Abstract
Background:
Gingival recession indicates oral display of the root surface due to apical movement of gingival margin. Coronally advanced flap (CAF) is often used periodontal plastic surgical technique to accomplish root coverage. The purpose of this clinical trial is to assess and compare the effectiveness of modified CAF with orthodontic button application (CAF+B) and without orthodontic button application (CAF) for the correction of multiple recession defects.
Materials and Methods:
Twenty patients exhibiting bilateral multiple proximate Millers Class I and/or Class II gingival recession defects were included in the study. Each set of proximate recession defects was designated randomly to test or control group. Control group was treated by CAF alone and test group by CAF+B. Baseline and postoperative clinical parameters at 2, 4, and 6 months time interval were recorded.
Results:
Mean root coverage percentage from baseline to 6 months in control group was 78.30% ± 20.75% and in test group was 92.23% ± 15.6%. Complete root coverage was 43.8% in control group and 77.47% in test group. Visual analog scale pain measurements did not reveal any difference among both the groups. Patient satisfaction with esthetics was very high in CAF+B group when compared with CAF group.
Conclusion:
Both treatment modalities, i.e., CAF and CAF+B are effectual in the treatment of proximate Miller's Class I and Class II gingival recession defects, but CAF+B showed significantly superior clinical results.
Keywords: Esthetics, gingival recession, guided tissue regeneration, orthodontic
Introduction
Gingival recession designates the oral exposure of root surface owing to migration of gingival margin (GM) apical to the cementoenamel junction (CEJ).[1] The primary causes of gingival recession are periodontal diseases and improper oral hygiene measures including a variety of other etiological factors such as tooth malpositions, friction from soft tissues, gingival inflammation, thin bony plates, and bone dehiscence.[2] Gingival recession may be a matter of relevance for clinicians and patients for a number of reasons such as erosion root caries, hypersensitivity, and esthetic reasons.[3] Treatment of gingival recession defects is mainly accorded to decrease root sensitivity and to enhance esthetics. It has been shown that preoperative recession depth is correlated with complete root coverage (CRC): The more the initial recession, the lesser the frequency of CRC.[4] Coronally advanced flap (CAF) is reliable and commonly used periodontal plastic surgical procedure to achieve root coverage.[5] Several authors have employed CAF by relocating the residual gingiva in a coronal direction alone or in association with free gingival or a connective tissue graft (CTG)[6,7,8] or with membranes, according to the principles of guided tissue regeneration.[9,10]
CAF along with CTG is one of the most successful and acceptable treatment options for the correction of an isolated type of gingival recession defect.[11] However, disadvantages of using CTG includes the necessity of the second surgical site and morbidity linked with procuring the autogenous palatal donor mucosa. In contrast, the CAF is a root coverage surgery that does not require a palatal donor site and has been confirmed to be safe and predictable.[12]
Recently, Zucchelli et al. have suggested modified CAF technique for the resolution of multiple adjacent recession-type defects (MARTD).[12] Another important observation reported in an earlier study is that the location of GM at the end of the surgery appeared to have an influence on attaining CRC. Suturing the GM at least 2 mm coronal to the CEJ resulted in CRC.[4]
Since it is important and technically difficult to achieve and protect the most possible coronal position of the GM in immediate postoperative phase with periodontal plastic surgery method alone, orthodontic buttons were applied in this study. The purpose of this randomized, controlled clinical trial is, therefore, to evaluate and compare the effectiveness of modified CAF procedure with (CAF+B) and without (CAF) orthodontic button application for the treatment of multiple Miller Class I and Class II recession-type defects.
Materials and Methods
Sample size and selection criteria
A split-mouth randomized clinical trial was planned and implemented to compare the clinical performance of CAFs with or without orthodontic button application for the treatment of multiple gingival recession defects. Twenty systemically and periodontally healthy patients with bilateral Millers Class I and II multiple gingival recession defects with ≥1 mm of attached gingiva and probing pocket depth ≤3 mm at gingival recession sites were included in this study (with α error 10% and power of 80% the sample size was estimated as twenty in each group). The study patients were selected on a consecutive basis and treated between September 2014 and October 2015 in the Department of Periodontics and Implantology at VSPM's Dental College and Research Centre, Nagpur, India. All the patients were required to sign a consent letter before being enrolled. The study was conducted after the clearance from the Institutional Ethics Committee. The study protocol satisfied the provisions of Helsinki Declaration. The study was registered with Clinical Trial Registry with no CTRI/2016/01/006543.
