Abstract
We sought to determine linkage to and retention in HIV care after HIV diagnosis in foreign-born compared with US-born individuals. From a clinical data registry, we identified 619 patients aged ≥18 years with a new HIV diagnosis between 2000 and 2012. Timely linkage to care was the proportion of patients with an ICD-9 code for HIV infection (V08 or 042) associated with a primary care or infectious disease physician within 90 days of the index positive HIV test. Retention in HIV care was the presence of an HIV primary care visit in each 6-month period of the 24-month measurement period from the index HIV test. We used Cox regression analysis with adjustment for hypothesized confounders (age, gender, race/ethnicity, substance abuse, year and location of HIV diagnosis). Foreign-born comprised 36% (225/619) of the cohort. Index CD4 count was 225/μl (IQR 67–439/μl) in foreign-born compared with 328/μl (IQR 121–527/μl) in US-born (p<0.001). The proportion linked to care was 87% (196/225) in foreign-born compared with 77% (302/394) in US-born (p=0.002). The adjusted hazard ratio of linkage to HIV care in foreign-born compared with US-born was 1.28 (95% confidence interval [CI], 1.05–1.56). Once linked, there was no difference in retention in care or virologic suppression at 24 months. These results show that despite late presentation to HIV care, foreign-born persons can subsequently engage in HIV care as well as US-born. Interventions that promote HIV screening in foreign-born persons are a promising way to improve outcomes in these populations.
Keywords: immigrant health, foreign-born, HIV/AIDS, outcomes, linkage to care, engagement in care
INTRODUCTION
Virologic suppression and survival is predicated on engagement in HIV care, defined as uptake of HIV testing and linkage to and retention in consistent HIV primary care (Giordano et al., 2007; Ulett et al., 2009). Despite the importance of engagement in HIV care, only three-quarters of HIV-diagnosed persons in the U.S. are linked to care within 90 days of diagnosis and one-half are retained in care (Bradley et al., 2014; Gray et al., 2014). Lower outcomes of linkage to and retention in HIV care are found in racial and ethnic minorities and are important targets to address disparities in HIV outcomes (Bradley et al., 2014).
Foreign-born persons, many of whom are racial and ethnic minorities, represent an understudied but rising subset of the US population disproportionately affected by the HIV epidemic. Foreign-born comprise 13% of the US population but 16% of new HIV infections (Prosser, Tang, & Hall, 2012). HIV-infected foreign-born tend to be younger, present with more advanced infection, and progress to AIDS faster than their native-born counterparts (ART-CC et al., 2013; Johnson, Hu, & Dean, 2010; Marc et al., 2010; Staehelin et al., 2003).
Our objective was to characterize linkage, retention, and virologic suppression in foreign-born compared with US-born HIV infected individuals. We hypothesized that HIV-infected foreign-born persons are less likely to link to HIV care in a timely way compared with US-born.
METHODS
Study population and data sources
We analyzed data from the Partners Research Patient Data Registry (RPDR), which comprises 4.5 million patients who receive care at two large academic medical centers and their affiliated health centers (Technical Appendix). The health system reflects the diverse racial and ethnic composition of the Eastern Massachusetts catchment area (Massachusetts General Hospital Disparities Solution Center and MGH/MGPO Center for Quality and Safety). HIV care is provided in primary care practices and two hospital-based HIV clinics. Clinical data points are derived from hospital electronic medical records (EMRs), administrative databases, and billing data.
Exposure characterization
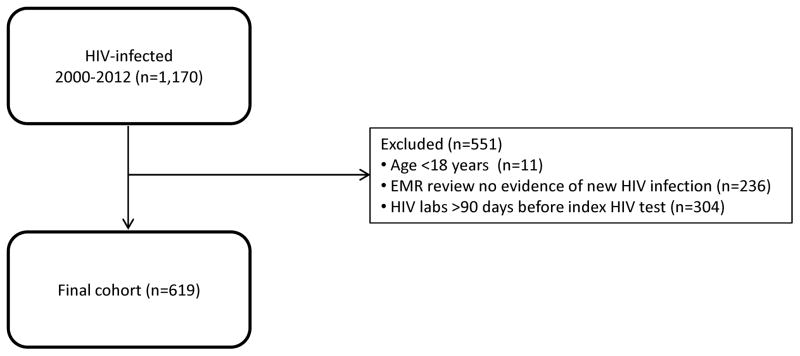
The eligible cohort (n=1,170) included all patients newly diagnosed with HIV infection (Figure 1). “Newly diagnosed” patients were those whose last HIV test was positive (index test) between 2000 and 2012. HIV tests included were enzyme immunoassay, direct antigen, Western Blot, and rapid antibody tests, for HIV-1 and HIV-2. We excluded 551 patients (Figure 1). Eleven were aged ≤18 years. To distinguish between new HIV diagnoses and confirmatory testing, we determined the duration of prior contact with our health care system. We categorized individuals with ≥30 days between the first clinical encounter and a positive HIV test as a new diagnosis. We reviewed the medical records of all 355 patients with <30 days follow-up prior to the index test and excluded 236 where the test represented confirmation of HIV infection. Consistent with a validated algorithm to identify new HIV diagnoses from the EMR, we excluded 304 who had a CD4 count or HIV viral load >90 days before the index HIV test. (Goetz, Hoang, Kan, Rimland, & Rodriguez-Barradas, 2014). The final cohort constituted 619 persons.
