Abstract
Background:
Seroma and hematoma formations are the most common complications after plastic surgery. The aim of this study was to assess the efficacy of autologous platelet-rich plasma (A-PRP) glue to reduce postoperative wound complications and improve surgical outcomes.
Methods:
Fifty-four patients were included in this study. They underwent breast reduction surgery, abdominoplasty, or limb lifting with A-PRP glue application on the entire surface of the subcutaneous tissue at the time of suture. Retrospective data were used for the control group. The primary endpoint was the incidence of postoperative seroma or hematoma. The secondary endpoint was the Patient and Observer Scar Assessment Scale score.
Results:
Demographics and clinical characteristics were not statistically different between the A-PRP glue group and the control group regarding age, sex ratio, and body mass index. After abdominoplasty, 37.5% of patients (3/8) in the control group experienced seroma and hematoma complications versus 12.5% of patients (2/16) in the A-PRP glue group (P = 0.55 and P = 0.25, respectively). After limb lifting, 50% of patients experienced postoperative complications in the control group versus no patient in the A-PRP glue group (P = 0.03*; * indicates that the P value is significant). After breast reduction, no patient experienced complication in the A-PRP glue group versus 25% of patients in the control group who experienced hematoma (P = 0.04*). The scar quality assessed 12 months after surgery showed no statistical differences between the groups.
Conclusions:
A-PRP glue seems effective to prevent seroma formation after limb lifting and hematoma formation after breast reduction. Wound-healing quality did not seem to be improved.
Weight loss sequelae surgery and breast reduction are common plastic surgery procedures. The incidence of obesity has recently increased worldwide. After bariatric surgery in obese patients, a massive weight loss usually leads to cutaneous deformities impairing their quality of life. Therefore, patients often require a body-contouring procedure such as abdominoplasty, thigh lift, brachioplasty, and body lift.1 The demand for weight loss sequelae surgery has markedly increased in recent years. Unfortunately, these procedures are usually associated with postoperative complications (seroma and hematoma), which may occur in 10% to 30% of cases2 with an increase in infection leading to delayed recovery times and impaired wound healing. In the field of breast reduction surgery, studies have demonstrated that the use of drains increases the incidence of seroma formation.3–5
Different methods may be used to reduce postoperative complications and the need for drains, including using complete haemostatic, quilting sutures, heterologous glue, compressive dressing, and tissue sealants.
Different types of surgical adhesive have emerged as alternative fixation methods for tissue adhesion. Among these, biological sealants (or fibrin sealants) are produced using a pool of known donors combined with bovine thrombin, whereas platelet-rich plasma (PRP) glue is an autologous preparation from the patient’s own blood, playing the role of growth factor reservoir during treatment.
Studies investigating the use of PRP in plastic surgery applications have shown faster restoration of damaged tissues and also a decrease in inflammation and pain.6 Therefore, the significant enrichment in locally acting growth factors plays an essential role in cell differentiation and tissue regeneration.7
Depending on the clinical indication, PRP may be either injected in liquid form or applied as a gel (referred to as platelet gel or PRP glue). When injected as a gel, the PRP must be mixed with a gelation inducer just before application on the site to be treated. Gelation may be achieved by different ways such as exogenous thrombin, calcium chloride, calcium gluconate, and autologous thrombin. Various studies have reported the positive effects of applying PRP glue in many different clinical fields, especially in orthopedic surgery and oral and maxillofacial surgery.8 To date, only a few studies on the use of autologous platelet gel as an adhesive have been published in the field of plastic surgery. Existing data in various plastic surgery indications, including rhytidectomy,9–11 abdominoplasty,11–13 and breast reduction,10,11 have shown encouraging results with a reduction in postoperative complications (ie, seroma and hematoma) after the use of autologous PRP (A-PRP) glue.
The aim of this prospective study was to assess the value of A-PRP glue in weight loss sequelae surgery and breast reduction surgery. The main outcomes were the incidence of postoperative collections and wound-healing quality.
