Abstract
Background
Technique failure is an important issue for peritoneal dialysis (PD) patients. In this study, we aimed to analyze technique failure rate in detail and to determine the predictors for technique failure in Korea.
Methods
We identified all patients who had started dialysis between January 1, 2005, and December 31, 2008, in Korea, using the Korean Health Insurance Review and Assessment Service database. A total of 7,614 PD patients were included, and the median follow-up was 24.9 months.
Results
The crude incidence rates of technique failure in PD patients were 54.1 per 1,000 patient-years. The cumulative 1-, 2-, and 3-year technique failure rates of PD patients were 4.9%, 10.3%, and 15.6%, respectively. However, those technique failure rates by Kaplan–Meier analysis were overestimated compared with the values by competing risks analysis, and the differences increased with the follow-up period. In multivariate analyses, diabetes mellitus and Medical Aid as a crude reflection of low socioeconomic status were independent risk factors in both the Cox proportional hazard model and Fine and Gray subdistribution model. In addition, cancer was independently associated with a lower risk of technique failure in the Fine and Gray model.
Conclusion
Technique failure was a major concern in patients initiating PD in Korea, especially in diabetic patients and Medical Aid beneficiaries. The results of our study offer a basis for risk stratification for technique failure.
Keywords: Peritoneal dialysis, Risk factors, Technique failure
Introduction
There has been a significant increase in the number of incident dialysis patients over the past decade in Korea. According to the 2012 annual report from the Korean nationwide registry program, the number of new end-stage renal disease (ESRD) patients with hemodialysis (HD), peritoneal dialysis (PD), or kidney transplantation (KT) was 8,811 (169.8 per million population [PMP]), 923 (17.8 PMP), or 1,738 (33.5 PMP), respectively [1].
Notably, the number of new patients on PD has been decreasing since 2007, whereas the number of those on HD and KT has been increasing continuously, consistent with the trend observed in the United States [2]. Possible reasons for the decreasing rate of choosing PD as an initial dialysis therapy could include increased number of HD centers, better outcome in HD patients [3], and concerns about PD-related complications including peritonitis. Moreover, high technique failure rate in PD patients has contributed to the decreasing number of prevalent PD [1].
ESRD patients on dialysis suffer not only from higher mortality compared with the general population [4] but also from high morbidity due to various cardiovascular diseases, cancer, and technique failure. Technique failure can induce medical stress including subsequent mortality and additional cost, especially in the earlier period after initiation of PD [5], [6], [7]. Accordingly, there has been a continuous effort to analyze the causes and predictors of technique failure. Nevertheless, there are still controversial issues for technique failure risk factors because of different medical and social environments across countries. Although a population-based study for technique failure was reported in Western countries, there has not been a similar study in Asian countries. Because there are significant differences between Western and Asian ESRD patients in etiology of renal failure and mortality rates [8], it is likely that there are different characteristics for technique failure in Asian patients.
In addition, it is known that there are various competing risks in the research for outcomes in PD, and the risk of the outcome of interest may be overestimated without consideration of these competing risks [9], [10].
In this study, we aimed to analyze technique failure rate in PD in detail and to determine the specific predictors for technical failure by both conventional analysis and competing risks analysis, using the Korean Health Insurance Review and Assessment Service (HIRA) database, which is a nationwide, population-based data set.
Methods
Data source and study population
We performed a retrospective cohort study that used information from the Korean HIRA database. In Korea, all medical care expenses for dialysis are reimbursed by HIRA. Therefore, we were able to collect all information from every ESRD patient and analyze data which represented the entire Korean population. We initially identified all the incident dialysis patients who had started PD therapy from January 1, 2005, to December 31, 2008, using detailed methods described elsewhere [3]. Among them, the patients who were younger than 18 years or the patients who survived for less than 90 days from the date of dialysis initiation were excluded. All included patients were followed up until December 31, 2009. The time to death was confirmed by the Certificate Database, which records the reasons for changes in eligibility for the health security system including death or emigration, as well as by the National Health Insurance Claims Database. Comorbidities of the participants were identified by reviewing their medical history during the last 1 year before the initiation of dialysis therapy. The list of analyzed comorbidities was determined on the basis of suggestions by Charlson et al [11], and International Classification of Diseases, 10th Revision, codes were used according to the proposed algorithms by Quan et al [12].
Definition
Technique failure was defined as transference from a specific modality of dialysis therapy to another modality that lasted for 30 days or more, and the end point of this study was time to technique failure. We considered the dialysis modality at day 90 as the initial dialysis modality and incorporated all events of shifting modality afterward. Most of the acutely ill patients who need urgent initiation of dialysis start dialysis preferentially with HD. Because we could not investigate the cause of dialysis initiation, education on dialysis modalities a priori, and referral timing, we evaluated the technique failure rate in “long-term dialysis” patients maintained on dialysis for 3 months or more. In addition, although some patients switched dialysis modalities multiple times, we only included the first event of technique failure for the entire analysis.
