Abstract
[Purpose] This study was conducted to clarify the difference in therapeutic effects between traction and decompression therapies, and their clinical therapeutic significance. [Subjects and Methods] The subjects were 31 patients aged 35 to 50 years who had unilateral or bilateral lumbar and radicular leg pain. An intervention program was implemented in 31 patients with lumbar herniated intervertebral disks. For the experimental group, 15 subjects were randomly selected to receive decompression therapy and trunk stabilization exercise. For the control group, 16 subjects were randomly selected to receive traction therapy and trunk stabilization exercise. [Results] Activities of the rectus abdominis, transverse abdominis, and external oblique muscles increased significantly in both groups. However, the activity of the erector spine muscle decreased, which was the only significant change in muscle activity among those of the other muscles in both groups. The disk herniation index in the experimental group decreased significantly in comparison with that in the control group, and the difference in the change in disk herniation index between the groups was significant. [Conclusion] Decompression therapy was demonstrated to be more effective clinically than conventional traction therapy as an intervention method for disk disease.
Keywords: Decompression therapy, Herniated intervertebral disk, MRI
INTRODUCTION
Human beings walk upright and maintain their postures with a narrow base of support and with the center of gravity of the upper trunk. Even if muscle tension slightly loosens, low back pain occurs because of stress from the mechanical posture of the muscle involved1). This causative factor of low back pain can lead to problems in sense and timing of muscle contraction awareness, sense of heaviness, acting force, and acting load force2). Of the cases of low back pain syndrome, 80% are related to the lumbar disk; and herniation of disk material is known as a secondary inflammatory response to stimulation of the dorsal root ganglion and nerve root is known as the cause of low back pain. The remaining 20% of cases are directly related to posterior elements such as lumbar facet joint, ligament, lamina of the vertebral arch, and fascia. In addition, the action of the local muscles attached directly to the spine plays an important role in maintaining spinal segmental stability3) and providing trunk stability generally4). In particular, lumbar disk herniation causes herniation of part or all of the nucleus pulposus by rupture of the mid, internal, or lateral fiber of the annulus fibrosus through an external force or lumbar disk degeneration. It is a disease that induces neurological signs such as hypoesthesia, muscle weakness, and radiating pain in the constricted innervation area, with back pain in the local part by pressing the dura mater or nerve root. Therefore, management of these neurological signs is important5). Generally, thermotherapy and electrotherapy have been used in physical therapy as interventions for low back pain syndrome. In addition, application of surface heat such as a hot pack and infrared light, and deep heat such as ultrasonography, short waves, and microwaves has been used in thermotherapy6). Spinal stabilization exercise is another widely used intervention method that improves muscle strength and trunk endurance, and stabilizes nervous system control of muscles and muscle coordination. This exercise focuses on muscle reconditioning for spinal stabilization7). Therapeutic methods for herniated intervertebral disks are divided into conservative and operational therapies. Excluding 5% of patients, most undergo conservative therapy but anti-inflammatory drugs, joint mobilization, acupuncture, traction, and so on are being used as interventions to recover degenerative disks and improve neurological symptoms8). Among these interventions, traction therapy is essential in clinical therapy, but its effect is not clear and differences in viewpoints at home and abroad are evident9). Recently, spinal decompression therapy is being performed to improve the limitations of traction therapy, as it does not have to set a direction and traction force unlike traction therapy. Adjusting the angle and direction of the traction force by adjusting the position of the disk by using a computer program has an advantage6). Therefore, this study measured disk height after decompression therapy and measured the activities of muscles that provide overall trunk stability by overcoming the gravity applied to the body. These muscles are not directly attached to the spine. In addition, we aimed to clarify the difference between the therapeutic effect of traction therapy and that of decompression therapy, and their clinical therapeutic significance by comparing low back pain disability index between the two intervention groups.
SUBJECTS AND METHODS
This study was approved by the bioethics committee (institutional review board) of Sehan University Center (approval No. 2015-17) in February 2016. The subjects were 31 patients aged 35 to 50 years who had unilateral or bilateral lumbar and radicular leg pains, who attended a medical institution located in Jeollanamdo, South Korea, between February 4, 2016, and April 3, 2016, for 2 months. They showed more than one bulging of the intervertebral disks on magnetic resonance imaging MRI, had had the onset of illness for less than 6 months, and did not receive spinal depression therapy. In addition, their complaint of pain matched the neurological symptoms, and their mean score in the Oswestry Disability Index (ODI)—Korean version questionnaire was >30 points (Table 1).
