influence approached, but did not reach statistical significance (p < 0.012).
Figure 2.
Mean, incidence rate ratio, and odds ratios of sexual risk behaviors by trajectory class membership
Note. Analyses were adjusted for age, sex, and race/ethnicity. The relatively resolved trajectory class was set as the referent class. The error bars indicate the 95% confidence intervals for comparisons between trajectory classes 1–4 with the referent class. Additional pairwise comparisons are not illustrated in these figures.
4. DISCUSSION
In a highly affected sample of adolescents followed into young adulthood, persistent co-occurring substance use and antisocial behavior was strongly associated with elevations in risky behaviors. The Dual Chronic class reported the highest level of all seven risky behaviors, providing support for our first hypothesis. The consistency and magnitude of these associations are noteworthy. For five of the seven risky driving and sexual behaviors, the Dual Chronic class was three or more times as likely than the Relatively Resolved class to have engaged in the behaviors. These findings are important because they indicate that young adults with a profile of chronic high levels of comorbid substance use and antisocial behavior are likely to engage in multiple high risk behaviors that put themselves and others in danger and are very costly to society.
Trajectory classes that had either persistent substance use or persistent antisocial behavior alone were not consistently associated with risky behaviors, with patterns varying by severity (e.g., reckless driving vs. DUI charges) and type (e.g., risky driving vs. sexual risk behavior) of risky behavior. Evidence for differential associations was most noticeable for past-year reckless driving, reported DUI of alcohol or drugs, and unprotected sex under the influence. Specifically, past-year reckless driving and reported DUI of alcohol or drugs were elevated in trajectory classes characterized by persistent ASB, whereas unprotected sex under the influence was elevated in the Persistent AOD/Adolescent ASB trajectory class. It is possible that there were more significant differential associations for these less severe outcomes because they have relatively higher base rates and are therefore more sensitive to statistical prediction. Alternatively, endorsement of more severe risky behaviors may reflect a common underlying pathway to multiple externalizing problems. As such, persistent substance use or persistent antisocial behavior alone may only be associated with the less severe and more frequently endorsed risky behaviors, whereas persistent co-occurrence of substance use and antisocial behavior was uniquely associated with the more severe and less frequently endorsed outcome of lifetime injection drug use.
Largely consistent with our second hypothesis, three out of four risky behaviors that are directly influenced by alcohol or drug use (past-year reported DUI, DUI charge, and unprotected sex under the influence) were elevated among the trajectory class with persistent substance use and adolescent-limited antisocial behavior. Inconsistent with our third hypothesis, persistent antisocial behavior alone also had clear associations with substance use related risky behaviors, with the Decreasing Drugs/Persistent ASB class being at least equal or more elevated than the Persistent AOD/Adolescent ASB class. Prior studies suggest a more robust positive link between substance use and risky driving than between ASPD and risky driving (Bingham and Shope, 2004; Lapham et al., 2001, 2006; Li et al., 2013). In the current study, we found that risky driving behaviors are also linked to persistent antisocial behaviors. These findings may reflect common etiological pathways to antisocial and risky driving behaviors such as low levels of conscientiousness or high levels of sensation seeking (Arnett, 1996; Bogg and Roberts, 2004; Krueger et al., 2002).
It is also important to note that, as a whole, the current sample had higher rates of risky behaviors than similar estimates from nationally representative data. Nearly 48% of the participants in this study reported DUI at least once in the past year, compared to about 20–23% among U.S. young adults aged 18–25 years (Park et al., 2014; Substance Abuse and Mental Health Services Administration, 2014). Over 10% of the participants reported lifetime injection drug use, whereas the lifetime prevalence of injection drug use was estimated to be 2.6% in the U.S. population aged 13 years or older (Lansky et al., 2014). The high rates of risky behaviors may be partially accounted for by an over-representation of males compared to females in the current sample. Further longitudinal follow-up of this severely affected sample provides a unique opportunity to examine extremely risky behaviors that are of low base rate in community samples. Current ongoing assessment of these participants into later adulthood will allow us to continue to differentially predict characteristics of those who decrease or desist problematic substance use and associated high-risk behaviors as well as those who persist with serious and costly behaviors.
This study has several limitations. Measurement of risky behaviors relied on retrospective self-report which may be prone to recall or report bias. For example, although meta-analytic data support test-retest reliability of self-report of sexual risk behaviors for recall periods of 1, 3, and 6 months (Napper et al., 2010), participants may have difficulty reporting number of sexual partners in the past five years. Because there were no comparable baseline measures for most non-substance use risky behaviors examined in this study, baseline risky behaviors were not controlled for and the direction of causality cannot be determined. Specifically, we cannot determine whether significant results reflect pre-existing differences, or if they are directly attributable to the shifts in substance use and/or antisocial behaviors that distinguished the trajectory classes. For the risky driving analyses, access to a vehicle and frequency of driving in the past year were not measured. Therefore, we cannot rule out the possibility that some participants did not engage in risk driving behaviors because they had fewer opportunities to drive. Due to skip patterns for two sexual risk behavior questions, past-year unprotected sex under the influence and lifetime STI may be overestimated. Finally, the demographics of this high-risk sample are not comparable to those in the general population due to recruitment biases (e.g., males are over-represented), which limits the generalizability of findings.