Statistical analysis
All data are expressed as mean ± standard deviation or number (percent) unless otherwise specified. A P value < 0.05 was considered statistically significant.
To assess technique failure–free survival, we used Kaplan–Meier survival curves with the log-rank test to compare the differences. Patients were censored at KT, death, or on December 31, 2009. Cox proportional hazards analysis was performed to determine predictive factors, and significant variables in univariate analyses were included in multivariate analysis with a threshold of 0.10 for retention. In addition, to compare the technique failure–free survival rates according to the dialysis initiation year, we constructed data sets in which the patients were followed up to 2 years to let each year cohort have the same follow-up period.
Next, we performed competing risks analysis because the Kaplan–Meier method is known to overestimate the probabilities of each event when there are competing events in PD patients [10], [13]. In our analysis, death and KT are considered to be competing events for technique failure. To explore the relationship between covariates and the cumulative incidences of each event, the Fine and Gray regression model was used. In addition, we compared results by competing risks analysis with those obtained by Kaplan–Meier analysis.
The statistical analyses were performed using the statistic software SPSS, version 18.0 (SPSS Inc., Chicago, IL, USA), and R 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria) including cmprsk package.
This investigation was conducted according to the principles expressed in the Declaration of Helsinki. The Institutional Review Board at the HIRA approved the survey of the study population.
Results
Baseline characteristics of the participants
A total of 7,614 eligible patients who started PD between January 1, 2005, and December 31, 2008, were analyzed. At the initiation of dialysis treatment, the mean patient age was 54.5 ± 13.8 years; 56.3% of the patients were male, and 50.4% of the patients had diabetes. A detailed description of characteristics among PD patients is shown in Table 1.
Table 1.
Baseline characteristics (N = 7,614)
| Variables | |
|---|---|
| Age (y) | 54.5 ± 13.8 |
| Males | 4,290 (56.3) |
| Health security system | |
| National Health Insurance | 6,650 (87.3) |
| Medical Aid | 964 (12.7) |
| Diabetes mellitus | 3,836 (50.4) |
| Myocardial infarction | 354 (4.6) |
| Congestive heart failure | 1,224 (16.1) |
| Peripheral vascular disease | 416 (5.5) |
| Cerebrovascular disease | 806 (10.6) |
| Dementia | 69 (0.9) |
| Chronic pulmonary disease | 1,177 (15.5) |
| Connective tissue disease | 208 (2.7) |
| Peptic ulcer disease | 1,035 (13.6) |
| Hemiparesis | 92 (1.2) |
| Liver disease | 753 (9.9) |
| Cancer | 313 (4.1) |
Age is presented as the mean ± SD, and all other data are presented as the n (%).
Crude incidence rates of technique failure
During the median follow-up of 24.9 months (range, 3.0–60.0 months), 942 (12.4%) PD patients had experienced technique failure, and the crude incidence rates of technique failure among PD patients were 54.1 per 1,000 patient-years. More detailed descriptions for crude incidence rates of PD technique failure are shown in Table 2.
Table 2.
Crude incidence rates of technique failure
| Subgroup | Cases (N)/patient-years | Incidence rate (1,000/patient-years) | |
|---|---|---|---|
| Sex | Male | 539/9,683.7 | 55.7 |
| Female | 403/7,743.6 | 52.0 | |
| Diabetes mellitus | Yes | 543/8,318.6 | 65.3 |
| No | 399/9,108.8 | 43.8 | |
| Age (y) | < 64 | 718/13,545.0 | 53.0 |
| 65+ | 224/3,882.3 | 57.7 | |
| Health security system | NHI | 793/15,275.1 | 51.9 |
| MA | 149/2,152.2 | 69.2 | |
| All patients | Overall | 942/17,427.0 | 54.1 |
MA, Medical Aid; NHI, National Health Insurance.
Median time of technique failure after initiation of dialysis therapy among PD patients was 25.0 months (interquartile range, 15.3–39.0 months).
