Abstract
Purpose of review
Despite the tremendous individual suffering and socioeconomic burden caused by osteoarthritis, there are currently no effective disease-modifying treatment options. This is in part because of our incomplete understanding of osteoarthritis disease mechanism. This review summarizes recent developments in therapeutic targets identified from surgical animal models of osteoarthritis that provide novel insight into osteoarthritis pathology and possess potential for progression into preclinical studies.
Recent findings
Several candidate pathways and processes that have been identified include chondrocyte autophagy, growth factor signaling, inflammation, and nociceptive signaling. Major strategies that possess therapeutic potential at the cellular level include inhibiting autophagy suppression and decreasing reactive oxygen species (ROS) production. Cartilage anabolism and prevention of cartilage degradation has been shown to result from growth factor signaling modulation, such as TGF-β, TGF-α, and FGF; however, the results are context-dependent and require further investigation. Pain assessment studies in rodent surgical models have demonstrated potential in employing anti-NGF strategies for minimizing osteoarthritis-associated pain.
Summary
Studies of potential therapeutic targets in osteoarthritis using animal surgical models are helping to elucidate osteoarthritis pathology and propel therapeutics development. Further studies should continue to elucidate pathological mechanisms and therapeutic targets in various joint tissues to improve overall joint health.
Keywords: animal surgical models, osteoarthritis, therapeutic targets
INTRODUCTION
Osteoarthritis is the most common type of arthritis and the primary cause of disability in elderly populations [1]. In fact, it has been estimated that 10% of men and 18% of women above 60 years of age report symptomatic osteoarthritis worldwide [2]. Although ageing is an important risk factor, osteoarthritis is multifactorial in nature and contributing sources to the pathophysiology of osteoarthritis include genetics, sex, weight, metabolism, and prior joint injury [3]. The most notable feature of osteoarthritis is articular cartilage degradation, however pathological changes can occur in all joint tissues including the underlying subchondral bone, as well as the supporting synovial membrane, ligaments, and menisci in the knee joint [3]. As articular cartilage is both aneural and avascular, changes in these tissues act as potential causes of symptomatic pain, which necessitates further research into the interplay of joint tissues as a whole in the pathology of osteoarthritis.
Despite major individual and socioeconomic burden inflicted by osteoarthritis, there are currently no effective disease-modifying therapies, and existing symptomatic treatment options are limited with unwanted side effects [4]. Our inability to diagnose osteoarthritis prior to irreversible joint damage hinders favorable management of the disease [5]. Better understanding of osteoarthritis pathogenesis is therefore crucial for identifying novel therapeutic targets. To date, the most commonly used animal models for the study of osteoarthritis pathophysiology are age-associated (spontaneous) and instability-induced through joint surgery. Among the most widely used surgical techniques include anterior cruciate ligament transection (ACLT) and destabilization of the medial meniscus (DMM) in rodents, which models human posttraumatic osteoarthritis (PTOA), and structural similarity [6]. In these modes, disease onset and progression occur with high reproducibility, which allows for the evaluation of specific genetic manipulations or pharmacological interventions on osteoarthritis progression. This review will focus on recent work on therapeutic targets identified from animal surgical models that provide novel insight into osteoarthritis pathology with potential for further progression into preclinical studies.
Box 1.
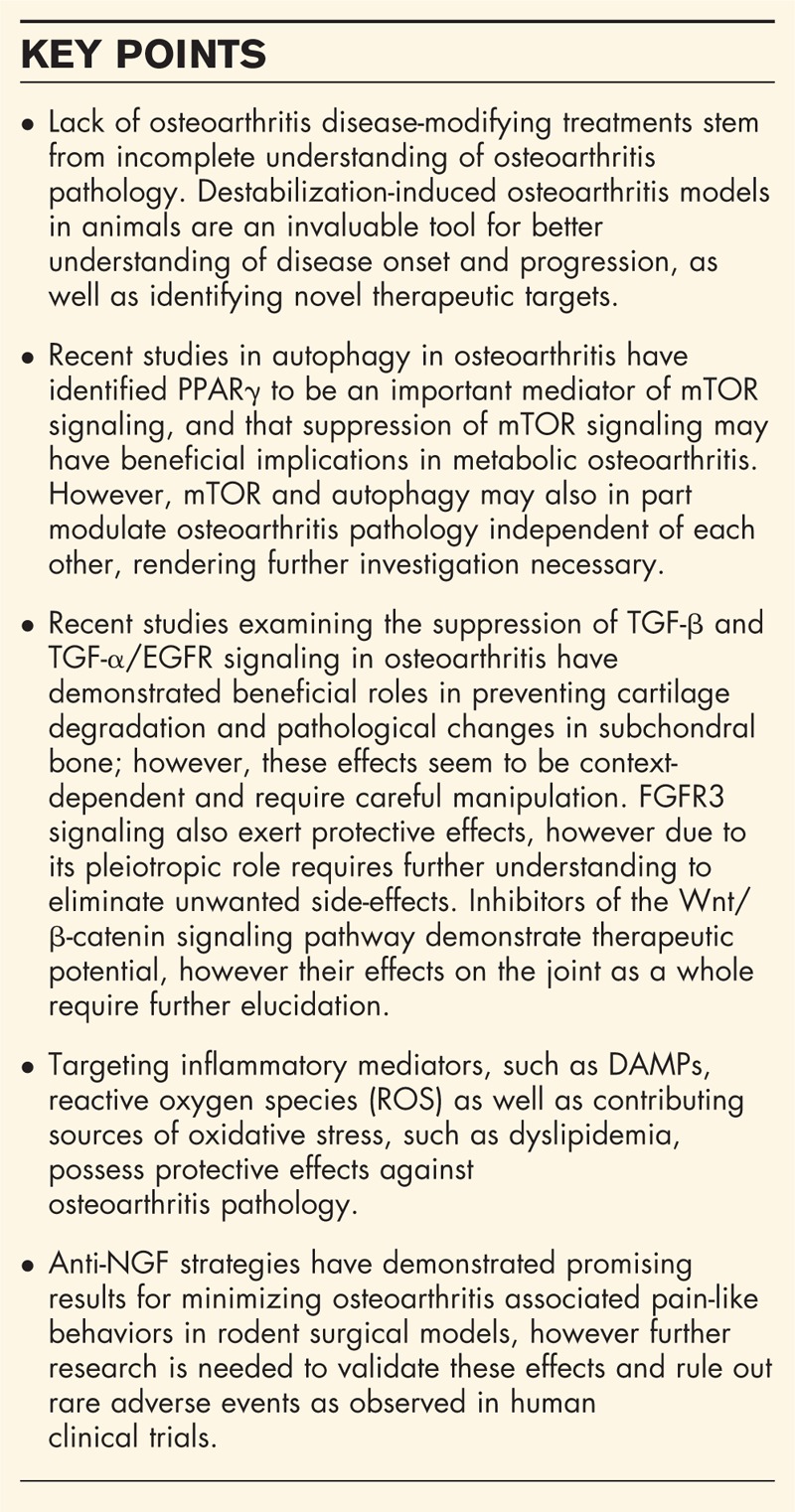
no caption available
CHONDROCYTE SURVIVAL AND AUTOPHAGY
Macroautophagy (referred to simply as ‘autophagy’) is a highly conserved eukaryotic process whereby damaged or harmful cytoplasmic materials are translocated to the lysosome for degradation [7]. It is most notably known for its roles in protecting cells from conditions of cellular stress, such as oxidative stress, endoplasmic reticulum stress, hypoxia, and nutrient and growth factor withdrawal, through maintenance of nutrient and energy homeostasis [8]. Alterations in autophagy occur in a variety of disease states, thus understanding these dysregulations in the disease context may bear therapeutic implications.
