Abstract
Anxiety is a common yet frequently overlooked psychiatric symptom in patients with ESRD treated with hemodialysis (HD). Anxiety is characterized by disruptive feelings of uncertainty, dread, and fearfulness. A variety of common medical complaints may be manifestations of an anxiety disorder, including palpitations, tremors, indigestion, numbness/tingling, nervousness, shortness of breath, diaphoresis, and fear. It is essential for the clinician to rule out specific medical conditions, including cardiovascular, pulmonary, and neurologic diseases, before ascribing these symptoms to an anxiety disorder. In addition, there is considerable overlap between the symptoms of anxiety and those of depression and uremia. This psychiatric condition has a significant adverse impact on patients’ perception of quality of life. Little is known regarding the prevalence and impact of anxiety disorders in patients with ESRD treated with HD; however, many of the seemingly irrational behaviors of patients, or behaviors which place them in conflict with staff and physicians, such as behavioral noncompliance, may be the expression of an underlying anxiety disorder. In this review, we present three clinical vignettes, highlighting the impact of anxiety disorders in patients with ESRD treated with HD.
Keywords: Hemodialysis, anxiety, benzodiazepine, Anxiety Disorders, depression, Depressive Disorder, Dyspepsia, Dyspnea, Fear, Humans, Hypesthesia, Kidney Failure, Chronic, Prevalence, quality of life, renal dialysis, Tremor, Uncertainty, uremia
Anxiety: Symptom and Diagnosis
Anxiety is a common yet frequently overlooked psychiatric symptom in patients with ESRD treated with hemodialysis (HD) (1–3), yet it is also a diagnosis, applicable in diverse populations. Anxiety is characterized by disruptive feelings of uncertainty, dread, and fearfulness (4,5) (Table 1). Anxiety is defined as anticipation of a future threat (4,5). Anxiety can be an adaptive life-saving response, helping one prepare for the long winter or other distal threats. However, pathologic anxiety is excessive, or persists beyond developmentally appropriate periods.
Table 1.
Anxiety disorders with their hallmark features (Diagnostic and Statistical Manual 5)
| Type of Anxiety Disorder | Hallmark Features |
| Specific phobia | Marked fear or anxiety about a specific object or situation. |
| Social anxiety disorder (social phobia) | Marked fear or anxiety about social situations in which the individual is exposed to possible scrutiny by others. |
| Panic disorder | Recurrent unexpected panic attacks (an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time the person experiences a variety of symptoms). |
| Agoraphobia | Marked fear or anxiety about two (or more) of the following situations: using public transportation, being in open spaces, being in enclosed places, standing in line or being in a crowd, being outside of the home alone. |
| Generalized anxiety disorder | Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least 6 months, about a number of events or activities. |
Anxiety becomes a disorder when the intensity and duration extend beyond what would be expected, given a typical response to a particular event (4,5). The minimum duration for most of the anxiety disorders is >6 months, and the intensity is deemed to be disproportionate to the actual level of threat. Anxiety can be a diagnostic symptom in other psychiatric disorders, including depression, post-traumatic stress disorder (PTSD), and obsessive compulsive disorder, among others. Women experience pathologic anxiety at a rate approximately twice that of men (5).
In this review, we present three clinical vignettes, highlighting the role of anxiety in patients with ESRD treated with HD. We consider the epidemiology, clinical presentation, and treatment of anxiety in ESRD patients treated with HD, while highlighting anxiety both as a primary diagnosis and a comorbid symptom, perhaps coexisting with other medical or psychiatric disorders, as both medical and psychiatric illnesses may complicate renal disease. These vignettes are composites of patients, used for illustrative purposes and to protect patient privacy.