Cumulative incidences by Kaplan–Meier analysis and competing risks analysis
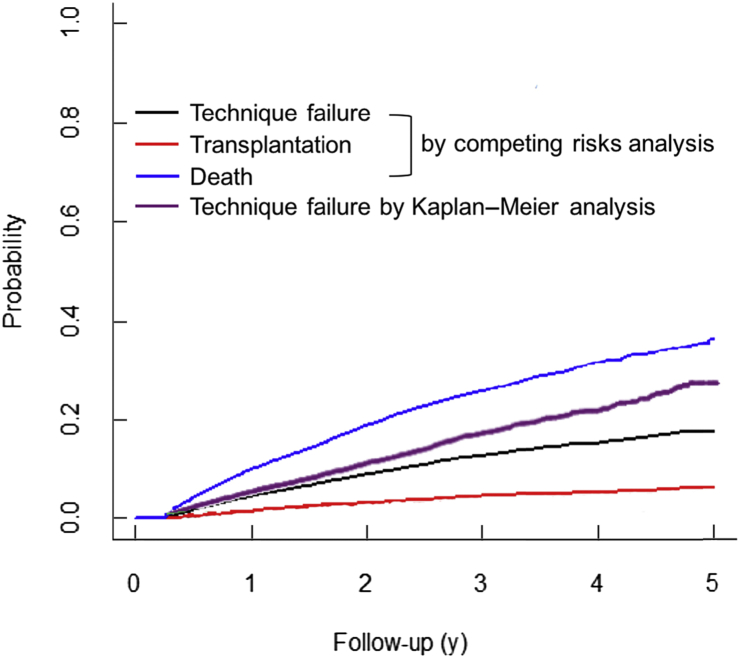
Table 3 shows the cumulative incidences calculated by Kaplan–Meier analysis and by competing risks analysis. We censored death and technique failure in Kaplan–Meier analysis, while all those were counted as events of interest in competing risks analysis. In Kaplan–Meier analysis, the 1-, 2-, and 3-year cumulative incidences of technique failure among PD patients were 4.9%, 10.3%, and 15.6%, respectively. However, cumulative incidences of technique failure calculated by competing risks analysis were lower than those determined by Kaplan–Meier analysis among PD patients (Table 3). Of note, the complement of Kaplan–Meier estimate (1 – KM) was higher than the estimate of cumulative incidence by competing risks analysis (Fig. 1).
Table 3.
Cumulative incidences of events of interest calculated by Kaplan–Meier analysis and by competing risks analysis
| Years after initiation of dialysis | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Kaplan–Meier analysis∗ | ||||
| Technique failure | 0.049 | 0.103 | 0.156 | 0.195 |
| Competing risks analysis | ||||
| Technique failure | 0.046 | 0.091 | 0.128 | 0.152 |
| Transplantation | 0.015 | 0.032 | 0.046 | 0.054 |
| Death | 0.100 | 0.190 | 0.258 | 0.316 |
In Kaplan–Meier analysis, transplantation and death were censored.
Figure 1.
Comparison of cumulative incidences of technique failure between curves calculated by Kaplan–Meier analysis and by competing risks analysis.
In addition, competing risks analysis allowed calculation of the cumulative incidence of the other outcomes, including death and transplantation. Cumulative incidences of death were higher than those of technique failure or transplantation. When calculating the 1-, 2-, and 3-year survival rates from cumulative incidences of death, the survival rates of PD patients were 90%, 81%, and 74%, respectively.
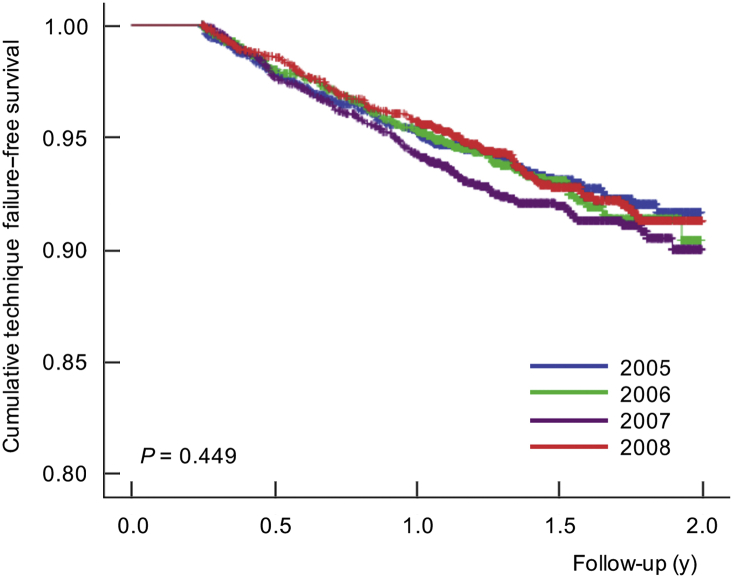
When we compare the technique failure–free survival rates according to the year of dialysis initiation, it was not significantly different up to 2 years among PD patients by the log-rank test (Fig. 2; P = 0.449).
Figure 2.
Technique failure–free survival curves according to the year of dialysis initiation. There was no significant difference in technique failure–free survival rates up to 2 years according to the year of dialysis initiation (log-rank test, P = 0.449).
