Abstract
PURPOSE:
The purpose of this study is to evaluate the causes of phakic implantable collamer lens (ICL) explantation/exchange at an eye hospital in Saudi Arabia.
MATERIALS AND METHODS:
A retrospective chart review was performed for patients who underwent ICL implantation from 2007 to March 2014 and data were collected on cases that underwent ICL explantation.
RESULTS:
Of the 787 ICL implants, 30 implants (3.8% [95% confidence interval 2.6%; 5.3%]) were explanted. The causes of explantation included incorrect lens size (22), cataract (4), high residual astigmatism (2), rhegmatogenous retinal detachment (1), and intolerable glare (1). Corrective measures mainly included an exchange with an appropriately sized lens (9), ICL explantation (11), with phacoemulsification and posterior chamber intraocular lens implantation (6), or replacement with an ICL of correct power (2).
CONCLUSION:
Incorrect ICL size was the most common cause of ICL explantation. More accurate sizing methods for ICL are required to reduce the explantation/exchange rate.
Key words: Explantation, implantable collamer lens, Saudi Arabia
Introduction
The implantable collamer lens (ICL) (Staar Surgical AG., Nidau, Switzerland) is a commonly used phakic intraocular lens (IOL).[1] However, explantation and exchange pose a risk to the eye and should be avoided. Identifying the preventable causes of explantation would minimize risk to the eye and the patient. At our institute, ICL surgery has been performed for 8 years. Complications of ICL are reported in case reports and a case series that reports intraocular pressure changes.[2,3] To the best of our knowledge, there is no published peer review study of the causes of explantation in an Arab country. We present the causes of ICL explantation and management of patients requiring ICL exchange or explantation.
Materials and Methods
In this case series, we included cases of ICL explantation at King Khaled Eye Specialist Hospital (KKESH) from January 2007 to March 2014. The KKESH Institutional Review Board approved this study (IRB-0915).
ICL implant power was calculated by the manufacturer (STAAR Surgical) using a modified vertex formula. The size of the ICL was based on the horizontal corneal diameter (CD) and anterior chamber (AC) depth. The CD was measured with calipers and scanning-slit topography (Orbscan IIz, Bausch and Lomb, Rochester, NY, USA) in some cases. The SRK-T formula was used to perform the IOL power calculations using the axial length measured with A-scan ultrasonography (US 800, NIDEK Co., Ltd, Gamagori, Japan) without correction for the ICL in situ. Keratometry readings were acquired with an autorefractor (OPD-Scan; NIDEK Co., Ltd., Gamagori Japan). Two peripheral iridectomies with a neodymium-yttrium aluminum garnet laser were performed before implantation. The pupil was pharmacologically dilated. After instillation of topical anesthesia, viscoelastic was injected into the AC. A model V4b ICL was inserted through a 3-mm corneal incision with an injector cartridge (STAAR Surgical). The ICL was placed in the posterior chamber. The remaining viscoelastic was completely removed and a miotic agent was instilled to stimulate pupil constriction. Standard follow-up was performed to minimize the risk of inflammation and infection and to ensure the target refractive outcome was achieved.
ICL explantation was performed by first instilling topical anesthesia followed by insertion of a lid speculum to maximize globe exposure. Viscoelastic was injected in AC. Then, the proximal end of the haptics of the ICL was dislocated. The ICL was then grasped with forceps and extracted from the AC.
Data were collected on patient demographics and clinical parameter including the cause of explantation, date of ICL implantation and explantation, surgical treatment at explantation and type of ICL.
The data were analyzed using Statistical Package for the Social Studies (SPSS 20.0) (IBM Corp., New York, NY, USA). The median and 25% quartile were calculated for continuous variables. Frequency and percentage proportions with 95% confidence interval (CI) were calculated for qualitative variables.
Results
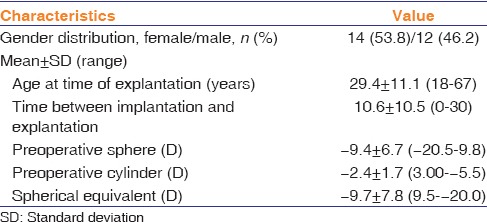
Of 787 ICLs (model V4b) implanted, 30 ICL (3.8%) in 26 patients (14 females) were explanted [Table 1]. The mean age at ICL explantation was 29.4 ± 11.1 years. The median interval between primary implantation and explantation was 15 months (25% quartile, 11 months). The median preoperative refractive status (spherical equivalent) was −10.6 D (25% quartile, −13.5 D).
