Abstract
Objective: This study examined the associations between the adequacy of childcare provided by adult caretakers and childhood undernutrition in rural Yemen, independent of household wealth and food consumption.
Methods: We analyzed data of 3,549 children under the age of 5 years living in rural areas of Yemen based on the 2013 Yemen Baseline Survey of Mother and Child Health. Nutritional status was evaluated by the presence of underweight, stunting, and wasting according to the World Health Organization child growth standards. The impact of childcare including leaving children alone, putting older children into labor force, and the use of antenatal care while pregnant on child undernutrition was assessed and adjusted for food consumption by children, household composition, demographic and educational background of caretakers, and household wealth.
Results: The prevalence of underweight, stunting, and wasting was 46.2%, 62.6%, and 11.1%, respectively. Not leaving children alone, keeping children out of the labor force, and use of antenatal care were associated with a lower risk of underweight (odds ratio [OR] = 0.84, P = 0.016; OR = 0.84, P = 0.036; and OR = 0.85, P = 0.042) and stunting (OR = 0.80, P = 0.004; OR = 0.82, P = 0.024; and OR = 0.78, P = 0.003). After further adjustment for food consumption, the associations between adequate childcare indicators and lower odds of stunting remained significant (OR = 0.73, P = 0.025; OR = 0.72, P = 0.046; and OR = 0.76, P = 0.038).
Conclusions: A marked prevalence of stunting among rural children in Yemen was observed. Adequate childcare by adult caretakers in families is associated with a lower incidence of underweight and stunting among children under 5 years of age. Promoting adequate childcare by adult household members is a feasible option for reducing undernutrition among children in rural Yemen.
Keywords: child nutrition, family support, antenatal care use, child left behind, child labor
Introduction
Child nutrition indicators in Yemen are some of the worst among low- to middle-income countries. The reported national prevalence of stunting in Yemen was the second highest in the world following Afghanistan in 20101). The national average prevalence of underweight, stunting, and wasting was 39.0%, 46.5%, and 16.3%, respectively, among children under 5 years of age in 2013; furthermore, the prevalence of underweight and wasting did not change significantly between 2003 and 20132). In 2015, it was projected that 1 million children under 5 years of age would experience moderate acute undernutrition and that 320,000 would be at risk of severe acute undernutrition3, 4).
With the escalating political crisis in Yemen, since late 2014, food insecurity has increased because of the sporadic availability of essential food commodities, insufficient fuel, lack of income or employment opportunities, and the disruption of markets and trade. Conflict-related damage to infrastructure, shortages, and a lack of staff are among the causes of the collapse of basic health services in Yemen4). In addition, agricultural production is failing because of inadequate rainfall and the high cost and uneven availability of agricultural inputs (such as seed, fertilizer, farm tools, animal feed, and fuel for irrigation pumps)3). Despite these critical situations and uncertainties, clues to relieve undernutrition should be sought.
The availability of adequate care for preschool children has recently been discussed as an important part of the home environment for early childhood development5). One in five children under 5 years of age in low- and middle-income countries is without adult care for at least an hour in a given week5). Parental unavailability and poor working conditions, limited support networks, and the inability to afford childcare were suggested as factors associated with children being left alone at home6). Children who receive longer and more intensive childcare reportedly eat a larger variety of foods and have higher height-for-age and weight-for-age values compared with children who receive poorer childcare7).
Child labor in low- to middle-income countries reflects poverty and a lack of care within families. Widespread child labor in low- and middle-income countries also indicates the disadvantages of children in poor households. Worldwide, 12% of children between the ages of 5 and 14 years must work8). Lower levels of education and poorer physical and mental health are more prevalent among children who work than among those who do not work9).
The attitudes of caregivers toward maternal and child health and knowledge acquired during antenatal care visits can lower the risk of child undernutrition. The formal education level of mothers and delivery at a health facility are associated with better child nutritional status10). Health education provided during antenatal care is also associated with better nutritional status among children living in low- and middle-income countries11).
The objectives of this study were to examine the associations between the adequacy of childcare provided by adult caretakers and childhood undernutrition in rural Yemen, independent of household wealth and food consumption.
Materials and Methods
Study design
We conducted a study using the 2013 UNICEF Yemen Baseline Survey of Mother and Child Health data, collected using the Arabic language version of the Multiple Indicator Cluster Survey (MICS) 4 household questionnaire forms12, 13). The survey protocol was reviewed and approved by the Central Statistics Office, Ministry of Planning and Cooperation–Yemen.
Study setting
Yemen is one of the poorest countries in the Middle East and North Africa region. It is the most densely populated country in the Arabian Peninsula with a population of 26 million14), most living in rural areas (71%)15).
Poverty, which has been significantly aggravated as a result of the political crisis, has risen from 42% of the population in 2009 to 54.5% in 2012; the gross domestic product (GDP) per capita was estimated to be US$ 1,408 in 2013 (Middle East and North Africa: US$ 4,677)15, 16). Political instability, widespread poverty, low educational attainment, and low agricultural productivity from a limited availability of land suitable for the cultivation of food grains, and water scarcity have subjected 41.1% of the population of Yemen to food insecurity17).
In Yemen, UNICEF has identified the 106 most vulnerable districts (of a total of 333 districts) as candidates for its development program interventions for the years 2012–201518). These districts have a total estimated population of 7.3 million, including 1.2 million children under the age of 5 years. The large majority (92%) of households in these UNICEF targeted districts live in rural areas13).
Subjects
A two-stage cluster sampling of subjects from 106 districts was performed based on a set of all available data at the district level. The 106 districts were split into five strata constituting 318 clusters. In the first stage, clusters were selected randomly within the strata with a probability proportional to the size of the population. In the second stage, households were selected from each selected cluster using simple random sampling. The household sampling frame was developed by counting or relisting.