Figure 1.
Study flow chart of newly diagnosed HIV-infected patients in a large clinical data registry. EMR denotes electronic medical record.
Place of birth was determined using a previously validated algorithm that combines a coded field for primary language spoken with computer-aided review of free text notes (Levison et al., 2014). We considered a patient US-born if place of birth was documented as US mainland, Puerto Rico, or other US territory (U. S. Census Bureau).
Data elements
The primary outcomes were linkage to and retention in HIV care as defined by U.S. Department of Health and Human Services (DHHS) (Mugavero, Davila, Nevin, & Giordano, 2010; U.S. DHHS Health Resources and Services Administration, 2015). Timely linkage to care was the presence of an encounter with a primary care or infectious disease physician ≤90 days from the index test that resulted in a billing code for HIV infection (ICD-9 codes V08 or 042). We examined an alternate definition of linkage to care where the HIV-coded encounter occurred ≤30 days from the index test. Patients were considered retained in HIV care if they had a visit in each 6-month interval of the 24-month period following the index HIV test with the visit in each 6-month interval separated by ≥60 days. We calculated the proportion retained and limited the denominator to those with ≥1 HIV medical visit in the first 6 months of the 24-month measurement period, consistent with DHHS reporting practice. The secondary outcome was virologic suppression. We calculated the proportion of patients with HIV RNA <400 copies/ml using the closest HIV RNA to the 24-month mark within a 3 month range (21–27 months) (Horberg et al., 2010; Panel on Antiretroviral Guidelines for Adults and Adolescents, 2015).
We evaluated a priori covariates hypothesized as predictors of HIV care utilization: place of birth (foreign compared with US-born), age (per decade), year and location (inpatient versus outpatient) of index HIV test, race/ethnicity, gender, history of substance abuse, and index CD4. Self-identified race and ethnicity were obtained from the EMR and were categorized as White, Black, Hispanic, Asian, and Other (including American Indian and unknown). Substance abuse or dependence was categorized separately for alcohol, opioid, and cocaine and/or amphetamine and defined by the presence of an ICD-9 code or coded problem list in the EMR. In order to categorize year at HIV diagnosis, we performed a bi-variate analysis between calendar year of diagnosis and linkage to care. The years 2000 and 2001 had statistically significant lower linkage to care. Therefore, we categorized year of diagnosis as 2000–2001, 2002–2006, and 2007–2012 when state-mandated health insurance took effect. We evaluated the index CD4 dated 30 days before to 100 days after the index HIV test.
Statistical Analysis
We compared estimates of timely linkage to and retention in HIV care in the foreign-born and US-born cohorts using a chi-square test. We assessed the relationship between the aforementioned hypothesized predictors and time to linkage using Cox proportional hazards models with linkage censored at 90 days from the index HIV test. Because CD4 counts were often not obtained at the time of diagnosis, we defined index CD4 as the first CD4 count obtained within 100 days of the HIV test. This definition has the effect of confounding availability of index CD4 with the outcome of linkage to care. For this reason we did not include index CD4 in the multivariable model of linkage to care. We explored the impact of various factors (location of diagnosis, gender, nativity, and linkage to care) on having an index CD4 using chi-squared tests. We used multivariable logistic regression of the dichotomous outcome of retention in care, and adjusted for hypothesized predictors, which included index CD4 as a marker of baseline disease severity. We present adjusted hazard ratios (AHR) and adjusted odds ratios (AOR with 95% confidence intervals (CI).
Statistical tests were two-sided with a significance level of 0.05. We assessed differences in demographic and clinical characteristics between foreign-born and US-born patients using chi-squared tests for categorical data and Wilcoxon ranksum tests and t-tests for continuous data. All statistical analyses were performed using Stata (StataCorp, 2013. Stata Statistical Software: Release 13. College Station, TX: Stata Corporation). This study was approved by the Partners HealthCare Institutional Review Board (Boston, MA).