Much research has been done demonstrating an extensive link between autophagy and osteoarthritis, in which a compensatory increase in key autophagy markers appears in early osteoarthritis pathogenesis but is reduced in late osteoarthritis in parallel with increased chondrocyte apoptosis [9,10]. This link was further supported when mice with cartilage-specific deletion of mammalian target of rapamycin (mTOR), a serine/threonine protein kinase that functions as a key suppressor of autophagy, exhibited protection from DMM-induced osteoarthritis [11▪▪]. Vasheghani et al.[12▪▪] went onto identify peroxisome proliferator-activated receptor gamma (PPARγ) to be an important player in maintaining mTOR signaling in cartilage homeostasis, where they showed cartilage-specific PPARγ deficiency to cause an accelerated osteoarthritis phenotype that was subsequently rescued in PPARγ/mTOR double knock-out mice. On the basis of PPARγs known roles in regulating metabolic homeostasis, inflammation and adipogenesis, its involvement in mTOR signaling reinforces the crosstalk between cellular metabolism, autophagy, and cell survival [13]. Indeed, intraperitoneal administration of rapamycin, an mTOR inhibitor, markedly reduced surgically induced osteoarthritis severity in wild-type as well as db/db (leptin receptor mutation) mice, suggesting therapies that suppress mTOR and upregulate autophagy to also be beneficial in metabolic osteoarthritis [14,15▪▪].
Interestingly, Alvarez-Garcia et al.[16▪] recently demonstrated REDD1, an endogenous inhibitor of mTOR whose expression is markedly reduced in aged and surgically induced osteoarthritis cartilage, to modulate autophagy in complex with thioredoxin-interacting protein TXNIP in an mTOR-independent manner. Likewise, cartilage-specific deletion of Atg5, a protein essential for autophagosome formation, led to the development of ageing-associated osteoarthritis but exerted no effect on surgically induced osteoarthritis [17▪]. These studies suggest autophagy and mTOR signaling to potentially modulate osteoarthritis pathology independent of each other (at least in part), rendering further elucidation of the regulatory mechanisms of autophagy necessary for developing therapeutic strategies targeting this process.
GROWTH FACTORS, CARTILAGE ANABOLISM AND SUBCHONDRAL BONE CHANGES
The transforming growth factor-beta (TGF-β) signaling pathway has been identified to play an important role in osteoarthritis development. Despite its anabolic functions in articular cartilage homeostasis through prevention of terminal chondrocyte maturation, TGF-β is also involved in pathological changes in the subchondral bone leading to osteoarthritic cartilage degeneration [18,19]. Modulation of TGF-β signaling as a therapeutic strategy therefore needs to be conducted in an optimized manner to balance the risks and benefits of TGF-β signaling modulation in different joint tissues.
Recent research advances are allowing further clarification into this predicament whereby Xie et al.[20▪▪] showed systemic administration of a TGF-β neutralizing antibody to ACLT-treated mice prevented articular cartilage degeneration, normalized subchondral bone structure, and prevented uncoupled subchondral bone remodeling and angiogenesis. Additionally, articular cartilage-specific deletion of Tgfbr-2 in adult mice subjected to DMM surgery protected from cartilage degeneration [21▪▪], suggesting inhibition of TGF-β signaling to be optimal in mature cartilage in order to avoid the harmful effects of TGF-β signaling ablation during cartilage development and homeostasis.
TGF-α is a member of the epidermal growth factor (EGF) family which binds to epidermal growth factor receptor and has been recently identified to be involved in osteoarthritis pathology, where its expression was found to be upregulated in osteoarthritic chondrocytes in a rat model of ACLT-induced osteoarthritis [22]. In line with previous in-vitro data showing that TGF-α induces catabolic activity in articular chondrocytes, TGF-α null mice experienced protection from DMM-induced osteoarthritis with significantly reduced cartilage damage, MMP13 expression, and type II collagen fragmentation [23▪▪]. However, this protective effect was not mirrored during ageing-associated osteoarthritis or DMM-induced osteoarthritis in older mice, suggesting therapeutic effects of TGF-α signaling to be context-dependent, such as in posttraumatic osteoarthritis of young individuals [23▪▪].