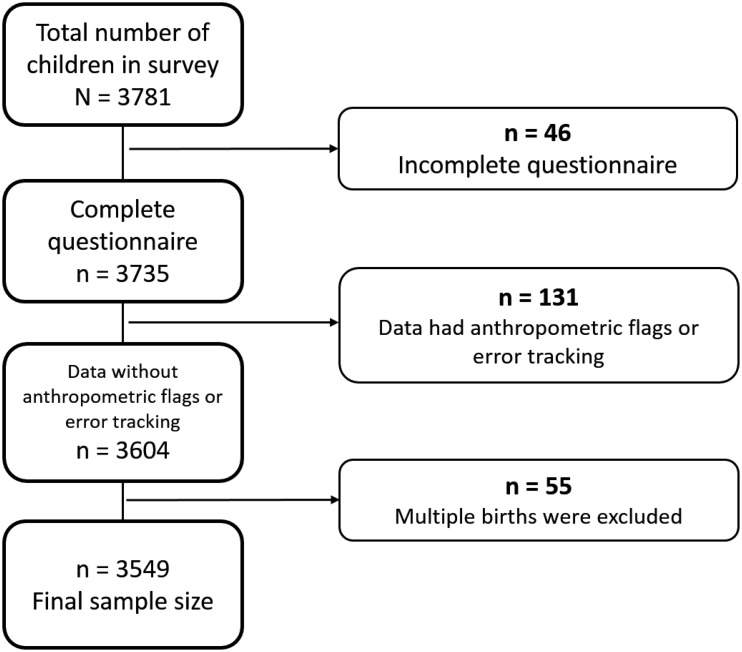
We conducted an analysis of 3,549 eligible children under 5 years of age (n = 2,300 mothers) nested in 2,115 households. The study was restricted to singleton birth children to control for confounders in the study design. Of 3,781 children, 232 cases were excluded from the analysis: 46 for incomplete questionnaires, 131 for anthropometric flags and error tracking, and 55 for multiple births. Criteria for the inclusion of subjects in the analysis were age under 5 years, singleton birth, and anthropometric measurements within specified ranges. Finally, 3,549 subjects were included in the analysis (Figure 1).
Figure 1.
Selection of subjects.
Variables
Nutritional status indicators: The main outcome variables in this study were nutritional status indicators, measured as underweight, stunting, and wasting. According to the measured weight and height, age in months, and sex, the Z-score values of weight-for-age, height-for-age, and weight-for-height were computed using World Health Organization (WHO) Anthro software19), which applies the WHO Child Growth Standards20). Subjects with Z-scores falling outside of the following ranges were excluded: weight-for-age Z-score of –6 to +5, height-for-age Z-score of –6 to +5, and weight-for-height Z-score of –5 to +519). Underweight, stunted, and wasted were defined by WHO as less than 2 SDs of weight-for-age, height-for-age, and weight-for-height, respectively20, 21).
Wealth index: Household wealth was measured using the wealth index calculated according to the Filmer and Pritchett method, which was developed using a principal component analysis based on household asset data (i.e., ownership of consumer items such as a TV, radio, car, refrigerator, mobile phone, computer, and generator) as well as housing characteristics (i.e., source of drinking water, sanitation facilities, type of floor materials, number of rooms, and access to electricity)22). Quintiles of the wealth index scores among the subjects were calculated, and the individual categories were named as follows: poorest, poor, middle, rich, and richest.
Food consumption: Food items consumed by children were reported for children aged 6–23 months of age. The consumption of any foods from each of the following six categories during the previous day was counted as the consumption of one item: (a) porridge/paste, bread, rice, pasta, or any foods made from grains or potatoes; (b) foods made from broad beans, pinto beans, peas, lentils, peanuts, or any other legumes; (c) milk, cheese, yogurt, buttermilk, ice cream, or other milk product; (d) fresh, dried, or packaged liver, kidney, heart, meat or other soup, beef, lamb or goat’s meat, chicken, or fish; (e) eggs; and (f) carrots, squash, sweet potato, leafy vegetables, or ripe mango or papaya. The sum of the number of items was used as a food consumption variable.
Caretaker characteristics: The age of the caretaker of the children who were examined as subjects and their school attendance (never or ever) were used as caretaker variables. If the caretaker was a woman who had delivered one or more children during the 2 years preceding the survey, the use of antenatal care at least once during that pregnancy (no or yes) was also used as a caretaker variable.
Number of family members: According to the ages of individual family members in the respective households, the following variables were evaluated: (1) number of children 0–4 years old, including the subject child; (2) number of children 5–14 years old; (3) number of adults 15–39 years old; and (4) number of adults 40–64 years old.
Adequate childcare environment of families: Whether or not the adult family members had left the subject children unattended for more than 1 hour in the 1 week preceding the survey (no or yes) was used as a variable of the childcare environment. This parameter included adults who left the subject child attended by another child under 10 years of age. The number of children in the family aged 5–14 years old who had joined the labor force was counted and used as another variable of the childcare environment.
Statistical methods
The prevalence of underweight, stunting, and wasting according to the characteristics of the children, caretakers, and households were calculated.
A multivariate logistic regression analysis was performed to investigate the relationships between nutritional indicators and the characteristics of children and caretakers and the number of family members. We applied multiple imputation methods to analyze dataset with some missing values. Multiple imputation is a statistical method used to improve the validity of epidemiological research results and to reduce the waste of resources caused by missing data23). Logistic regression models for binary and ordinal variables were used to handle missing dichotomous and ordinal data, respectively. The average proportion of missing data for all variables in this study was less than 2%. Predictive mean matching was used to handle missing continuous data.
An additional multivariate logistic regression analysis was performed to evaluate independent associations between nutritional indicators and variables of adequate childcare by adult caretakers (adult family members did not leave children alone, no children in the household who were 5–14 years old were engaged in labor, and the use of antenatal care by caretakers) after adjustment for the influence of household wealth and food consumption. Interaction effects between child age and adequate childcare were investigated.
