Abstract
Endoscopic treatment for superficial non-ampullary duodenal tumors is technically difficult and challenging due to the anatomical characteristics of the duodenum. It is frequently complicated by procedural accidents, such as perforation. Surgical repair has long been the standard treatment for acute iatrogenic gastrointestinal perforation. However, endoscopic closure has recently emerged as an attractive alternative. In the patient presented herein, the over-the-scope-clipping system (OTSC system) was found to be useful for closing a duodenal perforation that had occurred during endoscopic submucosal dissection. For endoscopists who perform endoscopic treatment of the duodenum, endoscopic closure with the OTSC system is considered to be a technique that is necessary to master.
Keywords: endoscopic closure, endoscopic submucosal dissection, duodenal tumor, OTSC, over-the-scope-clipping system, perforation
Introduction
While superficial non-ampullary duodenal tumors are relatively rare, the frequency of their detection has recently increased due to the widespread use of endoscopy and continual improvements in endoscopic techniques (1,2). Although there are no established indications or treatments for superficial non-ampullary duodenal tumors (2,3), appropriate treatment is necessary for lesions that are histopathologically diagnosed to be high-grade dysplasia or which measure at least 20 mm in diameter, as these present a high risk of malignancy (2,4). Endoscopic treatment for superficial non-ampullary duodenal tumors is technically challenging because of the anatomical features of the duodenum and a high incidence of adverse events, such as perforation (2-5). For many years, surgical repair has been the standard treatment for iatrogenic gastrointestinal perforations. However, surgical procedures in the duodenum are relatively invasive, and they are also associated with significant morbidity and mortality. For these reasons, endoscopic closure of gastrointestinal perforation has recently been introduced as an attractive alternative (6-8).
The over-the-scope-clipping system (OTSC system, Ovesco Endoscopy AG, Tübingen, Germany) is an endoscopic device used to mechanically compress gastrointestinal tract tissue (9). The OTSC system is composed of an applicator cap with a mounted OTSC clip, a thread fitted to the OTSC clip to assist clip release, and a hand wheel for clip release. The applicator cap is attached to the tip of the endoscope. The OTSC clip is deployed by rotating the hand wheel to pull the thread connected to the OTSC clip. The OTSC Twin Grasper with two jaws, which can be separately opened as an assistive device to approximate tissue, is also available (10) (Fig. 1). The OTSC system has made the closure of gastrointestinal tract defects, such as perforations, anastomotic insufficiency, and fistula, as well as hemostasis in difficult-to-treat non-variceal bleeding, possible (6-10). It also helps to achieve a more reliable closure, as its wide mouth allows it to hold a greater amount of tissue than the conventional through-the-scope clip (TTSC) (8,10). We herein describe a patient in whom the OTSC system was useful for the treatment of a duodenal perforation caused by endoscopic submucosal dissection (ESD).
Figure 1.

OTSC system and OTSC Twin Grasper. The OTSC system is composed of an applicator cap with a mounted OTSC clip, a thread fitted to the OTSC clip to assist clip release, and a hand wheel for clip release. The OTSC Twin Grasper with two jaws, which can be separately opened as an assistive device to approximate tissue, is available (Reproduced with the permission of Ovesco Endoscopy AG, Tübingen, Germany).
Case Report
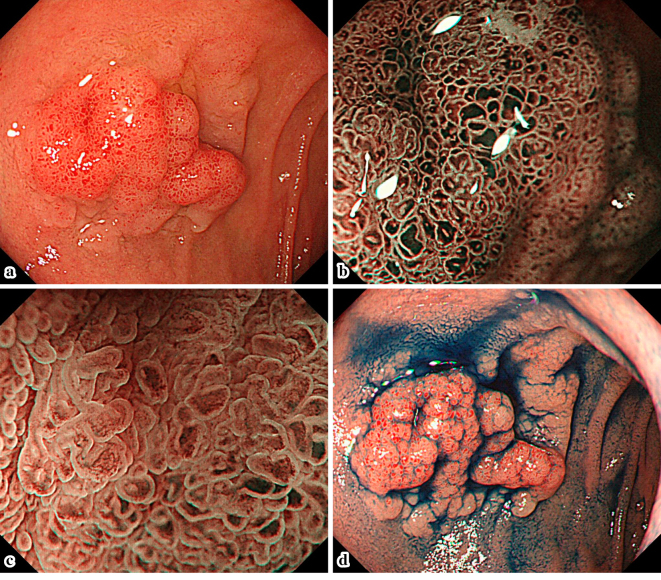
A 39-year-old male with no clinical history was referred to our hospital for close examination and treatment of a duodenal tumor detected by screening radiography of the stomach. On upper gastrointestinal endoscopy performed at our hospital, a reddened, sessile, elevated lesion measuring approximately 30 mm in diameter was detected in the anterior wall of the duodenal bulb, and a whitish lower elevated area spread around the lesion (Fig. 2a). Magnifying endoscopy with narrow-band imaging (OLYMPUS GIF TYPE H260Z, Olympus, Tokyo, Japan) revealed leaf-like villous structures of various sizes. The widths of the villi were greater than those in the surrounding normal areas (Fig. 2b and c). Chromoendoscopy with indigo carmine clearly showed the border of the lesion and the unevenness of its surface (Fig. 2d). On endoscopic ultrasonography, the lesion was found to be localized in the mucosa. The histopathological diagnosis by biopsy was tubular adenoma with low-grade dysplasia.