Additionally, another EGFR ligand-heparin-binding EGF (HB-EGF) – has also recently been shown to be increased in the knee joints of DMM operated mice, and elicits similar catabolic activities in cartilage whereas suppressing anabolic activity [24▪▪]. Cartilage-specific deletion of mitogen-inducible gene 6 (MIG6), an inhibitor of the EGFR pathway, resulted in induction of some osteoarthritis-like features in the knee joint including chondrocyte proliferation, osteophyte formation, articular cartilage degradation, and subchondral bone cyst formation [25–27]. However, marked anabolic increase of the articular cartilage thickness was also observed in these mice at an early age, and some models have shown that EGFR suppression exacerbates cartilage destruction, further supporting the context-dependent nature of the EGFR signaling pathway [26–28]. Using rodent models of PTOA, recent studies have suggested C-C motif chemokine ligand 2 (CCL2) and integrin α1β1 to be downstream and upstream mediators of EGFR signaling, respectively, further elucidating this complex pathway for better development of therapeutic targets [29▪,30▪▪].
The fibroblast growth factor (FGF) family consists of 22 pleiotropic growth factors that exert their effect by binding to one of four FGF receptors (FGFRs) [31]. Of the four FGFRs, FGFR1 and FGFR3 are most abundantly expressed in articular cartilage, and FGFR3 activation through FGF2 and FGF18 signaling has been proposed to result in anabolic activities in cartilage [32,33]. This is supported by Tang et al.[34▪▪], whose work examining conditional Fgfr3 deletion in adult chondrocytes showed accelerated DMM-induced osteoarthritis development, with increased proteoglycan loss and chondrocyte hypertrophy. Tang et al.[34▪▪] further showed conditional Fgfr3 activation to cause a chondroprotective effect by delaying osteoarthritis development, suggesting FGFR3 to play an important protective role in osteoarthritis. Development of therapeutic strategies targeting FGFR3 activation, however, requires careful optimization due to the pleiotropic nature of the FGF-signaling pathway. This is seen with intra-articular administration of FGF9 to DMM-induced osteoarthritis in mice. Despite FGF9 being another specific inducer of FGFR3 signaling in chondrocytes, exogenous FGF9 administration aggravated osteophyte formation in addition to attenuating cartilage degradation, cautioning against potential adverse side effects that may arise with FGF signaling modulation [35▪▪].
The Wnt/β-catenin signaling pathway has been shown to play major roles in joint development as well as maintenance of skeletal tissues [36,37]. Balanced Wnt-signaling is essential in cartilage health as both activation and inhibition of β-catenin in cartilage results in cartilage degradation and osteoarthritis [38,39]. Antagonists of Wnt, including frizzled-related protein (FRZB/sFRP3) and dickkopf-related protein 1 (DKK-1), have been shown to possess protective effects against articular cartilage degradation and osteoarthritis [40,41]. However, Wnt-antagonists also play important roles in bone biology, and modulations have been shown to affect subchondral bone changes observed in osteoarthritis pathology [41–43], suggesting further elucidation of Wnt-signaling in different joint tissues to be necessary for optimal targeting of this pathway.
Recent studies are shedding light on novel Wnt-inhibitors that demonstrate potential as therapeutic targets of osteoarthritis. Specifically, hypoxia-inducible factor 1α (HIF1α) has been shown to lower transcription factor 4 (TCF4)/β-catenin transcriptional activity and inhibit MMP13 levels. Intra-articular injection of PKF118–310, an inhibitor of TCF4/β-catenin interaction, resulted in decreased cartilage degradation in surgically induced osteoarthritis of cartilage-specific inducible HIF1α-null mice [44▪▪]. Similarly, intra-articular injections of an inhibitor of histone methyltransferase enhancer of zeste homolog 2 (EZH2), a chromatin modifier that activates Wnt/β-catenin signaling by suppressing sFRP1, also decreased articular cartilage degradation in surgically induced osteoarthritis [45▪▪]. Furthermore, recent preclinical and clinical trials have demonstrated that intra-articular administration of SM04690, a small-molecule inhibitor of the Wnt pathway, prevents cartilage degradation and promotes cartilage health [46▪▪,47▪▪]. This suggests Wnt-inhibitors to possess potential as disease-modifying therapies for osteoarthritis, however further studies examining potential toxicities of these inhibitors as well as their effects on other joint tissues is necessary to optimize its development and use.
INFLAMMATION, OXIDATIVE STRESS, AND DYSLIPIDEMIA
In addition to traditional proinflammatory mediators such as interleukin 1β (IL-1β), tumor necrosis factor-α (TNF-α), and other chemokines, recent studies have implicated damage-associated molecular patterns (DAMPs), or alarmins, in activating osteoarthritis inflammation pathophysiology [48,49]. DAMPs activate various pattern recognition receptors (PRRs) found on osteoarthritis chondrocytes and synovium, such as toll-like receptor 2, 4 (TLR2, TLR4) and receptor for advanced glycation end-products (RAGE), to induce cytokine production that cause further release of DAMPs and perpetuation of inflammatory responses and catabolic activity in the joint [49,50].