The data were identified and analyzed using StataMP version 13.0 (StataCorp LP, College Station, TX, USA).
Results
Table 1 shows the frequency distribution of children according to the characteristics of children, caretakers, and households. The average age of the children was 28.7 months (standard error [SE], 16.7 months), and the average age of the caretakers was 29.9 years (SE, 7.0 years). The average household size was 7.7 members (SE, 3.7 members) among 2,115 households.
Table 1. Characteristics of subjects, caretakers, and households (n = 3,549).
| Characteristics | % | ||
|---|---|---|---|
| Subject children | |||
| Sex | Boy | 53.5 | |
| Girl | 46.5 | ||
| Age (months) | 0–11 | 19.4 | |
| 12–23 | 20.8 | ||
| 24–35 | 21.4 | ||
| 36–47 | 20.3 | ||
| 48–59 | 18.2 | ||
| No. of food items consumed among children 6–23 months old (n = 1,114) | 0 | 14.0 | |
| 1 | 26.4 | ||
| 2 | 26.8 | ||
| 3 | 18.5 | ||
| ≥ 4 | 14.4 | ||
| Caretakers | |||
| Age (years) | 15–19 | 3.5 | |
| 20–29 | 49.0 | ||
| 30–39 | 37.0 | ||
| ≥ 40 | 10.6 | ||
| School attendance | Never | 72.4 | |
| Ever | 27.6 | ||
| Use of antenatal care by caretakers (n = 2,594) | No | 53.7 | |
| Yes | 46.3 | ||
| Households | |||
| Wealth | Poorest | 21.1 | |
| Poor | 20.5 | ||
| Middle | 20.1 | ||
| Rich | 19.3 | ||
| Richest | 19.0 | ||
| No. of children 0–4 years old | 1 | 27.0 | |
| 2 | 44.0 | ||
| 3 | 20.7 | ||
| ≥4 | 8.3 | ||
| No. of children 5–14 years old | 0 | 19.2 | |
| 1 | 13.6 | ||
| 2 | 16.4 | ||
| 3 | 18.2 | ||
| 4 | 15.0 | ||
| ≥ 5 | 17.5 | ||
| No. of adults 15–39 years old | 0–1 | 13.5 | |
| 2 | 48.5 | ||
| 3 | 12.0 | ||
| 4 | 9.9 | ||
| ≥ 5 | 16.1 | ||
| No. of adults 40–64 years old | 0 | 49.8 | |
| 1 | 28.1 | ||
| ≥ 2 | 22.1 | ||
| Adult family members left subject children unattended for > 1 hour in a week | No | 53.6 | |
| Yes | 46.4 | ||
| No. of children 5–14 years old engaged in labor (n = 2,827) | 0 | 43.0 | |
| ≥ 1 | 57.0 | ||
The Spearman rank correlation between the wealth index quintile and the number of food items consumed by children 6–23 months old was 0.20 (P < 0.001). Among 2,115 households, the Spearman rank correlation between household size and the wealth index quintile was 0.10 (P < 0.001).
Table 2 shows the prevalence of underweight, stunting, and wasting according to the characteristics of children, caretakers, and households. The overall prevalence of underweight, stunting, and wasting was 46.2%, 62.6%, and 11.1%, respectively. The consumption of fewer food items was associated with the prevalence of underweight, and the non-use of antenatal care by caretakers was associated with the prevalence of underweight, stunting, and wasting. The prevalence of underweight, stunting, and wasting among children from poor families was significantly higher than those among children from richer families. There were variations in the prevalence of undernutrition according to the number of adult members in the households. Children from families where adult family members left the subject children unattended for more than 1 hour in a week were more likely to exhibit an underweight, stunting, or wasting status. Children from families where older children in the family had entered the labor force were more likely to be underweight or stunted.
Table 2. Prevalence of underweight, stunting, and wasting according to characteristics of children, caretakers, and households (n = 3,549).
| Characteristics | Underweight | Stunting | Wasting | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | P | % | P | % | P | |||||
| All | 46.2 | 62.6 | 11.1 | |||||||
| Subject children | ||||||||||
| Sex | Boy | 48.5 | 0.003 | 64.0 | 0.065 | 12.4 | 0.007 | |||
| Girl | 43.5 | 61.0 | 9.6 | |||||||
| Age (months) | 0–11 | 45.9 | 0.104 | 51.0 | < 0.001 | 12.4 | 0.049 | |||
| 12–23 | 42.3 | 62.6 | 13.0 | |||||||
| 24–35 | 46.8 | 66.7 | 11.6 | |||||||
| 36–47 | 47.1 | 66.0 | 9.6 | |||||||
| 48–59 | 49.5 | 66.2 | 8.7 | |||||||
| No. of food items consumed among children 6–23 months old (n = 1,114) | 0 | 51.3 | 0.008 | 64.1 | 0.102 | 14.7 | 0.095 | |||
| 1 | 45.6 | 57.5 | 14.6 | |||||||
| 2 | 44.3 | 62.4 | 9.4 | |||||||