MATERIALS AND METHODS
Study Design and Patients
This prospective study was conducted in 51 patients who underwent breast reduction surgery, abdominoplasty, thigh lift (vertical and horizontal), or brachioplasty with application of A-PRP glue on the entire surface of the subcutaneous tissue at the time of suture. A control group was used, corresponding to patients whose retrospective data were already available in our department; they were all operated on by the same surgeons using the same techniques without PRP glue application.
Eligible participants were older than 18 years, scheduled to undergo a postbariatric surgery (mammoplasty, abdominoplasty, thigh lift, and brachioplasty). Potential participants were excluded based on the following criteria: age <18 years, patients with history of allergy to one of the components of the study product, patients with hematological diseases, anemia (hemoglobin, <10 g/dL), malignant disease, and patients treated with chemotherapy.
The study was approved by a French ethics committee (CPP Ile de France Paris IV), and the clinical trial authorization was obtained from the French National Agency for Medicines and Health Products Safety (study number: 2014-A00164-43).
Surgical Techniques
All the surgical procedures were performed using the same technique under general anesthesia as described by Le Louarn et al.14,15
Abdominoplasty with Umbilical Transposition
Detachment was performed above the fascia superficialis, rigorous hemostasis, 2 umbilicus quilting sutures, and 3 lateral suture points on either side. Application of A-PRP glue was performed in the undermined subcutaneous space (Fig. 1), followed by placement of blade drains, closure in 2 layers, and application of a compressive dressing.
Fig. 1.
Autologous platelet-rich plasma with autologous thrombin (syringe) before spraying.
Brachioplasty and Thigh Lift
Liposuction was performed in the resection cutaneous zone to preserve lymphatic vessels, rigorous hemostasis, cutaneous resection, and application of A-PRP glue under the suture in 2 layers. No drainage was performed.
Breast Reduction
Glandular cutaneous resection was performed according to the Wise pattern breast reduction technique. The flap with nipple was an internal posterosuperior pedicle. The PRP glue was sprayed at the subcutaneous tissue and applied under the suture (Fig. 2). The suture was made in 2 plans. No drainage was performed. A semimodeling dressing was used.
Fig. 2.
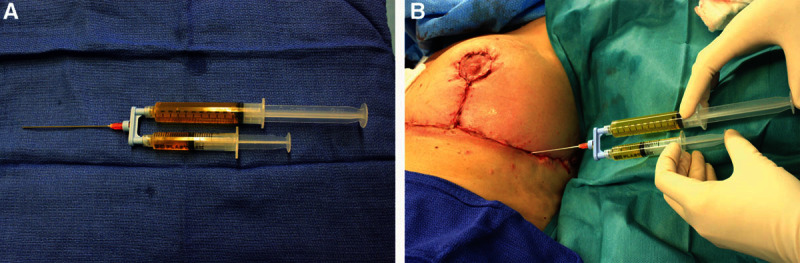
Application of platelet-rich plasma glue using RegenKit applicator (A) on the entire surface of the subcutaneous tissue before suturing the flap (B).