Table 1.
Demographics and refractive parameters of patients who underwent implantable collamer lens explantation
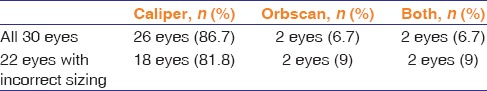
The overall explantation rate was 3.8% (95% CI: 2.6%-5.3%). The causes of explantation are presented in Figure 1. Of the 22 eyes with the incorrect ICL size, the caliper alone was used to measure white-to-white diameter for 18 (86%) eyes [Table 2]. The Orbscan II (Bausch and Lomb Inc., Rochester, NY, USA) alone was used in 2 (7%) eyes, and both were used in 2 (7%) eyes.
Figure 1.
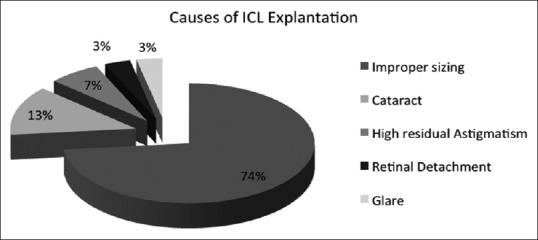
Causes for explantation of phakic implantable collamer lens used for treatment of refractive error
Table 2.
Instruments used for white-to-white measurements
The median time from ICL implantation to explantation was 6.5 months, (25% quartile, 2 months). In the cases with incorrect ICL size, time from implantation to explantation was 8.9 ± 9.6 months (range, 0–30 months). In patients who developed an anterior subcapsular cataract, the median time from implantation to explantation was 13.5 months. Patients with high residual astigmatism underwent explantation 26.5 ± 0.70 months after ICL implantation. A patient with retinal detachment underwent ICL explantation 3 months after implantation. A patient with intolerable glare underwent explantation 1 month after ICL implantation.
Discussion
We found that the rate of explantation of ICL was 3.8%. This is higher than documented in other studies.[1,2,3,4] We also noted that most ICL explantations were performed within the first 2 years of the introduction of the ICL in our institute. This observation suggests a learning curve effect.
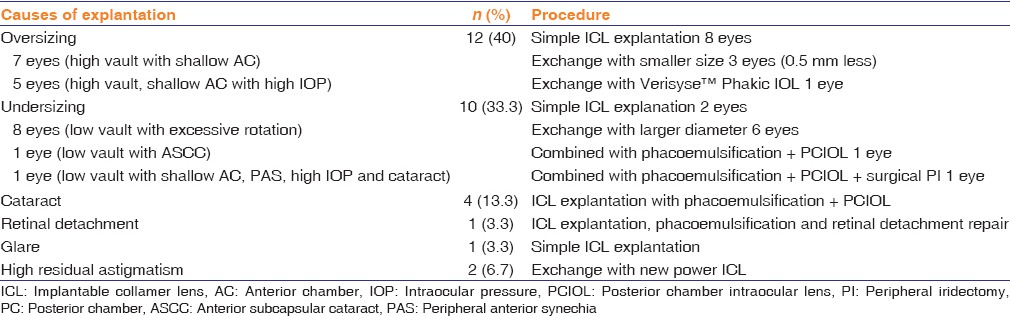
Improper sizing and poor vaulting were the main causes of ICL explantation in our study [Table 3]. ICL explantation due to improper sizing was <0.8% in the USA compared to our study (2.8%).[1] In the current study, calipers and the Orbscan II were used for CD measurement. CD measured by these methods did not differ in a study by Choi et al.[5] In this study, caliper was used in the majority of patients. We believe that ICL sizing with a caliper could be inadequate for several reasons. First, the sulcus diameter based on the white-to-white measurement may be inaccurate.[6] Second, there could be surgeon variability in detecting the exact sites for white-to-white measurement. Finally, the calibration of the instrument may not be accurate. The Orbscan II, in contrast, could overestimate the white-to-white measurement in cases with limbal pigmentation. Thus, both these methods have limitations in measuring CD.