Figure 2.
Endoscopic findings of duodenal tumor. a: Conventional endoscopy. A reddened, sessile, elevated lesion measuring approximately 30 mm in diameter was observed in the anterior wall of the duodenal bulb, and an area of whitish lower elevation extended around the lesion. b: Magnifying endoscopy with narrow-band imaging. Leaf-like villous structures of various sizes were observed in the elevated area. c: Magnifying endoscopy with narrow-band imaging combined with water-immersion technique. The widths of the villi were wider than those in the surrounding normal area. d: Chromoendoscopy. Spraying of indigo carmine clearly showed the border of the lesion and the unevenness of its surface.
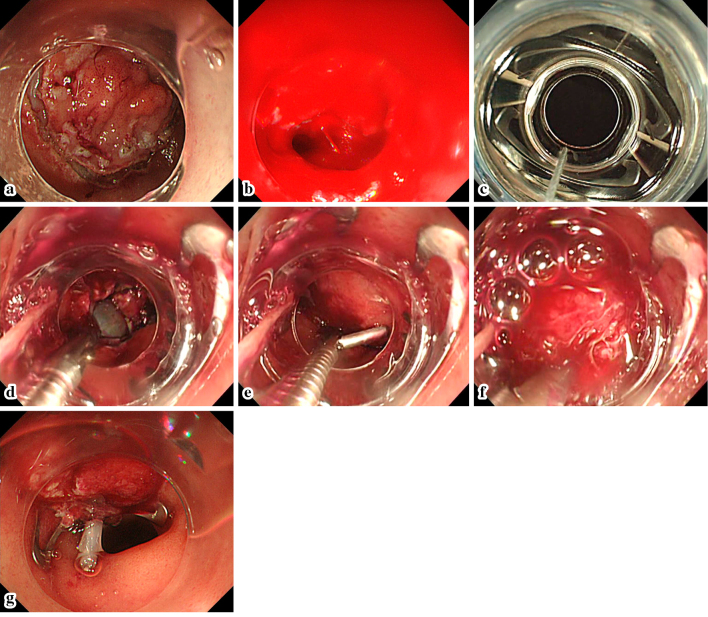
We performed ESD to confirm the histopathological diagnosis, because the accuracy of diagnosing duodenal tumor by biopsy is low, and because the risk of malignant transformation is high for tumors measuring at least 20 mm in diameter. The procedure was performed by carbon dioxide insufflation. Although a mixture of glyceol and hyaluronic acid was locally injected into the submucosa, the elevation of the lesion was insufficient, and submucosal dissection was difficult (Fig. 3a). Since a small perforation was noted during submucosal dissection, the procedure was changed to snaring with circumferential incision, which caused a full-thickness perforation measuring approximately 18 mm in diameter (Fig. 3b). Since the lesion was located in the anterior wall of the duodenal bulb, the resected lesion was not inverted into the peritoneal cavity, and the tumor was not exposed to the peritoneal cavity. The resected specimen was immediately removed to prevent peritoneal dissemination. Since arterial bleeding was observed from the full thickness resection site, hemostasis by cauterization was performed with hot biopsy forceps (Radial Jaw 4 Hot Biopsy Forceps, Boston Scientific, Marlborough, USA) at the perforated site. Afterwards, we decided to use the OTSC system to close the perforation. The endoscope (OLYMPUS GIF TYPE Q260J, Olympus) was immediately withdrawn. After being attached to an 11/6t OTSC system (Fig. 3c), it was then re-inserted. The perforation was visible from the front. Both edges of the perforation were grasped with both jaws of the OTSC Twin Grasper, which can be opened separately, in positions of correct approximation (Fig. 3d and e). The grasped tissue was pulled into the applicator cap, and the OTSC clip was then deployed while also performing continuous suction (Fig. 3f and g, Supplementary material). Additional TTSCs were then applied around the OTSC clip. The procedure was completed after the effective closure of the perforation was confirmed by the dilation of the duodenum under insufflation.