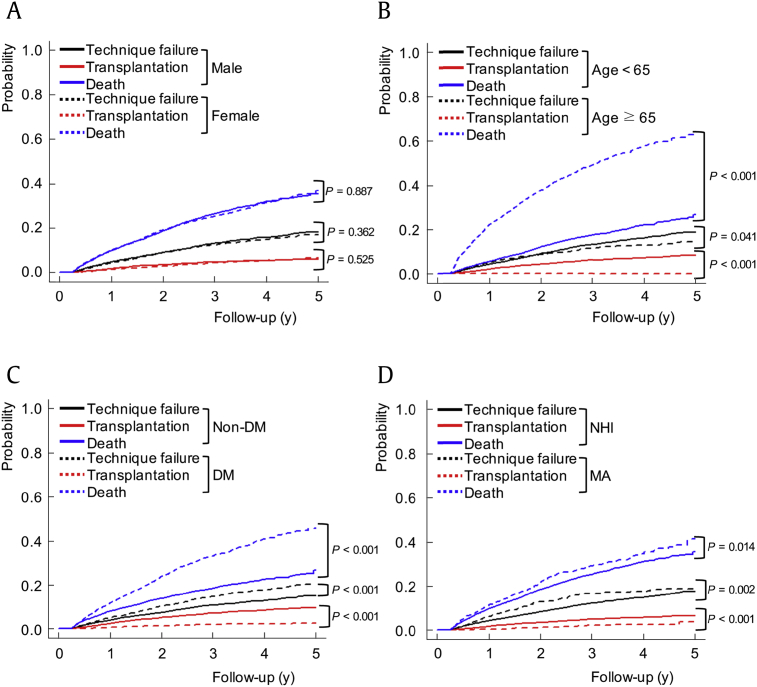
Comparison of cumulative incidences according to baseline characteristics among incident PD patients
We compared cumulative incidences calculated by competing risks analysis according to sex, age group, diabetes, or health security system among PD patients (Fig. 3). There was no significant difference in the cumulative incidences of technique failure between male and female patients (P = 0.362). However, cumulative incidence of technique failure was significantly higher in younger patients than in elderly patients (< 65 vs. ≥ 65 years, P = 0.041) and in diabetic patients than in nondiabetics (P < 0.001). In addition, Medical Aid beneficiaries had higher cumulative incidence of technique failure than patients covered by National Health Insurance (P = 0.002).
Figure 3.
Comparison of cumulative incidences of technique failure, transplantation, and death according to sex, age groups, DM, or health security system among PD patients.
DM, diabetes mellitus; MA, Medical Aid; NHI, National Health Insurance; PD, peritoneal dialysis.
(A) There was no significant difference in the cumulative incidences of technique failure between male and female patients (P = 0.362). (B-D) Cumulative incidence of technique failure was significantly higher in younger patients than in elderly patients (< 65 years vs. ≥ 65 years, P = 0.041), and in diabetic patients than in non-diabetics (P < 0.001). In addition, MA beneficiaries had higher cumulative incidence of technique failure compared to patients covered by NHI (P = 0.002).
Comparison of regression models among PD patients: Cox proportional hazard model versus Fine and Gray subdistribution hazard model
Table 4 shows a summary of the unadjusted and adjusted effects of covariates for technique failure based on the 2 types of analyses: Cox proportional hazard model and Fine and Gray subdistribution hazard model.
Table 4.
Comparison between results by the Cox model and those by the Fine and Gray model for technique failure
| Variables | Cox proportional hazard model (cause-specific hazard model) |
Fine and Gray model (hazard of the subdistribution model) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate |
Multivariate∗ |
Univariate |
Multivariate∗ |
|||||||||
| HR | 95% CI | P | HR | 95% CI | P | sHR | 95% CI | P | sHR | 95% CI | P | |
| Age (per 1-y increase) | 1.01 | 1.00–1.01 | 0.004 | 1.00 | 1.00–1.01 | 0.137 | 1.00 | 1.00–1.00 | 0.780 | – | – | – |
| Female (vs. male) | 0.94 | 0.82–1.06 | 0.304 | – | – | – | 0.95 | 0.83–1.08 | 0.400 | – | – | – |
| MA (vs. NHI) | 1.34 | 1.12–1.59 | 0.001 | 1.28 | 1.07–1.52 | 0.007 | 1.31 | 1.10–1.57 | 0.002 | 1.27 | 1.07–1.52 | 0.008 |
| Diabetes mellitus | 1.50 | 1.32–1.71 | < 0.001 | 1.42 | 1.24–1.62 | < 0.001 | 1.38 | 1.22–1.57 | < 0.001 | 1.35 | 1.19–1.54 | < 0.001 |
| Myocardial infarction | 0.96 | 0.69–1.35 | 0.827 | – | – | – | 0.78 | 0.55–1.09 | 0.140 | – | – | – |
| Congestive heart failure | 1.14 | 0.96–1.35 | 0.138 | – | – | – | 1.01 | 0.85–1.20 | 0.920 | – | – | – |
| Peripheral vascular disease | 1.32 | 1.01–1.72 | 0.043 | 1.17 | 0.90–1.54 | 0.241 | 1.18 | 0.91–1.55 | 0.210 | – | – | – |
| Cerebrovascular disease | 1.21 | 0.98–1.49 | 0.072 | 1.07 | 0.86–1.33 | 0.537 | 0.99 | 0.80–1.22 | 0.900 | – | – | – |
| Dementia | 0.96 | 0.43–2.14 | 0.916 | – | – | – | 0.69 | 0.31–1.56 | 0.370 | – | – | – |
| Chronic pulmonary disease | 1.23 | 1.04–1.46 | 0.017 | 1.17 | 0.99–1.40 | 0.061 | 1.14 | 0.96–1.35 | 0.140 | – | – | – |
| Connective tissue disease | 1.35 | 0.94–1.93 | 0.104 | – | – | – | 1.25 | 0.87–1.79 | 0.220 | – | – | – |
| Peptic ulcer disease | 1.01 | 0.84–1.22 | 0.926 | – | – | – | 0.96 | 0.80–1.16 | 0.680 | – | – | – |
| Hemiparesis | 1.57 | 0.94–2.61 | 0.085 | 1.43 | 0.85–2.43 | 0.182 | 1.30 | 0.78–2.16 | 0.310 | – | – | – |
| Liver disease | 0.87 | 0.70–1.10 | 0.241 | – | – | – | 0.87 | 0.69–1.09 | 0.210 | – | – | – |
| Cancer | 0.69 | 0.45–1.04 | 0.074 | 0.72 | 0.47–1.08 | 0.113 | 0.58 | 0.38–0.88 | 0.010 | 0.62 | 0.41–0.93 | 0.022 |
CI, confidence interval; HR, hazard ratio; MA, Medical Aid; NHI, National Health Insurance; sHR, subdistribution hazard ratio.