Clinical Vignette 1
Mrs. A is a 65-year-old woman with ESRD treated with HD on Tuesday, Thursday, and Saturday. Her kidney disease is secondary to type 2 diabetes mellitus of 18 years’ duration and longstanding hypertension. She has been treated with HD for approximately 3 years and has an arteriovenous (AV) graft. Her medications include metoprolol 25 mg twice a day, gabapentin 300 mg at bedtime, Glipizide 5 mg daily, Calcium Acetate 1 cap three times a day with meals, Sensipar 30 mg daily, Protonix 40 mg daily, Simvastatin 10 mg daily, and a renal vitamin daily. Her BP before dialysis ranged from 117/70 mmHg to 155/80 mmHg, with dry weight of 73 kg a year ago, followed by 71 kg 6 months ago, and 69 kg most recently.
Mrs. A never missed dialysis treatments and would always arrive on time, accompanied by her husband of 45 years. She engaged in handicrafts during treatments, making needlepoints, and giving them as gifts to other patients or staff to whom she had become close. She was meticulous about her medications, having developed her own system for knowing which medications she had taken already, and which ones she still needed to take. She was always considered a model patient.
Over the last 6 months she displayed decreased participation in center activities and began sleeping during most of her treatments. When questioned about her increased sleep at the center, she reported that she currently did not sleep well, and was experiencing daytime fatigue. Whereas she had always been cheery and pleasant with the staff in the past, she became less outgoing and less involved in conversations and the social life at the center.
A social worker was asked to evaluate Mrs. A. He reported that there had been no significant changes in Mrs. A’s life circumstances or health, but that she felt concerned about her prognosis and future in general, although there was only a minor increase in her recent level of depressive affect from her assessment 1 year ago.
In reviewing concerns with Mrs. A, she explained that she read on the Internet that AV grafts have a life expectancy of 2–3 years, and she was worried her graft will fail shortly, necessitating additional surgery. She hates having surgery, in particular undergoing anesthesia, and has found herself ruminating about the constant need for surgery. She has found herself preoccupied with thoughts of the surgery, often imagining the worst possible outcomes. Her labs show:
Hemoglobin 10.4 g/dl and hematocrit 31.2%
Albumin 2.0 g/dl
Calcium 8.8 mg/dl
Phosphate 3.3 mg/dl
Intact parathyroid hormone 542 pg/ml
Glucose 165 mg/dl
Hba1c 6.2%
BUN 34 mg/dl
Creatinine 7.8 mg/dl
Assessment: Mrs. A is a worrier. At times her worry can be adaptive but under some circumstances it can be quite detrimental. When her worry was directed toward preserving her health, it led her to be “meticulous” and a “model” of adherence. However, when the worry was focused on anticipated negative events, it had negative physical and psychologic consequences. The changes in her sleep pattern, withdrawal from social activities, irritability, and rumination about the presumed surgery are all signs of a generalized anxiety disorder (GAD). It is easy to imagine that if the GAD is not addressed, Mrs. A may soon find her ruminations leading to an episode of major depression or avoiding clinical responsibilities and becoming nonadherent. Because of the common prevalence of sleep disorders in ESRD patients, Mrs. A should have a polysomnography evaluation.
Anxiety Disorder: Clinical and Diagnostic Aspects
The Diagnostic and Statistical Manual 5 (5) defines GAD as characterized by “chronic persistent worry” for “at least 6 months” along with at least three of the following six symptoms: restlessness, feeling of being keyed up or ‘on edge’; fatigue; difficulty concentrating; irritability; muscle tension; and sleep disturbance. There are other psychiatric disorders that should be considered in the differential diagnosis of a GAD including agoraphobia, panic disorder, obsessive compulsive disorder, PTSD, social phobia, and specific phobias (4,5) (Table 1).
Anxiety can interfere with wellbeing and productivity, the ability to concentrate and process information, or the ability to make decisions and participate meaningfully in self-care. A variety of common medical complaints may be manifestations of an anxiety disorder, including palpitations, tremors, indigestion, numbness/tingling, nervousness, shortness of breath, diaphoresis, and fear (4,5). It is essential for the clinician to rule out specific medical conditions, including cardiovascular, pulmonary, and neurologic diseases, before ascribing these symptoms to an anxiety disorder.