Table 1. Characteristics of the study subjects.
| Items | Experimental group (n=15) | Control group (n=16) |
|---|---|---|
| Age (years) | 42.5 ± 6.3 | 45.2 ± 7.3 |
| Height (cm) | 167.1 ± 4.7 | 168.3 ± 3.9 |
| Weight (kg) | 61.7 ± 6.8 | 65.4 ± 7.1 |
| ODI (point) | 34.4 ± 3.9 | 35.3 ± 4.7 |
| Gender (male/female) | 8/7 | 7/9 |
Data are presented as mean ± SD, obtained by using the Shapiro-Wilk test. ODI: Oswestry Disability Index
In this study, an intervention program was conducted in 31 patients with lumbar herniated intervertebral disks. Fifteen subjects were randomly selected for the experimental group and received decompression therapy and trunk stabilization exercise. Sixteen subjects were randomly selected for the control group and received traction therapy and trunk stabilization exercise. These intervention programs were conducted for 3 weeks, and the disk heights at L4 and L5 were measured by using MRI. Moreover, trunk muscle activities were measured by using surface electromyography (sEMG), and the lumbar pain disability index was calculated by using the ODI and then analyzed and compared between the groups. The participants understood the purpose of this study very well and agreed to participate in this study voluntarily by providing written informed consent.
Vertebral height and disk herniation index were determined by using MRI (Signa HDe 1.5 T, GE Corporate, USA). Disk height was analyzed by using T2-weighted axial-section MRI, and the images were analyzed by using the PACS (picture archiving and communication system). The subject lay supine, and then the researcher put a cushion under the subject’s knee and had the subject bend the knee at a 25° angle. In this position, the lumbar vertebral L4 and L5 segments were photographed. Disk height was analyzed by using the image obtained (Fig. 1).
Fig. 1.
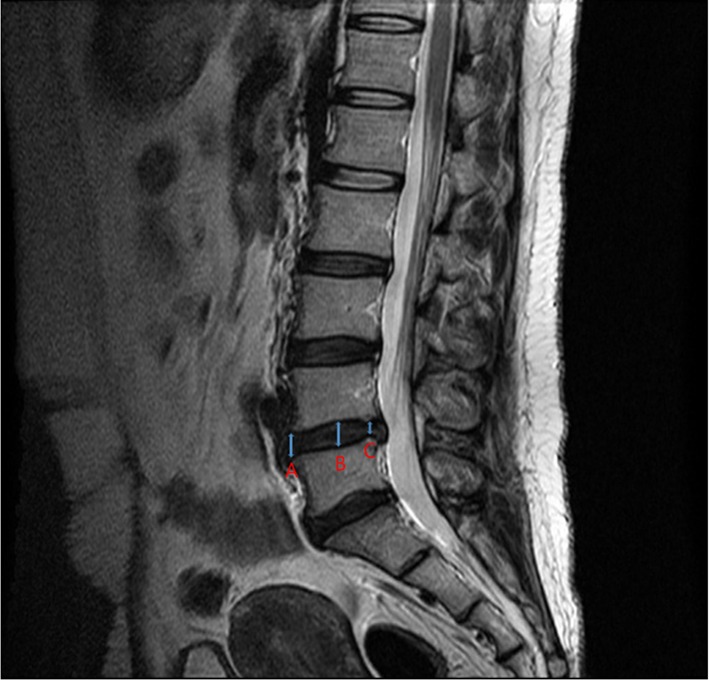
Measurement of lumber disk height. A: anterior disk height, B: middle disk height, C: posterior disk height. Disk height: (A + B + C)/3 (mm)
Disk herniation index measurement: The disk and intervertebral foramen were measured at intercept of the axial direction. The sagittal distance of the herniated disk was recorded as the maximum anteroposterior disk height (AB), and that of the vertebral foramen was recorded as the maximum anteroposterior canal length (EF). The width of the herniated material was measured by drawing a line at the mid level of the maximum anteroposterior disk length (CD). The width of the spinal canal was calculated at the same level (GH). The formula used for calculating the disk herniation index was ([AB ×CD]/[EF ×GH]) ×1,000 (Fig. 2)10, 11).
Fig. 2.