TLR signaling has been heavily studied in osteoarthritis pathology, with TLR expression found in various joint tissues including articular chondrocytes, synovium, subchondral bone, and infrapatellar fat pad [51,52]. Therapeutic strategies targeting TLR signaling has largely centered on agonist blockade and inhibition of TLR activation and signaling [52,53]. Proteoglycan 4 (PRG4/lubricin) has recently been identified as a novel regulator of TLR2, 4 and 5, where intra-articular PRG4 injections in a rat model of DMM-induced osteoarthritis showed decreased expression of inflammatory cytokines and NF-κB, as well as decreased pain response [54▪▪]. Furthermore, PRG4 has been shown to bind to both TLR2 and TLR4 in human osteoarthritis synovial fluid to significantly reduce subsequent TLR2 and TLR4 activation, suggesting PRG4 to possess a novel anti-inflammatory role and act as a potential therapeutic target for osteoarthritis [55▪▪].
Reactive oxygen species (ROS) present another type of inflammatory mediators found in osteoarthritis joints, whereby advanced glycation end products (AGEs) can activate RAGE to induce upregulation of inflammatory cytokines [56]. Superoxide dismutase 2 (SOD2) is an enzyme that metabolizes superoxides in the mitochondria and its downregulation has recently been implicated in osteoarthritis pathology [57▪▪]. Specific deletion of Sod2 in chondrocytes resulted in both accelerated cartilage degeneration during ageing and after DMM-induced osteoarthritis, further confirming the detrimental effect of mitochondrial superoxide production in osteoarthritis [57▪▪]. Alternatively, ablation of nuclear factor (erythroid-derived 2)-like 2 (Nrf2), a transcription factor that regulates the expression of antioxidant proteins to defend against oxidative damage, resulted in increased cartilage damage after DMM surgery in mice, suggesting that Nrf2 may possess protective functions in osteoarthritis [58▪▪]. Collectively, these studies highlight the importance of fine-tuning ROS levels in chondrocytes, and suggest regulators of cellular redox states to be potential therapeutic targets in osteoarthritis.
Features of metabolic syndrome, such as obesity and dyslipidemia, have been linked to osteoarthritis pathology in part through proinflammatory conditions and oxidative stress [59]. Alterations in lipid metabolism have been shown to compromise cartilage homeostasis through ectopic lipid accumulation in chondrocytes [59,60]. Indeed, attenuation of intracellular cholesterol accumulation in chondrocytes using pharmacologic cholesterol inhibition showed reduced severity in surgically induced osteoarthritis [61▪▪]. Additionally, cartilage-specific deletion of PPARδ, a nuclear receptor activated upon fatty acid binding to regulate downstream target genes, resulted in a marked chondroprotective effect against DMM-induced osteoarthritis [62▪▪]. This protective effect could be in part due to ablation of PPARδs induction of fatty acid oxidation, which may lead to greater production of ROS that is detrimental to cartilage health [63,64].
PAIN ASSESSMENT AND NERVE GROWTH FACTOR
The studies previously highlighted focus largely on the structural pathology associated with osteoarthritis; however, one of the most frequently cited reasons for osteoarthritis patients to seek medical attention is joint pain [65]. The mechanisms defining the sustained generation of joint pain in osteoarthritis are currently poorly understood. Indeed, radiographically visible signs of osteoarthritis such as joint space narrowing in humans may not be accompanied by symptoms of pain and vice versa [66]. Furthermore, assessment of pain-like behaviors in animal models is made more complicated as the rodents frequently used in osteoarthritis models appear to mask many outward signs of discomfort and disability [66].
Recent work in a rat ACLT/partial meniscectomy model of osteoarthritis has validated that measurements of joint sparing (e.g., asymmetry in hind limb weight bearing) and animal rearing behaviors progress in parallel to histological signs of cartilage degeneration [67▪▪]. Similar assessments have been frequently made in chemical models of osteoarthritis such as those induced by intra-articular monoiodoacetate (MIA) injection; however, the disease progression in these models develops far more rapidly than surgical models [68▪▪]. A recent study examining pain-related behaviors in rats with bilateral intra-articular injection of MIA demonstrated that decreased spontaneous animal burrowing is correlated with spontaneous animal activity and rearing indicative of pain [69▪▪]. These indications of pain were reversible with various analgesics including the controversial novel anti-nerve growth factor (NGF) therapies [69▪▪]. These techniques may also be valuable in assessing osteoarthritis related pain-like behaviors in comparable surgical models.
NGF binds to the tropomyosin receptor kinase A (TrkA) and is important during development for the formation of nociceptive sensory neurons [70▪▪]. NGF and TrkA are expressed by both chondrocytes and fibroblast-like synoviocytes, and appear to have a role in pain sensitization in osteoarthritis [69▪▪–72▪▪]. Recent clinical trials with anti-NGF monoclonal antibodies have produced results supporting the use of these therapies as antinociceptive in osteoarthritis patients; however, a small number of serious adverse events related to osteonecrosis have raised concern over these treatments [73]. Upregulation of NGF mRNA in articular chondrocytes has been shown to follow surgical induction of osteoarthritis by partial meniscectomy in mice, indicating a dynamic role for NGF in pain generation and sensitization following insult to articular cartilage [71▪▪]. Similarly, decreased pain-like behaviors (gait analysis) have been shown following treatment with the anti-NGF antibody tanezumab in a rat meniscal tear model [72▪▪]. Although the tanezumab treated animals in this study appeared to develop worsening cartilage degeneration, unloading of the joint by mid-tibial amputation largely prevented cartilage destruction [72▪▪]. This study may indicate that excessive loading due to loss of protective nociceptive signaling with anti-NGF treatment following surgical osteoarthritis induction may exacerbate disease progression. However, a comprehensive study using both the MIA and meniscal transection mouse osteoarthritis models in concert with oral delivery of a small molecule inhibitor of TrkA demonstrated antinociceptive effects in animal behaviors without increased cartilage damage [70▪▪]. It is important to note that the power of these studies may not be high enough to examine rare adverse events as seen in the human clinical trials [73], although continuing studies are promising for the use of these treatments for addressing pain in osteoarthritis patients.