Despite these limitations, this set of novel analyses has important public health implications. Individuals with co-occurring and persistent substance use and antisocial behaviors represent a high-risk segment of the population who are costly to society. Our findings highlight the need for tailored interventions not only for substance use and antisocial behaviors, but also for risky driving and STI/HIV prevention. Intervention efforts targeting this group will likely yield the greatest public health impact because it will not only reduce individual burden attributable to substance use and antisocial behaviors, but also mitigate societal burden related to motor vehicle crashes and transmission of STI/HIV. Future research could examine casual and mechanistic links between externalizing psychopathology and risky driving and sexual behaviors, which can inform developmentally optimized interventions. Developing cost-effective methods and policies that move youth from high-risk developmental trajectories to resolution of these behaviors remains an important priority in adolescent health research.
Highlights.
Participants in this unique sample reported notably high rates of risky behaviors.
The Dual Chronic class exhibited the highest rates of all seven risky behaviors.
Persistent antisocial behavior was linked to reckless driving and DUI.
Persistent substance use was linked to DUI, DUI charge, and unprotected sex.
Differential associations highlight the need for targeted interventions.
Acknowledgments
Role of Funding Source
This research was supported by National Institute of Drug Abuse grants R01 DA035804 (PIs: Hopfer, Stallings, & Wall), R01 DA021905 (PIs: Brown & Wall), R01 DA012845 (PI: Hewitt), F31 DA030861 (PI: Worley), P60 DA011015 (PI: Hewitt), R01 DA021913 (PI: Hopfer), R01 DA015522 (PI: Hopfer), and National Institute on Alcohol Abuse and Alcoholism (NIAAA) grants R37 AA07033 (PI: Brown) and T32 AA013525 (PI: Riley). This work was also supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content of this manuscript is solely the responsibility of the authors. The sponsoring agencies had no role in the design, analyses, or writing of this paper, or the decision to submit this paper for publication.
Footnotes
Conflict of Interest
The authors have no conflict of interest to declare.
Contributors
Jeremy Luk, Matthew Worley, Ryan Trim, Sandra Brown, and Tamara Wall conceptualized and designed the study. Jeremy Luk initiated this paper, ran preliminary data analyses, and wrote the first draft of this article. Matthew Worley completed final data analyses and provided detailed edits to an earlier draft. Evan Winiger assisted with literature review and the writing of the introduction. Christian Hopfer, John Hewitt, Sandra Brown, and Tamara Wall obtained funding and acquired the data. All authors have contributed substantially to the preparation of this article and approved the final submitted version.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adalbjarnardottir S, Rafnsson F. Adolescent antisocial behavior and substance use. Addict Behav. 2002;27:227–240. doi: 10.1016/s0306-4603(00)00179-9. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Sensation seeking, aggressiveness, and adolescent reckless behavior. Pers Individ Dif. 1996;20:693–702. [Google Scholar]
- Beauchaine TP, McNulty T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Dev Psychopathol. 2013;25:1505–1528. doi: 10.1017/S0954579413000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham CR, Shope JT. Adolescent problem behavior and problem driving in young adulthood. J Adolesc Res. 2004;19:205–223. [Google Scholar]
- Blincoe LJ, Seay A, Zaloshnja E, Miller T, Romano E, Luchter S, Spicer R. The economic impact of motor vehicle crashes, 2000. Washington, DC: US Department of Transportation, National Highway Traffic Safety Administration; 2002. [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A Meta-Analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Dev Psychol. 2012;48:1429–1442. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M, Clark S, Owen LD. Heterosexual risk behaviors in at-risk young men from early adolescence to young adulthood: Prevalence, prediction, and association with STD contraction. Dev Psychol. 2002;38:394–406. doi: 10.1037//0012-1649.38.3.394. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed March 8, 2016];Excessive drinking costs US $223.5 Billion Website. 2014 http://www.cdc.gov/features/alcoholconsumption/
- Chesson HW, Blandford JM, Gift TL, Tao G, Irwin KL. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspect Sex Reprod Health. 2004;36:11–19. doi: 10.1363/psrh.36.11.04. [DOI] [PubMed] [Google Scholar]
- Cohen MA, Piquero AR. New evidence on the monetary value of saving a high risk youth. J Quant Criminol. 2008;25:25–49. [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality Syndromes and alcohol and specific drug use disorders in the United States. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, Ehlers KM, Whitmore EA, MacDonald MJ. Validity of structured clinical evaluations in adolescents with conduct and substance problems. J Am Acad Child Adolesc Psychiatry. 2001;40:265–273. doi: 10.1097/00004583-200103000-00005. [DOI] [PubMed] [Google Scholar]