RESULTS
Cohort description
We identified 619 individuals with a new HIV diagnosis between 2000 and 2012 and 36% (n=225) were foreign-born (Table 1). The mean age was 41 years [SD ±10.6 years] and did not differ between the two groups. Foreign-born were more likely to be female (n=74, 33%) compared with US-born (n=88, 22%) (p=0.004). In foreign-born compared to US-born patients, there was a higher percentage of blacks (40% vs. 23%) and Hispanics (33% vs. 10%) (p<0.001). Inpatient HIV diagnosis occurred in 29% (n=66) of foreign-born and 26% (n=102) of US-born (p=0.35). Substance abuse was more common in the US-born group with alcohol abuse present in 25% (n=98), opioid in 12% (n=49), and cocaine/methamphetamine in 15% (n=61). In the foreign-born group alcohol abuse was present in 9% (n=20), opioid abuse in 2% (n=4), and cocaine/methamphetamine in 5% (n=11) (p<0.001).
Table 1.
Characteristics of patients with a new HIV diagnosis at a large urban health care system in Massachusetts, 2000–2012.
| Characteristic | Foreign-born (%) N=225 |
US-born (%) N=394 |
P-value |
|---|---|---|---|
| Age, mean years [SD ± years] | 40.5 [±10.5] | 41.4 [±10.7] | 0.34 |
| Females | 74 (33) | 88 (22) | 0.004 |
| Ethnicity/Race | <0.001 | ||
| White | 33 (15) | 236 (60) | |
| Black | 89 (40) | 91 (23) | |
| Hispanic | 76 (33) | 41 (10) | |
| Asian/Other/Unknown | 27 (12) | 26 (7) | |
| Year of HIV diagnosis | 0.51 | ||
| 2000–2001 | 28 (12) | 48 (12) | |
| 2002–2006 | 107 (48) | 170 (43) | |
| 2007–2012 | 90 (40) | 176 (45) | |
| Location of HIV diagnosis | 0.35 | ||
| Inpatient | 66 (29) | 102 (26) | |
| Outpatient | 159 (71) | 292 (74) | |
| CD4 count index, median cells/μl [IQR]* | 225 [67–439]† | 328 [121–527]‡ | 0.0003 |
| Substance abuse/dependence | |||
| Alcohol | 20 (9) | 98 (25) | <0.001 |
| Opioid | 4 (2) | 49 (12) | <0.001 |
| Cocaine/methamphetamine | 11 (5) | 61 (15) | <0.001 |
Abbreviation: SD= standard deviation; IQR= interquartile range.
Available data for 579 of 619 patients.
Available data for 215 of 225 patients.
Available data for 364 of 394 patients.
Of the 619 individuals, 579 had an available index CD4 cell count of whom 92% (364/394) were US born and 95% (215/225) were foreign-born, p=0.12. The median index CD4 count in newly diagnosed foreign-born was 225 cells/μl [IQR 67–439/μl] compared with 328 cells/μl [IQR 121–527/μl] in US-born (p=0.0003). When stratified by gender, median index CD4 count for foreign-born males was 190 cells/μl, [IQR 57–401]); foreign-born females was 286 cells/μl [IQR 89–529 cells/μl]; US-born males was 327 cells/μl [IQR 112–521]; and US-born females was 371 cells/μl [IQR 124–592 cells/μl].
Leading up to diagnosis, there was no significant difference in frequency of HIV testing in this health system between foreign-born and US-born individuals (p=0.28), and 76% (n=473) of all individuals had one HIV test.
Of the 607/619 individuals who had language data coded in the hospital database, 40% (87/221) of the foreign-born cohort identified as primary non-English language speakers. Spanish was the primary language in 61% (53/87) of this group. Other frequent non-English languages were Portuguese, French and Haitian Creole, and Cambodian.
As of 2013, there were 71 known deaths. Thirty-seven deaths occurred within 24 months of HIV diagnosis and 12 deaths occurred within the first 90 days. There was no difference in deaths by place of birth.
Linkage to care
The proportion of individuals with timely linkage to HIV care in the US-born group was 77% (302/394) [95% CI 72–81%] compared with 87% (196/225) [95% CI 82–91%] in the foreign-born group, p=0.002. In the alternate definition of linkage to care, where timely linkage represented a primary care HIV encounter <30 days from HIV diagnosis, the result was similar where the proportion of US-born linked to HIV care was 66% (260/394) [95% CI 61–71%] vs. 74% (166/225) [95% CI 67–80%] in the foreign-born group, p=0.04. When stratified by gender and place of birth, the percent with timely linkage to care was 67% [95% CI 57–76%] for US-born females, 79% [95% CI 74–84%] for US-born males, 80% [95% CI 69–87%] for foreign-born females and 91% [95% CI 85–94%] for foreign-born males. Of the 619 patients, 58 never returned for outpatient HIV care, 13% (n=50) of US-born, and 4% (N=8) of foreign-born, (p<0.001).