CONCLUSION
Pathology in surgical animal models of osteoarthritis is similar to the disease progression seen in humans, and gives us great insight into the mechanisms involved. This review focuses on only a few candidate pathways and molecules that have shown recent promise for further understanding of osteoarthritis pathophysiology and development of therapeutics. However, it is clear that the various joint tissues each play a distinct and important role in disease progression, and symptom generation. With this in mind it is important that future studies continue to address the joint as a whole in a physiological context, and for these reasons animal models will continue to be essential in ongoing osteoarthritis research.
Acknowledgements
The authors would like to thank all members of the Beier Lab for ongoing support. M.A.P. was supported by a Canadian Institutes of Health Research (CIHR) Doctoral Research Award, and M.M.-G.S. is supported by a Doctoral Scholarship from The Arthritis Society (Canada). M.A.P. and M.M.-G.S. are both partially supported by the collaborative training programme in musculoskeletal health research at the University of Western Ontario, and F.B. is the Canada Research Chair in Musculoskeletal Research. Work in the Beier laboratory is supported by operating grants from CIHR and The Arthritis Society.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Picavet HSJ. Prevalence of self reported musculoskeletal diseases is high. Ann Rheum Dis 2003; 62:644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ 2003; 81:646–656. [PMC free article] [PubMed] [Google Scholar]
- 3.Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. Lancet 2011; 377:2115–2126. [DOI] [PubMed] [Google Scholar]
- 4.Cutolo M, Berenbaum F, Hochberg M, et al. Commentary on recent therapeutic guidelines for osteoarthritis. Semin Arthritis Rheum 2015; 44:611–617. [DOI] [PubMed] [Google Scholar]
- 5.Chu CR, Williams AA, Coyle CH, Bowers ME. Early diagnosis to enable early treatment of preosteoarthritis. Arthritis Res Ther 2012; 14:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang H, Beier F. Mouse models of osteoarthritis: modelling risk factors and assessing outcomes. Nat Rev Rheumatol 2014; 10:413–421. [DOI] [PubMed] [Google Scholar]
- 7.Chen Y, Klionsky DJ. The regulation of autophagy – unanswered questions. J Cell Sci 2011; 124:161–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider JL, Cuervo AM. Autophagy and human disease: emerging themes. Curr Opin Genet Dev 2014; 26:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caramés B, Taniguchi N, Otsuki S, et al. Autophagy is a protective mechanism in normal cartilage, and its aging-related loss is linked with cell death and osteoarthritis. Arthritis Rheum 2010; 62:791–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sasaki H, Takayama K, Matsushita T, et al. Autophagy modulates osteoarthritis-related gene expression in human chondrocytes. Arthritis Rheum 2012; 64:1920–1928. [DOI] [PubMed] [Google Scholar]
- 11▪▪.Zhang Y, Vasheghani F, Li Y-H, et al. Cartilage-specific deletion of mTOR upregulates autophagy and protects mice from osteoarthritis. Ann Rheum Dis 2015; 74:1432–1440. [DOI] [PubMed] [Google Scholar]; The first in-vivo study examining cartilage-specific deletion of mTOR signaling in surgically induced osteoarthritis, showing lack of mTOR results in increased autophagy to exert protective roles against osteoarthritis.
- 12▪▪.Vasheghani F, Zhang Y, Li Y-H, et al. PPARγ deficiency results in severe, accelerated osteoarthritis associated with aberrant mTOR signalling in the articular cartilage. Ann Rheum Dis 2015; 74:569–578. [DOI] [PMC free article] [PubMed] [Google Scholar]; First in-vivo study showing the involvement of PPARγ in the regulation of mTOR/autophagy and deficiency of PPARg may, in part, upregulate mTOR signaling to suppress autophagy and cause catabolic effects in the articular cartilage.
- 13.Ahmadian M, Suh JM, Hah N, et al. PPARγ signaling and metabolism: the good, the bad and the future. Nat Med 2013; 99:557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caramés B, Hasegawa A, Taniguchi N, et al. Autophagy activation by rapamycin reduces severity of experimental osteoarthritis. Ann Rheum Dis 2012; 71:575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪▪.Ribeiro M, López de Figueroa P, Nogueira-Recalde U, et al. Diabetes-accelerated experimental osteoarthritis is prevented by autophagy activation. Osteoarthritis Cartilage 2016; S1063-4584(16)30170-4. [DOI] [PubMed] [Google Scholar]; This study provides evidence that pharmacological activation of autophagy via rapamycin may be an effective therapeutic strategy against metabolic osteoarthritis, specifically diabetes-associated osteoarthritis.
- 16▪.Alvarez-Garcia O, Olmer M, Akagi R, et al. Suppression of REDD1 in osteoarthritis cartilage, a novel mechanism for dysregulated mTOR signaling and defective autophagy. Osteoarthritis Cartilage 2016; 24:1639–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides evidence that REDD1 is an endogenous regulator of mTOR signaling, however it is also associated with TXNIP to form a protein complex for autophagy induction in chondrocytes.
- 17▪.Bouderlique T, Vuppalapati KK, Newton PT, et al. Targeted deletion of Atg5 in chondrocytes promotes age-related osteoarthritis. Ann Rheum Dis 2016; 75:627–631. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to demonstrated cartilage-specific deletion of Atg5 promotes ageing-associated osteoarthritis but exert no effect on surgically induced osteoarthritis.
- 18.Zhen G, Wen C, Jia X, et al. Inhibition of TGF-β signaling in mesenchymal stem cells of subchondral bone attenuates osteoarthritis. Nat Med 2013; 19:704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen J, Li S, Chen D, et al. TGF-β signaling and the development of osteoarthritis. Bone Res 2014; 2:14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20▪▪.Xie L, Tintani F, Wang X, et al. Systemic neutralization of TGF-β attenuates osteoarthritis. Ann N Y Acad Sci 2016; 1376:53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that systemic neutralization of TGF-β signaling with 1D11 decreased osteoarthritis progression by preventing subchondral bone changes essential to early osteoarthritis in ACLT-induced osteoarthritis.