Patients with a history of any known systemic disease, smoking, recession defects associated with caries, drug usage that would alter the healing response of the oral tissues, and patients with history of any kind of periodontal treatment in the past 6 months were excluded from the study.
Randomization
The patients were assigned into two treatment groups, i.e., Group I and Group II. The Group I acted as control group and Group II as test group. The participants in test group were treated with CAF+B while the participants in control group were treated by CAF alone. The randomization was achieved by the toss of a coin before the surgery of each patient. The outcome of coin toss was written on paper, which was put in the opaque envelope by a blinded staff (Abhay Kolte), which contained the treatment information for the specific patient. It was opened at the time of surgery by surgeon (Sumedh Khobragade), immediately after completing treatment of the root surfaces to prevent surgeon bias. So both, surgeon and participants were blinded about the intervention group.
Presurgical therapy and clinical measurements
The study population was subjected to instructions in oral hygiene, ultrasonic instrumentation, and coronal polishing and the plaque index (Turesky–Gilmore–Glickman modification of Quigley-Hein 1970)[13] and gingival index (Loe and Silness 1963)[14] were recorded.
Clinical recordings were performed at baseline, 2, 4, and 6 months after surgery, including; (1) Gingival recession depth (GRD) was measured as interspace between apical zenith of CEJ and GM, (2) probing depth (PD) was measured from the GM to depth of the gingival sulcus, (3) clinical attachment level (CAL) was measured as depth from CEJ to the bottom of sulcus, (4) width of keratinized tissue (KTW) being considered as distance from mucogingival junction (MGJ) to the GM, (5) Location of GM with respect to CEJ was calculated after suturing by deducting the distance between incisal margin and CEJ from the distance between incisal margin and GM, (6) Recession depth reduction, (7) mean root coverage, and (8) CRC.
All the measurements were carried out with UNC 15 periodontal probe (Hu-Friedy, Chicago, IL) by a single examiner (Rajashri Kolte) who was calibrated before the beginning of the present trail.
Surgical procedure
Surgical procedures were same for both groups and performed by the same operator. The CAF procedure used in this study has been detailed by Zucchelli et al.[12] Briefly, the flap design comprised two oblique, beveled divergent incisions performed at the mesial and distal line angles of the two peripheral teeth with gingival recessions, horizontal incisions performed mesial and distal to tooth with gingival recession and intrasulcular incision. The periodontal flap was elevated with a split-full-split design in the coronal-apical direction; the surgical papillae were split thickness in nature. Gingival tissue apical to the root exposures was raised full thickness and it was limited once 3–4 mm of bone was exposed. The most apical portion of the flap was raised split thickness to enable coronal displacement of the flap. The intact and undisturbed interdental papilla were scraped for deepithelization and create a raw bleeding bed for CAF. The flap was sutured by 5-0 nylon monofilament sutures (Ethicon, Johnson, and Johnson, Woluwe, Belgium) in apico-coronal direction to facilitate the coronal displacement of the flap and to lessen tenseness over last sutures. The final position of the flap margin was always coronal to CEJ of all teeth included in the design. For the protection of the surgical area, periodontal dressing was applied [Figure 1].
Figure 1.
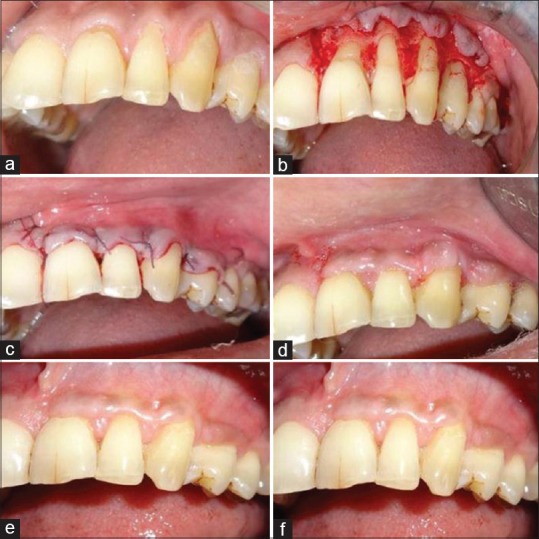
Surgical procedure in Group I (coronally advanced flap group), (a) teeth 21, 22, 23, 24 with gingival recession. (b) The flap extended to the most distal teeth with gingival recession on each side and elevated wit split-full-split approach. (c) Coronally advanced flap with sutures in position. (d) 2-month follow-up. (e) 4-month follow-up. (f) 6-month follow-up
For Group II, before the surgery, orthodontic buttons (Zhejiang Protect Medical Equipment Co., Ltd., Zhejiang Province, China) were applied on the teeth with gingival recession. The surgical procedure performed for recession defects in test group was same as that applied for the control group except that two types of sutures were used in test group; sling and stabilizing sutures. The sling 5-0 sutures with nylon monofilament were used to suspend the central area of the flaps on the buttons. The second 5-0 sutures were applied to establish a precise approximation and adaptation of the buccal flap on the convexity of crown surfaces. At the end of the surgery, the flap margins were a minimum of 3–4 mm coronal to the CEJ of all concerned teeth [Figure 2].
