Abstract
Aims and Objectives:
The aim and objective of this study was to establish the relationship of oral health-related quality of life (OHRQoL) as assessed by the Child Perception Questionnaire (CPQ 11–14) with the Index of Orthodontic Treatment Need (IOTN) and the child's apprehension with his/her dental appearance and how upset the child would feel if he/she is unable to obtain orthodontic treatment.
Materials and Methods:
An observational cross-sectional study was conducted among 604 children between the age group of 10–14 years to analyze the effect of malocclusion on the quality of life of children on the basis of impact on oral symptoms, functional limitation, emotional well-being, and social well-being. Malocclusion was evaluated using the IOTN, and the CPQ 11–14 was used to study the OHRQoL in children. The collected data were then subjected to statistical analysis.
Statistical Analysis:
Spearman's correlation coefficient was used to analyze the data statistically.
Results:
Out of the 604 children examined, boys showed effect on emotional well-being, whereas girls showed a significant correlation on both emotional and social well-being. There was a statistically significant correlation between IOTN and all the four domains of CPQ scores with respect to the two questions that were added to the CPQ questionnaire.
Conclusion:
A questionnaire when developed specifically for determining the effect of malocclusion on OHRQoL focusing more on emotional and psychological impact and less on oral symptoms and functional limitation will provide advantages of having limited questions, being less time-consuming, and providing better understanding of the patients’ concern.
Keywords: Child Perception Questionnaire 11-14, Index of Orthodontic Treatment Need, malocclusion, oral health-related quality of life
Introduction
The facial features that are most closely linked with physical attractiveness are the eyes and the mouth. The appearance and the position of teeth are factors that have greater psychological and social impact on children and young adults, since the appearance of the face has a vital role in building a good human life and stable relationships.[1]
Individuals with malaligned teeth, particularly in the anterior region, may require orthodontic management to improve esthetics, oral health, and dental function. Malocclusion has been evaluated traditionally with the help of normative indices. However, of all the oral problems studied, influence on psychosocial component is widely seen with malocclusion. Unfortunately, despite the fact that orthodontic treatment is mostly carried out to improve a person's social well-being, normative measures such as occlusal indices or cephalometric measurements have been used to analyze the acceptance and effectiveness of orthodontic treatment. This system takes into account only the professional viewpoint and not the patients’ personal or social requirements. In addition, it places minimal emphasis on patients’ perception of the difference that orthodontic treatment may make in their lives.[2] Hence, it is necessary to understand the subjective perception of patients to analyze the impact of malocclusion on the quality of life of children. This can be done by using standardized measures of child oral health-related quality of life (OHRQoL) such as Child Perceptions Questionnaire (CPQ 11-14). The impact of malocclusion is influenced by both orthodontic treatment need as well as subjective aspects. Hence, a dual approach that involves both clinician and patients’ perception is required to evaluate the need of orthodontic treatment.
It has been established that OHRQoL improved significantly following orthodontic treatment.[3] Investigations into esthetic alterations stemming from malocclusion are particularly important for a better assessment of treatment needs and for predicting the demand for public resources.[2] However, orthodontic treatment is elective as well as expensive, and Indian public health-care services do not offer orthodontic treatment. When planning new oral health initiatives, public health services should include malocclusions, since these are of high prevalence in our country and have an effect on the quality of life. Incisal crowding, an anterior maxillary irregularity, and increased overjet deserve special attention due to their great potential for causing social embarrassment and a possible decrease in the self-regard of individuals due to dissatisfaction with appearance. This becomes especially relevant among adolescents and young adults, in whom physical attractiveness has a vital role to play in social relationships.
There have been studies conducted that analyze the impact of malocclusion on the quality of life of children. However, as the cultural standards regarding dental esthetics may vary between countries and regions, the degree of attractiveness and the treatment need probably would change as well. Hence, there is a need to evaluate the impact on children from different parts of the country which are culturally varied compared with studies conducted within the same country and across different countries.[2] The present study was conducted to assess the influence of malocclusion on the quality of life using both normative indices (Index of Orthodontic Treatment Need [IOTN]) and subjective perception (CPQ 11-14) in children of Navi Mumbai, Maharashtra, India.