- 21▪▪.Chen R, Mian M, Fu M, et al. Attenuation of the progression of articular cartilage degeneration by inhibition of TGF-β1 signaling in a mouse model of osteoarthritis. Am J Pathol 2015; 185:2875–2885. [DOI] [PMC free article] [PubMed] [Google Scholar]; This was the first in-vivo study demonstrating cartilage-specific inhibition of TGF-β1 signaling to exert protection against cartilage degeneration in a context-specific manner, where it was only observed in adult mice after DMM surgery.
- 22.Appleton CTG, Pitelka V, Henry J, Beier F. Global analyses of gene expression in early experimental osteoarthritis. Arthritis Rheum 2007; 56:1854–1868. [DOI] [PubMed] [Google Scholar]
- 23▪▪.Usmani SE, Ulici V, Pest MA, et al. Context-specific protection of TGFα null mice from osteoarthritis. Sci Rep 2016; 6:30434. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to examine Tgfα-null mice in the context of DMM-induced osteoarthritis, demonstrating that young Tgfα-null mice, but not older mice, are protected from osteoarthritis progression.
- 24▪▪.Long DL, Ulici V, Chubinskaya S, Loeser RF. Heparin-binding epidermal growth factor-like growth factor (HB-EGF) is increased in osteoarthritis and regulates chondrocyte catabolic and anabolic activities. Osteoarthritis Cartilage 2015; 23:1523–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that HB-EGF is increased in the knee joints of DMM operated mice, and elicits catabolic activities in cartilage while suppressing anabolic activity.
- 25.Xu D, Makkinje A, Kyriakis JM. Gene 33 is an endogenous inhibitor of epidermal growth factor (EGF) receptor signaling and mediates dexamethasone-induced suppression of EGF function. J Biol Chem 2005; 280:2924–2933. [DOI] [PubMed] [Google Scholar]
- 26.Staal B, Williams BO, Beier F, et al. Cartilage-specific deletion of Mig-6 results in osteoarthritis-like disorder with excessive articular chondrocyte proliferation. Proc Natl Acad Sci 2014; 111:2590–2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pest MA, Russell BA, Zhang Y-W, et al. Disturbed cartilage and joint homeostasis resulting from a loss of mitogen-inducible Gene 6 in a mouse model of joint dysfunction. Arthritis Rheumatol 2014; 66:2816–2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Zhu J, Liu F, et al. Reduced EGFR signaling enhances cartilage destruction in a mouse osteoarthritis model. Bone Res 2014; 2:14015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪.Shin SY, Pozzi A, Boyd SK, Clark AL. Integrin α1β1 protects against signs of posttraumatic osteoarthritis in the female murine knee partially via regulation of epidermal growth factor receptor signalling. Osteoarthritis Cartilage 2016; 24:1795–1806. [DOI] [PubMed] [Google Scholar]; This study demonstrates that integrin α1β1 protects against DMM-induced osteoarthritis in part by decreasing EGFR signaling, providing evidence that integrin α1β1 mediates EGFR signaling to exert protection against osteoarthritis.
- 30▪▪.Appleton CTG, Usmani SE, Pest MA, et al. Reduction in disease progression by inhibition of transforming growth factor α-CCL2 signaling in experimental posttraumatic osteoarthritis. Arthritis Rheumatol 2015; 67:2691–2701. [DOI] [PubMed] [Google Scholar]; This study provided evidence that TGF-α signling may stimulate cartilage degradation in osteoarthritis through CCL2-dependent mechanisms.
- 31.Ornitz DM, Itoh N. The fibroblast growth factor signaling pathway. Wiley Interdiscip Rev Dev Biol 2015; 4:215–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yan D, Chen D, Cool SM, et al. Fibroblast growth factor receptor 1 is principally responsible for fibroblast growth factor 2-induced catabolic activities in human articular chondrocytes. Arthritis Res Ther 2011; 13:R130. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 33.Davidson D, Blanc A, Filion D, et al. Fibroblast growth factor (FGF) 18 signals through FGF receptor 3 to promote chondrogenesis. J Biol Chem 2005; 280:20509–20515. [DOI] [PubMed] [Google Scholar]
- 34▪▪.Tang J, Su N, Zhou S, et al. Fibroblast growth factor receptor 3 inhibits osteoarthritis progression in knee joints of adult mice. Arthritis Rheumatol 2016; doi: 10.1002/art.39739. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; The first study to elucidate the role of FGFR3 in surgically induced osteoarthritis, demonstrating that FGFR3 delays osteoarthritis progression in knee-joints.
- 35▪▪.Zhou S, Wang Z, Tang J, et al. Exogenous fibroblast growth factor 9 attenuates cartilage degradation and aggravates osteophyte formation in posttraumatic osteoarthritis. Osteoarthritis Cartilage 2016; S1063-4584(16)30185-6. [DOI] [PubMed] [Google Scholar]; This study examined administration of FGF9 and the effects of its activation of FGFR3 signaling on osteoarthritis pathology, demonstrating that while it attenuates cartilage degradation it aggrevates osteophyte formation.