Epidemiologic Considerations
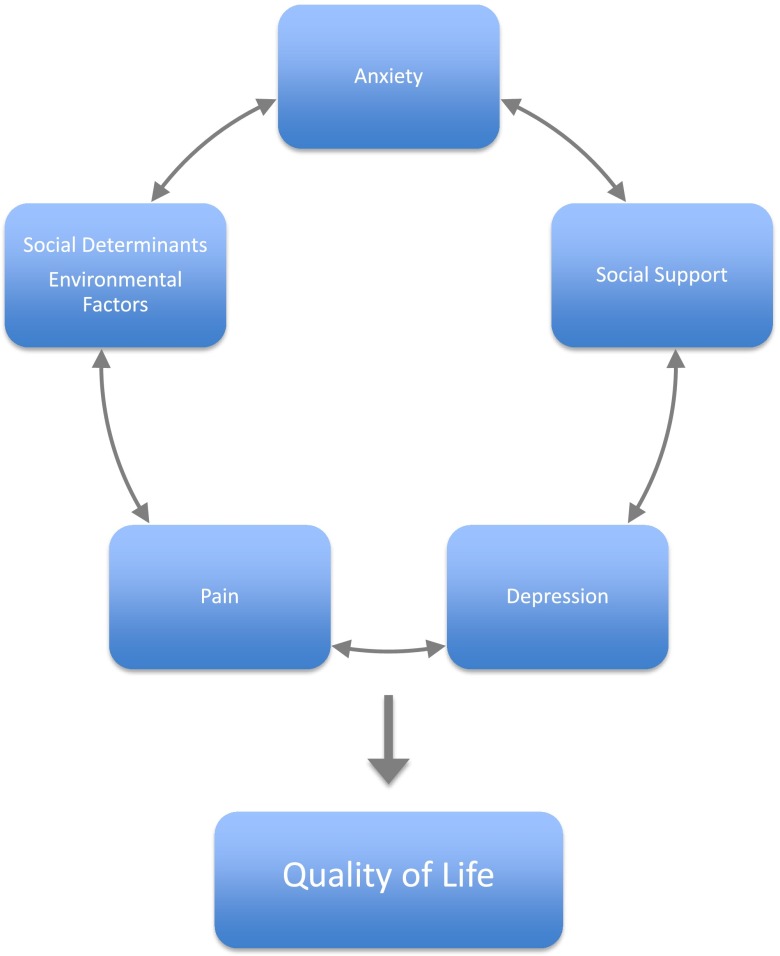
Anxiety disorders are highly prevalent in the general population, affecting approximately 40 million American adults (1,6). It is estimated that 7%–8% of patients seen in a primary care setting have a diagnosis of anxiety disorder (7). This psychiatric condition may have a significant adverse impact on patients’ perception of quality of life and is considered a significant cause of disability (Figure 1). Less is known regarding the prevalence and impact of anxiety disorders in patients with ESRD treated with HD. Much of the limited psychosocial research in this patient population has focused on depression, which is also highly prevalent in ESRD patients (8,9).
Figure 1.
Schematic depiction of the interaction of psychosocial and environmental factors and anxiety as they affect patient perception of quality of life.
Comorbidity
Another diagnostic challenge is the significant overlap in symptomatology between depression and anxiety disorders, and the fact that these two conditions often simultaneously coexist in the general population and in HD patients (2,3) (Figure 1). It is essential to distinguish anxiety from depressive disorders, so appropriate therapeutic interventions can be provided for each condition. Sleep apnea and other sleep disorders are quite common in ESRD patients (10). Therefore, as is the case with depression in ESRD patients, complete evaluation to exclude these disorders as part of the uremic milieu, and not a psychiatric disorder, is necessary. A final issue involves the potential overlap of symptoms of the anxiety disorder with complications of uremia. Fatigue may be related to diverse organ system disorders in ESRD, such as anemia or myopathies. Difficulty concentrating may reflect uremic encephalopathy, and cognitive dysfunction is increasingly recognized as a complication of ESRD (11).