Materials and Methods
An observational cross-sectional study was conducted to evaluate the effect of malocclusion on the quality of life of children on the basis of impact on oral symptoms, functional limitation, emotional well-being, and social well-being. The study was conducted in schoolchildren in Navi Mumbai, Maharashtra, India. Totally 604 children between the age group of 10 and 14 years were selected for the study. Children with altered mental status, history of chronic illness, any existing medical condition, and those who are undergoing or have undergone orthodontic treatment were excluded from the study.
Ethical clearance was obtained from the Institutional Ethical Committee. Parents/teachers of the children selected for the study, as well as the selected children were informed regarding the purpose of the study, and positive consent was obtained from them.
Information regarding the patients’ age and gender was recorded. Impact on OHRQoL was measured using CPQ 11-14. Two general questions about oral health which is a part of CPQ 11-14 were asked to the patients. This was followed by 37 questions pertaining to four domains, i.e. oral symptoms (6 items), functional limitation (9 items), emotional well-being (9 items), and social well-being (13 items) of CPQ 11-14 questionnaire. Questions were asked about the frequency of events in the past 3 months in relation to child's oral/orofacial condition. The response options were never (0), once/twice (1), sometimes (2), often (3), and everyday/almost every day (4).
Two additional questions focusing on malocclusion were added to determine child's interest in undergoing orthodontic treatment. These were as follows:
How bothered are you about how straight your teeth are at the moment?[4]
How upset will you be if you are not able to get treatment from the dentist to straighten your teeth?[4]
The responses were recorded on 5-point Likert scale.
All questions were asked by a single examiner using regional language to assist the child in understanding the questions. The four domain scores were computed by adding up all the item responses in a particular domain, and the overall CPQ 11–14 score was computed by summing up the four domain scores. The total score ranged from 0 (no impact of oral conditions on OHRQoL) to 148 (maximum impact of oral condition on OHRQoL).
IOTN was used to measure malocclusion. Both components of IOTN, i.e., dental health component (DHC) and esthetic component (AC) were recorded for the children.
DHC was recorded on a scale of 1–5; 1 being no need and 5 being great need of orthodontic treatment. This grade was obtained with the help of IOTN scale which helps in measuring the severity of malocclusion and quantifying it.
Treatment needs of the patients were categorized as follows:
IOTN Grade 1 - No treatment need
IOTN Grade 2 - Little treatment need
IOTN Grade 3 - Borderline treatment need
IOTN Grade 4 - Orthodontic treatment desirable
IOTN Grade 5 - Orthodontic treatment mandatory.
After allotting DHC grade to the patient, the patient was evaluated for AC. To achieve this, cheek retractor was placed, and the patient was asked to close the mouth in centric occlusion. This provided better view of the front teeth to assist both the child and the examiner while recording AC. The AC includes 10 dental-colored photographs showcasing the attractiveness of occlusion (Grade 1 is the most attractive and Grade 10 is the least attractive). Each student was asked to point at the photograph that showed maximum resemblance to his/her dental appearance. This gave us the self-perceived AC or AC of the child (CAC). The examiner also objectively selected a photograph that closely resembled the child's dental esthetics. This gave us the examiner AC (EAC).
The need for treatment was assessed based on the following factors:
EAC ≥6
Self-perceived AC (CAC) ≥6
DHC ≥3
The child being bothered, very bothered, or extremely bothered by how straight his/her teeth are
The child being upset, very upset, or extremely upset if he/she was unable to receive orthodontic treatment.
Statistical analysis
The data collected were entered into an excel sheet to carry out statistical analysis. The Excel and SPSS software (version 16, IBM company, New York, USA) were used for data analysis.
Results
The study was conducted to assess the impact of malocclusion on the quality of life of children aged 11–14 years residing in Navi Mumbai, Maharashtra. Data of 604 children were collected, of which 298 (49.3%) were boys and 306 (50.7%) were girls. Tables 1 and 2 show the frequency distribution of IOTN (DHC, EAC, and CAC) for the total sample. Tables 3–5 show correlation between CPQ and IOTN and the questions specifically related to malocclusion.
Table 1.