| 3 | 35.9 | 53.9 | 14.1 | |||||||
| ≥ 4 | 35.0 | 53.1 | 8.1 | |||||||
| Caretakers | ||||||||||
| Age (years) | 15–19 | 48.8 | 0.841 | 67.5 | 0.688 | 15.5 | 0.368 | |||
| 20–29 | 46.4 | 62.3 | 11.4 | |||||||
| 30–39 | 46.3 | 62.7 | 10.5 | |||||||
| ≥ 40 | 44.4 | 61.7 | 10.4 | |||||||
| School attendance | Never | 47.6 | 0.006 | 63.3 | 0.162 | 11.4 | 0.417 | |||
| Ever | 42.5 | 60.7 | 10.4 | |||||||
| Use of antenatal care by caretakers (n = 2,594) | No | 49.0 | 0.002 | 65.2 | < 0.001 | 12.8 | 0.032 | |||
| Yes | 43.1 | 58.2 | 10.1 | |||||||
| Households | ||||||||||
| Wealth | Poorest | 51.8 | < 0.001 | 65.6 | 0.001 | 13.9 | < 0.001 | |||
| Poor | 50.0 | 63.9 | 13.6 | |||||||
| Middle | 47.3 | 65.2 | 10.2 | |||||||
| Rich | 43.2 | 61.3 | 10.5 | |||||||
| Richest | 37.9 | 56.2 | 6.8 | |||||||
| No. of children 0–4 years old | 1 | 46.1 | < 0.001 | 61.3 | < 0.001 | 11.7 | 0.903 | |||
| 2 | 47.3 | 64.8 | 11.0 | |||||||
| 3 | 48.6 | 63.6 | 10.6 | |||||||
| ≥ 4 | 34.8 | 52.0 | 11.2 | |||||||
| No. of children 5–14 years old | 0 | 46.2 | 0.905 | 62.9 | 0.783 | 10.9 | 0.629 | |||
| 1 | 46.0 | 61.1 | 13.3 | |||||||
| 2 | 47.9 | 64.0 | 11.7 | |||||||
| 3 | 46.2 | 63.8 | 10.1 | |||||||
| 4 | 46.8 | 62.6 | 10.7 | |||||||
| ≥ 5 | 44.4 | 60.6 | 10.6 | |||||||
| No. of adults 15–39 years old | 0–1 | 50.2 | <0.001 | 63.4 | 0.008 | 11.3 | 0.340 | |||
| 2 | 46.6 | 63.2 | 12.1 | |||||||
| 3 | 52.0 | 68.2 | 10.1 | |||||||
| 4 | 45.1 | 60.3 | 10.6 | |||||||
| ≥ 5 | 38.0 | 57.3 | 9.1 | |||||||
| No. of adults 40–64 years old | 0 | 47.4 | 0.075 | 63.3 | 0.329 | 11.7 | 0.575 | |||
| 1 | 46.9 | 63.1 | 10.5 | |||||||
| ≥ 2 | 42.7 | 60.3 | 10.6 | |||||||
| Adult family members left subject children unattended for > 1 hour in a week | No | 43.8 | <0.001 | 59.9 | <0.001 | 59.9 | <0.001 | |||
| Yes | 50.0 | 66.6 | 66.6 | |||||||
| No. of children 5–14 years old engaged in labor (n = 2,827) | 0 | 43.6 | 0.017 | 59.8 | 0.012 | 11.1 | 0.922 | |||
| ≥ 1 | 48.1 | 64.5 | 11.2 | |||||||
Table 3 shows the results of a multivariable logistic regression analysis to show the associations between undernutrition and characteristics of child and caretakers and the number of household members according to age groups. A higher number of men and women 15–39 years old was significantly associated with a lower prevalence of underweight (OR, 0.94; 95% confidence interval [CI], 0.90–0.98; P = 0.007) and stunting (OR, 0.95; 95% CI, 0.91–0.99; P = 0.023).
Table 3. Associations between undernutrition and characteristics of children and caretakers and number of household members according to age (n = 3,549).
| Underweight | Stunting | Wasting | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||||||
| Sex of child | |||||||||||||||
| Boy = 0, Girl = 1 | 0.815 | 0.713 | 0.931 | 0.003 | 0.887 | 0.773 | 1.017 | 0.086 | 0.731 | 0.590 | 0.905 | 0.004 | |||
| Age of child | |||||||||||||||
| Increase of 1 month | 1.004 | 1.000 | 1.008 | 0.043 | 1.013 | 1.009 | 1.017 | <0.001 | 0.990 | 0.983 | 0.996 | 0.001 | |||
| Age of caretaker | |||||||||||||||
| Increase of 1 year | 0.986 | 0.974 | 0.997 | 0.017 | 0.981 | 0.969 | 0.993 | 0.002 | 0.989 | 0.970 | 1.008 | 0.250 | |||
| School attendance of caretaker | |||||||||||||||
| Never = 0, Ever = 1 | 0.798 | 0.684 | 0.932 | 0.004 | 0.887 | 0.757 | 1.039 | 0.138 | 0.862 | 0.673 | 1.105 | 0.242 | |||
| No. of children 0–4 y/o | |||||||||||||||
| Increase of 1 person | 0.964 | 0.904 | 1.028 | 0.267 | 0.962 | 0.902 | 1.027 | 0.248 | 1.044 | 0.944 | 1.155 | 0.404 | |||
| No. of children 5–14 y/o | |||||||||||||||
| Increase of 1 person | 1.021 | 0.982 | 1.062 | 0.287 | 1.027 | 0.986 | 1.068 | 0.199 | 1.008 | 0.948 | 1.073 | 0.793 | |||
| No. of adults 15–39 y/o | |||||||||||||||
| Increase of 1 person | 0.942 | 0.902 | 0.984 | 0.007 | 0.950 | 0.910 | 0.993 | 0.023 | 0.950 | 0.886 | 1.020 | 0.158 | |||
| No. of adults 40–64 y/o | |||||||||||||||
| Increase of 1 person | 0.997 | 0.906 | 1.096 | 0.948 | 1.034 | 0.937 | 1.140 | 0.507 | 0.997 | 0.857 | 1.160 | 0.969 | |||
OR, odds ratio; CI, confidence interval; y/o, years old. ORs were estimated using multivariable logistic regression analyses.