Hazard ratios of technique failure were adjusted for all parameters with a P < 0.10 in the univariate analysis.
In the unadjusted models for technique failure, we found that age, Medical Aid (vs. National Health Insurance), diabetes mellitus, peripheral vascular disease, and chronic pulmonary disease were significant factors in the Cox proportional hazard model, whereas Medical Aid, diabetes mellitus, and cancer were significant in the Fine and Gray subdistribution hazard model. After adjusting for factors with a P < 0.10 in the univariate analyses, Medical Aid (hazard ratio [HR], 1.28; 95% confidence interval [CI], 1.07–1.52; P = 0.007) and diabetes mellitus (HR, 1.42; 95% CI, 1.24–1.62; P < 0.001) remained statistically significant in Cox analysis. In comparison, Medical Aid (subdistribution HR, 1.27; 95% CI, 1.07–1.52; P = 0.008), diabetes mellitus (subdistribution HR, 1.35; 95% CI, 1.19–1.54; P < 0.001), and cancer (subdistribution HR, 0.62; 95% CI, 0.41–0.93, P = 0.022) were the independent predictors for technique failure in Fine and Gray analysis.
Discussion
In this study, we performed a national population-based study to evaluate technique failure in Korean patients initiating dialysis, using conventional survival analyses and competing risks analysis. The crude incidence rate of technique failure among PD patients was 54.1 per 1,000 patient-years. Because the incidence rate represented as cases per 1,000 patient-years is considered numerically equivalent to future 10-year incidence of events, thus it is recently regarded as essential for risk stratification and guiding therapy [14].
The annual technique failure rate among PD patients varies according to the region and the period when the study was conducted. The 2-year technique failure rate was 36% in an earlier Dutch study and in the recent US study [15], [16], which is higher than our rate of 10.3%. However, our 3-year technique failure rate is 15.6% and is similar to other studies that reported a rate of 16% in the early 1980s and a rate of 16.3% in a Korean single-center study [17], [18]. Those studies were mainly conducted in centers with particular experiences for treating PD patients, and a center's experience is associated with technique failure and mortality in PD [19]. Therefore, our results that included all Korean PD centers, regardless of centers' experiences, may not be inferior. In fact, a population-based Canadian study, which has a similar design to our study, reported a higher incidence of technique failure [20]. However, despite the decreasing rate of peritonitis in Korea [21], there has been no change in technique failure incidence over several decades. In addition, when we compared the crude technique failure–free survival rates among PD patients according to the dialysis initiation year between 2005 and 2008, there were no significant changes across the years. Although the period was not enough to investigate sequential changes, the survival rate among Korean PD patients initiating dialysis significantly improved from 2005 to 2008, as previously reported [22]. Therefore, technique failure in PD persists as a major problem in Korea.
In survival analysis of dialysis patients, there are several competing risks, such as death, transplantation, and technique failure [10]. The Kaplan–Meier method is likely to overestimate the incidence of technique failure. In this study, the 3-year cumulative incidence of technique failure in PD was 2.8% higher in Kaplan–Meier analysis compared to competing risks analysis. When comparing cumulative incidence function in competing risks analysis, we found that younger patients aged below 65 years, diabetics, and Medical Aid beneficiaries showed higher incidences of technique failure in PD patients.
Next, we also identified prognostic predictors for future technique failure events in PD, using both the Cox proportional hazard model and Fine and Gray subdistribution model. Of interest, independent predictors were not the same between the 2 modeling methods. In Cox analysis, Medical Aid and diabetes mellitus were significant factors, whereas Medical Aid, diabetes mellitus, and cancer were significant in the Fine and Gray model. Similarly to the previous report [23], the results in this study were also different between the Cox model and Fine and Gray model, thus we suggest that a competing risks analysis should be considered for the research on technique failure among PD patients. In another previous report, female gender, lower serum albumin, and higher body mass index were found to be independent risk factors [24]. However, because our database did not include laboratory data, we could not elucidate more valuable prognostic factors.