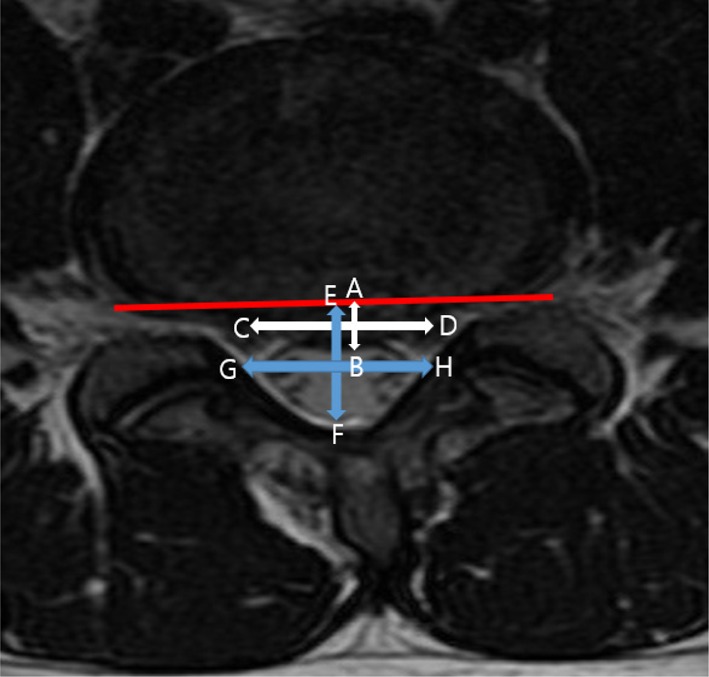
Measurement of the lumber disk herniation index. AB: maximum anteroposterior disk height, CD: width of the herniated material at the level of the mid AB distance, EF: maximum anteroposterior canal length, GH: width of the spinal canal at the level of the mid AB distance. The herniation index is calculated as ([AB ×CD]/[EF ×GH]) ×1,000
The four-channel sEMG system MP 100 (Biopac, USA) was used to measure the activities of the trunk muscles, and the sampling rate for collecting EMG signals was set at 1,000 Hz. A frequency band-pass filter was set at 20–450 Hz. The subjects’ skin was cleaned by removing hair, and dead skin cells were removed by using thin sandpaper to minimize skin resistance to the EMG signals. Then, the skin was rubbed with alcohol cotton and kept clean. Two Ag/Agcl surface electrodes were attached to the belly of each muscle in a direction parallel to the muscular fiber at 2-cm intervals. Standard electrodes were attached to the spinous process of the 12th thoracic vertebrae and scapula spine, which are the protruding parts. The EMG signals from the right rectus abdominis, transverse abdominis, external oblique abdominis, and erector spine muscles were collected. The sampling rate for EMG signal collection was set at 1,000 Hz, and the notch filter was set at 60 Hz. The band pass filter was set at 20–450 Hz. Signals from the measured muscles were converted to root mean square (RMS), and EMG signal analysis was performed by using the Acqknowledge 3.9.1 software program (Biopac). EMG data of the rectus abdominis, transverse abdominis, and external oblique abdominis muscles were collected while the subject was touching the knees with both hands in supine position for 5 seconds. For the measurement at the erector spine muscle, the subjects lay in a prone position and flexed both arms maximally and then extended their trunks maximally for 5 seconds. The EMG signal produced while performing this movement was set as a particular action, and the EMG signal while standing motionless for 5 seconds was set as the standard action. It was regarded as the reference voluntary contraction (RVC), and the %RVC method standardized based on RVC was used. Patients who complained of pain and difficulty in performing movement were excluded from this experiment.
The ODI was measured by using the Korean version of the ODI questionnaire to quantify physical difficulty in daily life due to lumbar pain. It is composed of 10 items, and each item was evaluated on a scale of 0–5 points. In this questionnaire, the higher the score, the more severe the disability. In the Korean version, in consideration of the Korean culture, the item about sexual life is excluded. Thus, it consists of 9 items; and each item was evaluated with a score from 0 to 5, and the highest possible total score was 45 points. The total score was divided by the number of items ×5 and was converted into a percentage12).
The trunk stability exercise described by Lee et al.13, 14) was used as spinal and pelvic stabilization exercise. It is composed of step 1 (awareness stage), step 2 (associative stage), and step 3 (exercise task stage) based on the research of Ok stage)15). The exercise method was performed for 30 minutes per session, four times a week, for 3 weeks and was applied step by step in subjects considering their exercise ability (Table 2).