In the Cox model, the adjusted hazard ratio of linkage to care in foreign-born individuals compared with US-born was 1.28 (95% CI, 1.05–1.56) (Table 2). Females (AHR = 0.73; 95% CI, 0.59–0.90), those diagnosed with opioid abuse disorder (AHR = 0.58; 95% CI, 0.39–0.86), those diagnosed with HIV as an outpatient (AHR = 0.56; 95% CI, 0.45–0.69), and those diagnosed in the years 2000–2001 (AHR = 0.34; 95% CI, 0.24–0.48), had longer time to linkage to HIV care. Age; race/ethnicity; alcohol or cocaine abuse; and the years 2007–2012, when state-mandated health insurance took effect, compared with 2002–2006, were not significantly associated with linkage to care.
Table 2.
Multivariable Cox proportional hazards model for the primary end point of timely linkage to care within 90 days of HIV diagnosis.
| Characteristic | N=619 Adjusted Hazard Ratioa (95% CI) |
P-value |
|---|---|---|
| Foreign-born | 1.28 (1.05–1.56) | 0.016 |
| Age (per decade) | 0.94 (0.86–1.02) | 0.151 |
| Female gender | 0.73 (0.59–0.90) | 0.003 |
| White race/ethnicity | 1.19 (0.98–1.44) | 0.085 |
| Alcohol abuse disorder† | 0.90 (0.69–1.17) | 0.439 |
| Opioid abuse disorder† | 0.58 (0.39–0.86) | 0.006 |
| Cocaine abuse disorder† | 1.04 (0.76–1.43) | 0.801 |
| Outpatient diagnosis | 0.56 (0.45–0.69) | <0.001 |
| Year of HIV diagnosis 2000–2001* | 0.34 (0.24–0.48) | <0.001 |
| Year of HIV diagnosis 2007–2012* | 0.94 (0.78–1.13) | 0.525 |
Abbreviation: CI= confidence interval.
Adjusted for all factors shown
One or more ICD9 billing codes vs. none
Reference group is year of HIV diagnosis 2002–2006
Having an index CD4 count measurement available was associated with being diagnosed with HIV as an inpatient and, as expected, with timely linkage to care. Of those individuals who received an HIV diagnosis as an inpatient, 97% (163/168) had an index CD4 count, compared with 92% (416/451) in those who were diagnosed as an outpatient (p=0.03). Those with timely linkage to care were more likely to have had an index CD4 count compared to those who did not link to care within 90 days (84% vs. 25%, p<0.001) and a lower index CD4 count (median: 278 cells/μl [IQR: 82–500] vs. 388 cells/μl [IQR: 181–581], p=0.002). These CD4 count trends were consistent in both US-born and foreign-born groups.
Retention in care
After excluding 11 individuals with <24 months of follow-up and 91 without an HIV visit in the first 6-month period, 517 patients were included in the retention analysis. At 24 months, 69% (355/517) met the DHHS definition of continuous retention in care. In the US-born, 67% (210/313) [95% 61–73%] were retained in HIV care through 24 months compared with 71% (145/204) [95% CI 64–77] of foreign-born (p=0.34). In a logistic regression model adjusting for predefined covariates, continuous retention in care through 24 months was associated with white race (AOR = 1.72; 95% CI, 1.09–2.71) and lower index CD4 (AOR 0.95; 95% CI, 0.92–0.99) (Table 3).
Table 3.
Multivariable logistic regression analysis of predictors of 24-month retention in HIV care
| Characteristic | N=500 Adjusted Odds Ratioa (95% CI) |
P-value |
|---|---|---|
| Foreign-born | 1.34 (0.84–2.12) | 0.222 |
| Age (per decade) | 1.01 (0.83–1.22) | 0.921 |
| Female gender | 0.92 (0.57–1.47) | 0.719 |
| White race/ethnicity* | 1.72 (1.09–2.71) | 0.020 |
| Opioid abuse disorder† | 0.63 (0.29–1.39) | 0.251 |
| Index CD4 count (per 50 cells/μl) | 0.95 (0.92–0.99) | 0.006 |
Abbreviation: CI= confidence interval.
Reference category is non-White race/ethnicity.
Reference category is no substance abuse history.
Virologic suppression
Of the 355 individuals retained in care at 24 months, 285 had a viral load (HIV RNA) available of whom 58% (n=164) were US-born and 42% (n=121) were foreign-born, p=0.21. Overall, 84% (n=240) of the cohort had virologic suppression (HIV RNA <400 copies/ml). Virologic suppression was present in 82% of US-born (134/164) and 88% of foreign-born (106/121), p=0.177.