Anxiety in Patients with Kidney Disease
The exact prevalence of anxiety disorders in HD patients is unclear, but estimates have ranged from approximately 12% to 52% in various studies (12). The wide disparity in range likely reflects differences in the screening methods for anxiety disorders used by the investigators and the different patient populations which were sampled. Cukor et al. (2) found that 45.7% of the 70 randomly selected HD patients in a single dialysis center in Brooklyn, NY, met criteria for an anxiety disorder. A semistructured clinical interview (SCID-IV) was used to determine diagnosis. The most common anxiety disorders in this patient population included specific phobias and panic disorders (with or without agoraphobia). Patients who met criteria for an anxiety disorder had lower perception of quality of life measured by the Kidney Disease Quality of Life–Short Form, compared with those without anxiety disorders. The authors concluded that the “intrusiveness of ESRD into multiple life domains, as well as its substantial daily demands, have a substantial impact on the psyche of patients and explain the greater than expected rates of anxiety.”
It is important to consider anxiety disorders when evaluating the psychosocial status of ESRD patients. Anxiety disorders are consistently associated with ESRD patients’ perception of quality of life, measured by a variety of scales, including the Kidney Disease Quality of Life–Short Form, the MOS SF-36, and the Health Related Quality of Life Scale (1–3,13–15) (Figure 1). Perception of quality of life has been associated with clinical outcomes of HD, including patients’ behavioral adherence, nutritional status, and mortality (16–18). Cukor et al. (3) found that compared with HD patients with depressive disorders, HD patients diagnosed with anxiety disorders have improved quality of life. However, compared with patients without psychiatric diagnoses, patients with anxiety disorders report lower quality of life.
Clinical Vignette 2
Mr. B is a 28-year-old man with ESRD secondary to hypertension, treated with HD for 2 years. He has secondary hyperparathyroidism and anemia. He was discharged from the Army 3 years ago after service in Afghanistan. There is a family history of ESRD in a grandfather, his mother, and a sibling. He has a long history of marijuana use for many years, dating back to the age of 12. He is scheduled for HD on Monday, Wednesday, and Friday at 6 am for 4 hours per treatment. His dialysis access has been revised several times due to episodes of clotting and nonfunction. He has been scheduled and rescheduled for vein mapping and AV fistula placement several times but is often a “No Call, No Show” for those appointments.
The patient says he is a “tough guy” who does what he wants, when and how he wants to do it. He does not like schedules or being told what to do. He states, “I know what I’m doing and nobody can tell me different.” He often shortens treatment and demands to be removed from the machine immediately. He becomes fidgety, agitated, and sometimes verbally aggressive if he is made to wait. His shortening behavior is of particular concern because he consistently has increased interdialytic weight gains, hyperkalemia, and hyperphosphatemia.
His dry weight is 89 kg and his average interdialytic weight gain is 4.8 kg. The social worker reports that he is usually pleasant with her, and when she asked about his demands, he explained that he is an “impatient guy” and has difficulty managing his emotions when he feels as though he is “being held hostage” by the medical team.
His current medications include Epogen 11,000 units intravenously (iv) every treatment, Venofer 100 mg iv every treatment × 10, Hectoral 6.5 μg iv every treatment, Renvela 800 mg three tablets with each meal, Labetalol 600 mg twice a day, Nifedipine 120 mg qhs, Losartan 50 mg qhs, and a dialysis vitamin daily. His predialysis BP ranges from 153/96 mmHg to 175/126 mmHg.