- 36.Usami Y, Gunawardena AT, Iwamoto M, Enomoto-Iwamoto M. Wnt signaling in cartilage development and diseases: lessons from animal studies. Lab Investig 2016; 96:186–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luyten FP, Tylzanowski P, Lories RJ. Wnt signaling and osteoarthritis. Bone 2009; 44:522–527. [DOI] [PubMed] [Google Scholar]
- 38.Zhu M, Chen M, Zuscik M, et al. Inhibition of β-catenin signaling in articular chondrocytes results in articular cartilage destruction. Arthritis Rheum 2008; 58:2053–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu M, Tang D, Wu Q, et al. Activation of β-catenin signaling in articular chondrocytes leads to osteoarthritis-like phenotype in adult β-catenin conditional activation mice. J Bone Miner Res 2009; 24:12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lories RJU, Peeters J, Bakker A, et al. Articular cartilage and biomechanical properties of the long bones in Frzb -knockout mice. Arthritis Rheum 2007; 56:4095–4103. [DOI] [PubMed] [Google Scholar]
- 41.Oh H, Chun C-H, Chun J-S. Dkk-1 expression in chondrocytes inhibits experimental osteoarthritic cartilage destruction in mice. Arthritis Rheum 2012; 64:2568–2578. [DOI] [PubMed] [Google Scholar]
- 42.Funck-Brentano T, Bouaziz W, Marty C, et al. Dkk-1-mediated inhibition of Wnt signaling in bone ameliorates osteoarthritis in mice. Arthritis Rheumatol 2014; 66:3028–3039. [DOI] [PubMed] [Google Scholar]
- 43.Thysen S, Luyten FP, Lories RJ. Loss of Frzb and Sfrp1 differentially affects joint homeostasis in instability-induced osteoarthritis. Osteoarthritis Cartilage 2015; 23:275–279. [DOI] [PubMed] [Google Scholar]
- 44▪▪.Bouaziz W, Sigaux J, Modrowski D, et al. Interaction of HIF1α and β-catenin inhibits matrix metalloproteinase 13 expression and prevents cartilage damage in mice. Proc Natl Acad Sci 2016; 113:5453–5458. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to elucidate the interaction between HIF1α and β-catenin, showing that HIF1α lowers TCF4-β-catenin activity, negatively regulating Wnt-signaling and MMP13 expression to reduce catabolic effects in osteoarthritis.
- 45▪▪.Chen L, Wu Y, Wu Y, et al. The inhibition of EZH2 ameliorates osteoarthritis development through the Wnt/β-catenin pathway. Sci Rep 2016; 6:29176. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to examine the role of EZH2 in osteoarthritis pathology, providing evidence that it activates β-catenin signaling by suppressing sFRP1. Pharmacological inhibition of EZH2 delayed osteoarthritis development in surgically induced osteoarthritis, suggesting it may be an effective therapeutic target for osteoarthritis.
- 46▪▪.Hood JD, Deshmukh V, Barroga C, Hu Y. Discovery of a small molecule inhibitor of the Wnt pathway (SM04690) as a potential disease modifying treatment for knee osteoarthritis. Osteoarthritis Cartilage 2016; 24:S14–S15. [DOI] [PubMed] [Google Scholar]; This study was the first to use SM04690 in a series of preclinical studies using instability-induced osteoarthritis models in rats and dogs, demonstrating that SM04690 inhibits the Wnt pathway to improve overall cartilage health.
- 47▪▪.Yazici Y, Majumdar S, McAlindon TE, et al. Magnetic resonance imaging outcomes using an intra-articular injection (SM04690) in the treatment of osteoarthritis of the knee: interim, exploratory analysis of results from a randomized, double-blind, placebo-controlled, Phase 1 Study [abstract]. Arthritis Rheumatol 2015; 67 (suppl 10): [Google Scholar]; This phase 1 clinical trials study examined the effects of intra-articular injection of SM04690 in the treatment of osteoarthritis in human patients, demonstrating with MRI outcomes that SM04690 may maintain cartilage thickness and therefore possess potential as a new disease-modifying therapy of osteoarthritis.
- 48.Goldring MB, Otero M. Inflammation in osteoarthritis. Curr Opin Rheumatol 2011; 23:471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu-Bryan R, Terkeltaub R. Emerging regulators of the inflammatory process in osteoarthritis. Nat Rev Rheumatol 2014; 11:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu-Bryan R. Synovium and the innate inflammatory network in osteoarthritis progression. Curr Rheumatol Rep 2013; 15:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mullen LM, Chamberlain G, Sacre S. Pattern recognition receptors as potential therapeutic targets in inflammatory rheumatic disease. Arthritis Res Ther 2015; 17:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gómez R, Villalvilla A, Largo R, et al. TLR4 signalling in osteoarthritis—finding targets for candidate DMOADs. Nat Rev Rheumatol 2014; 11:159–170. [DOI] [PubMed] [Google Scholar]
- 53.Hennessy EJ, Parker AE, O’Neill LAJ. Targeting Toll-like receptors: emerging therapeutics? Nat Rev Drug Discov 2010; 9:293–307. [DOI] [PubMed] [Google Scholar]
- 54▪▪.Iqbal SM, Leonard C, Regmi C, et al. Lubricin/Proteoglycan 4 binds to and regulates the activity of Toll-like receptors in vitro. Sci Rep 2016; 6:18910. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that administration of PRG4 binds to and regulates TLR-signaling in vitro, as well as inhibit systemic inflammation and reduction in pain in a rat osteoarthritis model.
- 55▪▪.Alquraini A, Garguilo S, D'Souza G, et al. The interaction of lubricin/proteoglycan 4 (PRG4) with toll-like receptors 2 and 4: an anti-inflammatory role of PRG4 in synovial fluid. Arthritis Res Ther 2015; 17:353. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to provide evidence that PRG4 binds to TLR2 and TLR4 to mediate an anti-inflammatory role in human synovial fluid.
- 56.Rasheed Z, Akhtar N, Haqqi TM. Advanced glycation end products induce the expression of interleukin-6 and interleukin-8 by receptor for advanced glycation end product-mediated activation of mitogen-activated protein kinases and nuclear factor-κB in human osteoarthritis chondrocytes. Rheumatology (Oxford) 2011; 50:838–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57▪▪.Koike M, Nojiri H, Ozawa Y, et al. Mechanical overloading causes mitochondrial superoxide and SOD2 imbalance in chondrocytes resulting in cartilage degeneration. Sci Rep 2015; 5:11722. [DOI] [PMC free article] [PubMed] [Google Scholar]; Through Sod2 deficiency in chondrocytes, this study demonstrated that the loss of Sod2 and the subsequent ROS imbalance accelerates cartilage denegeration.