Figure 2.
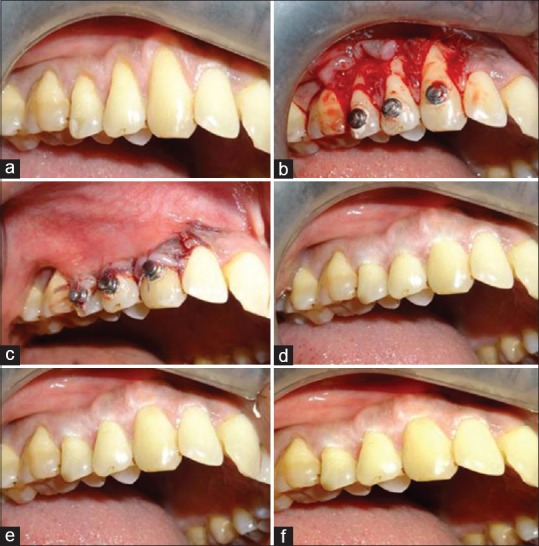
Surgical procedure in Group II (coronally advanced flap with orthodontic button application), (a) teeth 13, 14, and 15 with gingival recession. (b) The flap extended to the most distal teeth with gingival recession on each side and elevated with split-full-split approach. (c) The flap was maintained in coronally advanced position by suspended sutures around the orthodontic button at teeth. (d) 2-month follow-up. (e) 4-month follow-up. (f) 6-month follow-up
Postsurgical evaluation
Patient evaluation of postoperative discomfort and esthetics
Questions were asked to each patient for assessing the severity of the given event which was marked on a 100 mm visual analog scale (VAS). The questions were categorized into two parts: The first part, being postoperative morbidity evaluated 1 week after surgery based on a VAS (pain at immediate postoperative period [VAS-P]). The second part, related to patient satisfaction with the esthetic consequence evaluated at the 6-months follow-up visit based on a VAS (VAS-E).[10,15]
Evaluation of esthetic outcomes
The esthetic evaluation was performed according to the root coverage esthetic score (RES) system.[16] Five variables including GM, marginal tissue contour, soft tissue texture, MGJ alignment, and gingival color were evaluated.
Statistical analysis
The data were analyzed using the STATA version 13.0 (StataCorp LP, Texas, USA). P value was taken as statistically significant when <0.05. Descriptive statistics was expressed as the mean ± standard deviation for each parameter. Clinical parameters were compared at different time point postoperatively, within the group by performing two-way repeated measures of analysis of variance (ANOVA) and clinical parameters between the groups were compared by independent t-test and Mann–Whitney U-test. Post hoc comparisons were done by Tukey's test.
Results
Among the total study population of 20 patients (age range 22–45 years), 13 were male and 7 were female. Group I (control group) contributed 57 multiple gingival recession defects and were treated by CAF alone, and Group II (test group) contributed 59 multiple gingival recession which were treated by CAF+B.
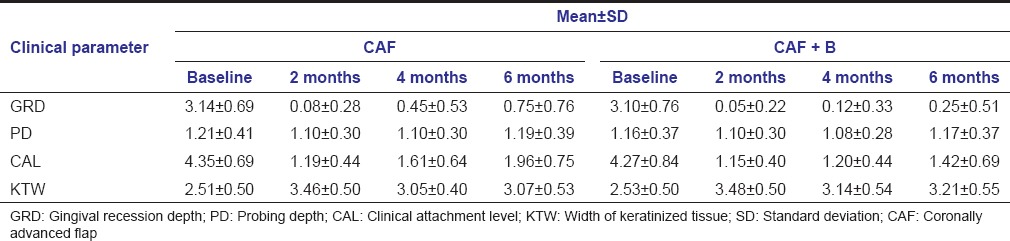
At baseline, no statistically significant differences in GRD, PD, CAL, and KTW were observed between Group I and Group II. Two-way repeated measures of ANOVA reveal statistically significant difference in GRD, CAL, and KTW when compared between baseline and 2, 4, and 6 months of follow-up [Table 1]. The analysis of mean difference of clinical parameters between baseline and different follow-up period exhibited significant difference among the groups for GRD and CAL (P < 0.0001 and P < 0.0001, respectively), with more GRD reduction and more CAL gain in Group II as compared to Group I.