Table 2. Intervention program for trunk muscle stabilization.
| Stage | Time | Contents | Program | |
|---|---|---|---|---|
| Warm-up exercise | 5 min | Whole-body flexibility exercise | Upper and lower extremity stretching and joint moving exercises | |
| Main exercise | 20 min | Trunk muscle stabilization exercise | 1. Pelvic posterior tilting in the supine position with flexion of both knees | |
| Stage 1 | 2. Abdominal draw-in in the supine position with flexion of both knees | |||
| 3. Pelvic anterior tilting in the supine position with extension of both knees | ||||
| 4. Abdominal draw-in in the supine position with extension of both knees | ||||
| Stage 2 | 5. Bridging in the supine position | |||
| 6. Ball bridge | ||||
| Stage 3 | 7. Unstable bridging: bridging with extension of the left/right leg | |||
| Cooling-down exercise | 5 min | Breathing and aerobic exercises | Breathing with the abdominalis muscle | |
The automatic electric traction equipment Rehatrac RC-100 (Sakai, Japan) was used for traction therapy. The duration of traction was 15 minutes, and the ratios of hold and rest times were 2:1 and 60:30 sec, respectively. The traction force for resting time was set to half of the traction force used in hold time. Traction force was started at one fourth of each weight and gradually increased in each session until the subjects did not feel uncomfortable. In the last week, the standard of the maximum traction force was half of the subjectsthweights. The pelvis was fixed with a pelvic stabilization belt, and the thorax was fixed with a thorax stabilization belt.
Spinal decompression therapy was performed by using a lumbar decompression device MAX-D (Medirex, Korea), and the subjects lay on a traction table in the supine position. Their knees were naturally positioned in a 90° angle on the knee support fixture installed in the device. The ankle was fixed with a hydraulic device according to the subject’s body type. Traction force and movement of the low extremity were supposed to be delivered through the fixed ankle. The upper extremity was fixed by using a trunk stabilization belt and an air pumping apparatus to maintain lumbar lordosis. A pelvic tilt of 15° was applied for patients with a lumbar herniated intervertebral disk at the L4 and L5 levels. The subjects were comfortably positioned in the device; then, their lower limbs were pulled within range so as not to make them feel uncomfortable during steps 1 to 5 of delivering traction force through the hydraulic device. The subject’s upper extremities were pulled within range so as not to make them feel uncomfortable during steps 1 to 5, using a trunk stabilization belt. First, the multi-mode of an automatic program of a decompression therapy device was used for steps 1 to 5. This multi-mode was programmed to make the lower part move in multiple directions. Traction force was started at one fourth of the subjects weight and increased by 2 kg at a steady rate daily. When pain occurred according to the increase in traction force, the traction force was lowered or maintained. The duration of the traction therapy was 30 min. The ratios of hold and rest times were 2:1 and 60:30 sec, respectively. The traction force for rest time was set to half of the traction force used in hold time. Both the traction and decompression therapy groups received their respective therapies once a day and five times a week for the first week and then once a day, four times a week (total 8 times) for the next 2 weeks.
Data analysis was performed by using SPSS 18.0 for Windows. The normality of the general characteristics of the subjects, and the respiratory muscle and physical activities of both groups were tested by using the Shapiro-Wilk test. Paired t-test was used to compare changes within the groups. Analysis of covariance was used to compare changes between the groups. The significance level was set at α=0.05.
RESULTS
No special variables related to the general characteristics of the subjects were found between the groups, thus indicating normality (Table 1). The activities of the rectus abdominis, transverse abdominis, and external oblique muscles increased significantly in both the experimental and control groups (p<0.05). The activity of the erector spinal muscle decreased significantly in comparison with the changes in both groups (p<0.05 and p<0.01, respectively; Table 3). This was the only significant difference between the groups (p<0.05; Table 3). The disk herniation index in the experimental group decreased significantly (p<0.01) in comparison with the changes in both groups. The difference in the changes in disk herniation index between the groups was significant (p<0.05; Table 3).
Table 3. Comparison of changes in muscle activity and disk height within and between the experimental and control groups.