There were conflicting results in regards to age. In this study, age was not a significant predictor for technique failure, whereas several studies have suggested that old age was associated with an increased risk of technique failure in PD [15], [20]. In a comparison of cumulative incidence by 2 age groups, however, the technique failure rate was significantly higher in younger patients than in elderly patients. Fear to change and low life expectancy in elderly patients are the possible reasons for a lower technique conversion rate. In addition, more active decision-making in younger patients and the easy accessibility of HD in Korea could contribute to a higher modality conversion rate. However, we need further investigation to evaluate the exact reason.
We also found that diabetes mellitus was an independent factor for predicting technique failure, which is consistent with several previous studies [25], [26], [27]. Recently, however, Cotovio et al [28] reported that diabetes was a significant predictor for death in PD patients but was not a predictor for technique failure. Moreover, another retrospective cohort study indicated that baseline HbA1c levels greater than 6.5% did not show a statistically significant correlation with technique failure in PD [29].
In addition, Medical Aid beneficiaries had higher technique failure rates than National Health Insurance patients. Although low socioeconomic status did not predict fundamental outcomes such as patient survival or technique survival for PD patients in previous studies [16], [30], it might not be a major determinant to outcomes because the included subjects were in a managed-care setting or had taken a special care service from centers with a wide range of PD experiences. On the contrary, we evaluated a technique failure rate in claims database which comprised all Korean PD patients irrespective of hospital characteristics or center experiences. In addition, poor socioeconomic status generally put ESRD patients in a more disadvantageous position in terms of higher mortality and more frequent laboratory abnormalities [31], [32]. Moreover, limited health literacy, which was significantly related to socioeconomic status, is associated with health outcomes including mortality in patients with chronic kidney disease [33], whereas its association with adverse outcomes was not found in a study with 36 PD patients [34]. Although Medical Aid and National Health Insurance are a crude dichotomous classification, complex and rigorous criteria are applied into the classification process in Korea, including lack of family support and/or incapability of labor as well as low income. Therefore, the type of health security system could serve as a rough estimate for each patient's socioeconomic status in Korea, and it could be postulated that economic and functional status of patients and family support for them would generally affect the clinical outcomes in PD patients.
In the present study, cancer was a negative predictor for technique failure in the Fine and Gray model. Frequent medical checkup and paying more attention to their own health status would be associated with lower technique failure rates in PD patients with cancer. On the other hand, cancer is a well-known risk factor for mortality in PD patients [3]. When considering poor survival rate and low activity in ESRD patients with cancer, it is unlikely to change dialysis modalities without any inevitable reason.
Our study had several limitations. First, the database used in this study provided insufficient individual characteristics, inadequate clinical information, and no specific laboratory data. We could not collect data on membrane characteristics, residual renal function, health literacy level, and timing of referral to the nephrologists. Therefore, more valuable independent predictors could not be identified. In addition, the database did not include data on the cause of technique failure such as peritonitis, thus we could not recommend any specific strategy to decrease the technique failure rate in the future. Second, we excluded cases of technique failure that occurred within 3 months from commencing dialysis therapy because we would like to include only patients on “long-term dialysis” in this study. Descoeudres et al [35] emphasized high technique failure rate within the first 6 months on PD. Therefore, the technique failure rate in this study is likely to be underestimated. Last, the present study did not evaluate the effect of renal center characteristics, payment policy, physicians' acknowledgment, and patients' awareness for dialysis modality selection at dialysis initiation on technique failure in PD patients.
In spite of database-related inherent limitations, this is the first study on technique failure among Asian dialysis patients that used a national population-based data set. Technique failure was still a major concern in patients initiating PD in Korea, especially in diabetic patients and Medical Aid beneficiaries. The results of our study offer a basis for risk stratification for technique failure.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF, 2010-0027945) funded by the Ministry of Science, ICT & Future Planning (2010-0027945).