Table 1.
Distribution of gingival recession depth, probing depth, clinical attachment level, width of keratinized tissue levels (in mm) between study groups at baseline and 2, 4, and 6 months postoperatively
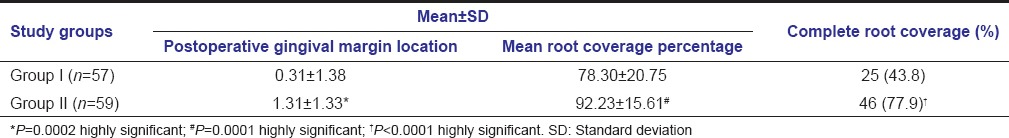
Group II exhibited more root coverage than Group I and this difference in root coverage was statistically highly significant (P < 0.0001). Similarly, in Group II, the final position of GM was more coronal to CEJ as compared to Group I [Table 2].
Table 2.
Distribution of the postoperative gingival margin location, root coverage percentage and complete root coverage between Group I and II at the end of 6 months
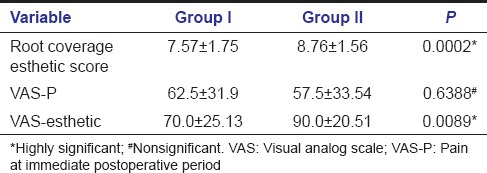
The RES score for Group I was 7.57 ± 1.75 and for Group II was 8.76 ± 1.56. This difference was found to be statistically highly significant (P < 0.001) showing better esthetic outcomes in Group II. The VAS-P scores show no statistically significant difference between the groups. Patients satisfaction with esthetic was evaluated at 6 months follow-up visit on VAS (VAS-E). VAS-E score indicates better patient satisfaction of treatment outcome observed in Group II [Table 3].
Table 3.
Distribution of root coverage esthetic score and visual analog scale -esthetic at 6 month postoperatively
Discussion
The present randomized controlled study was performed to evaluate and compare the clinical efficacy of CAF alone and CAF along with orthodontic button application in the treatment of multiple adjacent gingival recession defects.
The amount of biomaterials that is required for treatment of MARTD can be extensive, when compared to that required for treatment of single recession defects. The orthodontic button can be used in root coverage procedure as an anchorage on which sutures are suspended which provides maximum coronal placement of flap and accounts for stabilizing the flap in coronally advanced positions. CAF along with orthodontic button application is a procedure which is easy to perform, inexpensive, and highly acceptable as compared to the use of CTG, enamel matrix derivative, and acellular dermal matrix.[1]
The results of the present study indicate that utilization of CAF+B procedure aids in statistically significant GRD reduction as compared to CAF alone. It was revealed that a positive correlation exhibit between postoperative GM location and achieving CRC. The coronal advancement of the GM relative to CEJ following CAF+B procedure appears to augment the success of CRC. These results are in accordance with studies by Pini Prato et al. 2005, 1999 where they reported that the greater postoperative coronal displacement of the GM may ensure greater root coverage.[4,17] Pini Prato 2005 evaluated and observed that postsurgical location of GM is crucial factor for attaining CRC and a greater recession reduction was associated with greater coronal displacement of the flap. The results of the present study also demonstrated that application of CAF+B procedure increases the CRC rate in multiple gingival recession defects.