DISCUSSION
Foreign-born individuals, a rapidly growing part of the US population, contribute a disproportionally high number of new HIV cases and may be at higher risk for poor HIV outcomes (Prosser et al., 2012). Foreign-born patients are also difficult to identify and study on a population level, as country of origin is typically excluded from the EMR. We employed a validated algorithm to identify, characterize, and follow HIV-infected foreign-born patients in a large urban healthcare system (Levison et al., 2014). Compared with US-born, newly-infected foreign-born individuals presented to HIV primary care with lower CD4 counts, levels comparable to many resource-limited settings (Braitstein et al., 2006; Nash et al., 2008). Lower index CD4 count itself is a prognostic factor for AIDS and death (Antiretroviral Therapy Cohort, 2007). The difference in index CD4 count between foreign-born and US-born individuals represents an estimated 1 to 2 year delay in HIV diagnosis in foreign-born (Lang et al., 1989). While foreign-born patients entered HIV care with more advanced disease, they were at least as engaged and adherent to care as the US-born group.
The earlier linkage to care that we observed in the foreign-born group was contrary to our hypothesis and the findings of another large study on linkage to care, by Torian et al., that used New York City Department of Health surveillance data (Torian, Wiewel, Liu, Sackoff, & Frieden, 2008). Since index CD4 count was substantially lower in the foreign-born cohort, we hypothesize that foreign-born linked to care more quickly than US-born due to more symptomatic disease at diagnosis and a greater perceived need for HIV care. In the multivariable model, we also found that higher index CD4 decreased the odds of retention in care. The absence of symptomatic disease has been described in multiple settings as an important barrier to uptake of HIV care (Johnston et al., 2013; Turner et al., 2000).
Lower index CD4 count in the foreign-born group likely relates to delays in HIV diagnosis. We suspect that even prior to entering our healthcare system, unequal barriers to HIV testing due to perceived need, stigma, fear of deportation, and lack of a regular health care provider, may have contributed to the disparity in baseline disease severity (De Jesus, Carrete, Maine, & Nalls, 2015; Hacker et al., 2011; Levy et al., 2007; Ojikutu, Nnaji, Sithole-Berk, Bogart, & Gona, 2014; Ransome et al., 2015). While US Immigration and Customs Enforcement detention facilities house nearly 32,000 immigrants per day, HIV screening is not routine (Martinez-Donate et al., 2015; Venters, McNeely, & Keller, 2009). This public health practice departs from guidance of the DHHS and the National Commission on Correctional Health Care who both endorse universal, opt-out HIV testing, and may serve as an important impediment to HIV diagnosis and linkage to care in foreign-born (National Commission on Correctional Health Care, 2014; Panel on Antiretroviral Guidelines for Adults and Adolescents, 2015; U.S. Immigration and Customs Enforcement, 2011). Since substance abuse treatment centers in the US are important sites for HIV counseling and testing, the higher prevalence of substance abuse history in the US-born group may represent greater opportunities for HIV testing and earlier diagnosis (Pollack & D’Aunno, 2010).
Once delays in presentation to HIV care were overcome through linkage to care, we found no difference in retention in HIV care or virologic suppression in foreign-born compared with US-born persons, a finding supported in several cohorts (Breton et al., 2007; Poon, Dang, Davila, Hartman, & Giordano, 2013; Staehelin et al., 2003). Unmeasured protective factors that may support engagement in HIV care in foreign-born include social support and cultural values that prioritize the family and community well-being (Perez & Cruess, 2014; Remien et al., 2015).
Women in our study were less likely than men to link to care. In both US and foreign-born cohorts, index CD4 count was higher in women than men. EuroCoord, a large European collaboration of HIV cohorts, reported elevated mortality risk in HIV-infected migrant women that was related to the mode of HIV transmission and country of origin (Migrants Working Group on behalf of Cohere in EuroCoord, 2015). Together these data suggest women face ongoing barriers to HIV care that can influence women’s perceived need for HIV care particularly when disease is asymptomatic. Factors such as limited access to care, trauma, and family responsibilities may increase the risk for poor HIV outcomes in women (Aziz & Smith, 2011; Metsch et al., 2015).
Linkage to HIV care was not significantly different in the years 2007 to 2012 compared with 2002 to 2006, the period before state health care reform. This finding is consistent with a prior study that found that access to universal health insurance in Massachusetts improved insurance coverage but did not address language and other cultural factors that perpetuate health disparities (Maxwell, Cortes, Schneider, Graves, & Rosman, 2011).
This analysis has several limitations. The algorithm used to identify new HIV diagnoses may be subject to misclassification, though we attempted to address this by EMR review and including those with documented incident HIV infection. Some potentially important socio-demographic factors were unavailable (e.g. residency status, income, HIV transmission category, and insurance and country of origin data for all patients). Documentation of transfer of care was unavailable as data were drawn from an open healthcare system. Substance abuse may be undercounted with ICD-9 coding. Not all patients had available CD4 and viral load data, though there were no differences in the proportion of missing data between foreign-born and US-born.
These results identify an addressable gap in the HIV treatment cascade of foreign-born HIV-infected individuals: given their likelihood of remaining in care once diagnosed, interventions to promote earlier HIV diagnosis of foreign-born may portend improved clinical outcomes.