- Derringer J, Corley R, Haberstick BC, et al. Genome-wide association study of behavioral disinhibition in a selected adolescent sample. Behav Genet. 2015;45:375–381. doi: 10.1007/s10519-015-9705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health. 2002;31:354–362. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- Helzer JE. The predictive validity of lay diagnostic interview schedule diagnoses in the general population. Arch Gen Psychiatry. 1987;44:1069–1077. doi: 10.1001/archpsyc.1987.01800240045007. [DOI] [PubMed] [Google Scholar]
- Khan MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infection in the United States: Assessment of differences by race. Am J Public Health. 2012;102:867–876. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. J Abnorm Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. J Abnorm Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansky A, Finlayson T, Johnson C, et al. Estimating the number of persons who inject drugs in the United States by Meta-Analysis to calculate national rates of HIV and hepatitis C virus infections. PLoS ONE. 2014;9:e97596. doi: 10.1371/journal.pone.0097596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapham SC, Baca JC, Mcmillan GP, Lapidus J. Psychiatric disorders in a sample of repeat impaired-driving offenders. J Stud Alcohol. 2006;67:707–713. doi: 10.15288/jsa.2006.67.707. [DOI] [PubMed] [Google Scholar]
- Lapham SC, Smith E, C’de Baca J, et al. Prevalence of psychiatric disorders among persons convicted of driving while impaired. Arch Gen Psychiatry. 2001;58:943–949. doi: 10.1001/archpsyc.58.10.943. [DOI] [PubMed] [Google Scholar]
- Lavan H, Johnson JG. The association between axis I and II psychiatric symptoms and high-risk sexual behavior during adolescence. J Pers Disord. 2002;16:73–94. doi: 10.1521/pedi.16.1.73.22559. [DOI] [PubMed] [Google Scholar]
- Li K, Simons-Morton BG, Hingson R. Impaired-driving prevalence among US high school students: Associations with substance use and risky driving behaviors. Am J Public Health. 2013;103:e71–e77. doi: 10.2105/AJPH.2013.301296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitch JE, Kosterman R, McCarty CA, Herrenkohl TI, Hawkins DJ. Growth in adolescent delinquency and alcohol use in relation to young adult crime, alcohol use disorders, and risky sex: A comparison of youth from low- versus middle-income backgrounds. J Child Psychol Psychiatry. 2010;51:1377–1385. doi: 10.1111/j.1469-7610.2010.02292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- Melroy WE, Stephens SH, Sakai J, et al. Examination of genetic variation in GABRA2 with conduct disorder and alcohol abuse and dependence in a longitudinal study. Behav Genet. 2014;44:356–367. doi: 10.1007/s10519-014-9653-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS Behav. 2010;14:152–161. doi: 10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Statistics and Analysis. 2014 Crash Data Key Findings. Washington, DC: National Highway Traffic Safety Administration; 2015. (Traffic Safety Facts Crash•Stats. Report No. DOT HS 812-219) [Google Scholar]
- National Drug Intelligence Center. National Drug Threat Assessment. Washington, DC: United States Department of Justice; 2011. [Google Scholar]
- Newbern EC, Anschuetz GL, Eberhart MG, et al. Adolescent sexually transmitted infections and risk for subsequent HIV. Am J Public Health. 2013;103:1874–1881. doi: 10.2105/AJPH.2013.301463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MJ, Scott JT, Adams SH, Brindis CD, Irwin CE. Adolescent and young adult health in the United States in the past decade: Little improvement and young adults remain worse off than adolescents. J Adolesc Health. 2014;55:3–16. doi: 10.1016/j.jadohealth.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Ritchwood TD, Ford H, DeCoster J, Sutton M, Lochman JE. Risky sexual behavior and substance use among adolescents: A meta-analysis. Child Youth Serv Rev. 2015;52:74–88. doi: 10.1016/j.childyouth.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Schwab-Stone M, Fisher P, et al. The diagnostic interview schedule for children-revised version (DISC-R): I. Preparation, field testing, Interrater reliability, and acceptability. J Am Acad Child Adolesc Psychiatry. 1993;32:643–650. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. [Google Scholar]
- Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent substance use and sexual risk-taking behavior. J Adolesc Health. 2001;28:181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- Trim RS, Worley MJ, Wall TL, et al. Bivariate trajectories of substance use and antisocial behavior: Associations with emerging adult outcomes in a high-risk sample. Emerging Adulthood. 2015;3:265–276. doi: 10.1177/2167696815573791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valois RF, Oeltmann JE, Waller J, Hussey JR. Relationship between number of sexual intercourse partners and selected health risk behaviors among public high school adolescents. J Adolesc Health. 1999;25:328–335. doi: 10.1016/s1054-139x(99)00051-8. [DOI] [PubMed] [Google Scholar]
- Vassallo S, Smart D, Sanson A, et al. Risky driving among young Australian drivers II: Co-occurrence with other problem behaviours. Accid Anal Prev. 2008;40:376–386. doi: 10.1016/j.aap.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Define RS, DeLisi M, et al. Sociodemographic, behavioral, and substance use correlates of reckless driving in the United States: Findings from a national sample. J Psychiatr Res. 2011;45:347–353. doi: 10.1016/j.jpsychires.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]