Frequency distribution of dental health component of the total sample
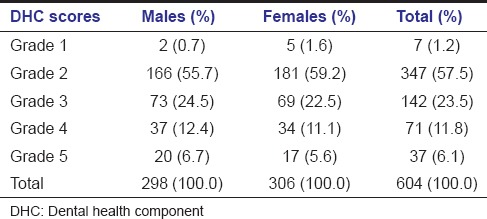
Table 2.
Frequency distribution of examiner esthetic component and child esthetic component for the total sample
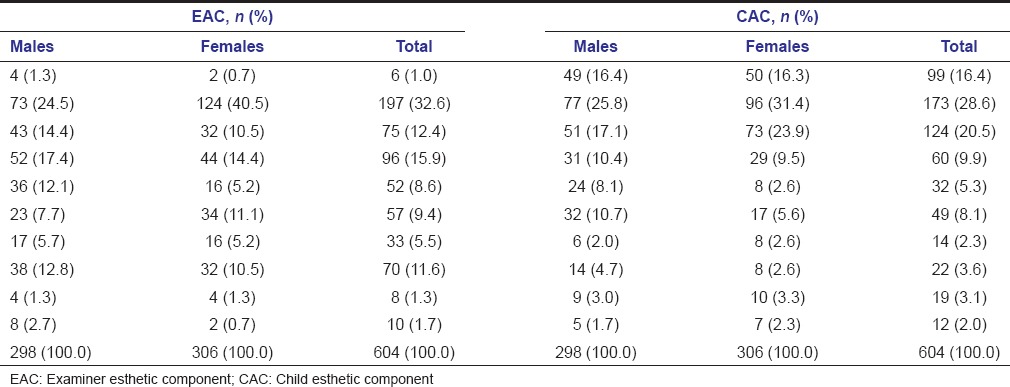
Table 3.
Correlations between the Index of Orthodontic Treatment Need and Child Perception Questionnaire for the total sample Spearman's rho
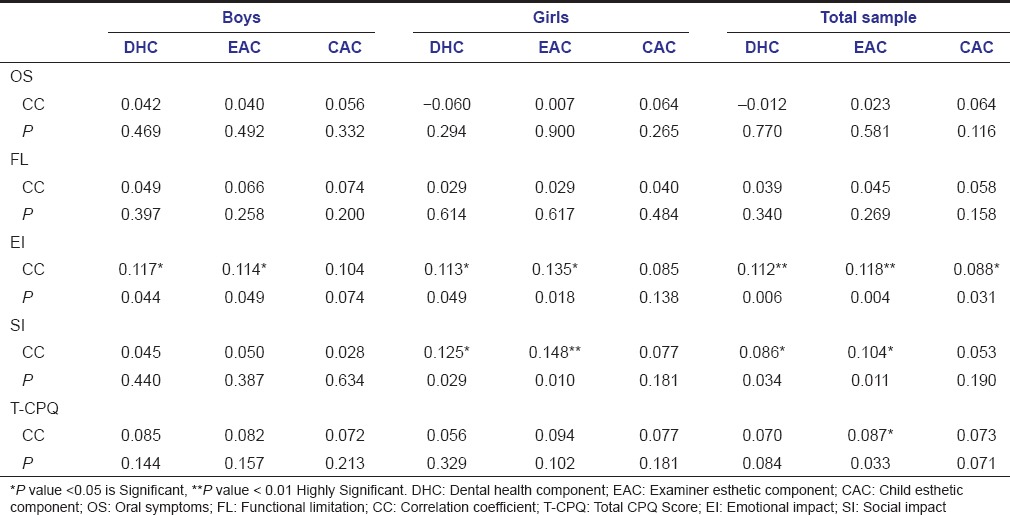
Table 5.