Table 4 shows the adjusted ORs of undernutrition for the variables of adequate childcare (adult family members did not leave children alone, no children in the household aged 5–14 years old and engaged in labor, and use of antenatal care by caretakers) after adjustment for the characteristics of children and caretakers, the number of family members, and household wealth. Not leaving children alone was significantly associated with a lower prevalence of underweight (OR, 0.84; 95% CI, 0.72–0.97; P = 0.016) and stunting (OR, 0.80; 95% CI, 0.69–0.93; P = 0.004). Older children not working was significantly associated with a lower prevalence of underweight (OR, 0.84; 95% CI, 0.71–0.99; P = 0.036) and stunting (OR, 0.82; 95% CI, 0.69–0.97; P = 0.024). Use of antenatal care was significantly associated with a lower prevalence of underweight (OR, 0.85; 95% CI, 0.72–0.99; P = 0.042) and stunting (OR, 0.78; 95% CI, 0.66–0.92; P = 0.003). Statistical significant interactions were observed between child age and both not leaving children alone (P = 0.003) and use of antenatal care (P = 0.029). The adjusted OR for not leaving children alone on underweight was 1.23 (95% CI, 0.92–1.65; P = 0.165) for child age of 0 months and 0.57 (95% CI, 0.42–0.76; P <0.001) for child age of 59 months. The adjusted OR for use of antenatal care on underweight was 1.10 (95% CI, 0.83–1.46; P = 0.505) for child age of 0 months and 0.59 (95% CI, 0.41–0.85; P = 0.004) for child age of 59 months.
Table 4. Associations among undernutrition, adequate childcare by adult caretakers, and household wealth.
| Underweight | Stunting | Wasting | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||||||
| Adult family members did not leave children alone (n = 3,549) | |||||||||||||||
| No = 0, Yes = 1 | 0.84 | 0.72 | 0.97 | 0.016 | 0.80 | 0.69 | 0.93 | 0.004 | 0.92 | 0.73 | 1.15 | 0.464 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.88 | 0.84 | 0.93 | <0.001 | 0.94 | 0.89 | 0.99 | 0.026 | 0.85 | 0.78 | 0.93 | <0.001 | |||
| No children 5–14 y/o in household engaged in labor (n = 2,827) | |||||||||||||||
| No = 0, Yes = 1 | 0.84 | 0.71 | 0.99 | 0.036 | 0.82 | 0.69 | 0.97 | 0.024 | 1.00 | 0.77 | 1.30 | 0.998 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.89 | 0.84 | 0.94 | <0.001 | 0.92 | 0.87 | 0.98 | 0.007 | 0.84 | 0.76 | 0.92 | <0.001 | |||
| Use of antenatal care by caretakers (n = 2,594) | |||||||||||||||
| No = 0, Yes = 1 | 0.85 | 0.72 | 0.99 | 0.042 | 0.78 | 0.66 | 0.92 | 0.003 | 0.82 | 0.64 | 1.05 | 0.120 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.89 | 0.84 | 0.94 | <0.001 | 0.95 | 0.89 | 1.01 | 0.087 | 0.83 | 0.75 | 0.91 | <0.001 | |||
OR, odds ratio; CI, confidence interval; y/o, years old. Other variables included in the multivariable logistic regression analyses were sex and age of child, age of caretaker, school attendance of caretaker, number of children 0–4 y/o, number of children 5–14 y/o, number of adults 15–39 y/o, and number of adults 40–64 y/o.
Table 5 shows the adjusted ORs of undernutrition for not leaving children alone, older children not working, and use of antenatal care after adjustments for food consumption by children and other variables shown in Table 4. A higher number of food items consumed was significantly associated with a lower prevalence of underweight and stunting. Variables of adequate childcare by adults (i.e., not leaving children alone, older children not working, and use of antenatal care) were significantly associated with a lower prevalence of stunting. A statistically significant interaction was observed between child age and use of antenatal care (P = 0.049). The adjusted OR for use of antenatal care on stunting was 5.03 (95% CI, 0.75–33.54; P = 0.095) for child age of 0 months and decreased to 0.44 (95% CI, 0.24–0.80; P = 0.008) for child age of 59 months.
Table 5. Associations of undernutrition, adequate childcare by adult caretakers, food consumption by children, and household wealth.
| Underweight | Stunting | Wasting | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||||||
| Adult family members did not leave children alone (n = 1,114) | |||||||||||||||
| No = 0, Yes = 1 | 0.84 | 0.64 | 1.09 | 0.191 | 0.73 | 0.56 | 0.96 | 0.025 | 1.27 | 0.85 | 1.88 | 0.245 | |||
| Food consumption by children | |||||||||||||||
| Increase of 1 item | 0.87 | 0.79 | 0.96 | 0.006 | 0.85 | 0.77 | 0.94 | 0.001 | 0.95 | 0.82 | 1.10 | 0.483 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.90 | 0.81 | 0.99 | 0.044 | 0.99 | 0.89 | 1.09 | 0.867 | 0.74 | 0.64 | 0.87 | <0.001 | |||
| No children 5–14 y/o in household engaged in labor (n = 841) | |||||||||||||||
| No = 0, Yes = 1 | 0.91 | 0.66 | 1.24 | 0.535 | 0.72 | 0.53 | 0.99 | 0.046 | 1.11 | 0.70 | 1.77 | 0.646 | |||
| Food consumption by children | |||||||||||||||
| Increase of 1 item | 0.86 | 0.77 | 0.95 | 0.005 | 0.86 | 0.77 | 0.95 | 0.005 | 0.92 | 0.78 | 1.08 | 0.301 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.88 | 0.79 | 0.98 | 0.030 | 0.97 | 0.87 | 1.08 | 0.592 | 0.77 | 0.65 | 0.91 | 0.002 | |||
| Use of antenatal care by caretakers (n = 1,062) | |||||||||||||||
| No = 0, Yes = 1 | 0.91 | 0.71 | 1.18 | 0.491 | 0.76 | 0.59 | 0.98 | 0.038 | 0.97 | 0.65 | 1.42 | 0.860 | |||
| Food consumption by children | |||||||||||||||
| Increase of 1 item | 0.83 | 0.76 | 0.92 | < 0.001 | 0.81 | 0.74 | 0.89 | < 0.001 | 0.89 | 0.77 | 1.04 | 0.141 | |||
| Household wealth | |||||||||||||||
| Increase of 1 quintile | 0.90 | 0.81 | 0.99 | 0.035 | 0.97 | 0.87 | 1.07 | 0.542 | 0.77 | 0.66 | 0.89 | 0.001 | |||
OR, odds ratio; CI, confidence interval; y/o, years old. Other variables included in the multivariable logistic regression analyses were sex and age of child, age of caretaker, school attendance of caretaker, number of children 0–4 y/o, number of children 5–14 y/o, number of adults 15–39 y/o, and number of adults 40–64 y/o.