References
- 1.Jin D.C., Han J.S. Renal replacement therapy in Korea, 2012. Kidney Res Clin Pract. 2014;33:9–18. doi: 10.1016/j.krcp.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Renal Data System (2013) 2013. Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Available at: https://www.usrds.org/atlas13.aspx [Date accessed: 02 August 2015] [Google Scholar]
- 3.Kim H., Kim K.H., Park K., Kang S.W., Yoo T.H., Ahn S.V., Ahn H.S., Hann H.J., Lee S., Ryu J.H., Kim S.J., Kang D.H., Choi K.B., Ryu D.R. A population-based approach indicates an overall higher patient mortality with peritoneal dialysis compared to hemodialysis in Korea. Kidney Int. 2014;86:991–1000. doi: 10.1038/ki.2014.163. [DOI] [PubMed] [Google Scholar]
- 4.Choi H., Kim M., Kim H., Lee J.P., Lee J., Park J.T., Kim K.H., Ahn H.S., Hann H.J., Ryu D.R. Excess mortality among patients on dialysis: comparison with the general population in Korea. Kidney Res Clin Pract. 2014;33:89–94. doi: 10.1016/j.krcp.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shih Y.C., Guo A., Just P.M., Mujais S. Impact of initial dialysis modality and modality switches on Medicare expenditures of end-stage renal disease patients. Kidney Int. 2005;68:319–329. doi: 10.1111/j.1523-1755.2005.00413.x. [DOI] [PubMed] [Google Scholar]
- 6.Pajek J., Hutchison A.J., Bhutani S., Brenchley P.E., Hurst H., Perme M.P., Summers A.M., Vardhan A. Outcomes of peritoneal dialysis patients and switching to hemodialysis: a competing risks analysis. Perit Dial Int. 2014;34:289–298. doi: 10.3747/pdi.2012.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bechade C., Guittet L., Evans D., Verger C., Ryckelynck J.P., Lobbedez T. Early failure in patients starting peritoneal dialysis: a competing risks approach. Nephrol Dial Transplant. 2014;29:2127–2135. doi: 10.1093/ndt/gft055. [DOI] [PubMed] [Google Scholar]
- 8.Wong J.S., Port F.K., Hulbert-Shearon T.E., Carroll C.E., Wolfe R.A., Agodoa L.Y., Daugirdas J.T. Survival advantage in Asian American end-stage renal disease patients. Kidney Int. 1999;55:2515–2523. doi: 10.1046/j.1523-1755.1999.00464.x. [DOI] [PubMed] [Google Scholar]
- 9.Teixeira L., Rodrigues A., Carvalho M.J., Cabrita A., Mendonca D. Modelling competing risks in nephrology research: an example in peritoneal dialysis. BMC Nephrol. 2013;14:110. doi: 10.1186/1471-2369-14-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beuscart J.B., Pagniez D., Boulanger E., Lessore de Sainte Foy C., Salleron J., Frimat L., Duhamel A. Overestimation of the probability of death on peritoneal dialysis by the Kaplan-Meier method: advantages of a competing risks approach. BMC Nephrol. 2012;13:31. doi: 10.1186/1471-2369-13-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Quan H., Sundararajan V., Halfon P., Fong A., Burnand B., Luthi J.C., Saunders L.D., Beck C.A., Feasby T.E., Ghali W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 13.Fine J.P., Gray R.J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 14.Wanner C., Tonelli M., Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014;85:1303–1309. doi: 10.1038/ki.2014.31. [DOI] [PubMed] [Google Scholar]
- 15.Jager K.J., Merkus M.P., Dekker F.W., Boeschoten E.W., Tijssen J.G., Stevens P., Bos W.J., Krediet R.T. Mortality and technique failure in patients starting chronic peritoneal dialysis: results of The Netherlands Cooperative Study on the Adequacy of Dialysis. NECOSAD Study Group. Kidney Int. 1999;55:1476–1485. doi: 10.1046/j.1523-1755.1999.00353.x. [DOI] [PubMed] [Google Scholar]
- 16.Kumar V.A., Sidell M.A., Yang W.T., Jones J.P. Predictors of peritonitis, hospital days, and technique survival for peritoneal dialysis patients in a managed care setting. Perit Dial Int. 2014;34:171–178. doi: 10.3747/pdi.2012.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maiorca R., Vonesh E., Cancarini G.C., Cantaluppi A., Manili L., Brunori G., Camerini C., Feller P., Strada A. A six-year comparison of patient and technique survivals in CAPD and HD. Kidney Int. 1988;34:518–524. doi: 10.1038/ki.1988.212. [DOI] [PubMed] [Google Scholar]
- 18.Han S.H., Lee J.E., Kim D.K., Moon S.J., Kim H.W., Chang J.H., Kim B.S., Kang S.W., Choi K.H., Lee H.Y., Han D.S. Long-term clinical outcomes of peritoneal dialysis patients: single center experience from Korea. Perit Dial Int. 2008;28(Suppl 3):S21–S26. [PubMed] [Google Scholar]