Figure 3.
Duodenal ESD and endoscopic closure of gastrointestinal perforation with the OTSC system. a: Although a mixture of glyceol and hyaluronic acid was locally injected into the submucosal layer, the elevation of the lesion was poor, and submucosal dissection was difficult. b: Resection of the lesion by snaring with a circumferential incision resulted in a full-thickness perforation measuring approximately 18 mm in diameter and arterial bleeding from the full thickness resection site. c: The applicator cap with a mounted OTSC clip was attached to the tip of the endoscope. d: The left edge of the perforation was grasped with one jaw of the OTSC Twin Grasper. e: The other jaw of the OTSC Twin Grasper was opened to grasp the right edge of the perforation while grasping the left edge with one jaw. f: The grasped tissue was pulled into the applicator cap, with continuous suctioning. g: The gastrointestinal perforation was endoscopically closed with the OTSC system.
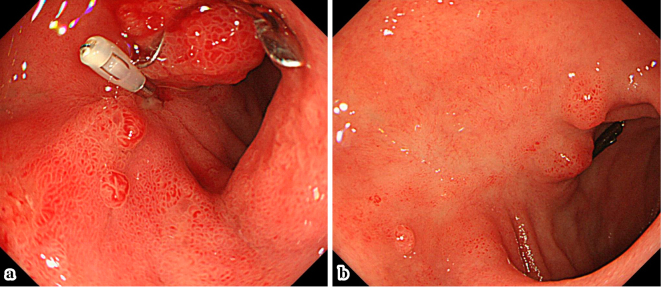
Transcutaneous needle decompression (Supercath, Medikit, Tokyo, Japan) was immediately performed for decompression after pneumoperitoneum. Thereafter, the patient fasted, was intravenously administered antibiotics and proton-pump inhibitors, and was intubated by nasogastric suction. No blood transfusion was necessary. Seven days after the procedure, the absence of leakage was confirmed by a gastrografin swallow (Fig. 4). Oral food intake was then initiated. The patient was discharged 14 days after the procedure. The tumor size in the resected specimen was 27×25 mm, and the pathological diagnosis was tubular adenoma with low-grade dysplasia. On follow-up upper gastrointestinal endoscopy performed one month later, the perforation was closed by the OTSC clip (Fig. 5a), and the endoscope could be advanced to the anal side. Upper gastrointestinal endoscopy performed one year later showed disengagement of the OTSC clip and scarring of the resection site (Fig. 5b).
Figure 4.
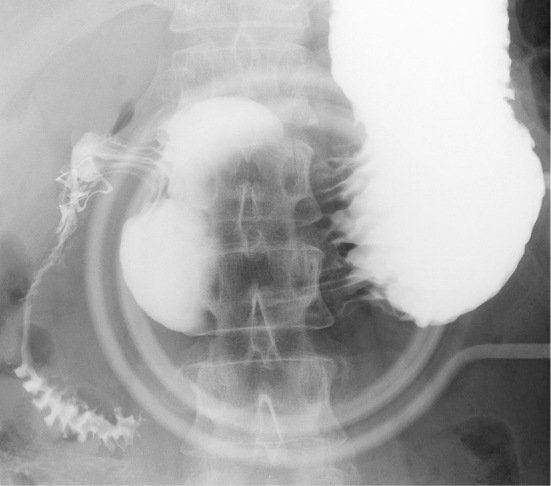
Gastrografin swallow seven days after OTSC clip placement. The OTSC clip was placed in the anterior wall of the duodenal bulb. Gastrografin passed to the anal side. No leakage was observed.
Figure 5.
Follow-up upper gastrointestinal endoscopy. a: Upper gastrointestinal endoscopy one month after the OTSC clip placement. The perforation was closed with the OTSC clip. b: Upper gastrointestinal endoscopy one year later. The OTSC clip was disengaged, and the resection site was scarred.
Discussion
While endoscopic treatment for superficial non-ampullary duodenal tumors is a challenging technique that is often associated with procedural accidents, the OTSC system was shown in this patient to be useful for the management of such iatrogenic events.
ESD is widely accepted as a treatment for gastrointestinal tumors because of its high en bloc resection rate, which makes accurate histopathological evaluation possible. However, the usage of this technique to treat duodenal lesions remains controversial due to its technical difficulty and its high incidence of procedural accidents (1-3,5). Based on excellent long-term outcomes, some endoscopic centers consider that piecemeal resection by endoscopic mucosal resection is acceptable, and refrain from aggressively performing duodenal ESD from the viewpoint of safety (3). Indeed, the incidence of adverse events in duodenal ESD has been reported to range from 6.7-36.6% for intraprocedural perforations and 0-14.3% for delayed perforations (1-5), being markedly higher than their incidences in other parts of the gastrointestinal tract. Moreover, emergency operations have been performed in 3.3-25.0% of the patients who underwent duodenal ESD due to the conversion of ESD to surgery necessitated by intraprocedural uncontrollable perforation or delayed perforation (1-5). This is due to the anatomical features of the duodenum, such as a narrow lumen, precipitous flexure that makes the endoscope unstable, abundant Brunner's glands in the submucosal layer that inhibit proper mucosal lifting, rich submucosal vasculature, and thin muscle layer associated with a high incidence of perforation (1,3,4,11).