Laboratory evaluation includes:
Hemoglobin 10.5 g/dl
Hematocrit 31.5%
Ferritin 181 ηg/dl
Iron 36 μg/dl
White blood cell 4100 per mm3
Phosphate 7.8 mg/dl
Calcium 8.6 mg/dl
Intact parathyroid hormone 758 pg/ml
Albumin 3.5 g/dl
Assessment: Mr. B should be fully evaluated for the presence of panic disorder. People with panic disorder have a difficult time tolerating somatic symptoms that are reminiscent of a panic attack. The last portion of each HD treatment can induce muscle cramping and soreness. The feelings of mounting restlessness from the hours already spent tethered to the dialysis machine, in combination with the anticipation of these physiologic symptoms, can create a vicious cycle of anticipatory anxiety and increased physiologic arousal leading to a panic attack. A hallmark of panic disorder is the attempt to avoid symptoms or situations that are perceived as triggers of panic attacks. Furthermore, it is possible that Mr. B’s long-term use of marijuana may be viewed as an attempt to self-medicate, by reducing his heightened state of anxiety, and a demonstration of his inability to tolerate his own physiologic arousal. If, indeed, Mr. B is acting the way he is in order to avoid his own anxiety reactions, his management within the unit will be quite different than if he is simply conceptualized as a “difficult patient.”
Clinical Presentation in Dialysis Units
Anxiety disorders can manifest at various times and with a variety of presentations during HD. This patient with seemingly early irrational sign-offs may be manifesting a form of panic disorder, PTSD, and/or GAD. Clinical evaluation for anxiety disorders should take place at the time of dialysis initiation; as part of an annual mental health evaluation; when coexistent depression is suspected; during the occurrence of major life stressors; when a marked change in patients’ health status is noted, including when evidence of dietary or medication nonadherence, such as hyperphosphatemia is discerned; or during disruptive patient behavior in the dialysis unit. If anxiety disorder is diagnosed, then simultaneous evaluation for depression and risk of suicide is always indicated (4). Furthermore, anxiety disorders place patients at higher risk for concomitant substance abuse (4). An estimated 35% of patients with anxiety disorder in the general population abuse alcohol and other drugs (4,19).
Treatment
There have been limited studies that have evaluated the treatment of anxiety disorders in ESRD patients. Therapeutic options include lifestyle modifications and psychotherapeutic interventions such as cognitive-behavioral psychotherapies and pharmacologic agents, including selective serotonin reuptake inhibitors and benzodiazepines (4,20–22). Lifestyle modifications should be discussed with patients with anxiety disorders. These include regular exercise regimens, attention to proper sleep hygiene, and avoidance of caffeine, smoking, and overuse of alcohol (4). Such simple strategies may help to mitigate the symptoms of anxiety disorder without the need for more intensive intervention.
Psychotherapies that have been shown to effectively treat anxiety disorders in the general medical population include relaxation-based therapies, mindfulness-based therapy, psychodynamic therapy, and cognitive behavioral therapy (CBT) (4,20–22). CBT has the most evidence supporting its role in the treatment of anxiety disorder in general medical patients (4,22–24). CBT consists of weekly individual or group-based therapy sessions that incorporate relaxation strategies along with “cognitive restructuring” to focus the patient on the idea that his or her worries are “counterproductive” (4,22,24,25). CBT also uses the power of “exposure therapy” to assure the patient that his or her concerns are unjustified (4,22). The positive impact of CBT on depressive affect in HD patients has been previously evaluated (26,27). CBT is currently undergoing additional study in a randomized controlled trial comparing its effect with that of sertraline in HD patients with increased depressive affect (23). The impact of psychotherapeutic interventions on anxiety disorder needs additional study in ESRD patients.