- 58▪▪.Cai D, Yin S, Yang J, et al. Histone deacetylase inhibition activates Nrf2 and protects against osteoarthritis. Arthritis Res Ther 2015; 17:269. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study was the first to demonstrate that Nfr2 deficiency in mice results in increased cartilage degradation in DMM-induced osteoarthritis.
- 59.Zhuo Q, Yang W, Chen J, Wang Y. Metabolic syndrome meets osteoarthritis. Nat Rev Rheumatol 2012; 8:729–737. [DOI] [PubMed] [Google Scholar]
- 60.Masuko K, Murata M, Suematsu N, et al. A metabolic aspect of osteoarthritis: lipid as a possible contributor to the pathogenesis of cartilage degradation. Clin Exp Rheumatol 2009; 27:347–353. [PubMed] [Google Scholar]
- 61▪▪.Ali SA, Al-Jazrawe M, Ma H, et al. Regulation of cholesterol homeostasis by hedgehog signaling in osteoarthritic cartilage. Arthritis Rheumatol 2016; 68:127–137. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that pharmacological blockade of cholesterol reduces the severity of DMM-induced osteoarthritis, in part through mediation of cholesterol homeostasis by hedgehod signaling in cartilage.
- 62▪▪.Ratneswaran A, LeBlanc EA, Walser E, et al. Peroxisome proliferator-activated receptor δ promotes the progression of posttraumatic osteoarthritis in a mouse model. Arthritis Rheumatol 2015; 67:454–464. [DOI] [PubMed] [Google Scholar]; This was the first study to determine the catabolic role of PPARδ in DMM-induced osteoarthritis, identifying inhibition of PPARδ to be a promising therapeutic target of osteoarthritis.
- 63.Kleiner S, Nguyen-Tran V, Bare O, et al. PPARα agonism activates fatty acid oxidation via PGC-1α but does not increase mitochondrial gene expression and function. J Biol Chem 2009; 284:18624–18633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yudoh K, van Trieu N, Nakamura H, et al. Potential involvement of oxidative stress in cartilage senescence and development of osteoarthritis: oxidative stress induces chondrocyte telomere instability and downregulation of chondrocyte function. Arthritis Res Ther 2005; 7:R380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peat G. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary healthcare. Ann Rheum Dis 2001; 60:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Malfait AM, Little CB, McDougall JJ. A commentary on modelling osteoarthritis pain in small animals. Osteoarthritis Cartilage 2013; 21:1316–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67▪▪.Hamilton CB, Pest MA, Pitelka V, et al. Weight-bearing asymmetry and vertical activity differences in a rat model of posttraumatic knee osteoarthritis. Osteoarthritis Cartilage 2015; 23:1178–1185. [DOI] [PubMed] [Google Scholar]; This study validated that measurement of joint sparing and animal rearing behaviors progress in parallel to histological signs of cartilage degeneration in a rat surgical model of osteoarthritis.
- 68▪▪.Nwosu LN, Mapp PI, Chapman V, Walsh DA. Relationship between structural pathology and pain behaviour in a model of osteoarthritis (OA). Osteoarthritis Cartilage 2016; S1063-4584(16)30144-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that varying MIA doses generate discrete osteoarthritis pain phenotypes, however the disease progression in MIA-induced osteoarthritis models develops far more rapidly than surgical models.
- 69▪▪.Bryden LA, Nicholson JR, Doods H, Pekcec A. Deficits in spontaneous burrowing behavior in the rat bilateral monosodium iodoacetate model of osteoarthritis: an objective measure of pain-related behavior and analgesic efficacy. Osteoarthritis Cartilage 2015; 23:1605–1612. [DOI] [PubMed] [Google Scholar]; This study examined pain-related behaviors in rats with bilateral intra-articular injection of MIA and showed that decreased spontaneous animal burrowing is correlated with spontaneous animal activity and rearing indicative of pain.
- 70▪▪.Nwosu LN, Mapp PI, Chapman V, Walsh DA. Blocking the tropomyosin receptor kinase A (TrkA) receptor inhibits pain behaviour in two rat models of osteoarthritis. Ann Rheum Dis 2016; 75:1246–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed that blocking NGF signaling via TrkA inhibition have a role in pain sensitization in both MIA-induced and meniscal transection-induced osteoarthritis.
- 71▪▪.Driscoll C, Chanalaris A, Knights C, et al. Nociceptive sensitizers are regulated in damaged joint tissues, including articular cartilage, when osteoarthritic mice display pain behavior. Arthritis Rheumatol 2016; 68:857–867. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study identified that pain-sensitizing molecules, in addition to NGF, are regulated in damaged joint tissues when mice subjected to DMM-induced osteoarthritis develop osteoarthritis-related pain behavior.
- 72▪▪.LaBranche TP, Bendele AM, Omura BC, et al. Nerve growth factor inhibition with tanezumab influences weight-bearing and subsequent cartilage damage in the rat medial meniscal tear model. Ann Rheum Dis 2016; doi: 10.1136/annrheumdis-2015-208913. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated decreased pain-like behaviors in rats treated with the anti-NGF antibody tanezumab following medial meniscal tear-induced osteoarthritis, causing increased voluntary weight bearing and subsequent cartilage damage.
- 73.Hochberg MC. Serious joint-related adverse events in randomized controlled trials of antinerve growth factor monoclonal antibodies. Osteoarthritis Cartilage 2015; 23:S18–S21. [DOI] [PubMed] [Google Scholar]