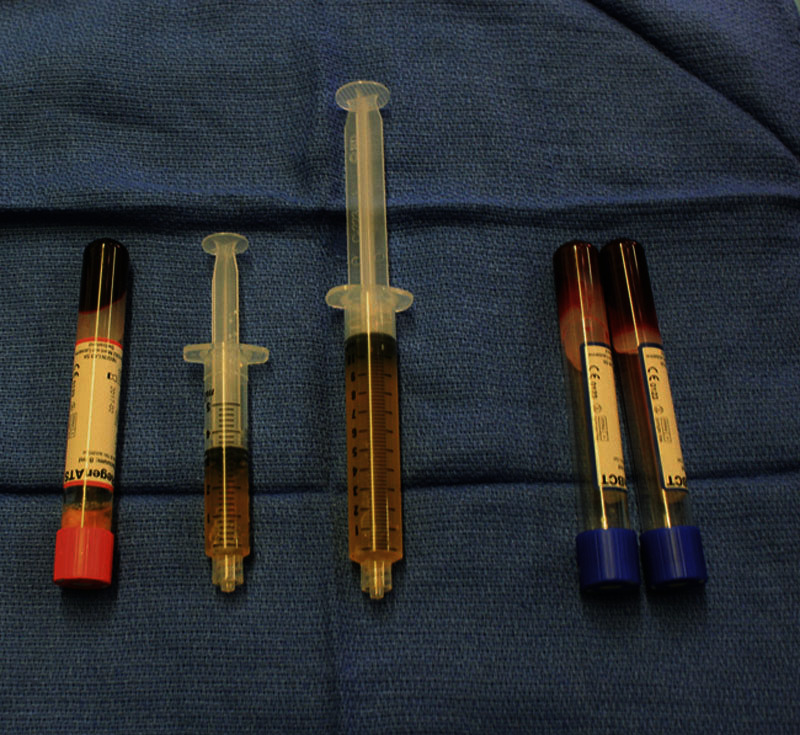
Preparation of A-PRP Glue
The peripheral blood was collected in 3 tubes of RegenKit-Surgery (RegenLab, Le Mont-sur-Lausanne, Switzerland) allowing preparation of 10 mL of A-PRP glue. Between 24 and 48 mL of blood was drawn from each donor depending on the indication: 1 RegenKit-Surgery for abdominoplasty and mammoplasty, 2 kits for type II thigh lift, and 1 kit for brachioplasty. The RegenKit-Surgery consisted of 2 RegenKit-blood cell therapy tubes for PRP preparation and 1 Regen autologous thrombin serum tube to isolate autologous thrombin. The PRP was collected after centrifugation at 1,500g for 5 minutes. From 8 mL of blood, the Regen-blood count therapy tube allowed preparation of 4 to 5 mL of A-PRP with a platelet recovery greater than 80% and a concentration factor of 1.6 (the platelet concentration was about 350–400 billion platelets per millimeter, data on file). A second centrifugation at 1,500g for 5 minutes was performed only for the Regen autologous thrombin serum tube for autologous thrombin serum extraction. The PRP was then mixed and activated with autologous thrombin using the Regen spray applicator with a 9:3 ratio (PRP:thrombin) to form PRP glue (Fig. 1).
Patient Follow-up
Five follow-up visits were scheduled at days 1, 7, 15, and 30 and the final visit at 12 months. The primary endpoint was the formation of postoperative seroma collection or hematoma. The secondary endpoint was the Patient and Observer Scar Assessment Scale (POSAS) score, which was the sum of the scores obtained using 2 scales: the Patient Scar Assessment Scale and the Observer Scar Assessment Scale. Both scales contained 6 items that were scored numerically on a 10-point scale. The Patient Scar Assessment Scale items were pain, itching, color, stiffness, average thickness of the scar edge, and surface irregularities. The Observer Scar Assessment Scale items were vascularity, pigmentation, average thickness of the edge, relief, pliability, and surface area of the scar. Moreover, both scales also included an assessment of patient and observer “overall opinion.”16
Statistical Analysis
Continuous variables following a normal distribution are presented as mean ± SD and were compared using a Student’s t test. Categorical variables are presented as counts and percentages and were compared using the Fisher’s exact test. Results are reported as mean ± SEM in detailed analyses. All P values were 2-sided and a value of P value less than 0.05 was considered significant. Normal distribution of the variables was evaluated for continuous variables using the Kolmogorov–Smirnov test. All analyses were performed with PRISM, version 5 (GraphPad). All the authors had full access to and take full responsibility for the integrity of the data.
RESULTS
PRP Glue in Weight Loss Sequelae Surgery
A total of 26 patients underwent weight loss sequelae surgery with application of PRP glue, including abdominoplasty (n = 16) and limb lifting (n = 10). For the retrospective control group, the data of patients who underwent abdominoplasty (n = 8) and limb lifting (n = 8) were used. The mean age (±SD) of patients was 40.2 ± 7.1 years in the control group and 38.48 ± 9.69 years in the PRP glue group (P = 523). The mean body mass index (BMI) was 26.7 ± 3.43 kg/m2 in the PRP glue group and 25.4 ± 3.86 kg/m2 in the control group (P = 0.262). When comparing demographics and clinical characteristics between the 2 groups of patients, no statistical differences were observed regarding age, sex ratio, and BMI (Table 1).