Discussion
This study presented the prevalence and determinants of underweight, stunting, and wasting among children under 5 years of age in rural areas of Yemen, which were influenced by food insecurity. Children living with a small number of adult members aged 15–39 years old were significantly underweight and stunted. Multivariate analyses revealed that stunting was negatively associated with adult family members who did not leave children alone, families with no older children engaged in labor, and the use of antenatal care by caretakers, independent of household wealth and food consumption by children.
The present study used a standardized questionnaire developed by UNICEF. The subjects were randomly selected according to a standard protocol, the household response rate was 93%, and 94% of eligible children were included in the analysis. The magnitude of the selection bias was considered relatively low. Child growth was assessed and analyzed according to the standard methods developed by the WHO. Household wealth was evaluated using a strategy similar to that used in the UNICEF Multiple Indicator Cluster Surveys as well as the Demographic and Health Surveys. Therefore, the results of this study can be interpreted with reference to previous surveys using UNICEF standardized protocols.
The prevalence of underweight and stunting among children in rural areas of Yemen estimated in this study were higher than the national average. Stunting is an indicator of previous growth failure resulting from chronic undernutrition, whereas wasting indicates current or acute undernutrition resulting from failure to gain weight or weight loss; underweight is a composite measure of stunting and wasting21).
The prevalence of stunting is reportedly higher in less wealthy households24), and the magnitude of socioeconomic inequalities in underweight and stunting was larger in countries with a higher prevalence of underweight and stunting, respectively25). Children whose families were educated and consisted of fewer than five family members had significantly lower odds of undernutrition compared with peers in illiterate families and family sizes of more than five members, respectively26). Independent of household wealth, a lower paternal and maternal education level was also associated with child stunting27). Household wealth and the educational status of caretakers consistently affected the nutritional status of children in this study, in agreement with earlier studies.
The average number of household members in Yemen is 6.7, which is higher than the averages of other Arabic countries such as Egypt (4.1, as of 2014) and Jordan (5.1, as of 2012)28, 29). There are some unique characteristics of family composition in Yemen. An extended family, where relatives live together, is common in Yemen, and more than 25% of households consist of nine or more family members2). There are also polygamous families, and 6.1% of women live with co-wives2).
The results of the present study showed that the number of household members between the ages of 15 and 39 years old was associated with the alleviation of undernutrition in children. Other studies counting the number of children and adults inclusive showed that the number of household members of all ages was associated with undernutrition30,31,32). Having a larger number of siblings, which often suggests more competition for food, was associated with child undernutrition among children under 5 years old30, 33). Within-household cooperation by adult members could improve the quality of childcare in the household34).
Children in households where children received adequate care from caretakers had a lower risk of child undernutrition; the prevalence of undernutrition was lower in households where adult members of the family did not leave the children alone and in which children had not entered the labor force. These associations remained significant after adjustments for the number of family members, household wealth, and food consumption by subject children. A large number of household adult members in households in Yemen have some protective functions that enable them to protect the health of children living within the household.
The present study showed an association between the use of antenatal care by caretakers and the nutritional status of children among poor populations in a food-insecure country, even after adjustments for within-population variations in socioeconomic status and educational level. These findings suggest that the potential health benefits of antenatal care services extend beyond the conditions at the time of the visit to influence a wider range of health issues in the future.
The potential mechanism that could explain the impact of inadequate childcare by adult family members on nutritional status may be exerted through a lack of feeding and hygiene practices35-38). Feeding practices do not just refer to the foods recommended for a child, but it means also the broad range of dietary, behavioral, and physiological processes involved39). Our findings have shown that food consumption is a mediator of the association between childcare and stunting. Children left alone at home could be exposed to poor feeding practices including breastfeeding and complementary feeding35, 36). Poor sanitation and high-risk hygiene behaviors expose children to infectious disease, especially diarrheal diseases, which would lead to undernutrition38, 40).
The number of food items consumed was associated with undernutrition in children. This study confirmed evidence from a previous study that a higher dietary diversity improves the nutritional condition of children41). An analysis of the Demographic and Health Surveys showed that a high dietary diversity was associated with a higher height-for-age Z-score in nine countries42). In addition to promoting appropriate childcare and improving the socioeconomic status of the household, efforts should be continued to secure the availability of food and to improve the nutritional status of children in poorer areas.
The present study has some limitations. Food consumption patterns were assessed among children aged 6–23 months old. This study had a cross-sectional design, and temporal relations are not provided. The cross-sectional nature of this study limits the potential influence of a selection bias on the population; for example, subjects who are severely malnourished might have died at a younger age and therefore would not be included in the present analysis. The inclusion of polygamous families in this study should be considered when generalizing the results of this study to other populations. Involvement in the occupation of caretakers and their families could have been a confounder of the association between adequate childcare and child nutrition; however, the potential magnitude of the confounding bias was considered to be limited because the variation of occupations in rural area is relatively small. Interactions by child age were observed. Associations between adequate childcare by adult caretakers and underweight among older-age children were strong, whereas those associations among infants were small or missing; however, these results do not contradict our conclusions. Inequities of availability of adequate childcare increases as children grow older, although the differences at very young ages are small.