| Group | Pre | Post# | |||
|---|---|---|---|---|---|
| %RVC | RA | Experimental group | 50.8 ± 4.7a | 54.1 ± 3.2* | |
| Control group | 51.2 ± 5.1 | 53.8 ± 5.2* | |||
| TA | Experimental group | 47.1 ± 3.6 | 49.7 ± 4.1* | ||
| Control group | 45.9 ± 3.7 | 48.7 ± 4.9* | |||
| EAO | Experimental group | 45.3 ± 2.2 | 47.5 ± 2.4* | ||
| Control group | 45.7 ± 3.2 | 48.1 ± 2.1* | |||
| ES | Experimental group | 59.4 ± 5.2 | 53 ± 5.4** | * | |
| Control group | 55.1 ± 4.8 | 52.7 ± 5.2* | |||
| Disk Height (mm) | Experimental group | 7.1 ± 2.7 | 7.3 ± 1.9 | ||
| Control group | 6.8 ± 2.3 | 6.8 ± 1.7 | |||
| Disk Herniation Index | Experimental group | 284 ± 12.3 | 198 ± 22.6** | ||
| Control group | 264 ± 9.5 | 248 ± 16.3 | * | ||
*p<0.05, **p<0.01. Data are presented as mean ± SD. #Paired t-test, analysis of covariance. RA: rectus abdominis muscle, TA: transverse abdominis muscle, EAO: external abdominal oblique muscle, ES: erector spine muscle
DISCUSSION
In this study, 31 patients with lumbar herniated intervertebral disk were randomly assigned to receive either trunk stabilization exercise and decompression therapy or traction therapy and trunk stabilization exercise. The intervention program was conducted for 3 weeks. The disk heights of the L4 and L5 segments were measured before and after the intervention by using MRI. In addition, trunk muscle activities were measured by using sEMG, and lumbar pain disability index was calculated by using the ODI questionnaire and then analyzed and compared between the groups. The discussion that follows is based on these results.
Guehring et al.16) reported that while decompression by distraction in an animal model with degenerative disk was conducted for 28 days, the detection rate of degenerative change on MRI decreased, gene expression levels of disk matrix components increased, and the nucleus pulposus was regenerated. Formation of the structural material of the matrix increases with the increase in hydrostatic pressure through decompression, moisture content increases through the improvement in the combining ability with moisture, and nutrition supply can be expected to increase owing to the improvement of degenerative change. Apfel et al.17) insisted that 30 patients with discogenic low back pain or disk herniation received treatment by using decompression therapy equipment for 6 weeks and conducted a cohort study that compared disk heights by using CT. Disk height increased significantly, and pain decreased. They insisted that disk height can be recovered based on their results. Kwon et al.11) performed acupuncture, cupping therapy, medicine treatment, and decompression therapy in six patients with disk disease. They reported significant differences in disk height and disk herniation index, and positive changes as results of their research. Moreover, Park and Kim18) compared disk herniation index and disk height by using MRI after applying traction and decompression therapies in 60 patients. As a result, they observed a significant difference in disk herniation index but no significant difference in disk height. This study supported the results of advanced studies because no significant difference in disk height was found in both groups, but a significant difference in disk herniation index was found in the decompression therapy group. Various factors cause the discrepant results between the present study and the advanced study, such as disk disease duration and activities of daily living. In particular, the reasons for having no difference in disk height could be that the patients were exposed to gravity in daily living and that treatment periods differed between the two studies. However, a significant difference in disk herniation index was found between the two groups. This verified the effect of decompression treatment on disk herniation index. The cause can be inferred from the research of Macario et al19). Only disk separation was discussed as the mechanism that explains the effectiveness of conventional traction therapy, and the effectiveness of automatic traction therapy for patients with chronic discogenic back pain in relation to spine decompression remains unclear. By comparison, Kwon et al.11) suggested that decompression therapy supplemented the limitation of traction therapy and had a great advantage of inducing physical change to the disk. It is known that it can measure load applied to the spine by using an electronic control system and allows delivery of traction force to the spine because based on the result, muscle tone did not occur by controlling the speed of traction therapy. In terms of muscle activity, the activity of the erector spine muscle in the decompression therapy group decreased significantly. Inflammation, pain caused by the inflammation, and neurological manifestations were observed in the paraspinal muscles as symptoms of disk disease. Inflammatory reaction of the spine surroundings made the paraspinal muscles hypertonus. Increased intervertebral foramen diameter by decompression can induce an increase in blood flow in the blood vessel within the foramen and intervertebral foramen, and increased blood flow can lead to decreased muscle tension and pain by removing inflammatory exudation20). Based on these results, the paraspinal muscles were verified to have a positive response to trunk stabilization exercise after decompression therapy, it is considered more effective clinically than conventional traction therapy as intervention method for patients with disk disease.
This study was conducted at only one medical institution. Normalizing the general characteristics of the study subjects was difficult because the study period was short and the subjects’ daily lives were not properly controlled. However, decompression therapy can be considered a more effective intervention method for patients with disk disease in the light of disk height and disk herniation index, change in muscle activity, and many advanced research studies. Prospective research on this intervention with adjustment of the study and disease periods will be needed in the future.