Correlations between responses of the question “How upset the child would be if he/she was unable to receive orthodontic treatment?” with the Index of Orthodontic Treatment Need and Child Perception Questionnaire for total sample
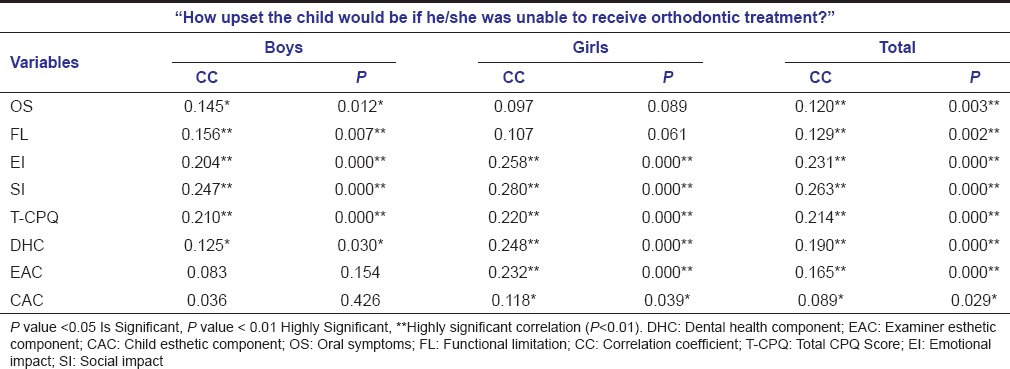
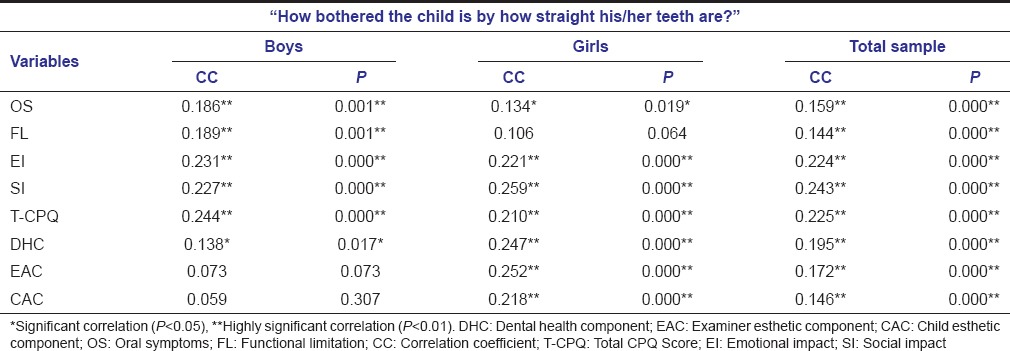
Table 4.
Correlations between responses of the question “How bothered the child is by how straight his/her teeth are?” and Index of Orthodontic Treatment Need and Child Perception Questionnaire scores for total sample
Discussion
Children of age 11–14 were selected for the study. It is important to evaluate schoolchildren presenting both in the late mixed dentition and early permanent dentition, as an early diagnosis may facilitate early treatment which in turn provides better treatment stability. Kragt et al. observed that the children between the age of 11 and 14 years were more likely to show impact of malocclusion on OHRQOL as compared to younger age group.[5]
The index used to assess malocclusion in our study was the IOTN. IOTN includes two components: The DHC and the AC. DHC is highly reproducible, allows faster application and easy usage.[6] The significance of AC is that it evaluates the AC of the malocclusion and enlightens us with the subjective impact of it.[7] It has been established that the dental concern expressed using the AC correlates with the demand for treatment. The time taken to record the IOTN was 1 min. However, in case there were several minor traits to be diagnosed, identifying the most severe trait and allocating a grade took 3 min as given by Shaw et al. in 1991.[8] The diagnostic accuracy of IOTN has been proven to be 98.6%.[9] Considering these advantages, assessment of prevalence of malocclusion and orthodontic treatment need using IOTN in schoolchildren aged 11–14 years was carried out.
The Child Oral Health Quality of Life Questionnaire (COHQoL) is a set of multidimensional questions measuring the effects of oral health on the functional, emotional, and social well-being of children and their families. The COHQoL consists of the Parental-Caregiver Perceptions Questionnaire, the family impact scale, and three age-specific questionnaires for children (CPQs). CPQ 11–14 was used for this study as it is specifically made for children in the age group of 11–14. The validity and reliability of CPQ 11–14 have been proven by Jokovic et al. in 2002[10] and O’Brien et al. in 2006.[11] The average time taken for recording the CPQ 11–14 in our study was 10 min.