Table 1.
Demographics of Patients with Weight Loss Sequelae Surgery
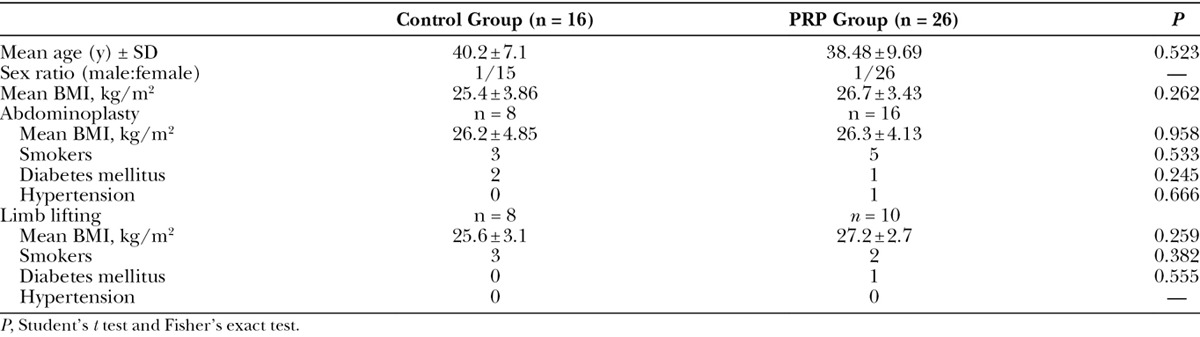
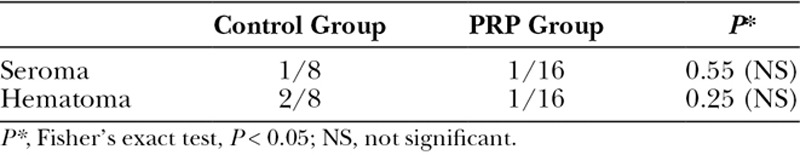
After abdominoplasty, 37.5% of patients (3/8) in the control group experienced seroma and hematoma complications versus 12.5% of patients (2/16) in the PRP glue group. The Fisher’s exact test was used to measure differences in the number of seroma and hematoma complications between both groups, and no statistical difference was observed (P = 0.55 and P = 0.25, respectively) (Table 2).
Table 2.
Patient’s Postoperative Complications after Abdominoplasty at 1 Month
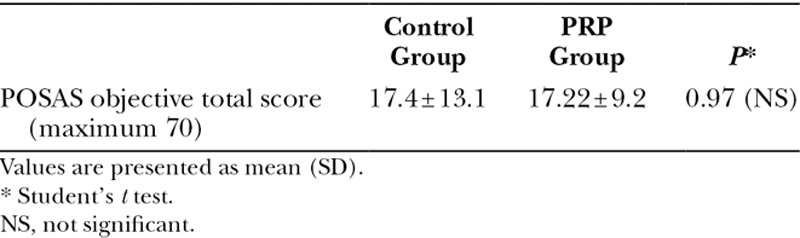
To assess scar quality in the 2 groups, the POSAS score was used 12 months after abdominoplasty. The analysis of the POSAS score showed no statistical difference between both groups (P = 0.97) (Table 3).
Table 3.