Acknowledgments
The work was supported by the US National Institute of Mental Health (K23 MH100978); National Institute of Allergy and Infectious Diseases (R01 AI042006); Harvard University Center for AIDS Research (P30-AI060354); Harvard Catalyst/Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award) 8UL1TR000170-05 and 8KL2TR000168-05; and the Harvard Medical School Eleanor and Miles Shore 50th Anniversary Award. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
Technical Appendix
METHODS
Study population and data sources
The Partners Research Patient Data Registry (RPDR) comprises data on 4.5 million patients who receive care in two large urban academic medical centers and their affiliated health centers in Boston. HIV care is provided in primary internal medicine practices as well as in two hospital-based HIV clinics, one at Massachusetts General Hospital that serves approximately 1200 patients and one at Brigham and Women’s Hospital that serves approximately 600 patients (Robbins et al., 2010). Fellows, residents, and nurse practitioners under the supervision of attending physicians or attending physicians alone manage patient care. In the registry, clinical data points are derived from hospital electronic medical records (EMRs), administrative databases, and billing data. Recorded variables include demographics, clinical encounters with associated notes, diagnoses [International Classification of Diseases, Ninth revision, Clinical Modification (ICD-9-CM) codes and locally specified codes], medications, procedures, and test results. The RPDR uses the Social Security Master Index to obtain vital status information, which is updated every two months. The Partners HIV Cohort, from which this cohort was drawn, is an observational cohort of HIV-infected persons identified using the RPDR and composed of patients from the Brigham and Women’s Hospital and Massachusetts General Hospital (Triant, Brown, Lee, & Grinspoon, 2008; Triant et al., 2010)
- Robbins GK, Johnson KL, Chang Y, Jackson KE, Sax PE, Meigs JB, Freedberg KA. Predicting virologic failure in an HIV clinic. Clin Infect Dis. 2010;50(5):779–786. doi: 10.1086/650537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triant VA, Brown TT, Lee H, Grinspoon SK. Fracture prevalence among human immunodeficiency virus (HIV)-infected versus non-HIV-infected patients in a large U.S. healthcare system. J Clin Endocrinol Metab. 2008;93(9):3499–3504. doi: 10.1210/jc.2008-0828. jc.2008-0828 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triant VA, Regan S, Lee H, Sax PE, Meigs JB, Grinspoon SK. Association of immunologic and virologic factors with myocardial infarction rates in a US healthcare system. J Acquir Immune Defic Syndr. 2010;55(5):615–619. doi: 10.1097/QAI.0b013e3181f4b752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Footnotes
These data were presented in part at the 10th International Conference on HIV treatment and Prevention Adherence, on June 28, 2015, Miami, Florida.
Conflicts of Interest. All authors have declared that no competing interests exist.
Human Subjects Protection. Study procedures were approved by Partners HealthCare Human Research Committee (Boston, Massachusetts, USA).
References
- Antiretroviral Therapy Cohort, Collaboration. Importance of baseline prognostic factors with increasing time since initiation of highly active antiretroviral therapy: collaborative analysis of cohorts of HIV-1-infected patients. J Acquir Immune Defic Syndr. 2007;46(5):607–615. doi: 10.1097/QAI.0b013e31815b7dba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ART-CC. Shepherd BE, Jenkins CA, Parrish DD, Glass TR, Cescon A, … Sterling TR. Higher rates of AIDS during the first year of antiretroviral therapy among migrants: the importance of tuberculosis. AIDS. 2013;27(8):1321–1329. doi: 10.1097/QAD.0b013e32835faa95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aziz M, Smith KY. Challenges and successes in linking HIV-infected women to care in the United States. Clin Infect Dis. 2011;52(Suppl 2):S231–237. doi: 10.1093/cid/ciq047. [DOI] [PubMed] [Google Scholar]
- Bradley H, Hall HI, Wolitski RJ, Van Handel MM, Stone AE, LaFlam M, … Valleroy LA. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV--United States, 2011. MMWR Morb Mortal Wkly Rep. 2014;63(47):1113–1117. [PMC free article] [PubMed] [Google Scholar]
- Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, Miotti P …groups, A. R. T. Cohort Collaboration. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367(9513):817–824. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- Breton G, Lewden C, Spire B, Salmon D, Brun-Vezinet F, Duong M …Group, Aproco Copilote Anrs Co Study. Characteristics and response to antiretroviral therapy of HIV-1-infected patients born in Africa and living in France. HIV Med. 2007;8(3):164–170. doi: 10.1111/j.1468-1293.2007.00447.x. [DOI] [PubMed] [Google Scholar]
- De Jesus M, Carrete C, Maine C, Nalls P. “Getting tested is almost like going to the Salem witch trials”: discordant discourses between Western public health messages and sociocultural expectations surrounding HIV testing among East African immigrant women. AIDS Care. 2015;27(5):604–611. doi: 10.1080/09540121.2014.1002827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano TP, Gifford AL, White AC, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, … Morgan RO. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–1499. doi: 10.1086/516778. CID41288 [pii] [DOI] [PubMed] [Google Scholar]
- Goetz MB, Hoang T, Kan VL, Rimland D, Rodriguez-Barradas M. Development and validation of an algorithm to identify patients newly diagnosed with HIV infection from electronic health records. AIDS Res Hum Retroviruses. 2014;30(7):626–633. doi: 10.1089/AID.2013.0287. [DOI] [PubMed] [Google Scholar]
- Gray KM, Cohen SM, Hu X, Li J, Mermin J, Hall HI. Jurisdiction level differences in HIV diagnosis, retention in care, and viral suppression in the United States. J Acquir Immune Defic Syndr. 2014;65(2):129–132. doi: 10.1097/QAI.0000000000000028. [DOI] [PubMed] [Google Scholar]
- Hacker K, Chu J, Leung C, Marra R, Pirie A, Brahimi M, … Marlin RP. The impact of Immigration and Customs Enforcement on immigrant health: perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011;73(4):586–594. doi: 10.1016/j.socscimed.2011.06.007. S0277-9536(11)00352-2 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horberg MA, Aberg JA, Cheever LW, Renner P, O’Brien Kaleba E, Asch SM. Development of national and multiagency HIV care quality measures. Clin Infect Dis. 2010;51(6):732–738. doi: 10.1086/655893. [DOI] [PubMed] [Google Scholar]
- Johnson AS, Hu X, Dean HD. Epidemiologic differences between native-born and foreign-born black people diagnosed with HIV infection in 33 U.S. states, 2001–2007. Public Health Rep. 2010;125(Suppl 4):61–69. doi: 10.1177/00333549101250S410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston SS, Juday T, Seekins D, Hebden T, Fulcher N, Farr AM, … Mullins CD. Patterns and correlates of linkage to appropriate HIV care after HIV diagnosis in the US Medicaid population. Sex Transm Dis. 2013;40(1):18–25. doi: 10.1097/OLQ.0b013e3182782014. [DOI] [PubMed] [Google Scholar]
- Lang W, Perkins H, Anderson RE, Royce R, Jewell N, Winkelstein W., Jr Patterns of T lymphocyte changes with human immunodeficiency virus infection: from seroconversion to the development of AIDS. J Acquir Immune Defic Syndr. 1989;2(1):63–69. [PubMed] [Google Scholar]
- Levison J, Triant V, Losina E, Keefe K, Freedberg K, Regan S. Development and validation of a computer-based algorithm to identify foreign-born patients with HIV infection from the electronic medical record. Appl Clin Inform. 2014;5(2):557–570. doi: 10.4338/ACI-2014-02-RA-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy V, Prentiss D, Balmas G, Chen S, Israelski D, Katzenstein D, Page-Shafer K. Factors in the delayed HIV presentation of immigrants in Northern California: implications for voluntary counseling and testing programs. J Immigr Minor Health. 2007;9(1):49–54. doi: 10.1007/s10903-006-9015-9. [DOI] [PubMed] [Google Scholar]
- Marc LG, Patel-Larson A, Hall HI, Hughes D, Alegria M, Jeanty G, … Jean-Louis E. HIV among Haitian-born persons in the United States, 1985–2007. AIDS. 2010;24(13):2089–2097. doi: 10.1097/QAD.0b013e32833bedff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Donate AP, Rangel MG, Rhoads N, Zhang X, Hovell M, Magis-Rodriguez C, Gonzalez-Fagoaga E. Identifying opportunities to increase HIV testing among mexican migrants: a call to step up efforts in health care and detention settings. PLoS One. 2015;10(4):e0123631. doi: 10.1371/journal.pone.0123631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massachusetts General Hospital Disparities Solution Center and MGH/MGPO Center for Quality and Safety. [Accessed on June 2016, 2016];Annual report on equity in health care quality. 2014 Available at: http://qualityandsafety.massgeneral.org/measures/2014_AREHQ_FINAL_PUBLIC.pdf.