This is the first study to focus on the roles of adequate childcare provided by adults among households in rural Yemen, where food insufficiency exists and undernutrition of children is prevalent. Caregiving practices, parenting, feeding, and caregiving resources are now partly considered when analyzing issues related to child nutrition and development in low- and middle-income countries43). The present study suggests potential alternative strategies for promoting child nutrition by improving the childcare environment under sustained limited access to food.
Child undernutrition is an urgent and prioritized public health issue in rural Yemen, where the majority of women are illiterate and economically poor. Food security in Yemen worsened between 2009 and 201117). The ongoing political crisis since 2014 has further worsened the situation44). Because food insecurity continues to exist, the caretaking environment for children can act as a control gate to improve the nutritional status of children. Although the recovery of food security and the alleviation of poverty might be direct and root-cause solutions for normalizing the nutritional status of children, provision of adequate childcare by adult family members should also be sought in Yemen. Attention to appropriate childcare should be a focus of interest and should be integrated into health programs. Inter-sectoral approaches should also be enhanced to promote adequate caretaking by adult family members.
In conclusion, severe undernutrition in children still exists in rural areas of Yemen. Gradients in the prevalence of undernutrition according to wealth and food consumption exist. Independent of household wealth and food consumption by children, factors such as continuous attention to childcare by adult caretakers who do not leave children alone, having no older children engaged in labor, and the participation of caretakers in childcare education by attending antenatal care were associated with a better nutritional status of children. In addition to international cooperation efforts to improve food security in rural areas affected by conflicts, integrated efforts to advance childcare by adult caretakers in families should be emphasized to prevent child undernutrition in rural Yemen.
Conflict of Interest: The authors declare that they have no competing interests.
References
- 1.United Nations Children’s Fund (UNICEF). Situation Analysis of Children in Yemen 2014. Sana’a, Yemen: UNICEF, Country Office Yemen; 2014. Available from: http://www.unicef.org/mena/MENA-Situation_Analysis_report_-_English_Final(1).pdf.
- 2.Ministry of Public Health and Population (MOPHP), Central Statistical Organization (CSO) [Yemen], Pan Arab Program for Family Health (PAPFAM), and ICF International. Yemen National Health and Demographic Survey 2013. Rockville, Maryland, USA: MOPHP, CSO, PAPFAM, and ICF International; 2015.
- 3.United Nations. Humanitarian Needs Overview – Yemen 2016. UN Office for the Coordination of Humanitarian Affairs; 2015. Available from: https://www.humanitarianresponse.info/en/operations/yemen/document/yemen-humanitarian-needs-overview-2016-english.
- 4.United Nations Children’s Fund (UNICEF). Yemen Humanitarian Situation Report: 27 January – 9 February 2016. Available from: http://www.unicef.org/appeals/files/UNICEF_Yemen_Humanitarian_SitRep_9_Feb_2016.pdf.
- 5.Samman E, Presler-Marshall E, Jones N, et al Women’s work: Mothers, children and the global childcare crisis. London: Overseas Development Institute; 2016. Available from: https://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/10333.pdf.
- 6.Ruiz-Casares M, Heymann J. Children home alone unsupervised: modeling parental decisions and associated factors in Botswana, Mexico, and Vietnam. Child Abuse Negl 2009; 33: 312–323. doi: 10.1016/j.chiabu.2008.09.010 [DOI] [PubMed] [Google Scholar]
- 7.Lamontagne JF, Engle PL, Zeitlin MF. Maternal employment, child care, and nutritional status of 1218-month-old children in Managua, Nicaragua. Soc Sci Med 1998; 46: 403–414. doi: 10.1016/S0277-9536(97)00184-6 [DOI] [PubMed] [Google Scholar]
- 8.International Labour Organization (ILO). The twin challenges of child labour and youth employment in the Arab States. Geneva: International Labour Office; ILO Regional Office for the Arab States; Fundamental Principles and Rights at Work Branch; 2016. Available from: http://www.ilo.org/ipec/Informationresources/WCMS_IPEC_PUB_27702/lang--en/index.htm.
- 9.Caglayan C, Hamzaoglu O, Yavuz CI. Working conditions and health status of child workers: cross-sectional study of the students at an apprenticeship school in Kocaeli. Pediatr Int 2010; 52: 6–12. doi: 10.1111/j.1442-200X.2009.02881.x [DOI] [PubMed] [Google Scholar]
- 10.Ickes SB, Hurst TE, Flax VL. Maternal Literacy, Facility Birth, and Education Are Positively Associated with Better Infant and Young Child Feeding Practices and Nutritional Status among Ugandan Children. J Nutr 2015; 145: 2578–2586. doi: 10.3945/jn.115.214346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lassi ZS, Das JK, Zahid G. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. BMC Public Health 2013; 13(Suppl 3): S13. doi: 10.1186/1471-2458-13-S3-S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United Nations Children’s Fund (UNICEF). Multiple Indicator Cluster Surveys (MICS): MICS4 Tools. Available from: http://mics.unicef.org/tools?round=mics4.
- 13.United Nations Children’s Fund (UNICEF) and Central Statistical Organization (CSO- Yemen). UNICEF Yemen Baseline Survey Report 2013. Sana’a: UNICEF Country Office of Yemen; 2013. [Google Scholar]
- 14.World Bank. Countries: Yemen Overview. Accessed March 17, 2016. Available from: http://www.worldbank.org/en/country/yemen.
- 15.Central Statistical Organization (CSO). Yemen Statistical Yearbook 2013. Sana’a: The Ministry of Planning and International Cooperation: CSO; 2014.
- 16.World Bank. Data: GDP per capita (current US$), 2013. Accessed March 17, 2016. Available from: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD/countries/YE-XQ-XN?display=graph.