The prevalence of malocclusion according to DHC Grades 3, 4, and 5 in our study was 41.4% for the total sample and 29.5% and 19.1% according to EAC and CAC 6–10, respectively. However, the aim of our study was not to find the prevalence of malocclusion in the region and thus, the percentage only describes the prevalence in our studied sample.
In our study, children graded themselves with AC score less than that of the examiner. The results of our study correspond with many other studies as that of Kerosuo et al. in 2004[12] and Abu Alhaija et al. in 2005,[13] where correlation was found between the students’ and EAC scores, and students were less critical in evaluating their esthetic appearance.
The data distribution of the four domains of CPQ revealed that boys and girls were equally affected on all the four domains of CPQ 11–14, namely, oral symptoms, functional limitation, emotional well-being, and social well-being. The result corroborates with previous studies by de Paula Júnior et al. in 2009[14] and Tessarollo et al. in 2012.[15] The correlation of individual components of IOTN with CPQ revealed highly significant correlation between emotional well-being and DHC and EAC. The correlation with CAC was weaker as compared to DHC and EAC but still statistically significant [Table 3]. This is in accordance to a study by Shue-Te Yeh et al. in 2000[16] and Grywacz in 2003[17] that showed E-AC to be a good predictor of subjective orthodontic treatment need. However, the result contradicts to those obtained by Kok et al. in 2004[4] which shows CAC to be a better predictor. This difference could be because children might not be able to relate their malocclusion to the 10 photographs of AC. There are no photographs for various malocclusions such as reverse overjet or anterior crossbite in the AC and also overjet is difficult to understand in the two-dimensional photographs. In addition, in our study, it was noted that boys showed impact only on emotional well-being whereas girls showed impact on both emotional and social well-being. To the best of our knowledge, this is an exclusive finding of our study.
CPQ 11–14 was not developed specifically for malocclusion, and symptoms such as pain and bleeding are not correlated to malocclusion and can be due to other oral conditions. Items in the oral symptom and functional limitation domains are generic and affected more by other oral conditions, whereas the emotional and social well-being domains contain items that could be affected mainly due to malocclusion.[18] To overcome these drawbacks, additional questions specifically aimed at malocclusion were added in our study to the CPQ questionnaire. The additional questions included were “How bothered are you about how straight your teeth are at the moment?” and “How upset will you be if you are not able to get treatment from the dentist to straighten your teeth?” to understand the orthodontic concern among children.[4] These questions helped in evaluating the child's perceived need for treatment. In addition, these questions about malocclusion were directly asked to children and prevented any ambiguity of the impact on quality of life for some other dental problem. The additional questions of malocclusion revealed that 35% were bothered about the alignment of their teeth and 29% would be upset if they were unable to receive orthodontic treatment. There was no significant difference with relation to gender, indicating boys and girls were equally interested in undergoing orthodontic dental treatment.
These additional questions showed statistically significant correlation with all the four domains of CPQ as well as DHC of IOTN. In boys, the correlation between the questions and EAC and CAC was not significant, but all the four domains of CPQ showed a significant correlation. However, in girls, there was no correlation between functional limitations and the questions specifically asked regarding orthodontic treatment. In addition, oral symptom domain did not have a significant correlation with the question – How upset would you be if you are unable to receive orthodontic treatment.
There was a high significant impact on the emotional well-being and social well-being of children aged 11–14 years. Thus, it can be derived that the impact of malocclusion is less on oral symptoms and functional limitations as compared to emotional and social impact. Hence, the quality of life questionnaire for malocclusion should focus more on these two domains. Till date, all the questionnaires of OHRQoL are generic and not made specifically for different dental problems. The need of the hour is to have a questionnaire that specially focuses on specific dental problem being studied because problems such as dental caries and periodontal problems may show more impact on oral symptoms and functional limitations unlike malocclusion that shows more emotional and psychological impact. A questionnaire when developed specifically for malocclusion will provide advantages of having limited questions, being less time-consuming, and providing better understanding of the patients’ concern.