Abdominoplasty Scar POSAS Scores at 12 Months
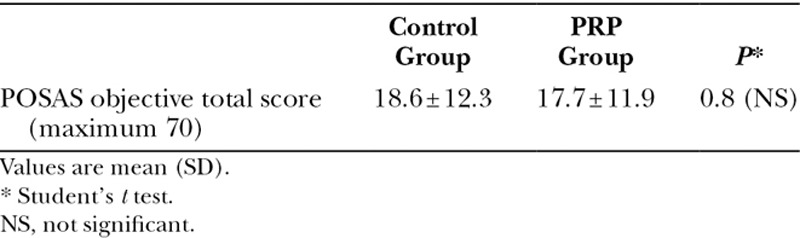
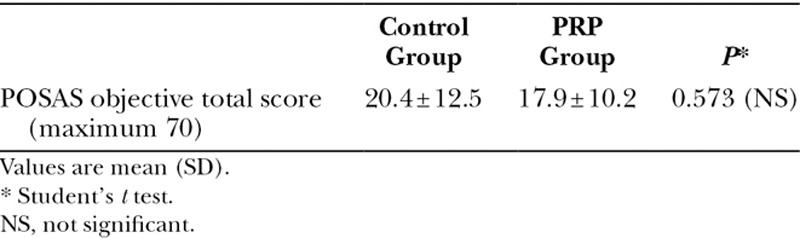
For patients who underwent limb lifting, the clinical examination of postoperative complications showed 4 cases at 1 month corresponding to 50% of total patients (3 patients with seroma and 1 patient with hematoma) in the control group, whereas no patient experienced any complication in the PRP glue group (P = 0.03*) (Table 4). The POSAS scores showed no statistical difference between the control group and the PRP glue group (P = 0.8) (Table 5).
Table 4.
Patient’s Postoperative Complications after Limb Lifting at 1 Month
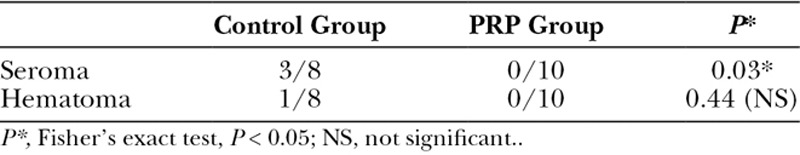
Table 5.
Limb Lifting Scar POSAS Scores at 12 Months
PRP Glue in Breast Reduction Surgery
Clinical and demographic characteristics in the control group and PRP glue group after breast reduction were similar in terms of age and BMI. The mean weight of tissue resection was 375 ± 234 g in the control group and 403 ± 145 g in the PRP glue group (P = 0.757) (Table 6). In the PRP glue group, no complication was reported compared with the control group where 2 patients (25%) reported the occurrence of hematoma (P = 0.04*) (Table 7). No seroma complication was reported in the 2 groups.
Table 6.
Demographics of Patients with Breast Reduction Surgery
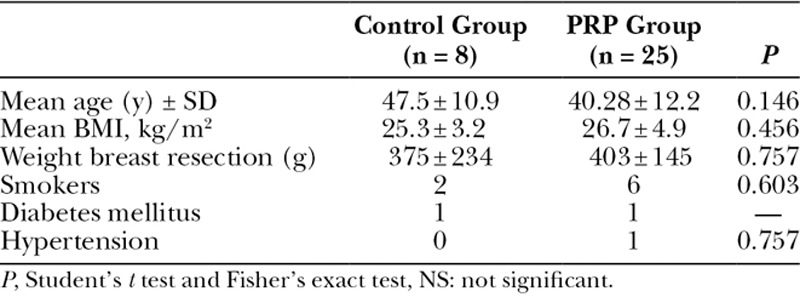
Table 7.
Patient’s Postoperative Complications after Breast Reduction at 1 Month
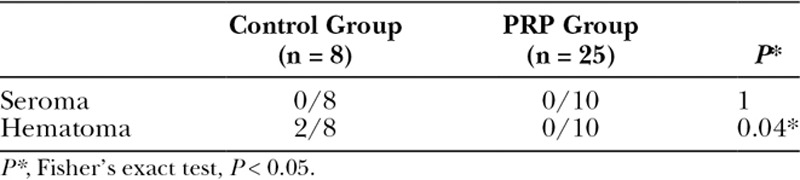
The scar quality assessed 12 months after breast reduction showed no statistical differences between the groups (Table 8).
Table 8.