Benzodiazepines have been used in the general population to reduce transient anxiety symptoms, particularly in patients with associated social phobias (4). Concern exists regarding the potential of such drugs for abuse (28,29). Benzodiazepines should not be used for chronic treatment or in patients with addiction disorders (29). β-blockers have also been tried to decrease autonomic nervous system hyperarousal symptoms and performance tremors in patients with anxiety disorders. Selective serotonin reuptake inhibitors and serotonin–norepinephrine reuptake inhibitors have been successfully used to treat anxiety disorders in the general population, and are often considered the first-line pharmacologic treatment (20). Other medication options for patients with anxiety disorders include buspirone, pregabalin, gabapentin, and quetiapine (4). Less is known regarding the effects of these therapeutic approaches in ESRD patients. All medications must be dosed for patients in accordance with their eGFR (30,31). The dialyzability of medications should also be considered, along with the timing of patients’ dialysis schedules, when initiating drug therapy for anxiety disorders in ESRD patients treated with HD (32).
Clinical Vignette 3
Mrs. C is a 75-year-old woman with ESRD treated for 1 year with 4 hours of HD on Tuesday, Thursday, and Saturday afternoons. Her other comorbidities include obesity, hypertension, and coronary artery disease. She became a widow approximately 5 years ago. She lives alone. Her daughter lives in the area and visits occasionally.
Two months ago, Mrs. C watched as her long-time treatment neighbor lost consciousness while being dialyzed. Although the man was quickly resuscitated, and there were no obvious long-term serious adverse effects for the patient, Mrs. C was greatly affected by watching the entire incident. Since that time her attendance at the dialysis center has been sporadic. She currently is often late and twice did not show at all. When asked about her behavior change she stated that she has been very stressed, hasn’t been sleeping well, and has been waking up late. After further discussion, she acknowledged that she has been feeling “like a total wreck” and can’t get the image of the man slumped in his chair out of her mind. The social worker learned that since this incident 2 months ago, she has been thinking much more about her husband’s death. He had died of an apparent heart attack overnight in their bed, and she discovered him dead in the morning. She began to cry as she related to the social worker that as a young girl in the Dominican Republic, her aunt, who had been living with her family, was hit by a car and killed in front of them. Mrs. C seemed to be having difficulty coping with her husband’s death and could not stop picturing an image of herself slumped over at dialysis or dead in her bed.
Assessment: Recent traumatic or difficult events often trigger memories of previous traumatic events, especially if they have not been fully psychologically processed. It is difficult to anticipate which events may tip the balance toward unsuccessful coping, particularly because of the synergistic effects of multiple traumas. Mrs. C’s reaction to the events in the dialysis center is clearly not commensurate with the degree of traumatic exposure, however, in combination with her husband’s and aunt’s deaths, she may have developed PTSD. After witnessing the friend’s loss of consciousness, which is a potentially life-threatening experience, Mrs. C exhibited intrusive distressing memories of the event, avoidance behaviors (not easily returning to the dialysis center), change in affect, and increased hypervigilance (insomnia).
Although the most recent Diagnostic and Statistical Manual 5 lists PTSD in a category called “Trauma and Stressor Related Disorders” and not in “Anxiety Disorders,” it does this to acknowledge that some presentations of PTSD involve depressive affect alone. In this case, however, anxiety is the hallmark symptom of the presentation. Mrs. C was referred to a mental health professional with expertise in trauma.
Anxiety disorders can coexist or be present with another psychiatric disorder, such as depression. The combination of anxiety with medical illness, with coexisting psychiatric disorders and with the social challenges of quotidian life, can result in a complex interaction which may threaten medical outcomes, perception of quality of life, and behavioral adherence (Figure 1), as well as potentially complicating therapy. The interrelationship of a multidisciplinary team of health care workers, including nephrologists, primary care physicians, mental health professionals, as well as the dialysis unit staff, is essential in helping patients with anxiety adjust to the challenging demands of the dialysis schedule and to the dialysis unit as a social milieu (9). Long-term outcomes of patients with ESRD and anxiety with comorbid psychiatric disorders remain to be determined in well designed studies.