Conclusion
Children tended to give themselves AC score lower than the examiner
There was a high significant correlation between emotional well-being and DHC and EAC
EAC was a better predictor of social and emotional impact as compared to CAC
Boys showed impact only on emotional well-being, but girls showed on both emotional and social well-being.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Traebert ES, Peres MA. Do malocclusions affect the individual's oral health-related quality of life? Oral Health Prev Dent. 2007;5:3–12. [PubMed] [Google Scholar]
- 2.de Oliveira CM, Sheiham A, Tsakos G, O’Brien KD. Oral health-related quality of life and the IOTN index as predictors of children's perceived needs and acceptance for orthodontic treatment. Br Dent J. 2008;204:1–5. doi: 10.1038/bdj.2008.239. [DOI] [PubMed] [Google Scholar]
- 3.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–8. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kok YV, Mageson P, Harradine NW, Sprod AJ. Comparing a quality of life measure and the aesthetic component of the Index of Orthodontic Treatment Need (IOTN) in assessing orthodontic treatment need and concern. J Orthod. 2004;31:312–8. doi: 10.1179/146531204225020625. [DOI] [PubMed] [Google Scholar]
- 5.Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM. The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig. 2015 doi: 10.1007/s00784-015-1681-3. Epub ahead of print. doi: 10.1007/s00784-015-1681-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.So LL, Tang EL. A comparative study using the occlusal index and the index of orthodontic treatment need. Angle Orthod. 1993;63:57–64. doi: 10.1043/0003-3219(1993)063<0057:ACSUTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Richmond S. A Critical Evaluation of Orthodontic Treatment in the General Dental Services of England and Wales, PhD Thesis. University of Manchester. 1990 [Google Scholar]
- 8.Shaw WC, Richmond S, O’Brien KD, Brook P, Stephens CD. Quality control in orthodontics: indices of treatment need and treatment standards. Br Dent J. 1991;170:107–12. doi: 10.1038/sj.bdj.4807429. [DOI] [PubMed] [Google Scholar]
- 9.Younis JW, Vig KW, Rinchuse DJ, Weyant RJ. A validation study of three indexes of orthodontic treatment need in the United States. Community Dent Oral Epidemiol. 1997;25:358–62. doi: 10.1111/j.1600-0528.1997.tb00955.x. [DOI] [PubMed] [Google Scholar]
- 10.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–63. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien K, Wright JL, Conboy F, Macfarlane T, Mandall N. The child perception questionnaire is valid for malocclusions in the United Kingdom. Am J Orthod Dentofacial Orthop. 2006;129:536–40. doi: 10.1016/j.ajodo.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Kerosuo H, Al Enezi S, Kerosuo E, Abdulkarim E. Association between normative and self-perceived orthodontic treatment need among Arab high school students. Am J Orthod Dentofacial Orthop. 2004;125:373–8. doi: 10.1016/j.ajodo.2003.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Abu Alhaija ES, Al-Nimri KS, Al-Khateeb SN. Self-perception of malocclusion among North Jordanian school children. Eur J Orthod. 2005;27:292–5. doi: 10.1093/ejo/cjh094. [DOI] [PubMed] [Google Scholar]
- 14.de Paula Júnior DF, Santos NC, da Silva ET, Nunes MF, Leles CR. Psychosocial impact of dental esthetics on quality of life in adolescents. Angle Orthod. 2009;79:1188–93. doi: 10.2319/082608-452R.1. [DOI] [PubMed] [Google Scholar]
- 15.Tessarollo FR, Feldens CA, Closs LQ. The impact of malocclusion on adolescents’ dissatisfaction with dental appearance and oral functions. Angle Orthod. 2012;82:403–9. doi: 10.2319/031911-195.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shue-Te Yeh M, Koochek AR, Vlaskalic V, Boyd R, Richmond S. The relationship of 2 professional occlusal indexes with patients’ perceptions of aesthetics, function, speech, and orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2000;118:421–8. doi: 10.1067/mod.2000.107008. [DOI] [PubMed] [Google Scholar]
- 17.Grzywacz I. The value of the aesthetic component of the index of orthodontic treatment need in the assessment of subjective orthodontic treatment need. Eur J Orthod. 2003;25:57–63. doi: 10.1093/ejo/25.1.57. [DOI] [PubMed] [Google Scholar]
- 18.Dawoodbhoy I, Delgado-Angulo EK, Bernabé E. Impact of malocclusion on the quality of life of Saudi children. Angle Orthod. 2013;83:1043–8. doi: 10.2319/012713-83.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