- 17.World Food Programme (WFP) and Central Statistical Organization (CSO). Yemen Comprehensive Food Security Survey 2014. Sana’a: WFP Country Office of Yemen; 2014. Available from: https://www.wfp.org/content/yemen-comprehensive-food-security-survey-november-2014.
- 18.United Nations Children’s Fund (UNICEF). Annual Report 2012 for Yemen. UNICEF; 2012. Available from: http://www.unicef.org/about/annualreport/files/Yemen_COAR_2012.pdf.
- 19.World Health Organization (WHO). WHO Anthro for personal computers manual: Software for assessing growth and development of the world’s children. Geneva: WHO, Department of Nutrition for Health and Development; 2010. Available from: http://www.who.int/childgrowth/software/en/.
- 20.World Health Organization (WHO). WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: WHO, Department of Nutrition for Health and Development; 2006. Available from: http://www.who.int/childgrowth/standards/technical_report/en/.
- 21.Cogill B. Anthropometric Indicators Measurement Guide. Washington, DC: Food and Nutrition Technical Assistance (FANTA) Project, FHI 360; 2003. [Google Scholar]
- 22.Rutstein SO, Kiersten J. The DHS Wealth Index. DHS Comparative Reports No. 6. Calverton, Maryland: ORC Macro; 2004.
- 23.Sterne JA, White IR, Carlin JB. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009; 338: b2393. doi: 10.1136/bmj.b2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van de Poel E, Hosseinpoor AR, Speybroeck N. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Organ 2008; 86: 282–291. doi: 10.2471/BLT.07.044800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bredenkamp C, Buisman LR, Van de Poel E. Persistent inequalities in child undernutrition: evidence from 80 countries, from 1990 to today. Int J Epidemiol 2014; 43: 1328–1335. doi: 10.1093/ije/dyu075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Degarege A, Hailemeskel E, Erko B. Age-related factors influencing the occurrence of undernutrition in northeastern Ethiopia. BMC Public Health 2015; 15: 108. doi: 10.1186/s12889-015-1490-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ikeda N, Irie Y, Shibuya K. Determinants of reduced child stunting in Cambodia: analysis of pooled data from three demographic and health surveys. Bull World Health Organ 2013; 91: 341–349. doi: 10.2471/BLT.12.113381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health and Population [Egypt], El-Zanaty and Associates [Egypt], and ICF International. Egypt Demographic and Health Survey 2014. Cairo, Egypt and Rockville, Maryland, USA: Ministry of Health and Population and ICF International; 2015.
- 29.Department of Statistics [Jordan] and ICF International. Jordan Population and Family Health Survey 2012. Calverton, Maryland, USA: Department of Statistics and ICF International; 2013.
- 30.Fikadu T, Assegid S, Dube L. Factors associated with stunting among children of age 24 to 59 months in Meskan district, Gurage Zone, South Ethiopia: a case-control study. BMC Public Health 2014; 14: 800. doi: 10.1186/1471-2458-14-800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kavosi E, Hassanzadeh Rostami Z, Kavosi Z. Prevalence and determinants of under-nutrition among children under six: a cross-sectional survey in Fars province, Iran. Int J Health Policy Manag 2014; 3: 71–76. doi: 10.15171/ijhpm.2014.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kinyoki DK, Berkley JA, Moloney GM. Predictors of the risk of malnutrition among children under the age of 5 years in Somalia. Public Health Nutr 2015; 18: 3125–3133. doi: 10.1017/S1368980015001913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong HJ, Moy FM, Nair S. Risk factors of malnutrition among preschool children in Terengganu, Malaysia: a case control study. BMC Public Health 2014; 14: 785. doi: 10.1186/1471-2458-14-785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kismul H, Hatløy A, Andersen P. The social context of severe child malnutrition: a qualitative household case study from a rural area of the Democratic Republic of Congo. Int J Equity Health 2015; 14: 47. doi: 10.1186/s12939-015-0175-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Longhurst R, Tomkins A. The role of care in nutrition a neglected essential ingredient. SCN News 1995; (12): 1–5. [PubMed] [Google Scholar]
- 36.Engle PL, Bentley M, Pelto G. The role of care in nutrition programmes: current research and a research agenda. Proc Nutr Soc 2000; 59: 25–35. doi: 10.1017/S0029665100000045 [DOI] [PubMed] [Google Scholar]
- 37.Rah JH, Cronin AA, Badgaiyan B. Household sanitation and personal hygiene practices are associated with child stunting in rural India: a cross-sectional analysis of surveys. BMJ Open 2015; 5: e005180. doi: 10.1136/bmjopen-2014-005180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization (WHO), United Nations Children’s Fund (UNICEF), United States Agency for International Development (USAID). Improving nutrition outcomes with better water, sanitation and hygiene: practical solutions for policies and programmes. Geneva: WHO; 2015. [Google Scholar]
- 39.Brown KH, Dewey K, Allen L. Complementary Feeding of Young Children in Developing Countries: a Review of Current Scientific Evidence. WHO/NUT/98.1. Geneva: WHO; 1998. [Google Scholar]
- 40.Dangour AD, Watson L, Cumming O. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst Rev 2013; CD009382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Darapheak C, Takano T, Kizuki M. Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int Arch Med 2013; 6: 29. doi: 10.1186/1755-7682-6-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arimond M, Ruel MT. Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. J Nutr 2004; 134: 2579–2585. [DOI] [PubMed] [Google Scholar]
- 43.Black RE, Victora CG, Walker SP. Maternal and Child Nutrition Study GroupMaternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013; 382: 427–451. doi: 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 44.United Nations Children’s Fund (UNICEF) Yemen: Childhood Under Threat. New York: Unicef; 2015. Available from: http://www.unicef.org/media/files/CHILD_ALERT_YEMEN-UNICEF_AUG_2015_ENG_FINAL.pdf.