Conclusions
Anxiety disorders are an under-recognized yet important clinical problem in ESRD patients. Anxiety disorders have been linked with depression, lower perceived quality of life, and perhaps most importantly, to poorer behavioral adherence. Many of the seemingly irrational behaviors of patients, or behaviors which place them in conflict with staff and physicians, may be the expression of an underlying anxiety disorder. Examples of such behaviors include aggressive demands to sign off therapy instantly, or to be treated by a particular technician or using a certain machine. Given their high prevalence, it is essential to evaluate ESRD HD patients for the presence of anxiety disorders as part of the overall psychosocial assessment. Assessment needs to go beyond simply asking patients about their moods or anxiety states, as for many people their anxious state is their “normal” state, and they may not readily identify it as pathologic.
Strategies for screening populations of ESRD patients for anxiety disorders have not yet been developed, but are needed. There is also a lack of evidence regarding the appropriate therapeutic approach to anxiety disorders in patients with ESRD. If an anxiety disorder is suspected, referral to mental health professionals and treatment with psychotherapy or pharmacotherapy is recommended. If pharmacotherapy is used, it is important to consider appropriate dose reduction for diminution in renal function and the timing of patients’ dialysis to avoid medication-dosing errors. Randomized controlled trials to evaluate the impact and consequences of screening and treating anxiety disorders in the ESRD patient population are urgently needed.
Disclosures
None.
Acknowledgments
A version of this paper was presented by Dr. R. Mehotra of the University of Washington at the Clinical Meeting of the National Kidney Foundation in March 25–29, 2015 as an educational exercise.
The opinions expressed in this paper do not necessarily reflect those of the National Institute of Diabetes Digestive and Kidney Diseases, the National Institutes of Health, the Department of Health and Human Services, or the Government of the United States of America.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Cukor D, Ver Halen N, Fruchter Y: Anxiety and quality of life in ESRD. Semin Dial 26: 265–268, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Cukor D, Coplan J, Brown C, Friedman S, Newville H, Safier M, Spielman LA, Peterson RA, Kimmel PL: Anxiety disorders in adults treated by hemodialysis: a single-center study. Am J Kidney Dis 52: 128–136, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Cukor D, Coplan J, Brown C, Peterson RA, Kimmel PL: Course of depression and anxiety diagnosis in patients treated with hemodialysis: a 16-month follow-up. Clin J Am Soc Nephrol 3: 1752–1758, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein MB, Sareen J: Generalized Anxiety Disorder. N Engl J Med 373: 2059–2068, 2015 [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association: Diagnostic and statistical manual of mental disorders, 5th Ed., Arlington, VA, American Psychiatric Association, 2013 [Google Scholar]
- 6.World Health Organization (WHO): New Understanding, New Hope: Burden of Mental and Behavioural Disorders. In: The World Health Report-Mental Health, Geneva, WHO Press, 2010, pp 1–65 [Google Scholar]
- 7.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B: Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 146: 317–325, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Cukor D, Peterson RA, Cohen SD, Kimmel PL: Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol 2: 678–687, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Cukor D, Cohen SD, Peterson RA, Kimmel PL: Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol 18: 3042–3055, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Merlino G, Piani A, Dolso P, Adorati M, Cancelli I, Valente M, Gigli GL: Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant 21: 184–190, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Kurella M, Chertow GM, Fried LF, Cummings SR, Harris T, Simonsick E, Satterfield S, Ayonayon H, Yaffe K: Chronic kidney disease and cognitive impairment in the elderly: the health, aging, and body composition study. J Am Soc Nephrol 16: 2127–2133, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Murtagh FE, Addington-Hall J, Higginson IJ: The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis 14: 82–99, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Martin C, Thompson D: Prediction of quality of life in patients with end stage renal disease. Brit J Health Psych 5: 41–55, 2000