Table 3.
Causes of implantable collamer lens explantation and surgical techniques
Accurate measurement of sulcus-to-sulcus diameter is a significant issue for ICL implantation because the anterior segment is not circular. It is well documented that the horizontal and vertical sulcus-to-sulcus measurements may differ.[7] We measured the white-to-white diameter and used it as an accurate representation of the sulcus-to-sulcus diameter. This assumption may have been another source of error. Perhaps, ultrasound biomicroscopy for measuring the sulcus-to-sulcus diameter could solve this issue in the future.[5]
The development of cataract due to ICL (V4 model) implantation in our study was 0.5%. This rate was well within the rates reported internationally that vary between 0.0% and 2.4%.[1,8] Anterior subcapsular cataract after ICL implantation is attributed to subclinical inflammation, disruption of the blood-aqueous barrier, laser-induced trauma, or accidental instrument touch. A decrease in ICL vault by 1 year postoperatively may also induce microtrauma and cataract.[9]
In our series, only one case required ICL explantation due to night vision symptoms. Chang and Meau[8] have reported glare is mainly due to peripheral iridectomies and glare decreases over 6 months (or later) postoperatively.
The rate of retinal detachment in our study was on par with reports from the USA.[1] High myopia and preexisting myopic degeneration likely contributed to eventual detachment in these eyes rather than the ICL procedure itself.
Conclusion
Phakic ICL is a common type of refractive surgery, with less than a 5% rate of explantation in our series. Improper sizing was the main cause of ICL explantation. More accurate methods for selecting a correctly sized ICL could further reduce the explantation rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sanders DR, Vukich JA, Doney K, Gaston M. Implantable Contact Lens in Treatment of Myopia Study Group. U.S. food and drug administration clinical trial of the implantable contact lens for moderate to high myopia. Ophthalmology. 2003;110:255–66. doi: 10.1016/s0161-6420(02)01771-2. [DOI] [PubMed] [Google Scholar]
- 2.Almalki S, Abubaker A, Alsabaani NA, Edward DP. Causes of elevated intraocular pressure following implantation of phakic intraocular lenses for myopia. Int Ophthalmol. 2016;36:259–65. doi: 10.1007/s10792-015-0112-4. [DOI] [PubMed] [Google Scholar]
- 3.Khalifa YM, Goldsmith J, Moshirfar M. Bilateral explantation of visian implantable collamer lenses secondary to bilateral acute angle closure resulting from a non-pupillary block mechanism. J Refract Surg. 2010;26:991–4. doi: 10.3928/1081597X-20100521-01. [DOI] [PubMed] [Google Scholar]
- 4.Pesando PM, Ghiringhello MP, Tagliavacche P. Posterior chamber collamer phakic intraocular lens for myopia and hyperopia. J Refract Surg. 1999;15:415–23. doi: 10.3928/1081-597X-19990701-05. [DOI] [PubMed] [Google Scholar]
- 5.Choi KH, Chung SE, Chung TY, Chung ES. Ultrasound biomicroscopy for determining visian implantable contact lens length in phakic IOL implantation. J Refract Surg. 2007;23:362–7. doi: 10.3928/1081-597X-20070401-08. [DOI] [PubMed] [Google Scholar]
- 6.Pop M, Payette Y, Mansour M. Predicting sulcus size using ocular measurements. J Cataract Refract Surg. 2001;27:1033–8. doi: 10.1016/s0886-3350(00)00830-0. [DOI] [PubMed] [Google Scholar]
- 7.Werner L, Lovisolo C, Chew J, Tetz M, Müller M. Meridional differences in internal dimensions of the anterior segment in human eyes evaluated with 2 imaging systems. J Cataract Refract Surg. 2008;34:1125–32. doi: 10.1016/j.jcrs.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 8.Sanders DR, Doney K, Poco M. ICL in Treatment of Myopia Study Group. United States food and drug administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: Three-year follow-up. Ophthalmology. 2004;111:1683–92. doi: 10.1016/j.ophtha.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 9.Chang JS, Meau AY. Visian collamer phakic intraocular lens in high myopic Asian eyes. J Refract Surg. 2007;23:17–25. doi: 10.3928/1081-597X-20070101-05. [DOI] [PubMed] [Google Scholar]