Breast Reduction Scar POSAS Scores at 12 Months
DISCUSSION
Seroma and hematoma formations are the most common complications occurring during plastic surgery, especially in breast reduction and postbariatric surgery. These complications may delay wound healing and require multiple aspirations and, in some cases, reoperation. In our study, using PRP glue decreased the incidence of seroma formation after limb lifting and prevented the occurrence of hematoma after breast reduction surgery.
Recently, different methods have been developed for the prevention of postoperative complications, including the use of fibrin sealant sprayed into the surgical areas to seal the subcutaneous space. These biological adhesives have the advantage of reproducing wound-healing mechanisms by mimicking the final stage of the coagulation cascade. However, biological glues are associated with some disadvantages, including their high cost, the possibility of allergic reaction due to the bovine origin of thrombin, and viral contamination and transmission (hepatitis, HIV). To overcome these disadvantages, the use of A-PRP activated with isolated autologous thrombin may offer a new surgical alternative with adhesive and hemostatic proprieties at low cost.
Previous studies on the efficacy of PRP glue as a tissue sealant in plastic surgery indications have shown controversial results. Various studies have reported positive effects of the use of autologous platelet-rich fibrin glue in plastic surgery applications. In a study, 12 patients undergoing abdominoplasty with A-PRP glue showed a reduced time of suction drain and a decreased incidence of seroma formation.12 In addition, Powell et al9 have shown a benefit from using platelet gels applied unilaterally to the undersurface of the superficial muscular aponeurotic system in patients who underwent rhytidectomy, with a decrease in ecchymosis and edema in the treated side of the face compared with the untreated side. Man et al10 have also demonstrated that the use of autologous fibrin glue, followed by the application of platelet gel in cosmetic procedures with flap creation, such as face lifts, reduction mammoplasty, and abdominoplasty resulted in many advantages, including shorter operating times, suppression of the need for drains, reduction in the need for compressive dressings, reduction in pain and postoperative swelling, and improved wound healing with an associated shorter recovery time. However, the blinded, randomized, and controlled trial by Anzarut et al17 has shown that the use of A-PRP gel did not improve outcomes after reduction mammoplasty.
In our study, using autologous platelet gel did not improve outcomes after abdominoplasty. The A-PRP glue sprayed on the entire surface of the subcutaneous tissue did not reduce hematoma or seroma formation or improve scar quality as assessed with the POSAS. We can make several assumptions to explain this finding. Multiple risk factors increasing the incidence of postoperative complications have been proposed, including smoking18 and obesity.19 Our demographic characteristics showed no statistical differences between both groups regarding these risk factors. Furthermore, Grieco et al20 have recently reported that in 25 patients who underwent abdominoplasty, 36% experienced seroma formation and 12% hematoma. These patients had a mean BMI of 31 kg/m2, which could explain the increased incidence of complications.
The main postoperative complication after limb lifting is seroma formation. In a prospective study by Gusenoff et al21, the seroma complication predominated, experienced by 70% of patients in a cohort of 101 subjects who underwent brachioplasty. In our study, the incidence of postoperative seroma after limb lifting (arm lift and thigh lift) was statistically different between the PRP glue group and the control group, showing the interest of the use of PRP glue in this indication. Moreover, after liposuction, the incidence of seroma complication was increased, confirming that the use of PRP glue in this indication is recommended to reduce and optimize outcomes.
In breast reduction indications, the PRP glue decreased significantly the incidence of hematoma formation compared with the control group. Hematoma is due to a sustained capillary bed bleeding from a large raw surface under the skin flap. This complication is usually associated with a risk of skin necrosis and wound infection. Various studies support the use of PRP as an adjunct to hemostasis.22 The interest of PRP glue application is to accelerate the healing cascade via the action of growth factors released in the application site and thus to reduce the risk of hematoma.23,24
Regarding the outcome of seroma, no statistical differences were observed between both groups. This finding is in accordance with the results of Anzarut et al17 showing no statistical differences in terms of drainage and seroma formation between breasts treated with PRP gel and contralateral breasts not treated with PRP gel.