During all the time intervals, i.e., 2, 4, and 6 months, there was statistically significant reduction in GRD when compared to baseline. The results of the present study are similar to results of studies by Ozcelik et al. 2011 and da Silva et al. 2004.[1,18] In the present study, at the end of 6 months, the mean GRD reduction for Group I was 2.38 ± 054 mm and for Group II was 2.84 ± 0.84 mm. The differences in results between the present study and the previous studies in terms of amount of root coverage can be attributed to differences in gingival recession defects present at baseline which was greater in these studies.[19]
This study showed statistically significant gain in CAL in both the groups when compared to baseline with more gain in CAL in Group II. In addition, the CAL gain was more at end of 2 months as compared to 6 months of follow-up in both the groups. The reduction in CAL gain at 6 months can be attributed to apical shift of the GM, which might be related to the delicate and thinner dimensions of keratinized tissue achieved.[20] Cetiner et al. 2004 reported a higher gain in CAL as compared to the present study which can be accredited to the use of CTG along with CAF; such combination enables to achieve thicker dimensions of gingiva postoperatively which appears to be more resistant to the initial apical shift.[21]
In the present study, the increase in KTW can be explained by the fact that MGJ is genetically determined as it demarcates the junction between the basal bone and alveolar process.[15] This MGJ has tendency to reestablish itself to the original position leading to gain in KTW.[22,23]
The difference in percentage of root coverage was found to be statistically highly significant between both the groups. Twenty-five out of 57 (43.8%) treated sites showed CRC in Group I and 46 out of 59 (77.47%) of treated sites showed CRC in Group II. As esthetic analysis is extremely vital and subjective in root coverage procedures, two sets of measurement techniques were used. The VAS analysis was adapted to calibrate the patient satisfaction with esthetics. The patients treated with CAF+B technique showed increased satisfaction esthetically in comparison to patients treated with CAF. This finding is in agreement with the patient-centered assessment results, which demonstrated that the patients treated with CAF+B had significantly advantageous RES scores when collated with the CAF.
Some clinical and biological benefits of the procedure utilized in the current study might be attributed to the split-full-split flap elevation.[24] The split-thickness elevation at the level of the surgical papilla assures stability and blood supply in the interproximal areas mesial and distal to the root exposure; the full-thickness portion accords increased thickness, and thus provides enhanced chances to achieve root coverage; the more apical split-thickness flap elevation enables the coronal positioning of the flap. A long-term analysis on a larger study population is however desired to enable us to further substantiate the results.
Limitations
The following limitations were observed in the present study:
The sample size in the present study was limited to twenty bilateral multiple gingival recession defects. A greater sample size would be desirable so as to further substantiate the results
Long-term analysis is required to determine whether the initial positive results are maintained over a longer observation period.
Conclusion
Within the limits of the study, we can conclude that, both the treatment modalities, i.e., CAF and CAF+B, were effective in treatment of Miller's Class I and Class II multiple gingival recession defects and CAF+B showed significantly better results in terms GRD reduction, CAL gain and esthetic outcome of patients at 6 months, compared to CAF alone. The placement of GM and its stabilization during early healing stages appears to have a profound influence over the root coverage as well as the esthetic outcome achieved in such procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ozcelik O, Haytac MC, Seydaoglu G. Treatment of multiple gingival recessions using a coronally advanced flap procedure combined with button application. J Clin Periodontol. 2011;38:572–80. doi: 10.1111/j.1600-051X.2011.01724.x. [DOI] [PubMed] [Google Scholar]
- 2.Löe H, Anerud A, Boysen H. The natural history of periodontal disease in man: Prevalence, severity, and extent of gingival recession. J Periodontol. 1992;63:489–95. doi: 10.1902/jop.1992.63.6.489. [DOI] [PubMed] [Google Scholar]
- 3.Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, et al. Treatment of class III multiple gingival recessions: A randomized-clinical trial. J Clin Periodontol. 2010;37:88–97. doi: 10.1111/j.1600-051X.2009.01492.x. [DOI] [PubMed] [Google Scholar]