In this patient, the OTSC system was shown to be useful for closing an acute iatrogenic duodenal perforation. Conventionally, TTSCs have been used for the endoscopic closure of gastrointestinal perforations. However, due to the narrow wingspan of the TTSC, multiple clips were needed for the repair, the leak rate after the repair of large perforations exceeding 1 cm was significant, and the treatment ended in mere surface layer closure rather than in full-thickness closure (6,7,10). The OTSC system, on the other hand, has higher gripping and holding strengths (10,11) and it is designed to achieve full-thickness closure of perforations with diameters up to 3 cm (6). It has been reported to be particularly effective for closing defects and leaks without causing fibrosis at the edges (8,10). According to a systematic review of the clinical outcomes of endoscopic closure of acute iatrogenic gastrointestinal perforations, the success rate using the OTSC system was remarkably high, namely at 87.8% (7). Few short- or long-term adverse events associated with OTSC placement have been reported (8), thus indicating its safety as an endoscopic device.
In duodenal ESD, it is necessary to pay attention not only to intraprocedural but also delayed perforation, due to exposure of the post-ESD ulcer to bile and pancreatic juice and to excessive thermal injury to the muscle layer (1-5,11). Complete closure of a post-ESD ulcer is useful for preventing delayed perforation (2,3,11). The usefulness of the OTSC system for complete closure of duodenal post-ESD ulcers has been reported (11). Prophylactic closure with the OTSC system makes re-ESD difficult. Provided a complete resection can be achieved, the OTSC system may therefore become useful not only for closing intraprocedural perforations, but also for preventing delayed perforations (2,11).
In conclusion, the OTSC system is considered to be a safe and efficient device for closing gastrointestinal perforations. For endoscopists who perform endoscopic treatments in the duodenum, which are technically difficult and associated with a high incidence of procedural accidents, endoscopic closure with the OTSC system is a technique that is necessary to master.
A full-thickness perforation measuring approximately 18 mm in diameter was endoscopically closed with the OTSC system.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Jung JH, Choi KD, Ahn JY, et al. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy 45: 133-135, 2013. [DOI] [PubMed] [Google Scholar]
- 2. Yamamoto Y, Yoshizawa N, Tomida H, Fujisaki J, Igarashi M. Therapeutic outcomes of endoscopic resection for superficial non-ampullary duodenal tumor. Dig Endosc 26: 50-56, 2014. [DOI] [PubMed] [Google Scholar]
- 3. Nonaka S, Oda I, Tada K, et al. Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy 47: 129-135, 2015. [DOI] [PubMed] [Google Scholar]
- 4. Hoteya S, Yahagi N, Iizuka T, et al. Endoscopic submucosal dissection for nonampullary large superficial adenocarcinoma/adenoma of the duodenum: feasibility and long-term outcomes. Endosc Int Open 1: 2-7, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Matsumoto S, Miyatani H, Yoshida Y. Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy 45: 136-137, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Voermans RP, Le Moine O, von Renteln D, et al. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol 10: 603-608, 2012. [DOI] [PubMed] [Google Scholar]
- 7. Verlaan T, Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Endoscopic closure of acute perforations of the GI tract: a systematic review of the literature. Gastrointest Endosc 82: 618-628.e5, 2015. [DOI] [PubMed] [Google Scholar]
- 8. Haito-Chavez Y, Law JK, Kratt T, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc 80: 610-622, 2014. [DOI] [PubMed] [Google Scholar]
- 9. Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc 66: 162-167, 2007. [DOI] [PubMed] [Google Scholar]
- 10. Singhal S, Changela K, Papafragkakis H, Anand S, Krishnaiah M, Duddempudi S. Over the scope clip: technique and expanding clinical applications. J Clin Gastroenterol 47: 749-756, 2013. [DOI] [PubMed] [Google Scholar]
- 11. Mori H, Fujihara S, Kobara H, et al. Successful closing of duodenal ulcer after endoscopic submucosal dissection with over-the-scope clip to prevent delayed perforation. Dig Endosc 25: 459-461, 2013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A full-thickness perforation measuring approximately 18 mm in diameter was endoscopically closed with the OTSC system.