This study has some limitations. First, the scar quality was assessed 12 months after surgical procedures, whereas wound healing was still ongoing. We assumed that spraying the PRP glue in the wound closure could improve scar quality. Moreover, the scar has been assessed using a subjective tool, the POSAS scale. There are more efficient yet expensive and time consuming tools for wound healing available, such as Vivascope (MAVIG GmbH, Munich), which allows in vivo noninvasive visualization and quantitative assessment of the various skin components (epidermis and dermis). Second, we used a retrospective control group to assess the efficacy of the adjunct of PRP glue as a sealant tissue. Thus, to compare our data, we used a prospective series without randomization so that our statistical analysis on weight loss sequelae and breast reduction showed no statistical differences between the PRP glue group and the control group in scar quality assessed. Another limitation of this study is the small number of patients included. A controlled randomized study in a larger series of patients with a longer follow-up would be needed to better demonstrate the effect of A-PRP glue.
The cost of autologous and heterologous glues warrants discussion of this study. Indeed, the cost of the A-PRP glue obtained with the RegenKit-Surgery is significantly lower than that of industrial glue: €200 for 10 mL of A-PRP glue (or €20/1 mL of glue) compared with €300 for 2 mL of industrial glue (such as Tissucol glue, SAS Laboratoire Baxter, Vienna, Austria). Moreover, the autologous glue cost is less than the total cost of the treatment of postoperative complications, including a second surgery to drain a hematoma or seroma with an additional hospitalization night (€200 per additional night in a public hospital) or multiple consultations for managing such complications. In addition, the cost of a postbariatric weight loss sequelae surgery is €1,900 for abdominoplasty, thigh lift, and brachioplasty and €2,500 for reduction mammoplasty.
Thus, the potential benefit of A-PRP glue may warrant its cost in reducing postoperative complications in patients who undergo postbariatric weight loss sequelae surgery.
CONCLUSIONS
By improving hemostasis and tissue adherence, the PRP glue seems to prevent seroma formation after limb lifting and hematoma after breast reduction. The quality of wound healing did not seem to be improved. To confirm these findings obtained in a series of 26 patients who had undergone weight loss sequelae surgery and 25 patients who had undergone breast reduction, it would be interesting to use in future research a valid control group in the context of a randomized controlled trial.
Footnotes
Disclosure: Dr. SidAhmed Mezi obtained a grant from RegenLab for performing her research activity. None of the other authors has any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Lazar CC, Clerc I, Deneuve S, et al. Abdominoplasty after major weight loss: improvement of quality of life and psychological status. Obes Surg. 2009;19:1170–1175. doi: 10.1007/s11695-009-9883-x. [DOI] [PubMed] [Google Scholar]
- 2.Arthurs ZM, Cuadrado D, Sohn V, et al. Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am J Surg. 2007;193:567–570. doi: 10.1016/j.amjsurg.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Jain PK, Sowdi R, Anderson AD, et al. Randomized clinical trial investigating the use of drains and fibrin sealant following surgery for breast cancer. Br J Surg. 2004;91:54–60. doi: 10.1002/bjs.4435. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez EA, Saltzstein EC, Riedner CS, et al. Seroma formation following breast cancer surgery. Breast J. 2003;9:385–388. doi: 10.1046/j.1524-4741.2003.09504.x. [DOI] [PubMed] [Google Scholar]
- 5.Vitug AF, Newman LA. Complications in breast surgery. Surg Clin North Am. 2007;87:431–451, x. doi: 10.1016/j.suc.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 6.El-Sharkawy H, Kantarci A, Deady J, et al. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. J Periodontol. 2007;78:661–669. doi: 10.1902/jop.2007.060302. [DOI] [PubMed] [Google Scholar]