- 4.Pini Prato GP, Baldi C, Nieri M, Franseschi D, Cortellini P, Clauser C, et al. Coronally advanced flap: The post-surgical position of the gingival margin is an important factor for achieving complete root coverage. J Periodontol. 2005;76:713–22. doi: 10.1902/jop.2005.76.5.713. [DOI] [PubMed] [Google Scholar]
- 5.de Sanctis M, Zucchelli G. Coronally advanced flap: A modified surgical approach for isolated recession-type defects: Three-year results. J Clin Periodontol. 2007;34:262–8. doi: 10.1111/j.1600-051X.2006.01039.x. [DOI] [PubMed] [Google Scholar]
- 6.Matter J. Free gingival grafts for the treatment of gingival recession. A review of some techniques. J Clin Periodontol. 1982;9:103–14. doi: 10.1111/j.1600-051x.1982.tb01226.x. [DOI] [PubMed] [Google Scholar]
- 7.Raetzke PB. Covering localized areas of root exposure employing the “envelope” technique. J Periodontol. 1985;56:397–402. doi: 10.1902/jop.1985.56.7.397. [DOI] [PubMed] [Google Scholar]
- 8.Wennstrom JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2 year prospective clinical study. J Clin Periodontol. 1996;23:770–7. doi: 10.1111/j.1600-051x.1996.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 9.Tinti C, Vincenzi G, Cocchetto R. Guided tissue regeneration in mucogingival surgery. J Periodontol. 1993;64(11 Suppl):1184–91. doi: 10.1902/jop.1993.64.11s.1184. [DOI] [PubMed] [Google Scholar]
- 10.Trombelli L, Schincaglia G, Scapoli C, Calura G. Healing response of human buccal gingival recessions treated with expanded polytetrafluoroethylene membranes. A retrospective report. J Periodontol. 1995;66:14–22. doi: 10.1902/jop.1995.66.1.14. [DOI] [PubMed] [Google Scholar]
- 11.Zucchelli G, Mounssif I, Mazzotti C, Stefanini M, Marzadori M, Petracci E, et al. Coronally advanced flap with and without connective tissue graft for the treatment of multiple gingival recessions: A comparative short- and long-term controlled randomized clinical trial. J Clin Periodontol. 2014;41:396–403. doi: 10.1111/jcpe.12224. [DOI] [PubMed] [Google Scholar]
- 12.Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M. Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: A comparative controlled randomized clinical trial. J Periodontol. 2009;80:1083–94. doi: 10.1902/jop.2009.090041. [DOI] [PubMed] [Google Scholar]
- 13.Peter S. Turesky-Gilmore-Glickman modification of the Quigley-Hein plaque index. Preventive and Community Dentistry. 4th ed. New Delhi: Arya (Medi) Publishing House; 2009. pp. 322–5. [Google Scholar]
- 14.Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(6):610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 15.Ainamo A, Bergenholtz A, Hugoson A, Ainamo J. Location of the mucogingival junction 18 years after apically repositioned flap surgery. J Clin Periodontol. 1992;19:49–52. doi: 10.1111/j.1600-051x.1992.tb01148.x. [DOI] [PubMed] [Google Scholar]
- 16.Cairo F, Rotundo R, Miller PD, Pini Prato GP. Root coverage esthetic score: A system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol. 2009;80:705–10. doi: 10.1902/jop.2009.080565. [DOI] [PubMed] [Google Scholar]
- 17.Pini Prato G, Baldi C, Pagliaro U, Nieri M, Saletta D, Rotundo R, et al. Coronally advanced flap procedure for root coverage. Treatment of root surface: Root planning versus polishing. J Periodontol. 1999;70:1064–76. doi: 10.1902/jop.1999.70.9.1064. [DOI] [PubMed] [Google Scholar]
- 18.da Silva RC, Joly JC, de Lima AF, Tatakis DN. Root coverage using the coronally positioned flap with or without a subepithelial connective tissue graft. J Periodontol. 2004;75:413–9. doi: 10.1902/jop.2004.75.3.413. [DOI] [PubMed] [Google Scholar]
- 19.Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: A systematic review. J Clin Periodontol. 2002;29(Suppl 3):178–94. doi: 10.1034/j.1600-051x.29.s3.11.x. [DOI] [PubMed] [Google Scholar]
- 20.Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J Clin Periodontol. 2008;35(8 Suppl):136–62. doi: 10.1111/j.1600-051X.2008.01267.x. [DOI] [PubMed] [Google Scholar]
- 21.Cetiner D, Bodur A, Uraz A. Expanded mesh connective tissue graft for the treatment of multiple gingival recessions. J Periodontol. 2004;75:1167–72. doi: 10.1902/jop.2004.75.8.1167. [DOI] [PubMed] [Google Scholar]
- 22.Karring T, Ostergaard E, Löe H. Conservation of tissue specificity after heterotopic transplantation of gingiva and alveolar mucosa. J Periodontal Res. 1971;6:282–93. doi: 10.1111/j.1600-0765.1971.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 23.Lundberg M, Wennström JL. Development of gingiva following surgical exposure of a facially positioned unerupted incisor. J Periodontol. 1988;59:652–5. doi: 10.1902/jop.1988.59.10.652. [DOI] [PubMed] [Google Scholar]
- 24.Zucchelli G, De Sanctis M. Treatment of multiple recession-type defects in patients with esthetic demands. J Periodontol. 2000;71:1506–14. doi: 10.1902/jop.2000.71.9.1506. [DOI] [PubMed] [Google Scholar]