- Maxwell J, Cortes DE, Schneider KL, Graves A, Rosman B. Massachusetts’ health care reform increased access to care for Hispanics, but disparities remain. Health Aff (Millwood) 2011;30(8):1451–1460. doi: 10.1377/hlthaff.2011.0347. 30/8/1451 [pii] [DOI] [PubMed] [Google Scholar]
- Metsch L, Philbin MM, Parish C, Shiu K, Frimpong JA, Giang le M. HIV testing, care, and treatment among women who use drugs from a global perspective: progress and challenges. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S162–168. doi: 10.1097/QAI.0000000000000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migrants Working Group on behalf of Cohere in EuroCoord. Mortality in migrants living with HIV in western Europe (1997–2013): a collaborative cohort study. Lancet HIV. 2015;2(12):e540–549. doi: 10.1016/S2352-3018(15)00203-9. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24(10):607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash D, Katyal M, Brinkhof MW, Keiser O, May M, Hughes R, … Egger M. Long-term immunologic response to antiretroviral therapy in low-income countries: a collaborative analysis of prospective studies. AIDS. 2008;22(17):2291–2302. doi: 10.1097/QAD.0b013e3283121ca9. 00002030-200811120-00008 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Commission on Correctional Health Care. [Accessed February 16, 2016];Position Statement: Administrative management of HIV in correctional institutions. 2014 Available at: http://www.ncchc.org/administrative-management-of-hiv-in-correctional-institutions.
- Ojikutu B, Nnaji C, Sithole-Berk J, Bogart LM, Gona P. Barriers to HIV Testing in Black Immigrants to the U.S. J Health Care Poor Underserved. 2014;25(3):1052–1066. doi: 10.1353/hpu.2014.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1 Infected Adults and Adolescents. Bethesda, MD: Department of Health and Human Services; 2015. [Accessed Feburary 20, 2016]. Available at: www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. [Google Scholar]
- Perez GK, Cruess D. The impact of familism on physical and mental health among Hispanics in the United States. Health Psychology Review. 2014;8(1):95–127. doi: 10.1080/17437199.2011.569936. [DOI] [PubMed] [Google Scholar]
- Pollack HA, D’Aunno T. HIV testing and counseling in the nation’s outpatient substance abuse treatment system, 1995–2005. J Subst Abuse Treat. 2010;38(4):307–316. doi: 10.1016/j.jsat.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Poon KK, Dang BN, Davila JA, Hartman C, Giordano TP. Treatment outcomes in undocumented Hispanic immigrants with HIV infection. PLoS One. 2013;8(3):e60022. doi: 10.1371/journal.pone.0060022. PONE-D-12-40183 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosser AT, Tang T, Hall HI. HIV in persons born outside the United States, 2007–2010. JAMA. 2012;308(6):601–607. doi: 10.1001/jama.2012.9046. [DOI] [PubMed] [Google Scholar]
- Ransome Y, Terzian A, Addison D, Braunstein S, Myers J, Abraham B, Nash D. Expanded HIV testing coverage is associated with decreases in late HIV diagnoses. AIDS. 2015;29(11):1369–1378. doi: 10.1097/QAD.0000000000000684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien RH, Bauman LJ, Mantell JE, Tsoi B, Lopez-Rios J, Chhabra R, … Warne P. Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York City. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S16–24. doi: 10.1097/QAI.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staehelin C, Rickenbach M, Low N, Egger M, Ledergerber B, Hirschel B, … Furrer H. Migrants from Sub-Saharan Africa in the Swiss HIV Cohort Study: access to antiretroviral therapy, disease progression and survival. AIDS. 2003;17(15):2237–2244. doi: 10.1097/01.aids.0000088208.77946.68. [DOI] [PubMed] [Google Scholar]
- Torian LV, Wiewel EW, Liu KL, Sackoff JE, Frieden TR. Risk factors for delayed initiation of medical care after diagnosis of human immunodeficiency virus. Arch Intern Med. 2008;168(11):1181–1187. doi: 10.1001/archinte.168.11.1181. 168/11/1181 [pii] [DOI] [PubMed] [Google Scholar]
- Turner BJ, Cunningham WE, Duan N, Andersen RM, Shapiro MF, Bozzette SA, … Zierler S. Delayed medical care after diagnosis in a US national probability sample of persons infected with human immunodeficiency virus. Arch Intern Med. 2000;160(17):2614–2622. doi: 10.1001/archinte.160.17.2614. [DOI] [PubMed] [Google Scholar]
- U. S. Census Bureau. [Accessed Februrary 20, 2016];About foreign-born population. Available at: http://www.census.gov/topics/population/foreign-born/about.html.
- U.S. DHHS Health Resources and Services Administration. [Accessed February 20, 2016];HIV/AIDS Bureau Performance Measures, January 2015. 2015 Available at: http://hab.hrsa.gov/deliverhivaidscare/systemlevelmeasures.pdf.
- U.S. Immigration and Customs Enforcement. [Accessed February 16, 2016];2009 Detention Reform Fact Sheet, December 2, 2011. 2011 Available at: http://www.ice.gov/factsheets/2009detention-reform.
- Ulett KB, Willig JH, Lin HY, Routman JS, Abroms S, Allison J, … Mugavero MJ. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–49. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venters HD, McNeely J, Keller AS. HIV screening and care for immigration detainees. Health Hum Rights. 2009;11(2):89–100. [PubMed] [Google Scholar]