- 14.Birmelé B, Le Gall A, Sautenet B, Aguerre C, Camus V: Clinical, sociodemographic, and psychological correlates of health-related quality of life in chronic hemodialysis patients. Psychosomatics 53: 30–37, 2012 [DOI] [PubMed] [Google Scholar]
- 15.Kallay E, Pop R, Balazsi R: Emotional profile and quality of life in chronic renal failure and renal transplant patients. Cogn Brain Behav 13: 313–328, 2009 [Google Scholar]
- 16.Kimmel PL, Patel SS: Quality of life in patients with chronic kidney disease: focus on end-stage renal disease treated with hemodialysis. Semin Nephrol 26: 68–79, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Mapes DL, Bragg-Gresham JL, Bommer J, Fukuhara S, McKevitt P, Wikström B, Lopes AA: Health-related quality of life in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis 44[Suppl 2]: 54–60, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F, Fukuhara S, Young EW, Kurokawa K, Saito A, Bommer J, Wolfe RA, Held PJ, Port FK: Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 64: 339–349, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Robinson J, Sareen J, Cox BJ, Bolton JM: Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch Gen Psychiatry 68: 800–807, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Reinhold JA, Rickels K: Pharmacological treatment for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother 16: 1669–1681, 2015 [DOI] [PubMed] [Google Scholar]
- 21.Bereza BG, Machado M, Ravindran AV, Einarson TR: Evidence-based review of clinical outcomes of guideline-recommended pharmacotherapies for generalized anxiety disorder. Can J Psychiatry 57: 470–478, 2012 [DOI] [PubMed] [Google Scholar]
- 22.Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G: Psychological treatment of generalized anxiety disorder: a meta-analysis. Clin Psychol Rev 34: 130–140, 2014 [DOI] [PubMed] [Google Scholar]
- 23.Hedayati SS, Daniel DM, Cohen S, Comstock B, Cukor D, Diaz-Linhart Y, Dember LM, Dubovsky A, Greene T, Grote N, Heagerty P, Katon W, Kimmel PL, Kutner N, Linke L, Quinn D, Rue T, Trivedi MH, Unruh M, Weisbord S, Young BA, Mehrotra R: Rationale and design of A Trial of Sertraline vs. Cognitive Behavioral Therapy for End-stage Renal Disease Patients with Depression (ASCEND). Contemp Clin Trials 47: 1–11, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chambless DL, Gillis MM: Cognitive therapy of anxiety disorders. J Consult Clin Psychol 61: 248–260, 1993 [DOI] [PubMed] [Google Scholar]
- 25.Erickson TM, Newman MG: Cognitive behavioral psychotherapy for generalized anxiety disorder: a primer. Expert Rev Neurother 5: 247–257, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Cukor D, Ver Halen N, Asher DR, Coplan JD, Weedon J, Wyka KE, Saggi SJ, Kimmel PL: Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol 25: 196–206, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duarte PS, Miyazaki MC, Blay SL, Sesso R: Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int 76: 414–421, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Olfson M, King M, Schoenbaum M: Benzodiazepine use in the United States. JAMA Psychiatry 72: 136–142, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Moore N, Pariente A, Bégaud B: Why are benzodiazepines not yet controlled substances? JAMA Psychiatry 72: 110–111, 2015 [DOI] [PubMed] [Google Scholar]
- 30.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration): A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fanton JH, Germain MJ, Cohen LM: Treatment of Psychiatric Disorders in Chronic Kidney Disease Patients. In: Chronic Renal Disease, edited by Kimmel PL, Rosenberg ME, San Diego, CA, Academic Press, 2015, pp 725–737 [Google Scholar]
- 32.Velenosi TJ, Urquhart BL: Pharmacokinetic considerations in chronic kidney disease and patients requiring dialysis. Expert Opin Drug Metab Toxicol 10: 1131–1143, 2014 [DOI] [PubMed] [Google Scholar]
- 33.Rickels K, Downing R, Schweizer E, Hassman H: Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 50: 884–895, 1993 [DOI] [PubMed] [Google Scholar]