- 19.Schaubel D.E., Blake P.G., Fenton S.S. Effect of renal center characteristics on mortality and technique failure on peritoneal dialysis. Kidney Int. 2001;60:1517–1524. doi: 10.1046/j.1523-1755.2001.00969.x. [DOI] [PubMed] [Google Scholar]
- 20.Chidambaram M., Bargman J.M., Quinn R.R., Austin P.C., Hux J.E., Laupacis A. Patient and physician predictors of peritoneal dialysis technique failure: a population based, retrospective cohort study. Perit Dial Int. 2011;31:565–573. doi: 10.3747/pdi.2010.00096. [DOI] [PubMed] [Google Scholar]
- 21.Kim D.K., Yoo T.H., Ryu D.R., Xu Z.G., Kim H.J., Choi K.H., Lee H.Y., Han D.S., Kang S.W. Changes in causative organisms and their antimicrobial susceptibilities in CAPD peritonitis: a single center's experience over one decade. Perit Dial Int. 2004;24:424–432. [PubMed] [Google Scholar]
- 22.Ryu J.H., Kim H., Kim K.H., Hann H.J., Ahn H.S., Lee S., Kim S.J., Kang D.H., Choi K.B., Ryu D.R. Improving survival rate of Korean patients initiating dialysis. Yonsei Med J. 2015;56:666–675. doi: 10.3349/ymj.2015.56.3.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lobbedez T., Verger C., Ryckelynck J.P., Fabre E., Evans D. Is assisted peritoneal dialysis associated with technique survival when competing events are considered? Clin J Am Soc Nephrol. 2012;7:612–618. doi: 10.2215/CJN.10161011. [DOI] [PubMed] [Google Scholar]
- 24.Fang W., Qian J., Lin A., Rowaie F., Ni Z., Yao Q., Bargman J.M., Oreopoulos D.G. Comparison of peritoneal dialysis practice patterns and outcomes between a Canadian and a Chinese centre. Nephrol Dial Transplant. 2008;23:4021–4028. doi: 10.1093/ndt/gfn372. [DOI] [PubMed] [Google Scholar]
- 25.Fang W., Yang X., Kothari J., Khandelwal M., Naimark D., Jassal S.V., Bargman J., Oreopoulos D.G. Patient and technique survival of diabetics on peritoneal dialysis: one-center's experience and review of the literature. Clin Nephrol. 2008;69:193–200. doi: 10.5414/cnp69193. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman S.W., Oxton L.L., Bidwell D., Wakeen M. Long-term outcome of diabetic patients receiving peritoneal dialysis. Perit Dial Int. 1996;16:63–68. [PubMed] [Google Scholar]
- 27.Konner K. Primary vascular access in diabetic patients: an audit. Nephrol Dial Transplant. 2000;15:1317–1325. doi: 10.1093/ndt/15.9.1317. [DOI] [PubMed] [Google Scholar]
- 28.Cotovio P., Rocha A., Carvalho M.J., Teixeira L., Mendonça D., Cabrita A., Rodrigues A. Better outcomes of peritoneal dialysis in diabetic patients in spite of risk of loss of autonomy for home dialysis. Perit Dial Int. 2014;34:775–780. doi: 10.3747/pdi.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sekercioglu N., Dimitriadis C., Pipili C., Elias R.M., Kim J., Oreopoulos D.G., Bargman J.M. Glycemic control and survival in peritoneal dialysis patients with diabetes mellitus. Int Urol Nephrol. 2012;44:1861–1869. doi: 10.1007/s11255-012-0180-6. [DOI] [PubMed] [Google Scholar]
- 30.de Andrade Bastos K., Qureshi A.R., Lopes A.A., Fernandes N., Barbosa L.M., Pecoits-Filho R., Divino-Filho J.C., Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD) Group Family income and survival in Brazilian Peritoneal Dialysis Multicenter Study Patients (BRAZPD): time to revisit a myth? Clin J Am Soc Nephrol. 2011;6:1676–1683. doi: 10.2215/CJN.09041010. [DOI] [PubMed] [Google Scholar]
- 31.Marinovich S., Lavorato C., Rosa-Diez G., Bisigniano L., Fernández V., Hansen-Krogh D. The lack of income is associated with reduced survival in chronic haemodialysis. Nefrologia. 2012;32:79–88. doi: 10.3265/Nefrologia.pre2011.Nov.11110. [DOI] [PubMed] [Google Scholar]
- 32.Ward M.M. Laboratory abnormalities at the onset of treatment of end-stage renal disease: are there racial or socioeconomic disparities in care? Arch Intern Med. 2007;167:1083–1091. doi: 10.1001/archinte.167.10.1083. [DOI] [PubMed] [Google Scholar]
- 33.Fraser S.D., Roderick P.J., Casey M., Taal M.W., Yuen H.M., Nutbeam D. Prevalence and associations of limited health literacy in chronic kidney disease: a systematic review. Nephrol Dial Transplant. 2013;28:129–137. doi: 10.1093/ndt/gfs371. [DOI] [PubMed] [Google Scholar]
- 34.Jain D., Sheth H., Green J.A., Bender F.H., Weisbord S.D. Health literacy in patients on maintenance peritoneal dialysis: prevalence and outcomes. Perit Dial Int. 2015;35:96–98. doi: 10.3747/pdi.2013.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Descoeudres B., Koller M.T., Garzoni D., Wolff T., Steiger J., Schaub S., Mayr M. Contribution of early failure to outcome on peritoneal dialysis. Perit Dial Int. 2008;28:259–267. [PubMed] [Google Scholar]