Acknowledgments
This paper was supported by the Sehan University Research Fund in 2016.
REFERENCES
- 1.Al-Obaidi SM, Al-Zoabi B, Al-Shuwaie N, et al. : The influence of pain and pain-related fear and disability beliefs on walking velocity in chronic low back pain. Int J Rehabil Res, 2003, 26: 101–108. [DOI] [PubMed] [Google Scholar]
- 2.Comerford MJ, Mottram SL: Movement and stability dysfunction—contemporary developments. Man Ther, 2001, 6: 15–26. [DOI] [PubMed] [Google Scholar]
- 3.Norris CM: Spinal stabilisation: 5. An exercise programme to enhance lumbar stabilisation. Physiotherapy, 1995, 81: 138–146. [Google Scholar]
- 4.Park JC, Han JM, Kim YS, et al. : The effects of stabilization exercise on muscle performance according to bearing surface. J Korean Acad Clin Electrophysiol, 2012, 10: 39–44. [Google Scholar]
- 5.Korean Acupuncture and Moxibustion Medicine Society Textbook Compilation Committee: The acupuncture, 1st ed. Paju: Jipmoondang, 2012, pp 250–251. [Google Scholar]
- 6.Ma SY: Effect of whole body cryotherapy with spinal decompression on lumbar disc herniation by functional assessment measures. J Korean Data & Information Sci Soc, 2010, 21: 101–1108. [Google Scholar]
- 7.Richardson CA, Hodges P, Hides JA: Therapeutic exercise for lumbopelvic stabilization: a motor control approach for the treatment and prevention of low back pain. Churchill Livingstone, 2004. [Google Scholar]
- 8.Gay RE, Bronfort G, Evans RL: Distraction manipulation of the lumbar spine: a review of the literature. J Manipulative Physiol Ther, 2005, 28: 266–273. [DOI] [PubMed] [Google Scholar]
- 9.Shin JH, Hwang SY, Lee YJ, et al. : Literature consideration on traction therapy and scoliosis in kyungkuen therapy. Korean J Acupunct, 2012, 29: 166–178. [Google Scholar]
- 10.Fagerlund MK, Thelander U, Friberg S: Size of lumbar disc hernias measured using computed tomography and related to sciatic symptoms. Acta Radiol, 1990, 31: 555–558. [PubMed] [Google Scholar]
- 11.Kwon WA, Lee SH, Lee JH: Effects of decompression therapy for 6 cases with lumbar herniated disc. JKAIS, 2012, 13: 2133–2141. [Google Scholar]
- 12.Kim ER, Kang MH, Kim YG, et al. : Effects of a home exercise program on the self-report disability index and gait parameters in patients with lumbar spinal stenosis. J Phys Ther Sci, 2014, 26: 305–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JY, Park JS, Lee DH, et al. : Effect of the trunk muscle stabilization training on balance for chronic stroke patients. JKAIS, 2012, 13: 1212–1219. [Google Scholar]
- 14.Kang JI, Jeong DK, Choi H: The effects of trunk stabilization exercise on bone density after menopause. J Phys Ther Sci, 2015, 27: 3869–3872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Sullivan PB: Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Man Ther, 2000, 5: 2–12. [DOI] [PubMed] [Google Scholar]
- 16.Guehring T, Omlor GW, Lorenz H, et al. : Disc distraction shows evidence of regenerative potential in degenerated intervertebral discs as evaluated by protein expression, magnetic resonance imaging, and messenger ribonucleic acid expression analysis. Spine, 2006, 31: 1658–1665. [DOI] [PubMed] [Google Scholar]
- 17.Apfel CC, Cakmakkaya OS, Martin W, et al. : Restoration of disk height through non-surgical spinal decompression is associated with decreased discogenic low back pain: a retrospective cohort study. BMC Musculoskelet Disord, 2010, 11: 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park JG, Kim DG: Effects of decompression therapy for the treatment of a herniated lumbar disc. Korean J Pain, 2008, 21: 143–149. [Google Scholar]
- 19.Macario A, Pergolizzi JV: Systematic literature review of spinal decompression via motorized traction for chronic discogenic low back pain. Pain Pract, 2006, 6: 171–178. [DOI] [PubMed] [Google Scholar]
- 20.Onel D, Tuzlaci M, Sari H, et al. : Computed tomographic investigation of the effect of traction on lumbar disc herniations. Spine, 1989, 14: 82–90. [DOI] [PubMed] [Google Scholar]