- 7.Burnouf T, Goubran HA, Chen TM, et al. Blood-derived biomaterials and platelet growth factors in regenerative medicine. Blood Rev. 2013;27:77–89. doi: 10.1016/j.blre.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Bielecki T, Dohan Ehrenfest DM. Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF): surgical adjuvants, preparations for in situ regenerative medicine and tools for tissue engineering. Curr Pharm Biotechnol. 2012;13:1121–1130. doi: 10.2174/138920112800624292. [DOI] [PubMed] [Google Scholar]
- 9.Powell DM, Chang E, Farrior EH. Recovery from deep-plane rhytidectomy following unilateral wound treatment with autologous platelet gel: a pilot study. Arch Facial Plast Surg. 2001;3:245–250. doi: 10.1001/archfaci.3.4.245. [DOI] [PubMed] [Google Scholar]
- 10.Man D, Plosker H, Winland-Brown JE. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstr Surg. 2001;107:229–237. doi: 10.1097/00006534-200101000-00037. discussion 238. [DOI] [PubMed] [Google Scholar]
- 11.Welsh WJ. Autologous platelet gel—clinical function and usage in plastic surgery. Cosmet Dermatol. 2000;13:13–19. [Google Scholar]
- 12.Schettino AM, de Oliveira DF, Franco TR. Use en autologous plasma in abdominoplasty: previous note. Rev Col Bras Cir. 2011;38:202–204. doi: 10.1590/s0100-69912011000300012. [DOI] [PubMed] [Google Scholar]
- 13.Vick VL, Holds JB, Hartstein ME, et al. Use of autologous platelet concentrate in blepharoplasty surgery. Ophthal Plast Reconstr Surg. 2006;22:102–104. doi: 10.1097/01.iop.0000202092.73888.4c. [DOI] [PubMed] [Google Scholar]
- 14.Le Louarn C, Pascal JF. The high-superior-tension technique: evolution of lipoabdominoplasty. Aesthetic Plast Surg. 2010;34:773–781. doi: 10.1007/s00266-010-9551-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le Louarn C, Pascal JF. Autologous gluteal augmentation after massive weight loss. Plast Reconstr Surg. 2008;121:1515–1516. doi: 10.1097/01.prs.0000305369.21408.92. [DOI] [PubMed] [Google Scholar]
- 16.van de Kar AL, Corion LU, Smeulders MJ, et al. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116:514–522. doi: 10.1097/01.prs.0000172982.43599.d6. [DOI] [PubMed] [Google Scholar]
- 17.Anzarut A, Guenther CR, Edwards DC, et al. Completely autologous platelet gel in breast reduction surgery: a blinded, randomized, controlled trial. Plast Reconstr Surg. 2007;119:1159–1166. doi: 10.1097/01.prs.0000254344.36092.47. [DOI] [PubMed] [Google Scholar]
- 18.Pluvy I, Panouillères M, Garrido I, et al. Smoking and plastic surgery, part II. Clinical implications: a systematic review with meta-analysis. Ann Chir Plast Esthet. 2015;60:e15–e49. doi: 10.1016/j.anplas.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Coon D, Gusenoff JA, Kannan N, et al. Body mass and surgical complications in the postbariatric reconstructive patient: analysis of 511 cases. Ann Surg. 2009;249:397–401. doi: 10.1097/SLA.0b013e318196d0c6. [DOI] [PubMed] [Google Scholar]
- 20.Grieco M, Grignaffini E, Simonacci F, et al. Analysis of complications in postbariatric abdominoplasty: our experience. Plast Surg Int. 2015;2015:209173. doi: 10.1155/2015/209173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gusenoff JA, Coon D, Rubin JP. Brachioplasty and concomitant procedures after massive weight loss: a statistical analysis from a prospective registry. Plast Reconstr Surg. 2008;122:595–603. doi: 10.1097/PRS.0b013e31817d54a9. [DOI] [PubMed] [Google Scholar]
- 22.Carless PA, Rubens FD, Anthony DM, et al. Platelet-rich-plasmaphersis for minimizing peri-operative allogenic blood transfusion. Cochrane Database Syst Rev. 2003:CD004172. doi: 10.1002/14651858.CD004172. [DOI] [PubMed] [Google Scholar]
- 23.Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489–496. doi: 10.1016/j.joms.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Bhanot S, Alex JC. Current applications of platelet gels in facial plastic surgery. Facial Plast Surg. 2002;18:27–33. doi: 10.1055/s-2002-19824. [DOI] [PubMed] [Google Scholar]


